Abstract
Background
Understanding the type and magnitude of services that patients receive postdischarge and the financial impact of readmissions is crucial to assessing the feasibility of accepting bundled payments.
Questions/purposes
The purposes of this study were to (1) determine the cost and service components of a 30-day total joint arthroplasty (TJA) episode of care; (2) analyze the portion of the total payment that is used for postdischarge services, including home care; and (3) to evaluate the frequency of readmissions and their impact on total episode-of-care payments.
Methods
All payments to Medicare providers (hospitals, postacute care facilities, physicians, and other healthcare providers) for services beginning with the index procedure and extending 30-days postdischarge were analyzed for 250 Medicare beneficiaries undergoing primary or revision TJA from a single institution over a 12 months. Payments and services were aggregated by procedure type and categorized as index procedure, postacute care, and related hospital readmissions.
Results
Mean episode-of-care payments ranged from USD 25,568 for primary TJA in patients with no comorbidities to USD 50,648 for revision TJA in patients with major comorbidities or complications, with wide variability within and across procedures. Postdischarge payments accounted for 36% of total payments. A total of 49% of patients were transferred to postacute care facilities, accounting for 70% of postdischarge payments. The overall 30-day unplanned readmission rate was 10%, accounting for 11% of postdischarge payments.
Conclusions
Episode-of-care payments for TJAs vary widely depending on the type of procedure, patient comorbidities and complications, discharge disposition, and readmission rates. Postdischarge care accounted for more than one-third of total episode payments and varied substantially across patients and procedures.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Total joint arthroplasty (TJA) procedure volumes have risen dramatically in recent years as a result of an aging population, advances in technology, and expansion of indications to include younger, more active patients [2]. At the same time, payers, providers, and policymakers all have placed increased emphasis on strategies to control costs and improve quality associated with elective surgical procedures such as TJA.
So-called value-based payment strategies, including episode-of-care or bundled payments, have been proposed as a mechanism to improve quality and reduce costs of TJA by incentivizing greater communication and coordination among providers across the continuum of care [3, 7]. Episode-of-care payments set a fixed reimbursement amount to be shared among all providers, including physicians, allied health professionals, hospitals, and other facilities, for a defined episode of care that meets certain quality standards. Such an approach requires hospitals and physicians to work collaboratively to manage costs and processes across the continuum of care from a single pool of resources instead of having each service provider charge independently for the portion of care that they provide. These value-based payment models are intended to shift the financial incentives away from volume of services toward more coordinated, reliable care and more predictable results. However, little is known regarding the financial risks assumed by providers who accept bundled payments.
Accordingly, we sought to (1) determine the cost and service components of a 30-day TJA episode; (2) analyze the portion of the total payment that is used for postdischarge services, including home care; and (3) to evaluate the frequency of unplanned, related readmissions and their impact on the total episode-of-care payment.
Patients and Methods
As part of an application to the Center for Medicare & Medicaid Innovation’s Bundled Payments for Care Innovation project, data on payments to all Medicare providers (hospitals, postacute care facilities, physicians, and other healthcare providers) were extracted and analyzed for 250 patients undergoing primary and revision TJA at the authors’ institution over a 12-month period. The institution is a 640 bed tertiary care academic medical center located in an urban area. These data enabled the determination of a bundled cost of care by linking together all payments for services stemming from the initial TJA through to 30 days postdischarge at the individual patient level. The patient population studied was composed of Medicare beneficiaries undergoing a primary or revision TJA. The majority of patients underwent unilateral primary TJA (68%) with 30% undergoing revision surgery and 2% having a bilateral TJA (Table 1).
Table 1.
Number of procedures by MS-DRG
| MS-DRG | Number of cases | Percentage |
|---|---|---|
| 462 Bilateral or multiple major joint procedures of lower extremity without CC/MCC | 6 | 2% |
| 466 Revision of hip or knee arthroplasty with MCC | 9 | 4% |
| 467 Revision of hip or knee arthroplasty with CC | 47 | 19% |
| 468 Revision of hip or knee arthroplasty without CC/MCC | 19 | 8% |
| 469 Major joint arthroplasty or reattachment of lower extremity with MCC | 23 | 9% |
| 470 Major joint arthroplasty or reattachment of lower extremity without CC/MCC | 146 | 58% |
| Total | 250 | 100% |
MS-DRG = Medicare Severity-Diagnosis Related Groups; CC = complication/comorbidity; MCC = major complication/comorbidity.
Payments and services were separated into three categories: index procedure/hospital stay, postacute care, and related hospital readmissions. Index procedure payments included both physician and hospital payments. Postacute care payments included services related to a patient’s stay in acute rehabilitation facilities, skilled nursing facilities, and services obtained as part of home health care. Related hospital readmission payments included physician and hospital fees for unplanned readmissions directly attributable to the surgical episode, including treatment of both medical and surgical complications. Readmissions were defined as related or unrelated based on the International Classification of Diseases, 9th Revision, Clinical Modification diagnosis and procedure codes and Medicare Severity-Diagnosis Related Groups (MS-DRG) codes associated with the readmission. Related readmission payments were captured whether the readmission occurred at the facility where the index procedure occurred or at another hospital.
Results
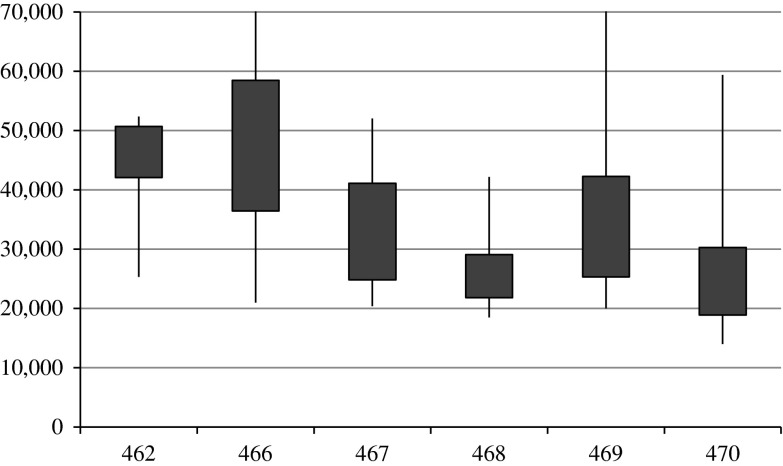
Total payments for a 30-day TJA episode ranges from a mean of USD 25,568 for primary TJAs in patients with no comorbidities or complications to a mean of USD 50,648 for revision TJAs in patients with major comorbidities or complications (Table 2) with wide variability within and across procedures (Fig. 1).
Table 2.
Costs by MS-DRG and expense category
| MS-DRG | Mean index stay payment (facility) | Mean index stay payment (professional fees) | Mean index postacute care payments | Mean readmission payment | Mean total episode payment | Postdischarge payments as percent of total episode payment |
|---|---|---|---|---|---|---|
| 462 | 21,815 | 4149 | 16,214 | 1422 | 43,600 | 40% |
| 466 | 27,060 | 3828 | 13,455 | 6315 | 50,648 | 39% |
| 467 | 19,813 | 3215 | 10,722 | 774 | 34,525 | 33% |
| 468 | 16,967 | 2413 | 5235 | 1464 | 26,079 | 26% |
| 469 | 19,888 | 3407 | 10,300 | 3980 | 37,575 | 38% |
| 470 | 13,862 | 2271 | 8919 | 517 | 25,568 | 37% |
| Total | 16,437 | 2665 | 9443 | 1186 | 29,731 | 36% |
MS-DRG = Medicare Severity-Diagnosis Related Groups.
Fig. 1.
The interquartile range, maximums, and minimums by MS-DRG show the range of episode costs in USD.
The portion of the total episode-of-care payments used for postdischarge payments varied from a low of 26% for revision TJAs in patients without comorbidities or complications (MS-DRG 468) to a high of 40% for bilateral TJAs (MS-DRG 462). Across all procedures, postdischarge payments accounted for an average of 36% of total episode-of-care payments (Table 2). Nearly half of all patients (49%) were transferred to postacute care facilities, ranging from a high of 83% for bilateral TJAs (MS-DRG 462) to a low of 37% for revision TJAs in patients without comorbidities or complications (MS-DRG 468) (Table 3). Of those patients who were transferred, the majority went to a skilled nursing facility (73%) with the remainder going to an inpatient rehabilitation facility (25%) and 1.6% going to a long-term care facility. In terms of total payments, skilled nursing facility stays represented 45% of postdischarge payments, inpatient rehabilitation facilities made up 24% of postdischarge payments, and long-term care facilities accounted for 1.5% of postdischarge payments. On average, postacute care facility payments accounted for 70% of all postdischarge payments.
Table 3.
Discharge disposition by MS-DRG
| MS-DRG | Number of surgical cases | Acute rehabilitation facility | Skilled nursing facility | Long-term care facility | Percent of patients discharged to a postacute care facility |
|---|---|---|---|---|---|
| 462 | 6 | 4 | 1 | 0 | 83% |
| 466 | 9 | 0 | 4 | 1 | 56% |
| 467 | 47 | 6 | 20 | 0 | 55% |
| 468 | 19 | 1 | 6 | 0 | 37% |
| 469 | 23 | 4 | 11 | 0 | 65% |
| 470 | 146 | 16 | 47 | 1 | 44% |
| Total | 250 | 34 | 89 | 2 | 50% |
MS-DRG = Medicare Severity-Diagnosis Related Groups; CC = complication/comorbidity; MCC = major complication/comorbidity.
The overall 30-day unplanned readmission rate across all procedures was 10% with a low of 5.5% for primary TJAs in patients without comorbidities or complications and a high of 33% for revision TJAs in patients with major comorbidities and complications. Overall, related, unplanned readmissions accounted for 11.2% of postdischarge payments. Over two-thirds (68%) of these patients were readmitted to the facility where the index primary TJA was performed (Table 4). The primary reasons for readmission were directly related to the original procedure with direct aftercare (MS-DRGs 559, 560, and 561) and knee procedures with a principal diagnosis of infection (MS-DRGs 486 and 487) accounting for half of the volume of readmissions (50%) (Table 5). Three of 24 of the patients who were readmitted (13%) required revision surgery, accounting for one-fourth (25%) of the total readmission-related costs. One-third (eight of 24) of readmissions were for infection, including one case of septicemia.
Table 4.
Readmission rates by index MS-DRG
| MS-DRG | Number of surgical cases | Number of readmissions | Rate |
|---|---|---|---|
| 462 Bilateral or multiple major joint procedures of lower extremity without CC/MCC | 6 | 1 | 17% |
| 466 Revision of hip or knee arthroplasty with MCC | 9 | 3 | 33% |
| 467 Revision of hip or knee arthroplasty with CC | 47 | 5 | 11% |
| 468 Revision of hip or knee arthroplasty without CC/MCC | 19 | 3 | 16% |
| 469 Major joint arthroplasty or reattachment of lower extremity with MCC | 23 | 4 | 17% |
| 470 Major joint arthroplasty or reattachment of lower extremity without CC/MCC | 146 | 8 | 6% |
| Total | 250 | 24 | 10% |
MS-DRG = Medicare Severity-Diagnosis Related Groups; CC = complication/comorbidity; MCC = major complication/comorbidity.
Table 5.
Readmission cause by MS-DRG
| DRG | Number of readmissions | Average length of stay (days) | Mean total payments |
|---|---|---|---|
| 560 Aftercare, musculoskeletal system and connective tissue with CC | 6 | 4.0 | 8029 |
| 561 Aftercare, musculoskeletal system and connective tissue without CC/MCC | 3 | 6.0 | 3652 |
| 576 Skin graft and/or débridement excision for skin ulcer or cellulitis with MCC | 2 | 16.0 | 17,477 |
| 486 Knee procedures with principal diagnosis of infection with CC | 2 | 8.0 | 15,350 |
| 487 Knee procedures with principal diagnosis of infection without CC/MCC | 2 | 6.0 | 9513 |
| 466 Revision of hip or knee arthroplasty with MCC | 1 | 47.0 | 41,566 |
| 467 Revision of hip or knee arthroplasty with CC | 1 | 5.0 | 22,064 |
| 468 Revision of hip or knee arthroplasty without CC/MCC | 1 | 8.0 | 14,965 |
| 493 Lower extremity and humerus procedure except hip, foot, femur with CC | 1 | 1.0 | 14,945 |
| 559 Aftercare, musculoskeletal system and connective tissue with MCC | 1 | 10.0 | 12,493 |
| 857 Postoperative or posttraumatic infections with operating room procedure with CC | 1 | 4.0 | 12,354 |
| 501 Soft tissue procedures with CC | 1 | 4.0 | 11,895 |
| 872 Septicemia without mechanical ventilation 96+ hours without MCC | 1 | 5.0 | 9044 |
| 863 Postoperative and posttraumatic infections without MCC | 1 | 3.0 | 6857 |
| 392 Esophagitis, gastroenteritis, and miscellaneous digestive disorders without MCC | 1 | 4.0 | 6452 |
| 603 Cellulitis without MCC | 1 | 3.0 | 5570 |
| 690 Kidney and urinary tract infections without MCC | 1 | 3.0 | 5413 |
| 641 Nutritional and miscellaneous metabolic disorders without MCC | 1 | 2.0 | 4975 |
| Total | 28 | 7.1 | 11,157 |
MS-DRG = Medicare Severity-Diagnosis Related Groups; CC = complication/comorbidity; MCC = major complication/comorbidity.
A total of 61% of patients received home health services, ranging from a low of 22% (two of nine patients) for revision TJAs in patients with major comorbidities and complications (MS-DRG 466) to a high of 67% for bilateral TJAs (MS-DRG 462) and accounting for an average of 17% of postdischarge payments across all procedures. Forty-three different home care agencies, including our institution’s own home health service, provided services to these 151 patients.
Discussion
We found that episode-of-care payments for primary and revision TJAs, inclusive of the index procedure and 30 days postdischarge, varied widely based on procedure type, patient comorbidities and complications, discharge disposition, and rates of unplanned readmissions. Furthermore, a considerable percentage (over 35%) of episode-of-care payments were related to postdischarge care.
Our study has several limitations. First, our findings are limited to patterns of care at a single academic institution. Further analysis will be necessary to determine whether our findings are generalizable to other TJA care delivery sites. However, we believe all hospitals and physicians that perform TJAs would benefit from evaluating their specific episode-of-care costs to understand the cost and service provision differences across each phase of the episode of care. Second, we only evaluated episode-of-care payments that were related to the index procedure and 30 days postdischarge. Certain bundled payment models may incorporate payments associated with preoperative testing and a longer duration of postoperative care, which could result in a different allocation of costs and services across the episode of care. Finally, we did not attempt to assess patient-reported functional outcomes; true value-based payment methodologies would incentivize high-value care from the patient’s perspective, which would necessitate a better understanding of the impact of bundled payments on patient-reported functional outcomes.
The rationale for bundled payments is that by paying a group of providers a fixed fee for all services provided for a patient with a particular condition or procedure, rather than piecemeal, those providers have an incentive to work collaboratively to deliver high-quality, coordinated care at the lowest possible cost. There is, however, a potential downside risk; in addition to incentives to provide the most appropriate care at the lowest possible cost, bundled payments also have the potential to create incentives to withhold care. Therefore, bundled payments require quality monitoring to assure that providers do not skimp on care and that patient outcomes do not suffer. The experiences of changes in treatment patterns resulting from the Medicare prospective payment system and earlier fixed-fee payment pilots should inform the design, implementation, and monitoring of new bundled payment models [1].
TJA has been an important testing ground for episode-based payment models. This is primarily because of the fact that despite their high volume and relatively homogeneous patient population, TJAs vary widely in both cost and quality [8]. In 2009, Medicare introduced the Acute Care Episode (ACE) demonstration project, in which physician-hospital organizations negotiated a prospective payment to cover both the inpatient facility (Part A) and inpatient physician (Part B) costs for patients undergoing TJA (and selected cardiovascular procedures). Although limited to facilities in the southwestern United States, participating centers reported lower costs with no negative impact on patient outcomes [4, 5, 10].
Bundled payment methodologies require a system for determining which services are included in the bundle and which are not. This can be straightforward in a healthy patient who undergoes a unilateral TJA but can be more challenging patients in with polyarticular arthritis and/or multiple medical comorbidities. In these cases, it can be difficult to determine which conditions and treatments are related to the index procedure and which are not. Because episode-of-care payments are fixed, there is a need for appropriate risk and case-mix adjustment. Without appropriate adjustment for patient and procedure-related differences, bundled payment methodologies could encourage hospitals and physicians to avoid providing care for more complex patients with multiple comorbid diseases, leaving this vulnerable population with limited access to care. Strategies tested in other bundled payment models such as outlier payments, required reinsurance, and gain/loss caps can help to mitigate the incentive to “cherry-pick” only healthy patients [9].
Vertical integration across the continuum of care, including inpatient and postacute care facilities, enables greater coordination of care and the potential to provide higher quality, lower cost care. Although our health system does not own any postacute care facilities, we do have our own home health service, which facilitates greater communication and coordination of care between inpatient and home health providers.
Finally, although episode-of-care payments may provide incentives to reduce the overall cost of care for patients who have TJAs, they do not address the question of whether the procedure was appropriate in the first place. To that end, bundled payments alone will not solve the value conundrum; inappropriate care at lower cost will not enhance the value of TJAs. Therefore, it will be important to a priori define the appropriate indications for TJAs and to incorporate patient preferences and values into complex medical decision-making regarding the timing of TJAs [11]. Currently, there are no explicitly defined referral criteria from the primary physician to an orthopaedic surgeon for evaluation and consideration for TJA, a deficiency at the start of the care pathway, which may lead to an inequitable and skewed distribution of procedures [6].
In summary, we found that episode-of-care payments for TJAs vary widely depending on the type of procedure (eg, primary versus revision), patient comorbidities and complications, discharge disposition, and readmission rates. Postdischarge care accounted for over one-third of total episode-of-care payments and varied substantially across patients and procedures. Nearly one in 10 patients was readmitted for a surgical or medical complication related to the TJA with significant variability in the readmission rate across the procedure types. Postacute care (skilled nursing facility, acute rehabilitation facility, and home health services) accounted for over 70% of postdischarge payments. Understanding the breakdown of costs and services across the entire episode of care is fundamental to a thorough assessment of the feasibility of implementing bundled payments.
Acknowledgments
We thank Vanessa Chan MPH, for her assistance in preparing this manuscript.
Footnotes
Financial support was received from the California Health Care Foundation (KJB) and the University of California Center for Health Quality and Innovation (KJB).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that the institution where the work was performed approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at University of California, San Francisco, CA, USA.
References
- 1.Altman SH. The lessons of Medicare’s prospective payment system show that the bundled payment program faces challenges. Health Aff (Millwood). 2012;31:1923–1930. doi: 10.1377/hlthaff.2012.0323. [DOI] [PubMed] [Google Scholar]
- 2.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012;366:1075–1077. doi: 10.1056/NEJMp1113361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis C. Bundled payments: Lessons learned from the ACE demo. 2010. Available at: http://www.fiercehealthfinance.com/story/bundled-payments-lessons-learned-ace-demo/2010-06-30. Accessed October 3, 2012
- 5.Dunn L. Bundled Pricing Opportunities & Challenges: Q&A With Baptist Health System’s Michael Zucker 2010. Available at: http://www.beckershospitalreview.com/hospital-physician-relationships/bundled-pricing-opportunities-a-challenges-qaa-with-baptist-health-systems-michael-zucker.html. Accessed October 3, 2012
- 6.Mandl LA. Determining who should be referred for total hip and knee replacements. Nat Rev Rheumatol. 2013 Mar 12. doi: 10.1038/nrrheum.2013.27 [Epub ahead of print] [DOI] [PubMed]
- 7.Mechanic RE. Opportunities and challenges for episode-based payment. N Engl J Med. 2011;365:777–779. doi: 10.1056/NEJMp1105963. [DOI] [PubMed] [Google Scholar]
- 8.Robinson JC, Pozen A, Tseng S, Bozic KJ. Variability in costs associated with total hip and knee replacement implants. J Bone Joint Surg Am. 2012;94:1693–1698. doi: 10.2106/JBJS.K.00355. [DOI] [PubMed] [Google Scholar]
- 9.Sood N, Huckfeldt PJ, Escarce JJ, Grabowski DC, Newhouse JP. Medicare’s bundled payment pilot for acute and postacute care: analysis and recommendations on where to begin. Health Aff (Millwood). 2011;30:1708–1717. doi: 10.1377/hlthaff.2010.0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whittingon GL. Acute Care Episode (ACE) Demonstration. 2010. Available at: http://www.stxhfma.org/files/file/Presentations/2010_05_Whittington_ACEDemonstration_2up.pdf. Accessed October 3, 2012
- 11.Youm J, Belkora J, Chan V, Bozic KJ. The emerging case for shared decision making in orthopaedics. J Bone Joint Surg Am. 2013;62:587–594. [PubMed] [Google Scholar]