Abstract
Primary care physicians can help drug-dependent patients mitigate adverse drug use consequences; instruments validated in primary care to measure these consequences would aid in this effort. This study evaluated the validity of the Short Inventory of Problems—Alcohol and Drugs modified for Drug Use (SIP-DU) among subjects recruited from a primary care clinic (n = 106). SIP-DU internal consistency was evaluated using Cronbach’s alphas, convergent validity by correlating the total SIP-DU score with the DAST-10, and construct validity by analyzing the factor structure. The SIP-DU demonstrated high internal consistency (Cronbach’s alpha for overall scale .95, subscales .72–.90) comparable with other SIP versions and correlated well with the DAST-10 (r = .70). Confirmatory factor analysis suggested an unacceptable fit of previously proposed factors; exploratory factor analyses suggested a single factor of drug use consequences. The SIP-DU offers primary care clinicians a valid and practical assessment tool for drug use consequences.
INTRODUCTION
Primary care physicians are in a position to identify drug users years before they have medical complications or present for drug treatment. During the clinical encounter, primary care physicians can detect and then provide early intervention to help their patients become aware of and prevent adverse effects of drug use.1 The individual consequences of drug use and dependence can be severe and may include loss of self-worth; loss of employment; loss of spouse, friends, and family; incarceration; as well as the development or worsening of chronic medical and/or psychiatric disorders. Understanding drug use consequences is central to addressing drug use and can provide motivation to the patient to address the problem. Understanding the severity of problems can also help a clinician determine what, if any, intervention is required (eg, a brief intervention in primary care for patients with milder symptoms or more intensive treatment for the dependent patient). Drug use instruments validated in a primary care setting are important; most such instruments were developed in specialty care settings and may not be appropriate for use in primary care.
One instrument that has been adapted to measure the consequences of alcohol and drug use combined is the Short Inventory of Problems (SIP). Originally developed and validated to measure alcohol consequences, the SIP has been modified to assess individual consequences related to substance (alcohol and other drug) use disorders (SIP-SUD), alcohol and other drug use (SIP-AD), drugs alone (SIP-D), and even bipolar disorder (SIP-BD).2–4 None has been validated in primary care settings. The original SIP for alcohol is a 15-item instrument created by selecting representative items from the Drinker Inventory of Consequences (DrInC) to assess the self-attributed consequences of drinking in five domains (Physical, Intrapersonal, Social Responsibility, Interpersonal, and Impulse Control) using two time frames (lifetime and recent consequences).5 The Physical domain assesses acute and chronic physical states resulting from heavy drinking. The Intrapersonal domain asks about personal states of feeling associated with drinking such as guilt or shame. The Social Responsibility domain asks about consequences observable by others such as failing to do what was expected because of drinking. The Interpersonal domain assesses an individual’s damage to or loss of personal relationships, including concern about drinking from family and friends. Finally, the Impulse Control domain asks about impulsive actions, risk-taking, increased use of other substances, and legal problems.5,6
The Inventory of Drug Use Consequences (InDUC) represented a next step in meeting the need for a standardized measure of both alcohol and other drug use consequences. The InDUC was created by taking the identical items used in the DrInC but modifying the wording from “drinking” to “drinking or using drugs.” The InDUC is available in two versions: one that assesses lifetime consequences of substance use and another that assesses the frequency of recent problems (ie, past 3 months).5 Like the DrInC, the InDUC was subsequently shortened to 15 items (of which 12 items are the same as those used in the SIP for alcohol) to enhance its clinical utility and became known as the SIP for alcohol or drugs (SIP-AD).2
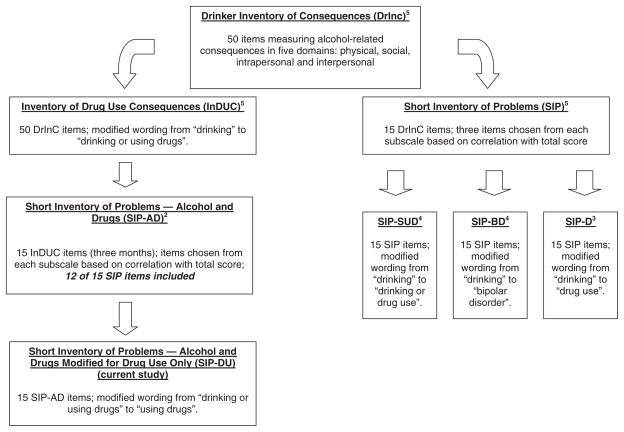
It is this version of the SIP that was modified for this study to focus on other drug problems, and we hypothesized that it would have similar properties of internal consistency and validity as its recently developed cousin instrument, the SIP for alcohol modified for other drugs (SIP-D).3 However, since the instrument used in this study is descended from a different branch of the SIP family tree than the SIP-D with three items that were not part of the SIP for alcohol, this instrument shall be referred to as the Short Inventory of Problems—Alcohol and Drugs modified for Drug Use (SIP-DU) to distinguish it from the SIP-D (Figure 1). Since no previous versions of the SIP have been validated exclusively in a primary care sample, the main objective of this study was to evaluate the validity of the SIP-DU in a sample of primary care patients.
FIGURE 1.
Derivation of the short inventories of problems. DrInC = Drinker Inventory of Consequences; InDUC = Inventory of Drug Use Consequences; SIP = Short Inventory of Problems; SIP-AD = Short Inventory of Problems—Alcohol and Drugs; SIP-SUD = Short Inventory of Problems—Substance Use Disorder; SIP-BD = Short Inventory of Problems—Bipolar Disorder; SIP-D = Short Inventory of Problems—Drugs; SIP-DU = Short Inventory of Problems—Drug Use.
MATERIALS AND METHODS
Participants
The study was conducted between October 2006 and June 2007 in the waiting room of a primary care clinic at an urban safety net hospital. To help minimize biased selection, subjects were systematically approached daily by one research associate according to a predetermined pattern based on waiting room seating, which was varied each day. Patients who were under the age of 18 were excluded, as were those who, in the judgment of the research associate, would be unable to complete the questionnaire because of limited English, cognitive impairment, or acute illness. People in the waiting room accompanying patients but who reported not themselves being patients of the clinic were also excluded. Eligible subjects were interviewed either before or after their primary care visit, or were scheduled to return at a later time for a research interview conducted in a private setting. All data were recorded anonymously without any unique identifiers.
Assessments
Subjects were first asked the single screening question validated in primary care to detect drug use, “How many times in the past year have you used an illegal drug or used a prescription medication for non-medical reasons?”7 A cross-sectional assessment of alcohol and drug use was then conducted including the Drug Abuse Screening Test (DAST-10), a computerized version of the Composite International Diagnostic Interview (CIDI) Substance Abuse Module and the SIP-DU.8,9 The questions included in the DAST-10 ask about possible involvement during the past 12 months with drugs by drug class, not including alcohol (eg, the use of prescribed or over-the-counter drugs in excess of the directions, any nonmedical use of drugs). As part of the CIDI, subjects were asked about past year use of illicit drugs (marijuana, cocaine, heroin, stimulants, or hallucinogens) and about past year non-medical use of prescription drugs. The SIP-DU asked questions about lifetime consequences of drug use (1 = Ever/0 = Never); subscale scores and the total score were then calculated by summing the item responses. All interviews were conducted by trained research staff (author PS trained the research associate by role play and by using the CIDI materials) in a private setting and data were recorded anonymously. All study procedures were reviewed and approved by the Institutional Review Board of Boston University Medical Center. Informed consent was given by all subjects before participating in the research.
Data Analysis
All analyses were conducted using SAS version 9.1 (SAS Inc., Cary, NC, USA). Scores were calculated for the total SIP-DU and each of the five subscales using the questions that asked about drug use consequences over the past 3 months. Cronbach’s alpha (α) was used to assess internal consistency, or how closely related the set of questions are, and to evaluate how well the SIP-DU subscales measured distinct underlying constructs of drug use consequences. Internal consistency estimates were compared with published results from other SIP instruments.4,5,10,11 The non-parametric Spearman’s rho (ρ) was used to assess correlation of the SIP-DU with the DAST-10, a measure of drug involvement that is conceptually related (convergent validity). To evaluate whether the SIP-DU questions correspond to the previously proposed five concepts of Physical, Social, Interpersonal, Intrapersonal, and Impulse control consequences (construct validity) a confirmatory factor analysis was performed. The following criteria were used to assess whether the model fit of the confirmatory factor analysis was acceptable: chi-square test (p-value .05); root mean square error of approximation (RMSEA) <.05; goodness of fit index (GFI) >.95; adjusted goodness of fit index (AGFI) >.90. If the analyses suggested an unacceptable model fit, an exploratory factor analysis was planned to further evaluate the possible underlying constructs of the SIP-DU. For the exploratory factor analysis, the number of factors to retain was determined based on the scree plot and the interpretability of the resulting factors. The exploratory factor analysis was performed using oblique rotation to allow for possible correlation among factors.
RESULTS
Sample Characteristics
Of 1,781 patients approached for screening 903 agreed to be screened and 394 were eligible for the study. Of the 394 eligible subjects, 303 arrived for the research interview and consented to participate in the study; 286 subjects completed the research interview. The sample for this analysis was limited (n=106) to subjects who were identified as drug dependent based on their responses to the CIDI since they represent a relevant primary care population for assessment of drug use consequences (and the original SIP was derived from people with dependence). Study participants were predominantly male with a median age of 46 (range 22–74 years, Table 1). A majority was African American (58%), high school educated (73%), and reported English as their primary language (82%).
TABLE 1.
Sample characteristics (n = 106)
| Characteristic | |
|---|---|
| Female | 37 (35) |
| Age | |
| Mean ± SD | 46 ± 9 |
| Median (range) | 46 (22–74) |
| Education | |
| Some high school | 35 (33) |
| High school graduate | 41 (39) |
| Some college | 25 (24) |
| College graduate or postgraduate education | 5 (5) |
| Race | |
| American Indian/Alaskan Native | 3 (3) |
| Black or African American | 62 (59) |
| White | 20 (19) |
| Unknown | 21 (20) |
| Hispanic or Latino ethnicity | 25 (24) |
| English is first language | 87 (82) |
| Drug use in past year | |
| Marijuana or hashish | 54 (51) |
| Cocaine | 57 (54) |
| Prescription drugs without a prescription | 32 (30) |
Values are represented as n (%) except where otherwise noted; SD = standard deviation.
Scale Internal Consistency and Convergent Validity
Table 2 presents the scale internal consistency of the SIP-DU and, for comparison, those from the previously published DrInC and previous versions of the SIP, the SIP for alcohol use consequences, and the SIP for substance use disorders (SIP-SUD). These previous studies assessed versions of the SIP in several different populations including outpatients diagnosed with substance use and bipolar disorder, problem drinkers recruited from the community, and Emergency Department patients presenting with alcohol-related injuries.4,5,10,11 Overall SIP-DU scale internal consistency was high (Cronbach’s α = .95) and the SIP-DU subscales had moderate-to-strong alphas (Physical = .71; Social = .89; Interpersonal = .85; Intrapersonal = .86; Impulse = .82). Overall and across all five domains the SIP-DU internal consistency appeared as good as that previously reported for the related SIP measures by other studies. The total SIP-DU score had moderate-to-strong correlation with a conceptually related instrument, the DAST-10 (Spearman’s ρ = .71), demonstrating convergent validity.
TABLE 2.
Internal consistency (Cronbach’s alpha) of the SIP-DU compared to other SIP instruments
| SIP scales | SIP-DU primary care (n = 106) | SIP-SUD (n = 57) | SIP community residents (n = 153) | SIP emergency department (n = 404) | DrInC (n = 1,389) |
|---|---|---|---|---|---|
| Total | .95 | .93 | .79 | .95 | .89 |
| Physical | .72 | .73 | .64 | .79 | .67 |
| Social | .90 | .74 | .62 | .85 | .76 |
| Interpersonal | .85 | .88 | .61 | .86 | .76 |
| Intrapersonal | .87 | .76 | .58 | .89 | .77 |
| Impulse | .82 | .62 | .56 | .73 | .61 |
Construct Validity
Confirmatory factor analysis revealed that the five-factor structure did not provide an acceptable fit to the data based on each of the four fit indexes (chi-square p < .0001; RMSEA = .17; GFI = .74; AGFI = .58). An exploratory factor analysis was therefore conducted to further evaluate the possible underlying constructs of the SIP-DU. The scree plot suggested two underlying factors. In evaluating the two-factor model, each factor had multiple items with strong loadings and there was only one item that loaded on more than one factor. However, these factors were unable to be interpreted as distinct concepts of drug use consequences and did not correspond with the hypothesized subscales (Table 3). A three-factor model was then considered; however, this model demonstrated poor loadings on the third factor (data not shown). A single-factor model was then fit; all items demonstrated acceptable loadings (.598–.855) and the single-factor model explained 82% of the variance. Cronbach’s alpha was .95 for the single-factor model suggesting a high degree of internal consistency. These results suggested a single-factor model provided the best fit to the data.
TABLE 3.
Exploratory factor analysis of the SIP-DU (n = 106)
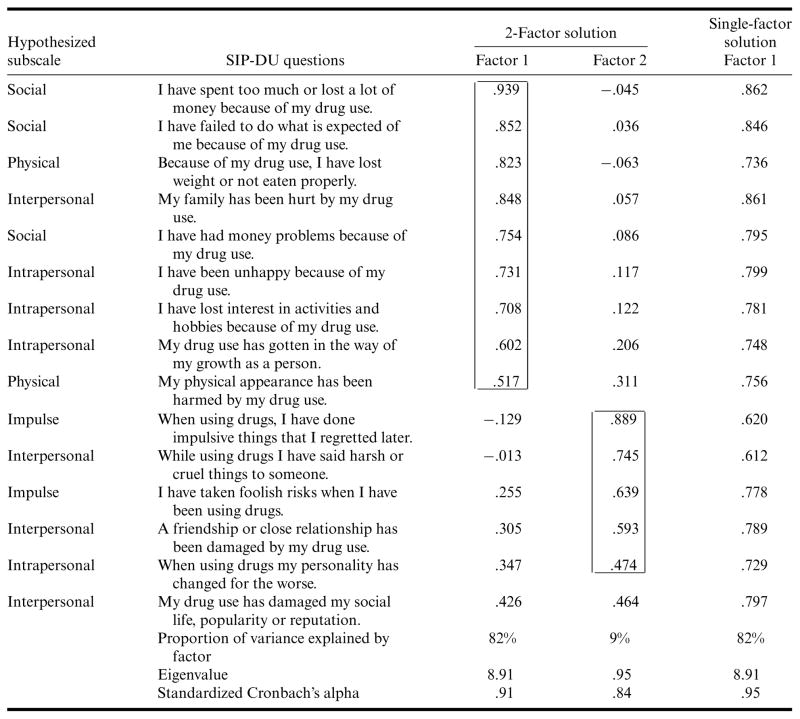
|
SIP-DU = Short Inventory of Problems—Drug Use. Values in boxes indicate which items distinctly loaded onto either Factor 1 or Factor 2.
DISCUSSION
Recent initiatives to promote screening and brief intervention have resulted in improved screening tools for drug use and dependence in a variety of patient populations. 7,12,13 However, it is also important to assess the consequences of drug use once it is identified. Certainly reducing the negative physical, social, and personal consequences of drug use is an important quality of life issue for drug users,14,15 and the involvement of primary care physicians in helping the patient find ways to reduce these consequences has the potential to improve both quality of care and outcomes. In fact, evidence suggests that higher quality primary care has the potential to reduce the odds of substance use.16 The purpose of this study was to validate a version of the SIP that can be used in the primary care setting for drug use consequences. The SIP-DU and a single screening question about drug use provide time-efficient tools for primary care teams in identifying and caring for drug-using patients.7
Previous research has shown that the SIP and its variants (eg, the SIP-AD) are valuable measurement tools that can reliably assess negative consequences in patients with alcohol or drug use disorders.2 Although one instrument that summarizes consequences of both alcohol and drug use can be useful as a global measure, tools that are more specific are needed for individual clinical care. Previous versions of the SIP have assessed consequences due to alcohol or drug use without distinguishing whether consequences were due to one or the other. This level of specificity is important when having a discussion with a patient about substance use consequences and when monitoring clinical progress of treatment outcomes in primary care. Having the ability to attribute consequences to alcohol and drugs separately may help clinicians and patients considering treatment options to prioritize and individualize interventions to mitigate the negative consequences experienced by the patient. The results of this study suggest that the SIP-DU retains strong internal consistency when administered in primary care and that this is comparable to those reported in earlier studies.
The observed correlation of the SIP-DU with the DAST-10 is sufficiently high to suggest that the SIP-DU is measuring an independent construct of drug use consequences. This further highlights the potential usefulness of the SIP-DU in primary care settings with drug-using patients. This study also provides additional evidence that the original SIP can be successfully modified to separately assess consequences of drug use and alcohol use.
The unacceptable fit of the originally proposed five-factor structure for the SIP-DU is consistent with findings reported by Gillespie et al.17 When they conducted confirmatory factor analysis with their data, they discovered that the loadings of the SIP-AD items were not consistent with a five-factor structure and concluded that a single-factor structure was most appropriate. The exploratory factor analysis findings of this study are consistent with those results.
This primary care sample was recruited from a single urban medical center, which may limit the generalizability of the findings. The patients at this medical center tend to be more socioeconomically disadvantaged, more racially and ethnically diverse, and may have more severe drug use or dependence than that seen at other hospitals that are not in urban underserved settings. Generalizability may also be limited to English-speaking patients willing to participate in a research study.
Since this was designed as a cross-sectional study, neither test-retest reliability nor the responsiveness of the SIP-DU to change over time could be evaluated. In addition, the sample size for this study was small and may not have been adequate to determine the true SIP-DU factor structure. Finally, unlike the full versions of the DrInC and InDUC, neither the original SIP for alcohol nor the SIP-DU contains a control subscale to detect careless responding.
As part of a growing interest in developing substance use measures relevant to primary care, the present study evaluated the validity of the SIP-DU in a primary care sample. As was recently found with the SIP-DU’s cousin instrument, the SIP-D,3 this analysis provides evidence of the SIP-DU’s validity in measuring drug use consequences in a primary care setting. Consistent with previous research, a five-factor structure for the SIP-DU could not be confirmed by this study. Instead, the results suggested a possible single-factor structure for the SIP-DU. Future research might include additional psychometric analysis of the SIP-DU in other clinical settings and other geographical regions with larger sample sizes, and might also test use of the SIP-DU for identifying consequences of drug use among patients without dependence. Nevertheless, the SIP-DU offers clinicians a practical assessment tool for drug use consequences in a primary care setting.
Acknowledgments
Data collection and data analysis were supported by grant DA010019 from the National Institute on Drug Abuse, Bethesda, MD (Dr. Samet) and by grant AA010870 from the National Institute on Alcohol Abuse and Alcoholism, Rockville, MD (Dr. Saitz). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, or the National Institutes of Health.
We thank Dr. Sue Eisen for her review and commentary on the initial draft of this manuscript.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.Haverkos HW, Stein MD. Identifying substance abuse in primary care. Am Fam Physician. 1995;52:2029–2035. [PubMed] [Google Scholar]
- 2.Blanchard KA, Morgenstern J, Morgan TJ, et al. Assessing consequences of substance use: Psychometric properties of the Inventory of Drug Use Consequences. Psychol Addict Behav. 2003;17:328–331. doi: 10.1037/0893-164X.17.4.328. [DOI] [PubMed] [Google Scholar]
- 3.Alterman AI, Cacciola JS, Ivey MA, et al. Reliability and validity of the alcohol short index of problems and a newly constructed drug short index of problems. J Stud Alcohol Drugs. 2009;70:304–307. doi: 10.15288/jsad.2009.70.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bender RE, Griffin ML, Gallop RJ, et al. Assessing negative consequences in patients with substance use and bipolar disorders: Psychometric properties of the short inventory of problems (SIP) Am J Addict. 2007;16:503–509. doi: 10.1080/10550490701641058. [DOI] [PubMed] [Google Scholar]
- 5.Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of Alcohol Abuse. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 6.Forcehimes AA, Tonigan JS, Miller WR, et al. Psychometrics of the Drinker Inventory of Consequences (DrInC) Addict Behav. 2007;32:1699–1704. doi: 10.1016/j.addbeh.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Smith PC, Schmidt SM, Allensworth-Davies D, et al. A single-question screening test for drug use in primary care. Arch Internal Med. 2010;170:1155–1160. doi: 10.1001/archinternmed.2010.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. J Subst Abuse Treat. 2007;32:189–198. doi: 10.1016/j.jsat.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC, Abelson J, Demler O, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) Int J Methods Psychiatr Res. 2004;13:122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feinn R, Tennen H, Kranzler HR. Psychometric properties of the short index of problems as a measure of recent alcohol-related problems. Alcohol Clin Exp Res. 2003;27:1436–1441. doi: 10.1097/01.ALC.0000087582.44674.AF. [DOI] [PubMed] [Google Scholar]
- 11.Kenna GA, Longabaugh R, Gogineni A, et al. Can the short index of problems (SIP) be improved? Validity and reliability of the three-month SIP in an emergency department sample. J Stud Alcohol. 2005;66:433–437. doi: 10.15288/jsa.2005.66.433. [DOI] [PubMed] [Google Scholar]
- 12.Amaro H, Reed E, Rowe E, et al. Brief screening and intervention for alcohol and drug use in a college student health clinic: Feasibility, implementation, and outcomes. J Am Coll Health. 2010;58:357–364. doi: 10.1080/07448480903501764. [DOI] [PubMed] [Google Scholar]
- 13.D’Onofrio G, Degutis LC. Integrating project ASSERT: A screening, intervention, and referral to treatment program for unhealthy alcohol and drug use into an urban emergency department. Acad Emerg Med. 2010;17:903–911. doi: 10.1111/j.1553-2712.2010.00824.x. [DOI] [PubMed] [Google Scholar]
- 14.De Maeyer J, Vanderplasschen W, Broekaert E. Quality of life among opiate-dependent individuals: A review of the literature. Int J Drug Policy. 2010;21:364–380. doi: 10.1016/j.drugpo.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Stein MD, Mulvey KP, Plough A, et al. The functioning and well being of persons who seek treatment for drug and alcohol use. J Subst Abuse. 1998;10:75–84. doi: 10.1016/s0899-3289(99)80142-4. [DOI] [PubMed] [Google Scholar]
- 16.Kim TW, Samet JH, Cheng DM, et al. Primary care quality and addiction severity: A prospective cohort study. Health Serv Res. 2007;42:755–772. doi: 10.1111/j.1475-6773.2006.00630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gillespie W, Holt JL, Blackwell RL. Measuring outcomes of alcohol, marijuana, and cocaine use among college students: A preliminary test of the Shortened Inventory of Problems—Alcohol and Drugs (SIP-AD) J Drug Issues. 2007;37:549–568. [Google Scholar]