Abstract
Background
Patients with femoroacetabular impingement (FAI) often develop pain, impaired function, and progression of osteoarthritis (OA); this is commonly treated using surgical hip dislocation, femoral neck and acetabular rim osteoplasty, and labral reattachment. However, results with these approaches, in particular risk factors for OA progression and conversion to THA, have varied.
Questions/purposes
We asked if patients undergoing surgical hip dislocation with labral reattachment to treat FAI experienced (1) improved hip pain and function; and (2) prevention of OA progression; we then determined (3) the survival of the hip at 5-year followup with the end points defined as the need for conversion to THA, progression of OA by at least one Tönnis grade, and/or a Merle d’Aubigné-Postel score less than 15; and calculated (4) factors predicting these end points.
Methods
Between July 2001 and March 2003, we performed 146 of these procedures in 121 patients. After excluding 35 patients (37 hips) who had prior open surgery and 11 patients (12 hips) who had a diagnosis of Perthes disease, this study evaluated the 75 patients (97 hips, 66% of the procedures we performed during that time) who had a mean followup of 6 years (range, 5–7 years). We used the anterior impingement test to assess pain, the Merle d’Aubigné-Postel score to assess function, and the Tönnis grade to assess OA. Survival and predictive factors were calculated using the method of Kaplan and Meier and Cox regression, respectively.
Results
The proportion of patients with anterior impingement decreased from 95% to 17% (p < 0.001); the Merle d’Aubigné-Postel score improved from a mean of 15 to 17 (p < 0.001). Seven hips (7%) showed progression of OA and another seven hips (7%) converted to THA Survival free from any end point (THA, progression of OA, or a Merle d’Aubigné-Postel < 15) of well-functioning joints at 5 years was 91%; and excessive acetabular rim trimming, preoperative OA, increased age at operation, and weight were predictive factors for the end points.
Conclusions
At 5-year followup, 91% of patients with FAI treated with surgical hip dislocation, osteoplasty, and labral reattachment showed no THA, progression of OA, or an insufficient clinical result, but excessive acetabular trimming, OA, increased age, and weight were associated with early failure. To prevent early deterioration of the joint, excessive rim trimming or trimming of borderline dysplastic hips has to be avoided.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Surgical hip dislocation with trimming of the head-neck junction and/or acetabulum was the first treatment available for femoroacetabular impingement (FAI) and was commonly approached with hip dislocation [13]. Midterm results of the first reported series of patients treated with surgical hip dislocation and trimming of the head-neck junction and/or acetabulum have shown the beneficial effect of this type of surgery [3]. However, 79% of patients in that study were treated with partial to complete labral resection, and none underwent labral reattachment. It has been shown that labral resection has an adverse effect on the outcome [11, 20, 37]. Therefore, since 2001, the accepted treatment for FAI at our institution has been surgical hip dislocation, resection of the cam lesion at the femoral head-neck junction, and, if necessary, acetabular rim trimming with reattachment of the labrum [10, 43]. To date, no minimum 5-year followup exists for hips after surgical hip dislocation with labral reattachment for the treatment of FAI.
We therefore asked if patients with FAI who underwent surgical hip dislocation with resection of a cam lesion and/or acetabular rim trimming with labral reattachment had (1) improved hip pain and function; and (2) no progression of osteoarthritis (OA); we then determined (3) the 5-year survival rate using the end points defined as the need for conversion to THA, progression of OA by at least one Tönnis grade [46], and a Merle d’Aubigné-Postel score [26] less than 15; and (4) calculated factors predicting these end points at a minimum of 5 years of followup.
Patients and Methods
Since July 2001 reattachment of the labrum has been performed routinely in the course of our surgical hip dislocation procedures for FAI at our institution. We retrospectively reviewed 121 patients (146 hips) who underwent surgical hip dislocation for the treatment of FAI between July 2001 and March 2003. We excluded 35 patients (37 hips [25%]) with FAI after previous surgery including 26 hips after a femoral and/or pelvic osteotomy, six hips after open reduction and internal fixation of the femur and/or acetabulum, and five hips after in situ pinning of a slipped capital femoral epiphysis. Additionally, we excluded 11 patients (12 hips [8%]) with Legg-Calvé-Perthes disease. This resulted in 75 patients (97 hips; Table 1) with idiopathic FAI undergoing surgical hip dislocation with resection of a cam lesion and/or acetabular rim trimming with labrum reattachment. We could followup all patients for a minimum of 5 years (mean, 6 ± 1 years; range, 5–7 years).
Table 1.
Demographic and intraoperative data of the patient series
| Parameters | Value |
|---|---|
| Number of patients (hips) | 75 (97) |
| Age (years)* | 32 ± 8 (15–52) |
| Sex (percentage male of all hips) | 57 |
| Side (percentage right of all hips) | 58 |
| Height (cm)* | 175 ± 11 (152–204) |
| Weight (kg)* | 79 ± 17 (50–145) |
| Body mass index (kg/cm2)* | 25 ± 5 (18–43) |
| Type of FAI | |
| Cam (percentage) | 4 |
| Pincer (percentage) | 11 |
| Mixed (percentage) | 85 |
| Hips with intraoperative labral damage (percentage) | 68 |
| Labral damage classified according to Beck et al. [2]† | |
| Degeneration (percentage) | 39 |
| Full-thickness tear (percentage) | 38 |
| Detachment (percentage) | 23 |
| Maximal incidence of labral damage (position) | 11–1 o’clock |
| Extension of labral damage (hours)*,† | 4.6 ± 1.7 (1–10) |
| Hips with intraoperative cartilage damage (percentage) | 85 |
| Cartilage damage classified according to Beck et al. [2]‡ | |
| Malacia (percentage) | 37 |
| Debonding (percentage) | 34 |
| Cleavage (percentage) | 15 |
| Defect (percentage) | 15 |
| Maximal incidence of cartilage damage (position) | 12 o’clock |
| Extension of cartilage damage (hours)*, ‡ | 4.5 ± 1.7 (1–10) |
* Mean ± SD (range); †only in hips with a labral damage (n = 66); ‡only in hips with cartilage damage (n = 82); FAI = femoroacetabular impingement.
The diagnosis of FAI was based on patient history, examination using the impingement test, and conventional radiographs. FAI was categorized as cam, pincer, or mixed type (Table 1); cam-type FAI was defined as an alpha angle exceeding 50° [31] on the axial view. Pincer-type FAI was present with a minimal lateral center-edge (LCE) angle of 39° [47] and a positive crossover sign [36] or positive posterior wall sign [36] (Table 2). Mixed-type FAI had features of both cam- and pincer-type of FAI on conventional radiographs (Table 1). A contraindication for surgical treatment during the time of this study was advanced OA, defined as a Tönnis grade [45] of III.
Table 2.
Pre- and postoperative radiographic data
| Parameter | Preoperative | Postoperative | p value |
|---|---|---|---|
| Lateral center-edge angle (degrees) [49] | 30 ± 6 (18–46) | 24 ± 7 (10–44) | < 0.001 |
| Acetabular index (degrees) [46] | 4 ± 6 (−11 to 17) | 7 ± 7 (−6 to 25) | < 0.001 |
| Extrusion index (percent) [28] | 21 ± 6 (6–32) | 26 ± 6 (8–39) | < 0.001 |
| ACM angle (degrees) [41] | 44 ± 4 (38–54) | 44 ± 6 (34–56) | 0.134 |
| Crossover sign (percent positive) [36] | 56 | 20 | < 0.001 |
| Retroversion index [44] (percent, of hips with positive crossover sign [36]) | 29 ± 13 (6–53) | 16 ± 12 (6–48) | 0.004 |
| Posterior wall sign (percent positive) [36] | 80 | 87 | 0.167 |
| Ischial spine sign (percent positive) [17] | 46 | 43 | 0.386 |
| Caudocranial coverage (percent) | 82 ± 7 (66–100) | 74 ± 8 (51–91) | < 0.001 |
| Anterior coverage (percent) | 24 ± 6 (11–37) | 18 ± 6 (8–35) | < 0.001 |
| Posterior coverage (percent) | 42 ± 8 (27–64) | 41 ± 8 (22–64) | 0.226 |
| Axial alpha angle (degrees) [31] | 61 ± 11 (37–85) | 46 ± 7 (30–76) | < 0.001 |
Values of continuous parameters are expressed as mean ± SD with range in parentheses.
Preoperative clinical evaluation was performed by different observers and included the patient history, anterior impingement test [44], and full goniometric ROM. As a clinical scoring system, the Merle d’Aubigné-Postel [26] score was used. Substantial inter- and intraobserver agreement has been reported for the anterior impingement test [24], ROM [15, 25, 50], and the Merle d’Aubigné-Postel score [19]. At followup, additional hip scores were assessed including the WOMAC [4], the Harris hip score (HHS) [14], the SF-12 Physical and Mental Component Scales [12, 48], and the University of California Los Angeles (UCLA) activity score [51].
Routine radiographic evaluation consisted of an AP pelvis radiograph and cross-table lateral view of the hip acquired in a standardized manner [44]. One of us not involved with the surgical care of the patients (SDS) assessed these images with the use of a validated software analysis program (Hip2Norm) [42, 45, 52]. This radiographic analysis provided parameters for proximal femoral and acetabular morphology and allows one to correct the measured parameters for malrotation of the pelvis during radiograph acquisition (Table 2).
Surgical hip dislocation was performed according to the technique described by Ganz et al. [13], and during the period of study, labral reattachment was routinely performed. Patients were placed in the lateral decubitus position, and the Gibson interval between the gluteus maximus and medius was dissected. A digastric trochanteric osteotomy was performed and the anterior capsule was exposed through the interval between the piriformis and the gluteus minimus muscle. A Z-shaped capsulotomy was performed. With the hip exposed, impingement was confirmed directly by ranging the hip. The hip was then subluxated, the ligamentum teres was cut, and the hip was dislocated. The remaining ligamentum teres was subsequently excised. The exposed proximal femur and acetabulum were inspected. On the femoral side, we identified the location and extent of the aspherical portion of the femoral head-neck junction using hemispherical plastic templates. On the acetabular side we probed the acetabular cartilage and labrum, and lesions were graded according to Beck et al. [2]. In hips with cam morphology, we corrected the femoral head-neck offset abnormality and trimmed or reattached any torn portions of the labrum. In hips with pincer morphology, the labrum was surgically detached along the area of excessive acetabular coverage, rim trimming was performed until impingement-free ROM was achieved, and the labrum subsequently reattached. Labral ossifications were treated with removal of the ossified portion and reattachment of the remaining healthy labrum. Reattachment of the labrum was performed with titanium bone anchors with nonabsorbable sutures (G II Titanium Anchor; DePuy, Mitek, Norwood, MA, USA) being passed through the base of the labrum and knots being placed on the outer surface. Once all corrections were performed, and impingement-free ROM was verified, the capsule was closed using absorbable sutures. The wound was closed in layers, the greater trochanter reattached with two to three 3.5-mm cortical screws, and a sterile dressing applied.
Our postoperative protocol included immediate use of crutches with partial weightbearing of 15 kg and restricted forced abduction and adduction to protect the trochanteric osteotomy. During their hospital stay, patients were kept on continuous passive motion to prevent capsular adhesions. Full weightbearing was allowed between 6 and 8 weeks, when the trochanteric osteotomy had healed, and abductor training was initiated. Patients were asked to return for evaluation to our clinic at 6 weeks, 3 months, 1 year, 2 years, and 5 years after surgery.
To evaluate for improvement in hip function, the following parameters were assessed preoperatively and at most recent followup: prevalence of a positive anterior impingement test (ie, pain with flexion and internal rotation), ROM (flexion/extension, internal/external rotation, abduction, and adduction), and total Merle d’Aubigné-Postel score [26]. At followup, the WOMAC, HHS, SF-12, and UCLA scores were evaluated and compared with the literature as a result of the missing preoperative values. Intraoperatively, the treating surgeon evaluated labral and cartilage damage. The highest degree of both labral and cartilage damage was assessed using the classification according to Beck et al. [2]. To describe the location of labral and cartilage damage, the clock system was used with the acetabulum divided into 12 sectors corresponding to a clock face [39]. Six o’clock was defined as the middle of the incision of the acetabular notch. For both right and left hips, 3 o’clock was defined as anterior and 9 o’clock as posterior. The location with the maximal incidence and the extent of labral or cartilage damage was evaluated (Table 1). To assess for progression of radiographic OA, AP pelvis radiographs were reviewed preoperatively and at most recent followup and the affected hip was graded using the Tönnis grade for OA [46]. Subsequent surgeries and complications were summarized and the complications were graded according to the adapted Dindo-Clavien complication classification system for orthopaedic surgery [9, 38]. As a result of the retrospective nature of the study, only grade > 1 complications were included (Table 3). We calculated survival at 5-year followup and defined failure if any of the following end points was achieved: conversion to THA, radiographic progression of OA, and a Merle d’Aubigné-Postel score [26] below 15 points at most recent followup. We evaluated demographic and intraoperative data (Table 1) and clinical (Table 4) and radiographic (Table 2) factors to calculate predictive factors for failure using the previously defined end points. The radiographic factors were evaluated with previously defined ranges for a normal acetabulum and deficient and excessive acetabular coverage [40].
Table 3.
Subsequent surgeries and complications graded according to the adapted Dindo-Clavien complication classification system for orthopaedic surgery [9, 38]
| Subsequent surgeries* and complications | Value | Sink classification [9, 38] |
|---|---|---|
| Trochanteric screw removal (percentage) | 25 | – |
| Arthroscopic adhesiolysis (percentage) | 6 | 3 |
| Evacuation of wound hematoma (percentage) | 2 | 3 |
| Irrigation and debridement for subcutaneous wound infection (percentage) | 1 | 3 |
| Refixation of greater trochanter (percentage) | 1 | 3 |
| Revision of iliotibial band dehiscence (percentage) | 1 | 3 |
* Other than THA.
Table 4.
Clinical results preoperatively and at followup of the hips with a preserved joint (n = 90 hips)
| Parameter (best-worst score possible) | Preoperative | Five-year followup | p value |
|---|---|---|---|
| Merle d’Aubigné-Postel score [26] (18–0) | 15 ± 1 (9–17) | 17 ± 1 (12–18) | < 0.001 |
| Pain (6–0) | 4 ± 0.7 (2–5) | 5 ± 0.9 (2–6) | < 0.001 |
| Mobility (6–0) | 6 ± 0.5 (4–6) | 6 ± 0.2 (5–6) | 0.022 |
| Walking ability (6–0) | 6 ± 0.7 (2–6) | 6 ± 0.2 (5–6) | 0.016 |
| WOMAC [4] (0–100) | – | 8 ± 12 (0–52) | – |
| Pain (0–100) | 10 ± 14 (0–56) | ||
| Stiffness (0–100) | 11 ± 14 (0–56) | ||
| Function (0–100) | 7 ± 12 (0–58) | ||
| Harris hip score [14] (100–0) | – | 92 ± 12 (48–100) | – |
| SF-12 [12, 48] | – | – | |
| Physical Component Scale (100–0) | 50 ± 8 (20–65) | ||
| Mental Component Scale (100–0) | 54 ± 8 (21–67) | ||
| University of California Los Angeles activity score [51] (10–0) | – | 7 ± 2 (2–10) | – |
| Anterior impingement test (percent positive) | 95 | 17 | < 0.001 |
| ROM | |||
| Flexion | 102 ± 11 (85–130) | 102 ± 9 (80–130) | 0.926 |
| Extension | 1 ± 4 (0–20) | 0 ± 2 (0–10) | 0.149 |
| Internal rotation | 14 ± 10 (0–45) | 19 ± 8 (0–40) | 0.003 |
| External rotation | 29 ± 11 (5–60) | 30 ± 8 (10–45) | 0.767 |
| Abduction | 31 ± 10 (0–60) | 39 ± 6 (20–50) | < 0.001 |
| Adduction | 21 ± 8 (0–35) | 24 ± 7 (10–40) | 0.200 |
Values of continuous parameters are expressed as mean ± SD with range in parentheses.
We tested normal distribution with the Kolmogorov-Smirnov test. We determined differences in hip function using the paired Student’s t-test for ROM, the Wilcoxon rank sum test for the Merle d’Aubigné-Postel score, and Fisher’s exact test for the incidence of a positive anterior impingement test. We determined differences in OA using the chi-square test. Hips with a conversion to a THA were included and considered as progression of OA. Survival of surgery was calculated using the previously defined three end points and the method of Kaplan and Meier [18]. Predictive factors for failure were calculated using the univariate and multivariate Cox proportional model with corresponding hazard ratios and adjusted hazard ratios [8]. Hazard ratios were calculated with 95% confidence intervals (CIs).
Results
Pain decreased and hip function improved in the large majority of these patients. The incidence of a positive anterior impingement test decreased from 95% preoperatively to 17% at most recent followup (p < 0.001; Table 4). We found an increase in internal rotation (p = 0.003; Table 4) and abduction (p < 0.001; Table 4). Flexion, extension, external rotation, and adduction did not differ (Table 4). The mean total Merle d’Aubigné-Postel score [26] increased from 15 ± 1 (range, 9–17) preoperatively to 17 ± 1 (range, 12–18) at followup as a result of an increase in all subscores (p < 0.001; Table 4). The mean pain subscore [26] of Merle d’Aubigné-Postel improved from 4 ± 0.7 (range, 2–5) preoperatively to 5 ± 0.9 (range, 2–6) postoperatively (p < 0.001; Table 4).
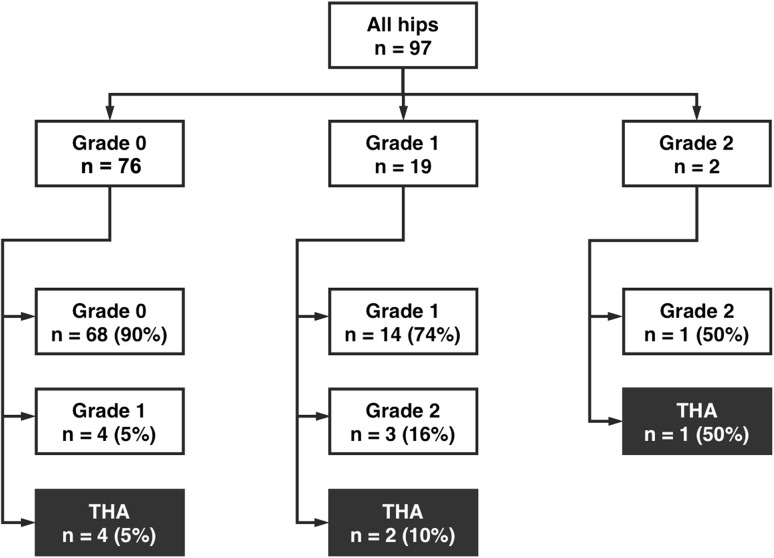
Seven hips (7%) showed progression of OA and another seven hips (7%) were converted to a THA (Fig. 1).
Fig. 1.
Flowchart showing the distribution of osteoarthritis progression and the rate of conversion to THA depending on the preoperative OA score of all 97 hips evaluated.
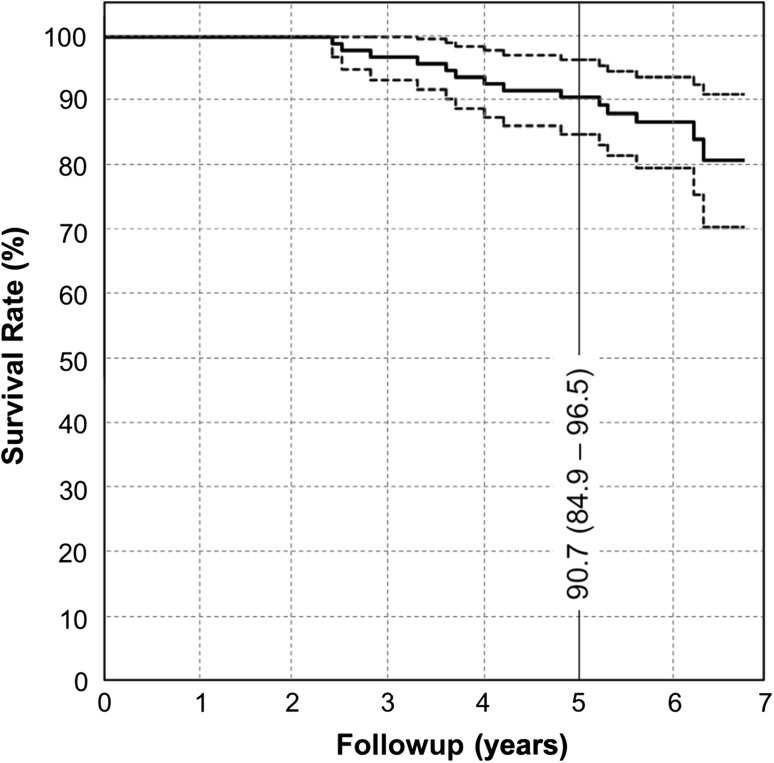
Fifteen hips (15%) reached an end point. Seven hips (7%) were converted to THA after 4 ± 1 years (range, 2–6 years) after the original surgery. Seven hips (7%) showed progression of OA during the followup period. One hip (1%) never had a Merle d’Aubigné-Postel score [26] more than 14 points after the original surgery. Using Kaplan-Meier regression analysis based on the presence of any of these three end points that defined failure, the 5-year cumulative survivorship was 91% (CI, 85%–97%; Fig. 2).
Fig. 2.
The Kaplan-Meier survival analysis is shown with the conversion to THA, progression of OA, and a Merle d’Aubigné-Postel score [26] below 15 points at most recent followup as end points. The cumulative survivorship is shown with the 95% CI in parentheses.
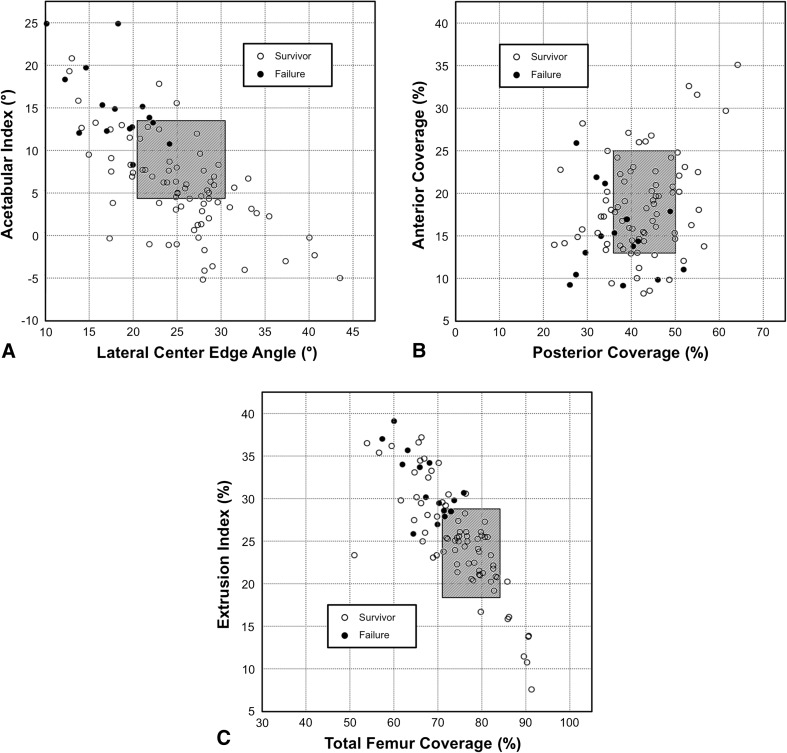
The strongest predictor of failure was an extrusion index > 28% (hazard ratio 11.5; CI, 10.0–13.0); other strong factors included acetabular index > 14° (hazard ratio 6.6; CI, 5.4–7.8), LCE angle < 22° (hazard ratio 5.7; CI, 4.6–7.0), and age > 40 years (hazard ratio 5.6; CI, 4.6–6.7). Overall, we identified 11 univariate predictors for failure including three demographic, two preoperative radiographic, and six postoperative radiographic factors (Table 5). The postoperative radiographic factors were all related to deficient acetabular coverage from excessive débridement of the acetabular rim or trimming of borderline dysplastic hips (Fig. 3). The multivariate analysis identified three predictive factors (Table 5).
Table 5.
Predictive factors for failure with corresponding hazard ratios
| Category | Parameter | Hazard ratio† (95% confidence interval) | p value | Adjusted hazard ratio‡ (95% confidence interval) | p value |
|---|---|---|---|---|---|
| Demographic factors | Age > 40 years | 5.6 (4.6–6.7) | < 0.001 | 11.8 (10.6–13.0) | < 0.001 |
| Weight > 90 kg | 3.4 (2.2–4.6) | 0.05 | |||
| BMI > 25 kg/m2 | 4.4 (3.0–5.7) | 0.03 | |||
| Preoperative radiographic factors | Anterior femoral coverage < 15% | 4.9 (3.6–6.3) | 0.02 | ||
| Osteoarthritis ≥ 1 | 3.9 (2.9–4.9) | 0.001 | |||
| Postoperative factors related to surgical accuracy | LCE angle < 22°* | 5.7 (4.6–7.0) | 0.004 | ||
| AI > 14°* [46] | 6.6 (5.4–7.8) | 0.001 | 6.1 (5.0–7.2) | 0.001 | |
| Extrusion index > 28%* [28] | 11.5 (10.0–13.0) | 0.002 | |||
| Total femoral coverage < 72%* | 4.9 (3.5–6.1) | 0.02 | 6.1 (4.9–7.4) | 0.004 | |
| Anterior femoral coverage < 13%* | 3.6 (2.5–4.7) | 0.02 | |||
| Posterior femoral coverage < 34%* | 3.8 (2.6–5.0) | 0.03 |
* Undercoverage defined by Tannast et al. [40]; †univariate analysis; ‡multivariate analysis; BMI = body mass index; LCE = lateral center-edge angle; AI = acetabular index.
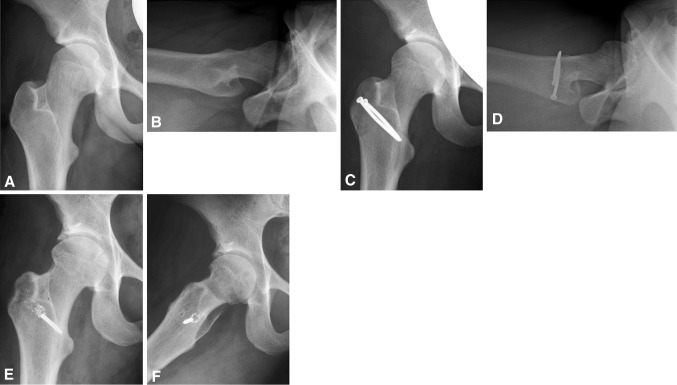
Fig. 3A–C.
Scatterplots showing the six postoperative radiographic factors predicting failure after surgical hip dislocation: failures had (A) an increased acetabular index and decreased LCE angle; (B) a decreased anterior and posterior acetabular coverage; and (C) decreased total femoral coverage or increased extrusion index. These factors all represent insufficient acetabular coverage. Gray boxes represent the normal zone for acetabular orientation, version, and coverage [40].
Discussion
FAI is a painful condition and a proposed etiology for the development of hip OA. Surgical hip dislocation is an accepted treatment of FAI with the goals of surgery being pain reduction, improved function, and preventing development or progression of OA. In reviewing the current surgical technique with labral reattachment developed at our institution, we asked if, at a minimum followup of 5 years, do patients treated with surgical hip dislocation have (1) improved function; and (2) progression of OA. In addition, we asked (3) what is the 5-year survival rate; and (4) what are the predictive factors for failure?
This study has several limitations. First, we do not have control groups of hips with untreated FAI (natural course) or of hips that underwent surgical hip dislocation without labral reattachment. However, it is possible to compare our results with other studies in the literature in which treatment was performed without labral reattachment (Table 6). Second, as a result of its retrospective design, the only clinical scoring system with preoperative values is the Merle d’Aubigné-Postel score. Despite the limited applicability of this relatively insensitive score for patients with FAI, improvements for all three subscores (pain, mobility, walking) were found. For the more detailed scores (WOMAC, HHS, SF-12, and UCLA), only followup results existed, and these were compared with the literature. Additionally, the Merle d’Aubigné-Postel score, the anterior impingement test, and ROM were assessed by different observers throughout the preoperative and followup visits. Nevertheless, substantial inter- and intraobserver agreement has been reported for these parameters [15, 19, 24, 25, 50]; therefore, we believe this does not jeopardize our conclusions in any substantial way. Next, the limited number of 97 hips included in the study series revealed three multivariate predictive factors only (Table 5). A substantial number of the univariate predictive factors were confounding (eg, LCE angle, acetabular index, extrusion index, or anterior, posterior, and total coverage all representing acetabular coverage). It is likely that an increased number of hips included would result in other multivariate predictive factors.
Table 6.
Selected publications with a minimal mean followup of 2 years for the outcome after joint-preserving surgery in hips with femoroacetabular impingement and reported results of labral surgery
| Author (year) | Mean (range of) followup (years) | Number of hips (patients) | Mean age (range) at surgery (years) | Type of surgery | Labral procedure (percent) | Results |
|---|---|---|---|---|---|---|
| Beck et al. [3] (2004) | 4.7 (4–5) | 19 (19) | 36 (21–52) | SHD | 79% resection | 5 hips (26%) converted to a THA, 9 hips (47%) were graded good to excellent using the MAP score; mean OA remained unchanged |
| Murphy et al. [27] (2004) | 5.2 (2–12) | 23 (23) | 35 (17–54) | SHD | 100% labral resection | 7 hips (30%) converted to a THA; hips at risk for failure showed advanced preoperative OA |
| Espinosa et al. [11] (2006) | 2.0 (NR) | I: 25 (20) II: 35 (32) | 30 (20–40) | SHD | I: 100% resection, II: 100% reattachment | At 2-year followup, hips with labrum reattachment showed superior MAP score and less OA progression than those with labrum resection |
| Beaule et al. [1] (2007) | 3.1 (2–5) | 37 (34) | 41 (19–54) | SHD | 95% resection, 5% reattachment | Increase of mean WOMAC, UCLA, and SF-12 score; 6 hips (18%) with no improvement or worsening of the scores |
| Peters et al. [33] (2010) | 2.2 (2–8) | 96 (94) | 28 (14–51) | SHD | 10% resection, 45% reattachment | 5 hips (5%) converted to THA; one hip showed a worse HHS at followup; failures showed advanced preoperative OA |
| Naal et al. [30] (2011) | 3.8 (1–7) | 30 (22) | 20 (16–25) | SHD | 87% reattachment | 21 high-level athletes (96%) with FAI after SHD were competing at a professional level at followup |
| Naal et al. [29] (2012) | 5.0 (2–10) | 233 (185) | 30 (14–55) | SHD | 82% partial débridement, 7% segment resection, 55% reattachment | 83% showed a good to excellent clinical result at followup; conversion to THA or major revision was performed in 14 hips (6%); predictors for poor outcome were female sex, low BMI, and need for microfracturing |
| Chiron et al. [7] (2012) | 2.2 (1–5) | 118 (106) | 34 (19–64) | MO | 43% resected, 1% reattachment | 4 hips (3%) converted to a THA; 18 hips (15%) showed progression of OA by 1° according to Tönnis |
| Laude et al. [22] (2009) | 4.9 (2–9) | 100 (97) | 33 (16–56) | MO/HAS | 40% reattachment, 53% resection | 11 hips (11%) converted to a THA; best results in patients younger than 40 years without preoperative OA; labral reattachment did not correlate with clinical result at followup |
| Lincoln et al. [23] (2009) | 2.0 (1–3) | 16 (14) | 37 (17–51) | MO/HAS | 75% resection | Improved mean HHS; no radiographic progression of OA |
| Ilizaliturri et al. [16] (2008) | 2.4 (2–3) | 19 (19) | 34 (27–43) | HAS | 79% resection | 16 hips (84%) showed an improved WOMAC score, at followup; 3 hips (16%) deteriorated including one conversion to THA |
| Brunner et al. [5] (2009) | 2.4 (2–3) | 53 (53) | 42 (17–66) | HAS | 77% resection | Arthroscopic treatment can improve the rate and level of sports activities in patients with FAI |
| Philippon et al. [34] (2009) | 2.3 (2–3) | 122 (122) | 41 (38–44) | HAS | 44% resection, 48% reattachment | Predictors for better outcome were the preoperative HHS, preoperative radiographic joint space narrowing and labral repair, 10 hips (8%) underwent THA |
| Philippon et al. [35] (2010) | 2.0 (1–4) | 28 (28) | 27 (18–37) | HAS | 100% reattachment | Arthroscopic treatment of FAI with labral repair allows professional hockey player a prompt return to sport; 2 patients (7%) had reinjury and additional hip arthroscopy |
| Byrd and Jones [6] (2011) | Minimum 2 | 100 (100) | 34 (13–76) | HAS | 92% resection | Improved mean HHS, 79 hips (79%) with good to excellent result, no conversion to THA |
| Larson et al. [21] (2012) | 3.5 (2–6) | I: 44 (42) II: 50 (48) | I: 32 (16–57) II: 28 (16–52) | HAS | I: 100% resection, II: 100% reattachment | HHS and VAS pain score was superior in hips with labral reattachment: 92% showed an good to excellent clinical result with labral reattachment compared with 68% with labral débridement |
| Palmer et al. [32] (2012) | 3.8 | 201 (185) | 40 (14–87) | HAS | 97% resection, 3% repair | Improvement in NAHS, pain, and satisfaction level, 12 hips (6%) converted to a THA, higher rate of conversion to THA in hips with preoperative advanced OA |
| Current study | 6.0 (5–7) | 75 (97) | 32 (15–52) | SHD | 100% reattachment | At 5-year followup, 91% preserved the native joint and showed a good clinical result without radiographic evidence of OA progression; excessive trimming of the acetabulum was a major predictor for poor outcome |
NR = not reported; SHD = surgical hip dislocation; MO = miniopen; HAS = hip arthroscopy; MAP = Merle d’Aubigné-Postel score; HHS = Harris hip score; OA = osteoarthritis; UCLA = University of California Los Angeles; FAI = femoroacetabular impingement; BMI = body mass index; VAS = visual analog scale; NAHS = nonarthritic hip score.
We observed decreased pain and improved hip function at last followup. This included a decrease in the incidence of a positive anterior impingement test or pain and an improvement of internal rotation, abduction, and the Merle d’Aubigné-Postel score (Table 4). Internal rotation in flexion is typically decreased in hips with FAI [41] and improvement after surgical correction has been reported [5, 7, 23, 29]. Additionally, improvement in flexion has been reported in these studies [5, 7, 23, 29] but could not be seen in the current study (Table 4). However, we found postoperative improvement in abduction (Table 4), which has not been described so far. In a study using computer-animated hip motion, decreased abduction was found for hips with FAI along with decreased internal rotation in flexion [41]. Improved clinical scores have been found for both labral reattachments and resection (Table 6) [1, 5, 11, 16, 21, 23]. Espinosa et al. [11] found a superior Merle d’Aubigné-Postel score for hips with labral reattachment compared with labral resection after surgical hip dislocation. Larson et al. [21] compared the results of labral reattachment and resection for hips after hip arthroscopy using the HHS. A good to excellent result was found in 92% of hips with reattachment and in 68% of hips with resection. In contrast, Laude et al. [22] found no difference for the clinical results comparing labral reattachment and resection. An improvement in pain has been reported for both labral reattachment and resection (Table 6) [3, 5, 7, 11, 21, 33]. However, Larson et al. [21] reported superior results in pain reduction (using the visual analog scale) comparing labral reattachment and resection after hip arthroscopy. At followup, we found comparable results for the WOMAC [1, 16, 29], HHS [6, 21, 23, 33, 34], SF-12 [1, 29], and UCLA [1] scores reported in the literature for studies with a variable percentage of labral reattachment (Table 6).
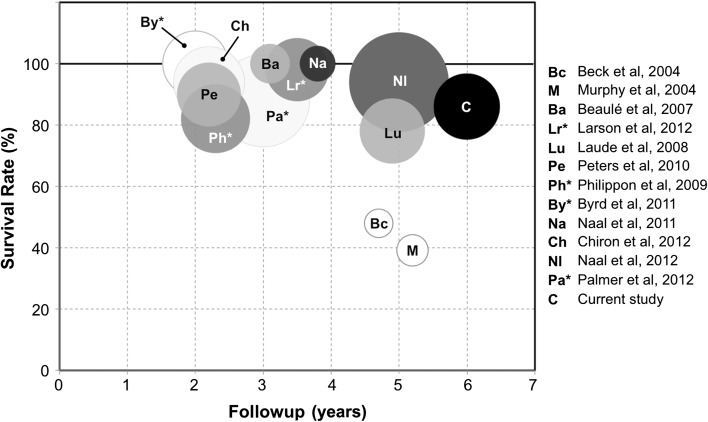
At a minimum 5-year followup, a minority of seven hips (7%) demonstrated progression of OA. This is consistent with results in the literature [11, 29]. In the current study at a 5-year followup, 91% of the hips presented without progression of OA with a good or excellent clinical score without conversion to a THA (Fig. 2). The early results of surgical hip dislocation without labral reattachment [3, 27] are inferior compared with more recent studies including labral reattachment in some or all hips (Fig. 4). As expected, studies reporting the results after arthroscopic treatment have shorter maximum followup compared with those with open treatment (Fig. 4). Nevertheless, the survivorships are comparable to those after surgical hip dislocation (Fig. 4).
Fig. 4.
Graph showing survival rate (conversion to THA) and followup of selected studies in the literature for open and arthroscopic (asterisk) treatment of FAI. The size indicates the number of hips included and the gray scale indicates the percentage of labral reattachment from no reattachment (white) to 100% (black).
We found new predictive factors for failure after surgical hip dislocation, all indicating postoperative acetabular undercoverage (Fig. 3). This likely is the result of too radical acetabular rim trimming or a false indication of acetabular trimming in hips without excessive acetabular coverage (Fig. 5). The strongest predictors for failure were all associated with postoperative undercoverage (extrusion index > 28%, acetabular index > 14°, LCE angle < 22°) or age > 40 years at operation (Table 5). The great majority of failures occurred if one or more of the radiographic parameters describing acetabular coverage were outside a previously described normal range (Fig. 3) [40]. Normative radiographic data [40] can help a surgeon to decide whether rim trimming is possible without the risk of acetabular undercoverage and can be used to quantify the maximal amount of resection possible. Intraoperatively, rim trimming should be performed according to the preoperative planning until impingement-free ROM is achieved. Care must be taken not to trim all the damaged acetabular cartilage per se because this could result in acetabular undercoverage. Known negative predictive factors are preoperative advanced OA [22, 27, 32, 34] and increased age [22]. In contrast to our results with increased weight or body mass index (BMI) being inversely related to failure of the procedure, Naal et al. [29] found a lower BMI in patients with hips that converted to a THA than for those with a preserved joint (21 versus 24 kg/m2).
Fig. 5A–F.
A 25-year-old female patient with (A) normal acetabular coverage and version and (B) a cam-type deformity of the anterosuperior head-neck area. (C) A surgical hip dislocation with (D) trimming of the head-neck area was performed. The torn labrum was reattached and the acetabulum excessively trimmed. At 5-year followup, early joint degeneration occurred with (E) joint space narrowing and acetabular and (F) femoral osteophytes.
Our study showed that surgical hip dislocation for treatment of FAI including labral reattachment improved hip function and clinical scores at a mean of 6-year followup. In over 90% of the patients, this treatment provided a good to excellent clinical result, no progression of OA, and no need for conversion to a THA at 5-year followup. Seven hips (7%) had to be converted to a THA. Preoperative advanced age, advanced OA, and increased weight/BMI represent relative contraindications. Excessive acetabular rim trimming with resulting insufficient femoral coverage leads to early deterioration of the joint.
Footnotes
One or more of the authors have received funding from the Deutsche Arthrose-Hilfe e.V. (SDS) and the Swiss National Science Foundation (MT).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Beaule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Brunner A, Horisberger M, Herzog RF. Sports and recreation activity of patients with femoroacetabular impingement before and after arthroscopic osteoplasty. Am J Sports Med. 2009;37:917–922. doi: 10.1177/0363546508330144. [DOI] [PubMed] [Google Scholar]
- 6.Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27:1379–1388. doi: 10.1016/j.arthro.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 7.Chiron P, Espie A, Reina N, Cavaignac E, Molinier F, Laffosse JM. Surgery for femoroacetabular impingement using a minimally invasive anterolateral approach: analysis of 118 cases at 2.2-year follow-up. Orthop Traumatol Surg Res. 2012;98:30–38. [DOI] [PubMed]
- 8.Cox DR. Regression models and life tables. J Roy Stat Soc B. 1972;34:187–220. [Google Scholar]
- 9.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Espinosa N, Beck M, Rothenfluh DA, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am. 2007;89(Suppl 2):36–53. doi: 10.2106/JBJS.F.01123. [DOI] [PubMed] [Google Scholar]
- 11.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 12.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–1178. doi: 10.1016/S0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 13.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 15.Holm I, Bolstad B, Lutken T, Ervik A, Rokkum M, Steen H. Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–248. doi: 10.1002/pri.204. [DOI] [PubMed] [Google Scholar]
- 16.Ilizaliturri VMJ, Orozco-Rodriguez L, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23:226–234. doi: 10.1016/j.arth.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan EL, Meier P. Nonparametric estimation from incomplete oberservations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 19.Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil. 2005;19:659–661. doi: 10.1191/0269215505cr869oa. [DOI] [PubMed] [Google Scholar]
- 20.Larson CM, Giveans MR. Arthroscopic débridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 21.Larson CM, Giveans MR, Stone RM. Arthroscopic débridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 22.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467:747–752. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lincoln M, Johnston K, Muldoon M, Santore R. Combined arthroscopic and modified open approach for cam femoroacetabular impingement: a preliminary experience. Arthroscopy. 2009;25:392–399. doi: 10.1016/j.arthro.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Martin RL, Sekiya JK. The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J Orthop Sports Phys Ther. 2008;38:71–77. doi: 10.2519/jospt.2008.2677. [DOI] [PubMed] [Google Scholar]
- 25.McWhirk LB, Glanzman AM. Within-session inter-rater realiability of goniometric measures in patients with spastic cerebral palsy. Pediatr Phys Ther. 2006;18:262–265. doi: 10.1097/01.pep.0000234960.88761.97. [DOI] [PubMed] [Google Scholar]
- 26.Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prostesis. J Bone Joint Surg. 1954;36:451–475. [PubMed]
- 27.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Débridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 28.Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. doi: 10.2106/00004623-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Naal FD, Miozzari HH, Schar M, Hesper T, Notzli HP. Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med. 2012;40:1501–1510. doi: 10.1177/0363546512445884. [DOI] [PubMed] [Google Scholar]
- 30.Naal FD, Miozzari HH, Wyss TF, Notzli HP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011;39:544–550. doi: 10.1177/0363546510387263. [DOI] [PubMed] [Google Scholar]
- 31.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 32.Palmer DH, Ganesh V, Comfort T, Tatman P. Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy. 2012;28:1671–1681. doi: 10.1016/j.arthro.2012.04.154. [DOI] [PubMed] [Google Scholar]
- 33.Peters CL, Schabel K, Anderson L, Erickson J. Open treatment of femoroacetabular impingement is associated with clinical improvement and low complication rate at short-term followup. Clin Orthop Relat Res. 2010;468:504–510. doi: 10.1007/s11999-009-1152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 35.Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38:99–104. doi: 10.1177/0363546509346393. [DOI] [PubMed] [Google Scholar]
- 36.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 37.Schilders E, Dimitrakopoulou A, Bismil Q, Marchant P, Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement: a comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg Br. 2011;93:1027–1032. doi: 10.1302/0301-620X.93B8.26065. [DOI] [PubMed] [Google Scholar]
- 38.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J. Reliability of a complication classification system for orthopaedic survey. Clin Orthop Relat Res. 2012;470:2220–2226. doi: 10.1007/s11999-012-2343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tannast M, Goricki D, Beck M, Murphy SB, Siebenrock KA. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;466:273–280. doi: 10.1007/s11999-007-0061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tannast M, Kakaty DK, Zheng G, Siebenrock KA. What is a normal acetabulum? A computer-assisted radiographic study. In: Davies BL, Joskowicz L, Murphy SB, editors. Computer Assisted Orthopaedic Surgery. Berlin, Germany: Pro Business; 2009. pp. 254–257. [Google Scholar]
- 41.Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122–131. doi: 10.1002/jor.20309. [DOI] [PubMed] [Google Scholar]
- 42.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm—reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 43.Tannast M, Siebenrock KA. [Open therapy of femoroacetabular impingement] [in German] Oper Orthop Traumatol. 2010;22:3–16. doi: 10.1007/s00064-010-3001-7. [DOI] [PubMed] [Google Scholar]
- 44.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 45.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 46.Tönnis D. General radiography of the hip joint. In: Tönnis D, editor. Congenital Dysplasia, Dislocation of the Hip. New York, NY, USA: Springer; 1987. pp. 100–142. [Google Scholar]
- 47.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 48.Ware JJ, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 49.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83:7–38.
- 50.Wyss TF, Clark JM, Weishaupt D, Notzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158. doi: 10.1097/BLO.0b013e3180399430. [DOI] [PubMed] [Google Scholar]
- 51.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 52.Zheng G, Tannast M, Anderegg C, Siebenrock KA, Langlotz F. Hip2Norm: an object-oriented cross-platform program for 3D analysis of hip joint morphology using 2D pelvic radiographs. Comput Methods Programs Biomed. 2007;87:36–45. doi: 10.1016/j.cmpb.2007.02.010. [DOI] [PubMed] [Google Scholar]