Abstract
Background
Because of incomplete ossification of the coracoid process and acromion, acromioclavicular joint configuration in the skeletally immature patient differs from that of adults. Although comparison to radiographic standards for this joint is critical in the evaluation of acromioclavicular joint injuries, these standards are not well defined for children or adolescents.
Questions/purposes
We therefore sought to determine (1) the reliability of numerous radiographic measurements of the skeletally immature acromioclavicular joint, including the vertical and shortest coracoclavicular interval, and the acromioclavicular joint offset; (2) the timing of ossification of the acromion and coracoid in males and females; and (3) the differences in the values of these radiographic measurements based on age and sex.
Methods
This study was based on a total of 485 subjects, 8 to 18 years old, who underwent conventional AP view radiographs of both shoulders. The 485 subjects were included to assess normal configuration around the acromioclavicular joint and 466 of these subjects were evaluated for comparison between both sides. The vertical and shortest coracoclavicular interval, coracoclavicular clavicle width ratio, acromioclavicular joint offset, and difference of the coracoclavicular interval of both sides were measured. A reliability test was conducted before obtaining the main measurements. The relationship of measurements with sex, age, and stage of ossification was evaluated.
Results
The vertical and shortest coracoclavicular interval showed excellent reliability (intraclass correlation coefficient ([ICC], 0.918 and 0.934). The acromioclavicular joint offset showed low reliability (ICC, 0.543). The ossification centers of the acromion and the coracoid processes appeared and fused earlier in females than in males. The vertical coracoclavicular interval, which was not affected by partial ossification of the coracoid process, was less than 11 mm in the 90% quantile of total subjects in males and 10 mm in the 90% quantile in females. The difference of the vertical coracoclavicular interval of both sides was less than 50% in 436 of 466 (93.4%) patients.
Conclusions
The vertical coracoclavicular interval was the best parameter to assess acromioclavicular joint dislocation in skeletally immature patients. Comparison of both sides of the acromioclavicular joint could help to inform physicians in predicting the need for additional evaluations.
Level of Evidence
Level III, diagnostic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Acromioclavicular joint dislocations are relatively common in young athletes [11]. Direct force caused by a fall or blow with the arm in the adducted position is the most common mechanism of injury. Approximately 9% of shoulder girdle injuries involve damage to the acromioclavicular joint, and a similar study showed that most acromioclavicular joint dislocations occur in adults in their 20s [10]. In pediatric patients, transphyseal fractures of the distal clavicle usually occur, rather than true acromioclavicular joint dislocation. Because the fracture may mimic an acromioclavicular joint dislocation, it often is called pseudodislocation of the acromioclavicular joint [3]. However, true acromioclavicular joint dislocation in skeletally immature patients sometimes may occur [2, 8].
To diagnose acromioclavicular joint dislocations or pseudodislocations, physical examination and plain radiographs should be performed. These injuries most commonly are categorized according to the Rockwood classification system, which is composed of six types [7, 15]. This classification is based on the coracoclavicular interval and the relationship between the lateral end of the clavicle and the superior border of the acromion. Considerable research has been conducted on treatment outcomes of acromioclavicular joint dislocations based on this classification [10, 11].
Understanding the normal configuration of the acromioclavicular joint is essential to diagnosing abnormalities. There are several studies regarding normal radiologic configuration of the acromioclavicular joint observed on conventional AP view radiographs of the shoulder [1, 5, 13, 16]. In adults, the normal acromioclavicular joint space is 1 to 3 mm wide [16] and diminishes with increasing age [13]. The average distance between the clavicle and coracoid process is between 1.1 and 1.3 cm [1, 5]. Bearden et al. [1] reported that an increase in the coracoclavicular distance of 50% more than the normal side meant complete coracoclavicular ligament rupture. However, because of incomplete ossification of the coracoid process and acromion, measurement values for adults do not apply to the skeletally immature patient. Therefore, acromioclavicular joint injury in the skeletally immature patient can be overdiagnosed and overtreated. Nevertheless, to our knowledge, there are few studies regarding determination of the normal configuration of the acromioclavicular joint on radiographs in skeletally immature patients.
We therefore sought to determine (1) the reliability of numerous radiographic measurements of the skeletally immature acromioclavicular joint, including the vertical and shortest coracoclavicular interval, and the acromioclavicular joint offset; (2) the timing of ossification of the acromion and coracoid in males and females; and (3) the differences in the values of these radiographic measurements based on age and sex.
Patients and Methods
This study was approved by the institutional review board at our institute. Informed consent was waived because the study was retrospective.
We evaluated the radiographs of consecutive subjects to determine their suitability for inclusion in this study. We considered the images of all patients between the ages of 8 and 18 years who had bilateral AP radiographs of the shoulder obtained at our hospital between May 2003 and November 2012. Radiographs taken with the patient in the standing position were included in our study. The exclusion criteria were: (1) fracture around the acromioclavicular joint: clavicle, acromion, and coracoid process; (2) proven acromioclavicular joint injury; (3) other diseases that might affect acromioclavicular joint configuration such as osteochondromatosis; and (4) inadequate shoulder radiographs for measurement.
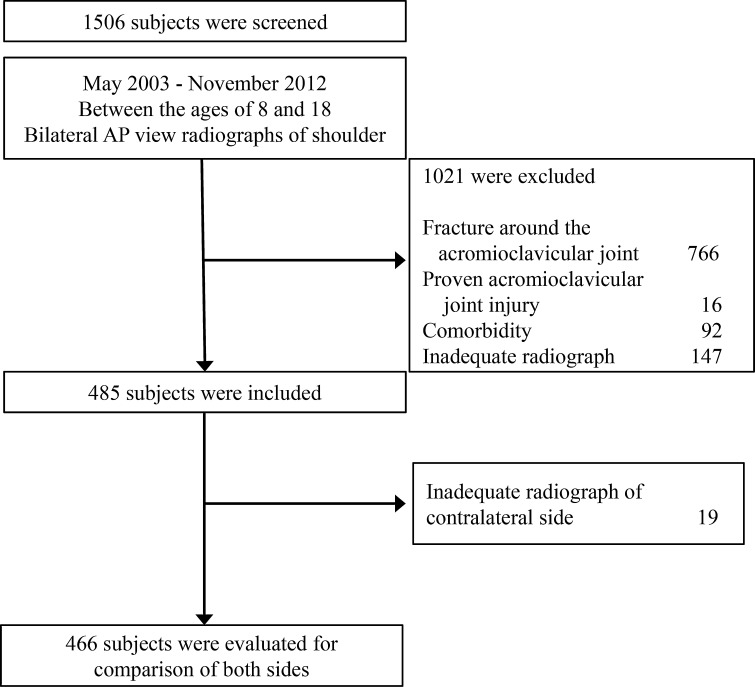
We retrieved conventional AP view radiographs of both shoulders of 1506 children and adolescents 8 to 18 years old. After implementation of inclusion and exclusion criteria, a total of 485 subjects were included to assess normal configuration around the acromioclavicular joint (Table 1) and 466 subjects were evaluated for comparison between both sides (Fig. 1).
Table 1.
Demographic data
| Sex | Age group (years) | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 8–9 | 9–10 | 10–11 | 11–12 | 12–13 | 13–14 | 14–15 | 15–16 | 16–17 | 17–18 | ||
| Male | 29 | 20 | 26 | 22 | 31 | 27 | 38 | 35 | 44 | 55 | 327 |
| Female | 9 | 22 | 14 | 13 | 12 | 13 | 15 | 17 | 19 | 24 | 158 |
| Total | 38 | 42 | 40 | 35 | 43 | 40 | 53 | 52 | 63 | 79 | 485 |
Fig. 1.
The flow chart shows the process for subject selection.
Shoulder radiographs were obtained using a UT 2000 x-ray machine (Philips Research, Eindhoven, The Netherlands) at a source-to-image distance of approximately 100 cm. Settings for the radiographs depended on the patient’s body size: 58 kVp and 6.3 to 8 mAs for smaller patients and 60 kVp and 10 mAs for larger patients. All of the radiographs evaluated were frontal AP views of the shoulder. The right and left shoulders were examined separately. The subjects were not holding weights in their hands at the time that the radiographs were taken. All conventional radiographic images were acquired digitally, and measurements subsequently were made using a picture archiving and communication system (PACS; Infinitt, Seoul, Korea).
Consensus-building Session
Initially, we reviewed the literature to search the index for acromioclavicular joint dislocation. We conducted a PubMed search using the Boolean operator (OR) to combine the keywords (acromioclavicular joint injury [tiab] OR acromioclavicular joint dislocation [tiab] OR acromioclavicular joint separation [tiab] AND English [lang]) from the abstracts. A search on the PubMed database identified a total of 97 published articles. Four relevant articles that assessed measurement values around an acromioclavicular joint on conventional radiographs were chosen [1, 5, 13, 16]. One of the authors (SYL) selected the items that he believed would be relevant to measure acromioclavicular joint dislocation. This literature suggested the coracoclavicular interval and gap of the acromioclavicular joint space as appropriate measurement methods for use on the AP shoulder view. Six orthopaedic surgeons with 25, 9, 7, 5, 4, and 3 years of orthopaedic experience held a consensus-building session before measuring the radiographs. As the literature did not describe the measurement methods in minute detail, the panel decided that the coracoclavicular interval would be measured by using two different methods: the vertical and shortest coracoclavicular intervals. The panel added the acromioclavicular joint offset and excluded the gap of the acromioclavicular joint because they believed that measuring the acromioclavicular joint gap was not appropriate in skeletally immature patients. Finally, the vertical and shortest coracoclavicular interval, acromioclavicular joint offset, coracoclavicular interval-clavicle width ratio, and difference in the coracoclavicular interval of both sides were chosen by panel consensus.
Evaluation of ossification of the acromion and coracoid process on conventional AP view radiographs of the shoulder was performed. Ossification was categorized into three groups: nonossification, partial ossification, and complete ossification. Nonossification was defined as an invisible secondary ossification center of the acromion or coracoid process on radiographs (Fig. 2A). Partial ossification was defined as a visible secondary ossification center incompletely fused with the scapula. A radiolucent line between the secondary ossification center and the scapula can be seen in the partial ossification group (Fig. 2B). Complete ossification is defined as the secondary ossification center fused with the scapula (Fig. 2C).
Fig. 2A–C.

Ossification of the acromion and coracoid process on conventional AP view radiographs of the shoulder is shown. (A) In an 8-year-old boy, there is no evidence of ossification around the acromion and coracoid process. The convex side of the coracoid process is flatter than the full ossified coracoid process seen on the radiograph in Illustration C. (B) Secondary ossifications at the center of the acromion and coracoid process appeared as bony fragments in a 14-year-old boy. (C) In a 17 year-old boy, a radiolucency that was observed between the secondary ossification center and the scapula disappeared.
The coracoclavicular interval was measured by two different methods: the vertical coracoclavicular interval and shortest coracoclavicular interval. The vertical coracoclavicular interval was defined as length of the vertical line to the ground from the highest point of the superior cortex of the coracoid process to the inferior cortex of the clavicle (Fig. 3). The other measurement method of the coracoclavicular interval was the shortest coracoclavicular interval defined as length of the shortest interval between the coracoid and the clavicle (Fig. 3). The coracoclavicular interval could change according to age and body size. Thus, we measured clavicle width and calculated the ratio of the coracoclavicular interval to clavicle width. Clavicle width was measured at the intersection of the inferior cortex of the clavicle and lateral cortex of the second rib (Fig. 3).
Fig. 3.

The measurement methods are shown. The arrows represent the distance to be measured and the direction of the measurement. Vertical coracoclavicular interval (A); shortest coracoclavicular interval (B); clavicle width (C); acromioclavicular joint offset (D).
The acromioclavicular joint offset between the acromial tip and the clavicular tip also was measured. After making a horizontal line to the ground at the point of the superior tip of the acromion, a vertical line was made from the superolateral edge of the clavicle to the horizontal line (Fig. 3). In the case of nonossification of the acromion, the superolateral edge of the scapular spine was used instead of the acromion.
For comparing both sides of the coracoclavicular interval (vertical and shortest coracoclavicular interval), the difference of the two coracoclavicular intervals was divided by the shorter coracoclavicular interval. The measurements were documented as percent.
Reliability Test and Measurement of Parameters
After consensus building, a reliability test was conducted before the main measurements. Interobserver reliability was determined using intraclass correlation coefficients (ICCs) for the three orthopaedic surgeons (KHS, SYL, SHW) with 5, 4, and 3 years of orthopaedic experience, respectively. These three surgeons measured radiographs independently without knowledge of the findings of the other surgeons. Three weeks after measurements were taken by all three surgeons, one surgeon repeated the radiographic measurements to assess intraobserver reliability. After establishing the reliabilities, the main measurements were performed.
Statistical Analysis
In this study, reliability was assessed using ICC and a two-way random effect model, assuming a single measurement and absolute agreement [9, 14]. Using an ICC target value of 0.8, Bonett’s approximation was used in setting 0.2 as a width of 95% CIs [4]. The minimal sample size was calculated to be 36. Therefore, the sample size of a reliability test in this study was set at 40 to select subjects equally from each sex and age group. Four subjects (two males and two females) were randomly selected from each age group (for ages 8.0–18.0 years, 1-year interval).
For the purpose of statistical independence, except the measurements that are compared with the contralateral side, only data from the right shoulder in each patient were included for statistical analysis [12].
To determine the timing of the ossification center of the acromion and coracoid process, multinomial logistic regression was used. The Pearson correlation coefficients were used to determine the correlation between age and measurements on the radiographs. Two-way ANOVA was used to determine whether there was a difference between sex and age group in measurements. The 100-quantiles were calculated to determine the normal value of the coracoclavicular interval. Statistical analyses were performed using SPSS Version 20.0 for Windows (SPSS, Inc, an IBM Company, Chicago, IL, USA). Null hypotheses of no difference were rejected if p values were less than 0.05.
Results
Intraobserver and interobserver reliabilities of measurements were the highest for the shortest coracoclavicular interval (ICC, 0.984 and 0.934) followed by the vertical coracoclavicular interval (ICC, 0.971 and 0.918). Intraobserver and interobserver reliabilities of measurements were the lowest for the acromioclavicular joint offset (ICC, 0.569 and 0.543) (Table 2).
Table 2.
Intraobserver and interobserver reliabilities of measurements
| Measurements | Intraobserver reliability | Interobserver reliability | ||
|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | |
| Ossification of acromion | 0.922 | 0.858–0.958 | 0.868 | 0.790–0.923 |
| Ossification of coracoid process | 0.950 | 0.907–0.973 | 0.886 | 0.817–0.933 |
| Vertical coracoclavicular interval | 0.971 | 0.920–0.987 | 0.918 | 0.862–0.954 |
| Shortest coracoclavicular interval | 0.984 | 0.971–0.992 | 0.934 | 0.890–0.963 |
| Clavicle width | 0.905 | 0.828–0.949 | 0.832 | 0.538–0.928 |
| Vertical coracoclavicular interval-clavicle width ratio | 0.959 | 0.921–0.978 | 0.864 | 0.686–0.936 |
| Shortest coracoclavicular interval-clavicle width ratio | 0.965 | 0.936–0.981 | 0.873 | 0.793–0.926 |
| Acromioclavicular joint offset | 0.569 | 0.314–0.747 | 0.543 | 0.364–0.702 |
| Difference of the vertical coracoclavicular interval (%) | 0.868 | 0.765–0.928 | 0.790 | 0.676–0.874 |
| Difference of the shortest coracoclavicular interval (%) | 0.964 | 0.933–0.981 | 0.873 | 0.793–0.926 |
ICC = intraclass correlation coefficient.
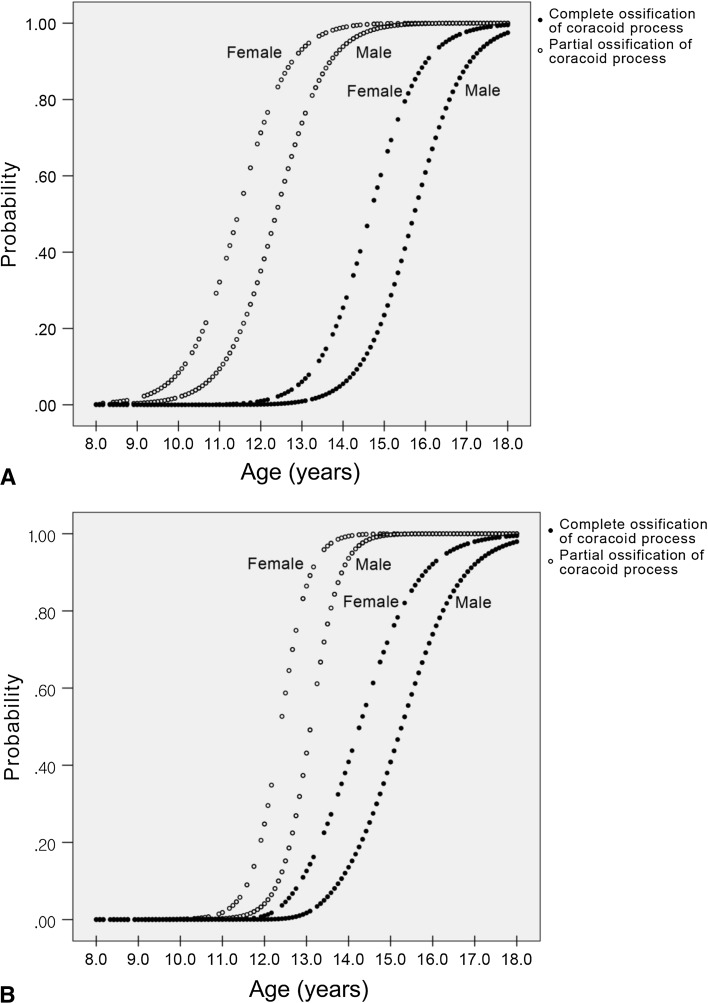
The ossification center of the acromion appeared in females earlier than in males. Complete ossification of the acromion also occurred earlier in females than in males. In males, the ossification center of the acromion occurred at 11 to 18 years and fused from 13 years. Complete ossification of the acromion had not occurred in four of 55 (7.3%) males in the oldest age group (17–18 years). In females, the ossification center of the acromion occurred at 9 to 15 years and fused from 13 to 16 years (Fig. 4A). In the secondary ossification of the coracoid process, the same phenomenon was observed. In males, the secondary ossification center in the coracoid process occurred at 12 to 17 years and fused from 13 years. Complete ossification of the coracoid process had not occurred in four of 55 (7.3%) males in the in the oldest age group (17–18 years). In females, the secondary ossification center in the coracoid process occurred at 12 to 15 years and fused from 13 to 16 years (Fig. 4B). Of the 485 subjects, 37 (7.7%) showed partial ossification of the acromion with nonossification of the coracoid process on radiographs, while only two (0.4%) subjects showed nonossification of the acromion with partial ossification of the coracoid process. This suggests that partial ossification of the acromion tends to develop earlier than partial ossification of the coracoid process. However, 7 (1.4%) subjects had complete ossification of the acromion with partial ossification of the coracoid process, while 28 (5.8%) subjects had partial ossification of the acromion with complete ossification of the coracoid process. This shows a tendency for complete ossification of the coracoid process to be achieved earlier than the acromion.
Fig. 4A–B.
Timing of ossification of (A) the acromion and (B) coracoid process according to sex was analyzed using multinomial logistic regression. The ossification center of the acromion and coracoid process appeared earlier in females than in males. Complete ossification was achieved earlier in females than in males. Complete ossification of the acromion and coracoid process was not achieved in males by 18 years of age.
Males had substantially larger values than females for the vertical coracoclavicular interval (8.6 versus 7.9 mm), shortest coracoclavicular interval (7.8 versus 7.2 mm), and acromioclavicular joint offset (6.4 versus 6.0 mm) (Fig. 5). There were no differences in coracoclavicular-clavicle width ratio and coracoclavicular interval for both sides (Table 3). As children grew older, there were increasing patterns of clavicle width and a decreasing pattern of vertical coracoclavicular interval-clavicle width ratio (Pearson correlation coefficients, −0.436; p < 0.001), the shortest coracoclavicular interval-clavicle width ratio (Pearson correlation coefficients, −0.446; p < 0.001), and acromioclavicular joint offset (Pearson correlation coefficients, −0.410; p < 0.001). The average of the vertical coracoclavicular interval was 8.6 ± 2.3 mm in males and 7.9 ± 2.1 mm in females. In males, the vertical coracoclavicular interval was less than 11 mm in the 90% quantile of all subjects and 12 mm in the 95% quantile of all subjects. In females, the vertical coracoclavicular interval was less than 10 mm in the 90% quantile of all subjects and 11 mm in the 95% quantile of all subjects (Table 4). The vertical coracoclavicular interval was affected only by complete ossification of the coracoid process. There was no difference between the nonossification and partial ossification groups in vertical coracoclavicular interval, whereas the shortest coracoclavicular interval was affected by the secondary ossification center of the coracoid process (Table 5). The difference in vertical coracoclavicular interval of both sides was less than 50% in 436 of 466 (93.4%) patients and 60% in 450 of 466 (96.6%) patients. The difference in the shortest coracoclavicular interval of both sides was less than 50% in 420 of 466 (90.1%) patients and 60% in 440 of 466 (94.4%) patients (Table 6).
Fig. 5A–D.
The estimated mean of measurements (A) vertical coracoclavicular interval, (B) shortest coracoclavicular interval, (C) difference in the vertical coracoclavicular interval, (D) difference in the shortest coracoclavicular interval, and (E) acromioclavicular joint offset, grouped by age and sex, were compared using two-way ANOVA. AC = acromioclavicular; CC = coracoclavicular.
Table 3.
Comparison of measurements by gender
| Measurements | Gender | Age group (years) | Average | p value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 8–9 | 9–10 | 10–11 | 11–12 | 12–13 | 13–14 | 14–15 | 15–16 | 16–17 | 17–18 | ||||
| Vertical coracoclavicular interval | M | 7.7 ± 1.9 | 8.8 ± 2.4 | 9.0 ± 2.4 | 9.4 ± 1.8 | 9.1 ± 2.4 | 8.5 ± 2.3 | 9.2 ± 2.2 | 9.1 ± 3.1 | 8.2 ± 2.0 | 7.7 ± 2.1 | 8.6 ± 2.3 | 0.002 |
| F | 8.2 ± 1.8 | 8.1 ± 2.1 | 8.7 ± 2.2 | 8.9 ± 2.2 | 8.4 ± 1.7 | 7.5 ± 1.4 | 8.3 ± 2.1 | 6.6 ± 1.5 | 7.7 ± 2.7 | 7.8 ± 2.1 | 7.9 ± 2.1 | ||
| Shortest coracoclavicular interval | M | 7.3 ± 1.9 | 8.3 ± 2.3 | 8.4 ± 2.3 | 9.1 ± 1.8 | 8.3 ± 2.2 | 7.8 ± 2.1 | 7.9 ± 2.0 | 8.1 ± 2.9 | 7.3 ± 2.1 | 6.9 ± 2.2 | 7.8 ± 2.2 | 0.002 |
| F | 7.4 ± 1.9 | 7.5 ± 2.1 | 8.1 ± 1.9 | 8.4 ± 2.1 | 7.4 ± 2.1 | 6.5 ± 1.9 | 7.6 ± 2.2 | 5.8 ± 1.8 | 7.0 ± 2.7 | 7.3 ± 2.2 | 7.2 ± 2.2 | ||
| Vertical coracoclavicular interval-clavicle width ratio | M | 0.9 ± 0.3 | 0.9 ± 0.2 | 0.9 ± 0.3 | 1.0 ± 0.2 | 0.8 ± 0.3 | 0.7 ± 0.2 | 0.8 ± 0.2 | 0.7 ± 0.3 | 0.6 ± 0.2 | 0.6 ± 0.2 | 0.8 ± 0.3 | 0.128 |
| F | 0.8 ± 0.2 | 0.9 ± 0.3 | 1.0 ± 0.3 | 1.0 ± 0.3 | 0.9 ± 0.3 | 0.7 ± 0.2 | 0.8 ± 0.2 | 0.6 ± 0.2 | 0.7 ± 0.3 | 0.5 ± 0.2 | 0.8 ± 0.3 | ||
| Shortest coracoclavicular interval-clavicle width ratio | M | 0.9 ± 0.3 | 0.9 ± 0.3 | 0.9 ± 0.3 | 1.0 ± 0.2 | 0.8 ± 0.3 | 0.6 ± 0.2 | 0.7 ± 0.2 | 0.7 ± 0.2 | 0.5 ± 0.2 | 0.5 ± 0.2 | 0.7 ± 0.3 | 0.317 |
| F | 0.8 ± 0.2 | 0.9 ± 0.3 | 0.9 ± 0.3 | 1.0 . ± 0.3 | 0.8 ± 0.4 | 0.6 ± 0.2 | 0.7 ± 0.2 | 0.5 ± 0.2 | 0.7 ± 0.3 | 0.6 ± 0.2 | 0.7 ± 0.3 | ||
| Acromioclavicular joint offset | M | 8.1 ± 2.8 | 6.8 ± 3.1 | 8.8 ± 3.7 | 7.9 ± 2.6 | 7.0 ± 3.4 | 6.5 ± 2.9 | 5.7 ± 2.8 | 4.5 ± 2.6 | 4.6 ± 2.2 | 4.7 ± 1.9 | 6.4 ± 2.9 | 0.016 |
| F | 5.7 ± 3.0 | 6.6 ± 2.9 | 8.2 ± 3.1 | 7.2 ± 1.0 | 5.6 ± 1.7 | 5.1 ± 2.0 | 5.7 ± 2.8 | 3.8 ± 2.2 | 4.9 ± 1.6 | 4.3 ± 2.8 | 6.0 ± 2.6 | ||
| Difference of the vertical coracoclavicular interval (%) | M | 25.2 ± 26.1 | 20.5 ± 16.3 | 14.1 ± 11.6 | 14.0 ± 12.2 | 22.8 ± 23.4 | 20.0 ± 17.1 | 18.8 ± 20.4 | 21.2 ± 18.7 | 21.1 ± 16.8 | 21.7 ± 26.9 | 20.3 ± 18.3 | 0.824 |
| F | 18.6 ± 18.4 | 19.0 ± 15.6 | 15.2 ± 15.5 | 14.4 ± 11.5 | 22.8 ± 21.6 | 19.3 ± 10.8 | 33.2 ± 35.7 | 20.3 ± 15.9 | 25.0 ± 15.7 | 15.1 ± 9.2 | 20.0 ± 22.6 | ||
| Difference of the shortest coracoclavicular interval (%) | M | 28.2 ± 27.5 | 22.8 ± 21.7 | 15.5 ± 12.6 | 15.0 ± 12.3 | 22.5 ± 20.9 | 23.4 ± 19.4 | 22.5 ± 21.5 | 19.1 ± 17.0 | 23.4 ± 22.1 | 28.3 ± 38.2 | 22.9 ± 21.6 | 0.996 |
| F | 26.0 ± 13.9 | 20.4 ± 14.1 | 12.9 ± 16.1 | 15.8 ± 12.1 | 23.7 ± 19.2 | 24.3 ± 19.6 | 41.3 ± 43.8 | 25.3 ± 21.1 | 22.1 ± 23.7 | 17.1 ± 13.3 | 21.3 ± 26.2 | ||
p value provided for gender differences of each measurement.
Table 4.
Reference values of coracoclavicular interval in 100 quantiles
| Coracoclavicular interval | Sex | 100 quantiles | |||
|---|---|---|---|---|---|
| < 50 | < 75 | < 90 | < 95 | ||
| Vertical (mm) | M | 8.0 | 10.0 | 11.0 | 12.0 |
| F | 7.0 | 9.0 | 10.0 | 11.0 | |
| Shortest (mm) | M | 7.0 | 9.0 | 10.0 | 11.0 |
| F | 7.0 | 8.0 | 9.0 | 10.1 | |
Table 5.
Comparison of vertical and shortest coracoclavicular intervals by ossification of coracoid process
| Coracoclavicular interval | Ossification of coracoid process | ||
|---|---|---|---|
| None | Partial | Complete | |
| Vertical (mm) | 8.19 ± 0.17 | 7.89 ± 0.23 | 7.57* ± 0.16 |
| Shortest (mm) | 7.61 ± 0.16 | 6.79* ± 0.22 | 6.74* ± 0.16 |
Values are mean ± SD; * significant difference from nonossification of the coracoid process based on Bonferroni’s multiple comparison test.
Table 6.
Proportion of subjects according to the range of difference of coracoclavicular joint of both sides
| Measurement | Difference of both sides | ||
|---|---|---|---|
| < 40% | < 50% | < 60% | |
| Vertical coracoclavicular interval | 406/466 (87.1%) | 436/466 (93.4%) | 450/466 (96.6%) |
| Shortest coracoclavicular interval | 385/466 (82.6%) | 420/466 (90.1%) | 440/466 (94.4%) |
Discussion
Acromioclavicular joint dislocation sometimes may occur in skeletally immature patients. Although comparison to radiographic standards for this joint is critical for evaluation of acromioclavicular joint injuries, such standards are not well defined for children and adolescents. We therefore sought to determine (1) the reliability of numerous radiographic measurements of the skeletally immature acromioclavicular joint, including the vertical and shortest coracoclavicular intervals and the acromioclavicular joint offset; (2) the timing of ossification of the acromion and coracoid in males and females; and (3) the differences in the values of these radiographic measurements based on age and sex.
The limitations of this study should be addressed before discussing these findings in detail. First, this study is retrospective. All subjects were patients who visited our institution for evaluation of issues with the upper extremity. There could be differences from the general population. However, we excluded all patients with any conditions that could affect the anatomy of the shoulder. Therefore, we believe that our results are representative of normal values measured on conventional radiographs of the shoulder. Second, this is not a comparative study. We assessed the normal value of anatomic configuration around the acromioclavicular joint. Therefore, further evaluation comparing normal values with measurement values of patients with acromioclavicular joint dislocation is needed. Third, most of the patients included in this study were Korean. Owing to potential differences in average skeletal size between Asian and Western populations, the values of the absolute measurements (such as the coracoclavicular interval) obtained in our study could differ from the values of the Western population. In this study, the differences in body size were adjusted based on the coracoclavicular interval-clavicle width ratio and the differences in the coracoclavicular interval between both sides. We thought the ratio reflected the patient’s body size. However, as the children grew older, the ratio decreased with the increase in the clavicle width. Therefore, we believe that the differences in the coracoclavicular interval between both sides can be applied to Western populations. Further evaluation comparing interracial shoulder anatomy is required.
Reliability is used to describe the overall consistency of a measure. It is an important concept in medical practice because it can be used to reduce errors during diagnostic evaluations, during the analysis of responses to questionnaires, and even during surgical procedures [9]. Various statistical methods can be used to test reliability according to the characteristics of the data. The ICC is commonly used to determine the test reliability of continuous variables. According to the reliability test of our study, all measurements except the acromioclavicular joint offset showed excellent intraobserver and interobserver reliabilities. The acromioclavicular joint offset generally is used to diagnose and classify acromioclavicular joint dislocation in adults [11]. However, relatively low intraobserver and interobserver reliabilities of the acromioclavicular joint offset (ICC, 0.569 and 0.543) may lead to a misdiagnosis of acromioclavicular joint dislocation in skeletally immature patients. Therefore, we believe that the acromioclavicular joint offset should not be used to diagnose acromioclavicular joint dislocation in skeletally immature patients.
Secondary ossification centers of the scapula have been described by Caffey [6]. He reported that multifocal secondary ossification in the acromion occurred at 15 to 18 years and fused from 18 to 19 years. A secondary center in the coracoid process occurred in the superior margin at 15 to 17 years and fused to the scapula between 18 and 21 years. In our study subjects, secondary ossification centers of the acromion and the coracoid process occurred and fused earlier than reported by Caffey. In addition, there were differences in timing of secondary ossifications of the acromion and the coracoid process according to sex. In females, the secondary ossifications occurred and fused earlier than in males (Fig. 4).
Previous studies showed that the average distance between the clavicle and coracoid process is between 11 and 13 mm in adults [1, 5]. The measurement method was not described in these studies. We measured the coracoclavicular interval with two different methods, vertical and shortest coracoclavicular intervals. Our results showed that the vertical (8.6 ± 2.3 mm in males, 7.9 ± 2.1 mm in females) and the shortest coracoclavicular intervals (7.8 ± 2.2 mm in males, 7.2 ± 2.2 mm in females) were narrower than the coracoclavicular interval in adults. In our study, the coracoclavicular interval was affected by the ossification stage of the coracoid process. However, the vertical coracoclavicular interval was not affected by partial ossification of the coracoid process. We thought that the shortest coracoclavicular interval was more affected by the ossification stage because the secondary ossification center appeared on the superomedial side of the coracoid process on radiographs. We believe the vertical coracoclavicular interval is more applicable in measuring the relationship between the coracoid and clavicle in skeletally immature patients. Fewer than 10% quantile of patients had a vertical coracoclavicular interval greater than 11 mm in males and 10 mm in females. Additional evaluations should be considered in patients with these criteria. The differences in the coracoclavicular interval of both sides were not affected by sex or age. This is a simple method used to evaluate acromioclavicular joint dislocation for children and adults. The results of our study were consistent with the results of a previous study [1] for adults. Further evaluation should be considered when there is a 50% increase in the interval more than the normal side with clinical symptoms around the acromioclavicular joint.
To the best of our knowledge, normative values for the common radiographic measurement techniques in children and adolescents have not been reported. In the current study, we suggest several measurement values of the acromioclavicular joint of the shoulder measured on conventional AP shoulder radiographs in 8- to 18-year-old children and adolescents. We found the vertical coracoclavicular interval to be the best measurement parameter to assess acromioclavicular joint dislocation in skeletally immature patients. Comparison of both sides of the acromioclavicular joint could help to inform physicians in predicting the need for additional evaluations. For skeletally immature patients with greater than a 12-mm vertical coracoclavicular interval in males, 11-mm vertical coracoclavicular interval in females, and a 50% increase in coracoclavicular interval more than the normal side on a conventional AP view radiograph of a shoulder, additional evaluation, such as stress view radiography or CT, and treatment should be considered, as an acromioclavicular joint dislocation is likely in that situation. In addition, physicians should be careful not to overdiagnose acromioclavicular joint dislocation in skeletally immature patients with a large acromioclavicular joint offset because the acromioclavicular joint offset is wider in younger patients and has relatively low intraobserver and interobserver reliabilities.
Acknowledgments
We thank Ki Hyuk Sung MD and Sung Hun Won MD, for reliability measurements and Mi Sun Ryu BS, for data collection.
Footnotes
Seung Yeol Lee and Soon-Sun Kwon contributed equally to the writing of this article.
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was waived due to retrospective design.
References
- 1.Bearden JM, Hughston JC, Whatley GS. Acromioclavicular dislocation: method of treatment. J Sports Med. 1973;1:5–17. doi: 10.1177/036354657300100401. [DOI] [PubMed] [Google Scholar]
- 2.Bishop JY, Flatow EL. Pediatric shoulder trauma. Clin Orthop Relat Res. 2005;432:41–48. doi: 10.1097/01.blo.0000156005.01503.43<. [DOI] [PubMed] [Google Scholar]
- 3.Black GB, McPherson JA, Reed MH. Traumatic pseudodislocation of the acromioclavicular joint in children: a fifteen year review. Am J Sports Med. 1991;19:644–646. doi: 10.1177/036354659101900616. [DOI] [PubMed] [Google Scholar]
- 4.Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21:1331–1335. doi: 10.1002/sim.1108. [DOI] [PubMed] [Google Scholar]
- 5.Bosworth BM. Complete acromioclavicular dislocation. N Engl J Med. 1949;241:221–225. doi: 10.1056/NEJM194908112410601. [DOI] [PubMed] [Google Scholar]
- 6.Caffey J. Pediatric X-ray Diagnosis. Chicago, IL: Year Book Medical Publishers; 1985. [Google Scholar]
- 7.Dameron TB, Jr, Rockwood CA., Jr . Fractures and dislocations of the shoulder. In: Rockwood CA Jr, Wilkins KE, King RE, editors. Fractures in Children. Philadelphia, PA: JB Lippincott; 1984. pp. 624–653. [Google Scholar]
- 8.Kirkos JM, Papavasiliou KA, Sarris IK, Kapetanos GA. A rare acromioclavicular joint injury in a twelve-year-old boy: a case report. J Bone Joint Surg Am. 2007;89:2504–2507. doi: 10.2106/JBJS.F.01549. [DOI] [PubMed] [Google Scholar]
- 9.Lee KM, Lee J, Chung CY, Ahn S, Sung KH, Kim TW, Lee HJ, Park MS. Pitfalls and important issues in testing reliability using intraclass correlation coefficients in orthopaedic research. Clin Orthop Surg. 2012;4:149–155. doi: 10.4055/cios.2012.4.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316–329. doi: 10.1177/0363546506298022. [DOI] [PubMed] [Google Scholar]
- 11.Pallis M, Cameron KL, Svoboda SJ, Owens BD. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med. 2012;40:2072–2077. doi: 10.1177/0363546512450162. [DOI] [PubMed] [Google Scholar]
- 12.Park MS, Kim SJ, Chung CY, Choi IH, Lee SH, Lee KM. Statistical consideration for bilateral cases in orthopaedic research. J Bone Joint Surg Am. 2010;92:1732–1737. doi: 10.2106/JBJS.I.00724. [DOI] [PubMed] [Google Scholar]
- 13.Petersson CJ, Redlund-Johnell I. Radiographic joint space in normal acromioclavicular joints. Acta Orthop Scand. 1983;54:431–433. doi: 10.3109/17453678308996596. [DOI] [PubMed] [Google Scholar]
- 14.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 15.Williams GR, Nguyen VD, Rockwood CA., Jr Classification and radiographic analysis of acromioclavicular dislocations. Appl Radiol. 1989;18:29–34. [Google Scholar]
- 16.Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases.) Am J Roentgenol Radium Ther Nucl Med. 1971;112:493–506. doi: 10.2214/ajr.112.3.493. [DOI] [PubMed] [Google Scholar]