Abstract
Osteonecrosis of the jaw (ONJ) is a clinical condition associated with long-term exposure to inhibitors of bone resorption, mainly bisphosphonates. Denosumab (DMab) is a human monoclonal antibody of the receptor activator of nuclear factor kappa-B ligand. It prevents osteoclast-mediated bone resorption and is widely prescribed for the management of postmenopausal osteoporosis. Whereas ONJ has already been reported in women treated with DMab, we report for the first time the development of ONJ, following tooth extraction, in a male patient treated for idiopathic osteoporosis with DMab. Due to the constant increase in DMab prescription, for the management of osteoporosis, in both genders, physicians should be made aware of this potential risk.
Keywords: Denosumab, Jaw, Osteonecrosis, Osteoporosis
Osteoporosis is widely considered to be much more prevalent in women even though approximately 39 % of new osteoporotic fractures estimated to have occurred worldwide in the year 2000 were in men [1]. Men have greater morbidity and mortality rates due to hip fractures compared to women [2]. Most of the drugs currently available to treat osteoporosis in women show a similar response in men than that observed in postmenopausal osteoporosis [1].
A 58-year-old Caucasian man was diagnosed with idiopathic, predominantly trabecular, osteoporosis (OP) in June 2012, based on the following:
A previous history of three atraumatic rib fractures (2005)
A bone mineral density T-score of −2.9 and −1.5 at the lumbar spine and femoral neck, respectively
The prevalence of a morphometric vertebral deformity (semi quantitative Grade 2) at T8
Serum 25 (OH) Vitamin D was in the lower range of recommended values [3] (60 nmol/l) and serum intact parathormone was slightly abnormal at 27 pg/ml (normal range, 4–26 pg/ml) [1–84 PTH (DiaSorin, Stillwater, MN, USA] [4]. The absolute 10-year fracture risk calculated with the FRAX® algorithm was 17 and 3.9 % for major osteoporotic and hip fracture, respectively. These values are above the thresholds for therapeutic interventions that were previously published for Belgium [5, 6].
All investigations for causes of secondary osteoporosis remained negative. Due to past history of myocardial infarctions (2002 and 2009), hypertension (i.e., controlled with simvastatin), and the suspicion of a potentially poor adherence to oral medications, denosumab (DMab)(Prolia®, Amgen) was initiated (July 12) at a dose of 60 mg, given subcutaneously every 6 months together with daily supplementation of calcium (1 g/day) and vitamin D (800 IU/day).
DMab is a human monoclonal antibody of the receptor activator of nuclear factor kappa-B ligand (RANKL). It competes with RANKL for RANK-binding sites, thereby preventing osteoclast-mediated bone resorption [7]. DMab is a well-established, widely-prescribed treatment for the management of postmenopausal osteoporosis [8].
It should be noted that despite promising clinical results were published in male patients with low bone mineral density [9] and notwithstanding DMab was recently shown to be cost-effective compared to oral bisphosphonates (BP) in osteoporotic men [10], this chemical entity is not yet approved nor marketed in Europe for the treatment of osteoporosis in males [1].
During DMab treatment (November 2012), extraction of a right wisdom tooth took (48) place and was followed by a mild, slightly progressive pain in the right mandible. A dentist initiated (December 2012) systemic antibiotherapy (AB) (amoxicillin, 1.5 g/day) and antibacterial mouth rinse with no impact on the symptoms.
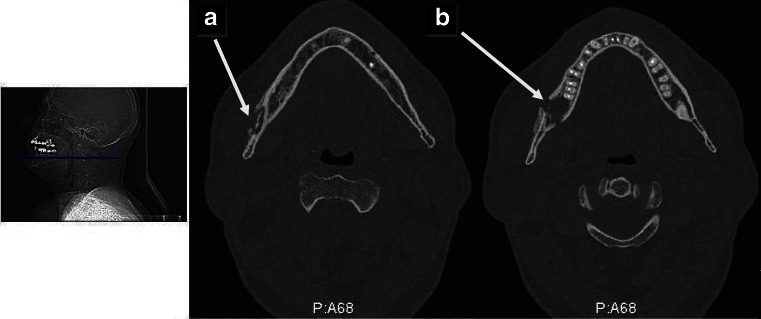
The patient was referred to us (April 2013). Clinical examination revealed oral lesions with bone exposure. CT of the right mandible showed an extensive osteolysis, with a sequestrum in the medullary cavity, surrounded by a periosteal thickening, highly suggestive of an osteonecrosis of the jaw (ONJ), subsequent to a mandibular osteomyelitis (Fig. 1).
Fig. 1.
CT scan of the right mandible revealing osteonecrosis. a Sequestrum in the medullary cavity (white arrow) and b extensive osteolysis of the right mandible (white arrow)
Concomitant malignant tumor was excluded. Treatment included AB coverage, removal of necrotic bone, and treatment with a bone anabolic agent (teriparatide, 20 g/day subcutaneously) with the maintenance of a calcium and vitamin D daily supplementation.
ONJ is a clinical condition that presents as exposed bone in the mandible, maxilla, or both, that persists for at least 8 weeks, in the absence of previous radiation and of metastases in the jaw. Whereas no epidemiologic data on the incidence of ONJ in the general population are available, a positive relationship was described between ONJ occurrence and the use of inhibitors of bone resorption (mainly BP) in patients with multiple myeloma, metastatic breast cancer, Paget’s disease, osteoporosis, or other skeletal disorders [11]. Several pathogenic mechanisms have been proposed. One of them suggests that ONJ can be caused by BP-induced low-bone turnover, which leads to decreased blood flow and bone cell necrosis and apoptosis. In conjunction with chronic oral or dental infection, this leads to the development of exposed, nonhealing bone areas in the mouth [12]. The use of inhibitors of bone resorption prevents bone remodeling to ensure the replacement of defective bone with an equivalent volume of healthy bone [13].
DMab was previously related to the development of ONJ, during treatment for sacral giant cell tumor [14], metastatic bone disease [15], and prostatic adenocarcinoma [16, 17], the doses of DMab used in metastatic bone diseases being 12 times greater than in the management of OP.
A recent meta-analysis assessing a total of 8,963 patients of both genders, with a variety of solid tumors, from seven studies (i.e., the majority of these patients had either prostate or breast cancer) revealed an overall incidence of ONJ in cancer patients receiving DMab of 1.7 % (95 % Cl, 0.9–3.1 %). This study concluded that, in such patients, the use of DMab is associated with an increased risk of developing ONJ when compared with BP treatment or placebo, although the increased risk was not statistically significant between DMab and BP treatments [18].
In postmenopausal osteoporosis, two cases of ONJ were described in a cohort of 2,207 women treated with 60 mg subcutaneously. DMab every 6 months, for 2 years, after having received a placebo during the previous 3 years [19].
In conclusion, we describe for the first time the development of ONJ following tooth extraction, in a male patient, treated for idiopathic osteoporosis with DMab. Due to the constant increase in DMab prescription, for the management of osteoporosis, in both genders, physicians should be made aware of this potential risk.
Conflicts of interest
J.Y. Reginster has received consulting fees or paid advisory boards from Servier, Novartis, Negma, Lilly, Wyeth, Amgen, GlaxoSmithKline, Roche, Merckle, Nycomed, NPS, and Theramex; lecture fees when speaking at the invitation of a commercial sponsor from Merck Sharp and Dohme, Lilly, Rottapharm, IBSA, Genevrier, Novartis, Servier, Roche, GlaxoSmithKline, Teijin, Teva, Ebewee Pharma, Zodiac, Analis, Theramex, Nycomed, and Novo-Nordisk; and grant support from Bristol Myers Squibb, Merck Sharp & Dohme, Rottapharm, Teva, Eli Lilly, Novartis, Roche, GlaxoSmithKline, Amgen, and Servier.
A. Neuprez received travel grant from Amgen and Servier.
S. Coste received travel grant from Amgen and Servier.
E. Rompen has no conflict of interest.
J.M. Crielaard has no conflict of interest.
References
- 1.Kaufman JM, Reginster JY, Boonen S, Brandi ML, Cooper C, Dere W, Devogelaer JP, Diez-Perez A, Kanis JA, McCloskey E, Mitlak B, Orwoll E, Ringe JD, Weryha G, Rizzoli R. Treatment of osteoporosis in men. Bone. 2013;53:134–144. doi: 10.1016/j.bone.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaufman JM, Goemaere S. Osteoporosis in men. Best Pract Res Clin Endocrinol Metab. 2008;22:787–812. doi: 10.1016/j.beem.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Rizzoli R, Boonen S, Brandi ML, Bruyère O, Cooper C, Kanis JA, Kaufman JM, Ringe JD, Weryha G, Reginster JY. Vitamin D supplementation in elderly or postmenopausal women: a 2013 update of the 2008 recommendations of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) Curr Med Res Opin. 2013;29:305–313. doi: 10.1185/03007995.2013.766162. [DOI] [PubMed] [Google Scholar]
- 4.Cavalier E, Delanaye P, Moranne O. Variability of new bone mineral metabolism markers in patients treated with maintenance hemodialysis : implications for clinical decision making. Am J Kindey Dis. 2013;61:847–848. doi: 10.1053/j.ajkd.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 5.Johansson H, Kanis JA, McCloskey EV, Oden A, Devogelaer JP, Kaufman JM, Neuprez A, Hiligsmann M, Bruyère O, Reginster JY. A FRAX° model for the assessment of fracture probability in Belgium. Osteoporos Int. 2011;22:453–461. doi: 10.1007/s00198-010-1218-1. [DOI] [PubMed] [Google Scholar]
- 6.Neuprez A, Johansson H, Kanis JA, McCloskey EV, Oden A, Bruyère O, Hiligsmann M, Devogelaer JP, Kaufman JM, Reginster JY. A FRAX model for the assessment of fracture probability in Belgium. Rev Med Liège. 2009;64:612–619. [PubMed] [Google Scholar]
- 7.Bekker PJ, Holloway DL, Rasmussen AS, Murphy R, Martin SW, Leese PT, Holmes GB, Dunstan CR, DePaoli AM. A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. J Bone Miner Res. 2004;19:1059–1066. doi: 10.1359/JBMR.040305. [DOI] [PubMed] [Google Scholar]
- 8.Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23–57. doi: 10.1007/s00198-012-2074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orwoll E, Teglbjaerg CS, Langdahl BL, Chapurlat R, Czerwinski E, Kendler DL, Reginster JY, Kivitz A, Lewiecki EM, Miller PD, Bolognese MA, McClung MR, Bone HG, Ljunggren O, Abrahamsen B, Gruntmanis U, Yang YC, Wagman RB, Siddhanti S, Grauer A, Hall JW, Boonen S. A randomized, placebo-controlled study of the effects of denosumab for the treatment of men with low bone mineral density. J Clin Endocrinol Metab. 2012;97:3161–3169. doi: 10.1210/jc.2012-1569. [DOI] [PubMed] [Google Scholar]
- 10.Parthan A, Kruse MM, Agodoa I, Tao CY, Silverman SL, Orwoll E. Is denosumab cost-effective compared to oral bisphosphonates for the treatment of male osteoporosis (mop) in Sweden? Value Health. 2013;16:A223. doi: 10.1016/j.jval.2013.03.1130. [DOI] [Google Scholar]
- 11.Rizzoli R, Burlet N, Cahall D, Delmas PD, Eriksen EF, Felsenberg D, Grbic J, Jontell M, Landesberg R, Laslop A, Wollenhaupt M, Papapoulos S, Sezer O, Sprafka M, Reginster JY. Osteonecrosis of the jaw and bisphosphonate treatment for osteoporosis. Bone. 2008;42:841–847. doi: 10.1016/j.bone.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Ruggiera SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527–534. doi: 10.1016/j.joms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Subramanian G, Cohen HV, Quek SY. A model for the pathogenesis of bisphosphonate-associated osteonecrosis of the jaw and teriparatide’s potential role in its resolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:744–753. doi: 10.1016/j.tripleo.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 14.Aghaloo TL, Felsenfeld AL, Tetradis S. Osteonecrosis of the jaw in a patient on Denosumab. J Oral Maxillofac Surg. 2010;68:959–963. doi: 10.1016/j.joms.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raylor KH, Middlefell LS, Mizen KD. Osteonecrosis of the jaws induced by anti-RANK ligand therapy. Br J Oral Maxillofac Surg. 2010;48:221–223. doi: 10.1016/j.bjoms.2009.08.030. [DOI] [PubMed] [Google Scholar]
- 16.Diz P, Lopez-Cedrun JL, Arenaz J, Scully C. Denosumab-related osteonecrosis of the jaw. J Am Dent Assoc. 2012;143:981–984. doi: 10.14219/jada.archive.2012.0323. [DOI] [PubMed] [Google Scholar]
- 17.Pichardo SE, Kuypers SC, Van Merkesteyn JP. Denosumab osteonecrosis of the mandible: a new entity? A case report. J Craniomaxillofac Surg. 2013;41:e65–e69. doi: 10.1016/j.jcms.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 18.Qi WX, Tang LN, He AN, Yao Y (2013) Shen Z Risk of osteonecrosis of the jaw in cancer patients receiving denosumab: a meta-analysis of seven randomized controlled trials. Int J Clin Oncol (in press) [DOI] [PubMed]
- 19.Papapoulos S, Chapurlat R, Libanati C, Brandi ML, Brown JP, Czerwinski E, Krieg MA, Man Z, Mellström D, Radominski SC, Reginster JY, Resch H, Roman Ivorra JA, Roux C, Vittinghoff E, Austin M, Daizadeh N, Bradley MN, Grauer A, Cummings SR, Bone HG. Five years of denosumab exposure in women with postmenopausal osteoporosis: results from the first two years of the FREEDOM extension. J Bone Miner Res. 2012;27:694–701. doi: 10.1002/jbmr.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]