Abstract
Background
In a previous study, we described the distribution of coronal alignment in a normal asymptomatic population and recognized the occurrence of constitutional varus in one of four individuals. It is important to further investigate the influence of this condition on the joint line orientation and how the latter is affected by the onset and progression of arthritis.
Questions/purposes
The purposes of this study are (1) to describe the distribution of joint line orientation in the coronal plane in the normal population; (2) to compare joint line orientation between patients with constitutional varus and neutral mechanical alignment; and (3) to compare joint line orientation between a cohort of patients with prearthritic constitutional varus and a cohort of patients with established symptomatic varus arthritis.
Methods
Full-leg standing hip-to-ankle digital radiographs were performed in 248 young healthy individuals and 532 patients with knee arthritis. Hip-knee-ankle (HKA) angle and tibial joint line angle (TJLA) were measured in the coronal plane. Patients were subdivided into varus (HKA ≤ −3°), neutral, and valgus (HKA ≥ 3°).
Results
The mean TJLA in healthy subjects was 0.3° (SD 2.0°). TJLA was parallel to the floor in healthy subgroups with neutral alignment (TJLA 0.3°, SD 1.9) and constitutional varus (TJLA 0.2°, SD 2.2°). In patients with symptomatic arthritis and varus alignment, the TJLA opened medially (mean −1.9°, SD 3.5°).
Conclusions
Constitutional varus does not affect joint line orientation. Advanced medial arthritis causes divergence of the joint line from parallel to the floor. These findings influence decision-making for osteotomy and alignment in total knee arthroplasty.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Osteoarthritis is the most common form of arthritis, affecting 30% of adults over the age of 60 years [15]. Causes of knee arthritis have traditionally been divided into biological and mechanical. Although age is a major risk factor for developing osteoarthritis, other risk factors have been identified, including major joint trauma, repetitive stress, obesity, genetic predisposition, kinematic alterations, and lower limb malalignment [3–6]. Current knowledge of the morphological bases of knee osteoarthritis onset and progression is mainly limited to lower limb alignment in the coronal plane [3–6, 25, 26]. A systematic understanding of normal mean values and variance in the population is lacking. We have reported detailed values on the distribution and means of knee alignment in the coronal and axial planes [2, 28]. In these studies, performed on asymptomatic young individuals, we found that a substantial proportion of the population (24%) has so-called constitutional varus, defined as coronal tibiofemoral mechanical alignment of more than 3° varus.
Within the description of coronal alignment, joint line orientation plays an important role [7–12, 22–24]. Varus alignment of the articular surface of the proximal tibia has been reported to be present in 88% of patients with medial compartment osteoarthritis [9]. Cooke et al. [11] identified the distal femoral and proximal tibial anatomy as the major contributors to coronal malalignment. They described the distal femoral and proximal tibial surface in relation to the mechanical axis of, respectively, the femur and tibia. The importance of periarticular knee anatomy as a contributor to overall coronal lower limb alignment was confirmed in asymptomatic patients by Bellemans et al. [2] who showed that distal femoral and proximal tibial anatomy accounted for 70% of varus deformity. Despite the importance of describing the intrinsic geometry of the bone relative to the respective mechanical axis, the coronal joint line orientation, relative to the floor, is an important variable that has received little attention. This relative orientation of the joint line to the floor is an alternative method of evaluating coronal alignment. Its importance lies in the direct biomechanical consequences of joint loading and shear stress [9]. As recent studies argue to step back from mechanical alignment in TKA, and follow the natural slope of the tibial surface in the coronal plane for positioning the tibial plateau, a better understanding of the distribution of joint line orientation in a normal and an arthritic population is relevant information [19–21].
The aims of this study were as follows: (1) to describe the distribution of joint line orientation, relative to the floor, in the coronal plane in the normal population; (2) to compare the joint line orientation between patients with constitutional varus alignment and neutral mechanical alignment; and (3) to compare the joint line orientation between a cohort of patients with prearthritic constitutional varus and a cohort of patients with established symptomatic varus arthritis.
Patients and Methods
We evaluated a total of 780 volunteers and patients; for purposes of comparison, they were considered in two cohorts. The first cohort consisted of 248 healthy volunteers (496 knees) on whom we reported in a previous article [2].The second cohort consisted of a consecutive series of 532 patients with arthritis, planned for surgery, excluding patients with prior osteotomy, lower limb fractures, or fixed flexion deformity. Within this cohort, 315 patients were scheduled for high tibial osteotomy and 217 for TKA. Indications for osteotomy were varus deformity of the lower limb, joint degeneration up to Ahlbäck Grade II [1], and age < 55 years. The patients consented to the analysis of their radiographs and data. The local ethics committee approved the study.
All patients underwent full-leg standing hip-to-ankle digital radiographs. These weightbearing full-leg radiographs were obtained with patients standing barefoot with both feet together and patellae facing forward as described by Paley et al. [24] using an Ysio digital radiography system (Siemens, Erlangen, Germany) with 85 kV and a focus-to-detector distance of 3 m. Adjacent foot position was chosen for being the most reproducible posture. Bipedal stance better approaches foot position during walking than the single-stance position in which the foot is placed under the mass center of gravity of the body. The position of the camera was always parallel to the floor. As mentioned by Skyttä et al. [27], special attention was paid to obtain a true AP projection because even a slight rotation or flexion of the knees can cause distortion of the alignment measurement. The entire leg from the hip to the ankle was visible on the radiograph. Measurements were performed using the measurement functions of the PACS system (Agfa Gevaert, Mortsel, Belgium).
We measured two alignment parameters on each radiograph: hip-knee-ankle (HKA) angle in the coronal plane and tibial joint line angle (TJLA) in the coronal plane. HKA describes the angular relation between the mechanical femoral and tibial axis. These axes were defined by three reference points as indicated by Hagstedt et al. [17]. The first reference point was the center of the femoral head, determined with the use of a digital template with concentric circles. The midpoint of the knee was defined by the center of the femoral condyles at the level of the top of the intercondylar notch and served as a second reference point. The third reference point was the center of the superior facet of the talus. The HKA angle was noted as a deviation from 180°. Negative values represent varus alignment and positive values represent valgus alignment of the lower limb. Based on these measurements, patients were divided into three groups: varus deformity (HKA ≤ −3°), neutral alignment (−3° < HKA < 3°), and valgus alignment (HKA ≥ 3°). The TJLA in the coronal plane was the angle formed between the parallel to the floor and the tangential to the medial and lateral tibial plateau. The Cobb angle function in PACS was used to calculate this angle. These angles were defined as lateral open or medial open. An angle with intersection of both lines located on the lateral side of the leg is named a medial open angle. An angle with an intersection of both lines located on the medial side of the leg is named a lateral open angle. Positive values represent a lateral open angle and negative values a medial open angle (Fig. 1).
Fig. 1.
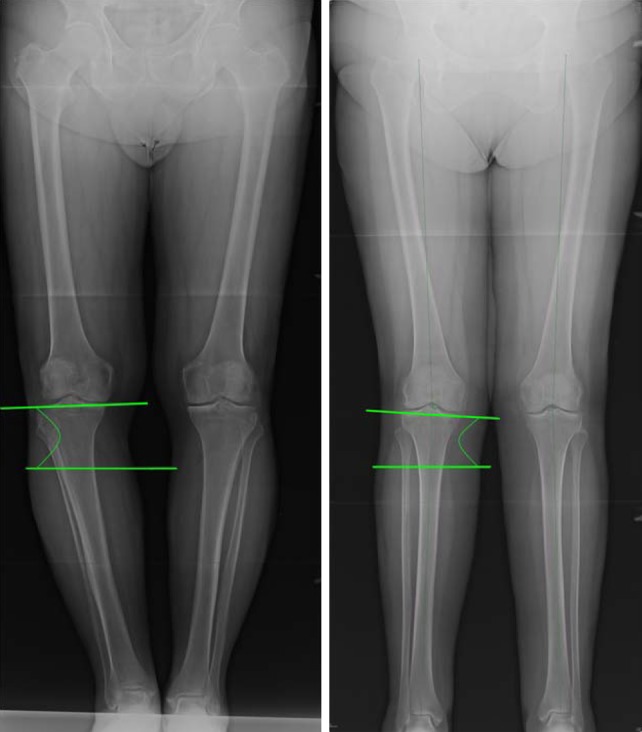
An example is shown of a medial open tibial joint line angle (left) and a lateral open tibial joint line angle (right).
Statistical analysis of the data was performed using the software package SPSS statistics 2.0 (SPSS Inc, Chicago, IL, USA). The data were summarized using descriptive statistics of mean and SD. Normality of the distributions was tested and confirmed using the Kolmogorov-Smirnov test. Pearson’s correlation test was used to find any correlation between HKA and joint line orientation. Mean values in both populations were compared using the independent samples t-test. Differences between two groups were considered statistically significant if the p value was < 0.05 in a two-tailed t-test.
Results
Constitutional varus (HKA ≤ −3°) was present in 24% of the knees within the cohort of asymptomatic subjects (117 of 496); among these, the mean HKA was −4.5° (SD 1.0°). There were 366 (74%) knees with neutral alignment (−3° < HKA < 3°). In this group, the mean HKA was −0.5° (SD 1.5°). Thirteen (2.6%) of the asymptomatic knees showed valgus alignment (HKA ≥ 3°) of the lower limb with a mean HKA of 3.6° (SD 0.6°). The mean HKA of the asymptomatic group overall was −1.3° (varus) (SD 2.3°) with a range between −8.1° and 5.4°. The mean TJLA in the cohort of asymptomatic subjects was 0.3° (SD 2.0°) with a range of −5.9° to 6.2° (Table 1).
Table 1.
Essential mean values of hip-knee-ankle angle (HKA) and tibial joint line angle (TJLA) with SD in Cohorts A and B for the different subgroups
| Cohort A | HKA | TJLA | Cohort B | HKA | TJLA |
|---|---|---|---|---|---|
| All | −1.3° (SD 2.3°) | 0.3° (SD 2.0°) | All | −6.0° (SD 6.2°) | −1.2° (SD 3.7°) |
| Varus (≤ −3°) | −4.5° (SD 1.0°) | 0.2° (SD 2.2°) | Varus (≤ −3°) | −9.0° (SD 4.0°) | −1.9° (SD 3.5°) |
| Neutral | −0.5° (SD 1.5°) | 0.3° (SD 1.9°) | Neutral | −0.9° (SD 1.8°) | −0.5° (SD 2.9°) |
| Valgus (≥ 3°) | 3.6° (SD 0.6°) | 1.8° (SD 2.3°) | Valgus (≥ 3°) | 6.6° (SD 3.1°) | 3.1° (SD 3.8°) |
The mean joint line orientation did not significantly differ between subjects with constitutional varus and subjects with neutral mechanical alignment; in both groups it was parallel to the floor (TJLA 0.2°, SD 2.2° and TJLA 0.3°, SD 1.9°, respectively; p > 0.05; Table 1).
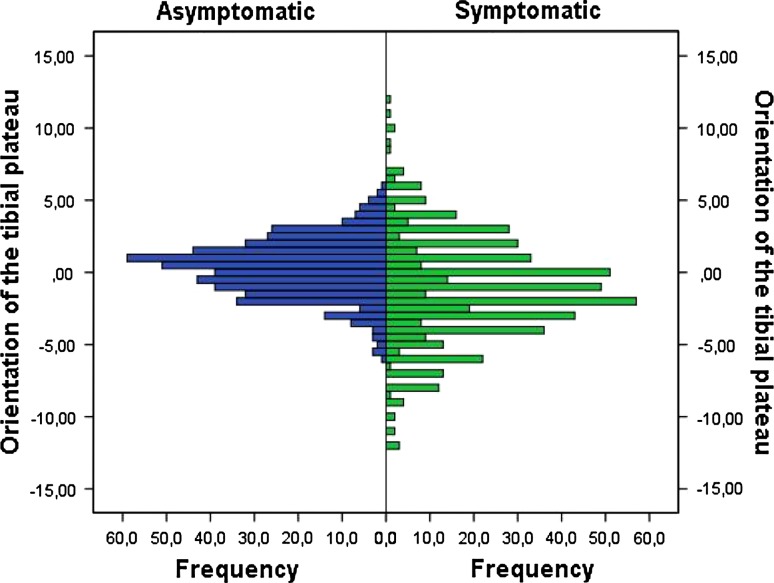
Unlike patients with asymptomatic constitutional varus, joint line orientation in patients with symptomatic varus arthritis was not parallel to the floor. In the cohort of symptomatic arthritic knees (N = 532 knees), we found a mean HKA of −6.0° (varus) (SD 6.2°) with a range between −27.0° and 15.0°. Three hundred eighty-two (71.8%) had varus alignment of the lower limb. The mean HKA in this group was −9.0° (SD 4.0°). The mean TJLA in this cohort of symptomatic arthritic varus knees was −1.9° (SD 3.5°). Cross-cohort comparison between the healthy varus subgroup from cohort 1 versus the symptomatic arthritic varus subgroup from cohort 2 showed a significant difference of TJLA (p < 0.001) between asymptomatic (mean 0.2°, SD 2.2°) and symptomatic knees (mean −1.9°, SD 3.5°). As suggested by the larger SD in the arthritic cohort, this cohort displays a wider distribution of TJLA values. This observation was made in comparing complete cohorts (Fig. 2) as well as in comparing the varus subgroups in both cohorts (Fig. 3).
Fig. 2.
Distribution of the joint line orientation angles in the symptomatic and asymptomatic cohorts is demonstrated.
Fig. 3.
Distribution of the joint line orientation angles in the symptomatic and asymptomatic cohorts for the subgroup with constitutional varus is demonstrated.
Discussion
In this study we wanted to (1) describe the distribution of joint line orientation, relative to the floor, in the coronal plane in the normal population; (2) compare the joint line orientation between patients with constitutional varus alignment and neutral mechanical alignment; and (3) compare the joint line orientation between a cohort of patients with prearthritic constitutional varus and a cohort of patients with established symptomatic varus arthritis.
This study had several limitations. First, some bias may be present in the symptomatic group because a high number of these patients was scheduled for high tibial osteotomy. In the symptomatic cohort of this study, 72% had varus alignment and 9% valgus alignment. As such, the arthritic valgus deformity is somewhat underrepresented in this cohort as compared with an unbiased cohort of patients presenting with end-stage arthritis. Second, the symptomatic cohort consisted only of patients scheduled for corrective surgery. As such, it was a population with more severe complaints than the general osteoarthritis population, representing the more deformed spectrum of the pathology. Third, the method used for measuring coronal alignment is subject to criticism because the three-dimensional geometry of the limb is projected in two dimensions. We selected the method described by Paley et al. [24] because radiology technicians were well trained and had long-standing experience with the patellar orientation method. However, aligning the lower limb with the patella facing forward is a potential risk for rotational errors when there is patellar malalignment [12] but because we excluded patients with fixed flexion deformity, the risk of misinterpreting the HKA angle was minimized.
In recent publications we reported detailed values on the distribution and means of knee alignment in the coronal and horizontal planes, diverging from previous assumptions that ruled for a long time [12, 28]. However, a systematic understanding of the role of joint line orientation and its association with the development of malalignment and arthritis is lacking. Several studies looked at joint line orientation in association with coronal malalignment [2, 7–9, 12, 22–24], but joint line orientation was mostly described in relation to the femoral and tibial mechanical axis [7, 12, 13, 23]. We took a different approach and looked at the orientation of the joint line relative to the floor in bipedal stance. We believed this would shed a different light on the analysis of malalignment because of the orientation of tibial and femoral axis relative to the floor changes with the type and extent of coronal malalignment.
In the asymptomatic cohort that was studied, the main finding was the mean joint line being parallel to the floor (TJLA mean 0.3°, SD 2.0°) when standing with both feet adjacent. These findings are in line with previously published work. According to Kapandji [22], the mechanical axis that passes through the center of the knee makes an angle of 93° with the tibial joint line in the coronal plane during single-leg stance in gait or during two-legged stance with the feet together. This was confirmed by Moreland et al. [23], who showed that the transverse axis of the knee is, on average, oriented with 3° (right knee) and 2.6° (left knee) varus inclination (sloping down medially) with respect to the mechanical axis of the tibia (Fig. 3). In this position, the joint line is parallel to the ground in a single-leg stance or during gait. Slightly smaller values were reported by Chao et al. [7] (1.9°) and Paley et al. [24] (2.2°).
The novel observation from this study is that the joint line appears to maintain its parallelism to the floor, irrespective of the magnitude of nonarthritic varus deformity (TJLA in constitutional varus group 0.2°, SD 2.2°). This can be explained by the fact that the deformity is mainly present in the proximal tibia and distal femur as a result of delayed growth on the medial side induced by mechanical overload during growth. Bellemans et al. [2] attributed this phenomenon to Hueter-Volkman’s law. They showed that in neutrally aligned knees, the mean varus inclination of the tibial plateau relative to the mechanical axis of the tibia is 3°, but in nonarthritic constitutional varus knees, it is 5°. If this tibial joint line angle relative to the tibial mechanical axis increases in constitutional varus knees, why does the joint line remain parallel to the floor? The resulting varus deformity pushes the knee outward, thereby changing the relative position of the tibial mechanical axis to the floor (Fig. 4A–B). This explains why the joint line parallelism is maintained despite the presence of constitutional varus. This phenomenon is not observed in valgus deformity (TJLA mean 1.8°, SD 2.3°), mainly because of the inability of the patient to bring his or her feet together, because the knees touch on the medial side. As such, he or she cannot compensate for the joint line obliquity (Fig. 1). This observation has clinical consequences. In biomechanical modeling of coronal varus malalignment, it is important to keep the joint line parallel to the surface, because this is the setting that is found in individuals with constitutional varus. This joint line orientation will influence the estimated loads that are transmitted through cartilage and subchondral bone. Also, the findings have consequences for the type of osteotomy that is chosen in patients with constitutional varus. After the developmental changes induced by higher loads on the medial growth plate, the correct treatment to restore the anatomy is a medial opening wedge osteotomy [16]. This procedure can correct the proximal tibial joint line orientation. As the overall varus configuration of the lower limb is restored, the corrected tibial joint line will remain parallel to the floor in the standing position with both feet adjacent.
Fig. 5.
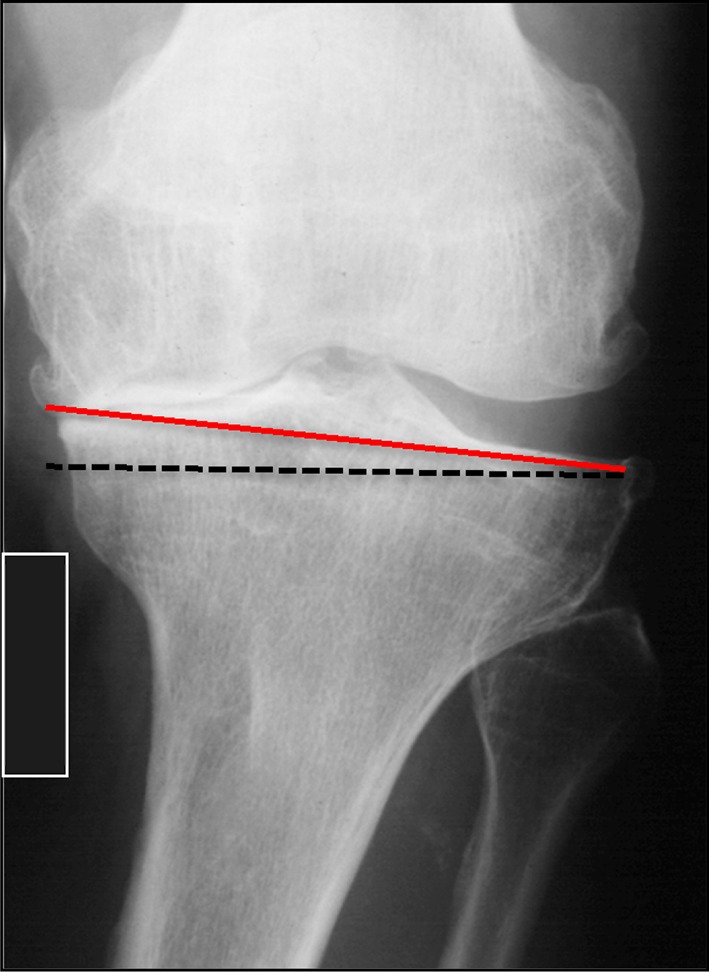
Example of an arthritic knee with constitutional varus (taken from a full-leg standing radiograph). The loss of distal femoral bone pushes the knee further outward and changes the joint line orientation. The red line represents the tangential to the proximal tibia; the dotted black line is the parallel to the floor. Compare the radiographic image with Fig. 4C.
Fig. 4A–C.
(A) Geometric illustration of normal alignment. When the angle a between the floor and the mechanical axis of the tibia equals the angle formed between the mechanical axis of the tibia and the tibial plateau, the joint is parallel to the floor. (B) Geometric illustration of constitutional varus. The proximal tibia displays an increased varus configuration, reducing the angle between the tibial plateau and the mechanical axis of the tibia to a′. As the tibia is pushed outward, the angle between the floor and the mechanical axis of the tibia is also reduced to a′ and the joint line remains parallel to the floor. (C) Geometric illustration of constitutional varus with advanced arthritis. When bone loss is occurring at the level of the distal femur, the intrinsic geometry of the tibia remains unchanged and the angle between the tibial plateau and the mechanical axis remains a′. However, as the tibia is further pushed outward, the angle between the tibial mechanical axis and the floor is reduced to a″ resulting in a medial opening of TJLA (see also Fig. 5). TMA = tibial mechanical axis; FMA = femoral mechanical axis.
A second novel observation was made in comparing the cohort of asymptomatic patients with constitutional varus and the cohort of patients with established, symptomatic varus arthritis. As shown in the results, the TJLA in the nonarthritic constitutional varus knee is substantially different from the TJLA in the arthritic constitutional varus knee. This change in coronal TJLA can be geometrically explained on the basis of femoral bone loss (Fig. 4C). It is in line with observations made by Cooke et al. [10, 11] reporting reduced femoral valgus in patients with medial compartment arthritis. Finally, this analysis has consequences for the concept of kinematic alignment in TKA [19–21]. It can be tempting to aim at restoring the original joint line orientation in TKA, but one should be aware of the specific geometric characteristics of a patient with constitutional varus who developed medial compartment arthritis. Traditional surgical techniques tend to undercorrect coronal deformity in unicompartmental replacement [18], fully correct in TKA [14], and overcorrect in high tibial osteotomy [16]. New techniques tend to copy the original proximal tibial coronal joint line orientation and redress the overall coronal alignment by correcting varus on the distal femur [19–21]. This may induce an oblique TJLA with potentially high loads on the medial proximal tibia and increased shear stress on the polyethylene. So far this has not yet been shown clinically, but awareness of the potential risk is a logic interpretation of the values that were measured in this study.
We conclude that the joint line is parallel to the floor in the coronal plane in asymptomatic individuals. Constitutional varus does not change this observation, but advanced arthritis does cause divergence of the joint line from the parallel to the floor. This finding has consequences for planning alignment correction in osteotomy and arthroplasty. Further research, including gait analysis, is needed to extend this knowledge from the static standing position toward the walking condition.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ahlbäck S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn (Stockh). 1968;Suppl 277:7–72. [PubMed]
- 2.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53. doi: 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belo JN, Berger MY, Reijman M, Koes BW, Bierma-Zeinstra SMA. Prognostic factors of progression of osteoarthritis of the knee: a systematic review of observational studies. Arthritis Rheum. 2007;57:13–26. doi: 10.1002/art.22475. [DOI] [PubMed] [Google Scholar]
- 4.Birmingham TB, Kramer JF, Kirkley A, Inglis JT, Spaulding SJ, Vandervoort AA. Association among neuromuscular and anatomic measures for patients with knee osteoarthritis. Arch Phys Med Rehabil. 2001;82:1112–1118. doi: 10.1053/apmr.2001.24306. [DOI] [PubMed] [Google Scholar]
- 5.Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RMD, Reijman M. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56:1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 6.Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–2636. doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 7.Chao EY, Neluheni EV, Hsu RW, Paley D. Biomechanics of malalignment. Orthop Clin North Am. 1994;25:379–386. [PubMed] [Google Scholar]
- 8.Cooke TDV, Li J, Scudamor RA. Radiographic assessment of bony contributions to knee deformity. Orthop Clin North Am. 1994;25:387–393. [PubMed] [Google Scholar]
- 9.Cooke TDV, Pichora D, Siu D, Scudamore RA, Bryant JT. Surgical implications of varus deformity of the knee with obliquity of joint surfaces. J Bone Joint Surg Br. 1989;71:560–565. doi: 10.1302/0301-620X.71B4.2768297. [DOI] [PubMed] [Google Scholar]
- 10.Cooke TDV, Scudamore A, Greer W. Varus knee osteoarthritis: whence the varus? J Rheumatol. 2003;30:2521–2523. [PubMed] [Google Scholar]
- 11.Cooke TDV, Scudamore A, Li JA, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment. Comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5:39–47. doi: 10.1016/S1063-4584(97)80030-1. [DOI] [PubMed] [Google Scholar]
- 12.Cooke TDV, Sled E. Optimizing limb position for measuring knee anatomical axis alignment from standing knee radiographs. J Rheumatol. 2009;36:471–477. doi: 10.3899/jrheum.080732. [DOI] [PubMed] [Google Scholar]
- 13.Cooke TDV, Sled E, Scudamore RA. Frontal plane alignment. A call for standardized measurement. J Rheumatol. 2007;34:1796–1801. [PubMed] [Google Scholar]
- 14.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(Suppl):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 15.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly: the Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 16.Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2012 Jun 29 [Epub ahead of print]. [DOI] [PubMed]
- 17.Hagstedt B, Norman O, Olsson TH, Tjornstrand B. Technical accuracy in high tibial osteotomy for gonarthrosis. Acta Orthop. 1980;51:963–970. doi: 10.3109/17453678008990901. [DOI] [PubMed] [Google Scholar]
- 18.Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2004;423:161–165. doi: 10.1097/01.blo.0000128285.90459.12. [DOI] [PubMed] [Google Scholar]
- 19.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2012 Sept 21 [Epub ahead of print]. DOI: 10.1007/s11999-012-2613-z. [DOI] [PMC free article] [PubMed]
- 20.Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31:857–863. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 21.Howell SM, Kuznik K, Hull ML, Siston RA. Longitudinal shapes of the tibia and femur are unrelated and variable. Clin Orthop Relat Res. 2010;468:1142–1148. doi: 10.1007/s11999-009-0984-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kapandji IA. The Physiology of Joints: The Lower Limb. Vol 2, 6th ed. Edinburgh, UK: Churchill Livingstone; 2010.
- 23.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 24.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–465. [PubMed] [Google Scholar]
- 25.Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69:1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–196. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 27.Skyttä ET, Lohman M, Tallroth K, Remes V. Comparison of standard anteroposterior knee and hip-to-ankle radiographs in determining the lower limb and implant alignment after total knee arthroplasty. Scand J Surg. 2009;98:250–253. doi: 10.1177/145749690909800411. [DOI] [PubMed] [Google Scholar]
- 28.Victor J, Van Doninck D, Labey L, Van Glabbeek F, Parizel P, Bellemans J. A common reference frame for describing rotation of the distal femur. J Bone Joint Surg Br. 2009;91:683–690. doi: 10.1302/0301-620X.91B5.21827. [DOI] [PubMed] [Google Scholar]