Abstract
To assess effects of a short-term strength training (ST) program on muscle quality (MQ) and functional capacity, 36 sedentary elderly women (age = 66.0 ± 8 year, height = 159.1 ± 9.2 cm, body mass = 68.3 ± 12.1 kg, body fat = 37.0 ± 4.2 %) were randomly divided into an experimental group (EG; n = 19) or a control group (CG; n = 17). The EG performed two to three sets of 12–15 repeats of leg press, knee extension, and knee flexion exercises, 2 days/week for 6 weeks. Before and after training, lower body one repetition maximum (1RM), functional performance tests, quadriceps femoris muscle thickness (MT), and muscle quality (MQ) (1RM and quadriceps MT quotient) were assessed. After training, only the EG showed significant improvements in 1RM (p < 0.05), 30-s sit-to-stand (p < 0.001), and 8 foot up-and-go (p < 0.001). In addition, only in the EG, significant increases in all quadriceps femoris MT measurements (vastus lateralis, vastus medialis, vastus intermedius, and rectus femoris) (p ≤ 0.05), and MQ (p < 0.001) were demonstrated. No changes were observed in the CG. Furthermore, there were significant associations between individual changes in MQ and corresponding changes in 30-s sit-to-stand (r = 0.62, p < 0.001), and 8 foot up-and-go (r = −0.71, p < 0.001). In conclusion, a ST program of only 6 weeks was sufficient to enhance MQ of the knee extensors in elderly women, which resulted in beneficial changes in functional capacity.
Keywords: Early-phase adaptations, Ultrasonography, Muscle hypertrophy, Functional performance, Aging
Introduction
The aging process is associated with a progressive loss of muscle mass (i.e., sarcopenia) with a corresponding decline in strength and power (i.e., dynapenia) (Doherty 2003; Clark and Manini 2008, 2012; Manini and Clark 2012; Morley 2012). However, it seems that the decrease in muscle strength and power in the elderly occurs to a greater extent than the concomitant loss of muscle mass (Delmonico et al. 2009), and muscle strength may have greater clinical importance in weak older adults than muscle mass per se (Kim et al. 2012). These impairments are the consequence of changes in neural and morphological parameters. Neural mechanisms include reduced maximal agonist activation, increased antagonistic coactivation (Klass et al. 2007), neuronal loss, and muscle denervation. Morphological mechanisms include decrease in type II fiber diameter and decreased fascicle length (Aagaard et al. 2010). These physiological changes promote drastic impairments in muscle quality (MQ) and in functional capacity in elderly persons (Frontera et al. 2008; Kallman et al. 1990).
Muscle quality (MQ) refers to the force produced per unit of active muscle mass (Ivey et al. 2000; Reeves et al. 2004; Cadore et al. 2012; Correa et al. 2012b). In addition, MQ provides an estimation of the contribution of neuromuscular factors associated with changes in strength development, since an improvement in strength with no change in muscle mass suggests neural adaptations to training (Korhonen et al. 2009). Moreover, MQ is associated with decreased functional capacity in older individuals and is possibly associated with reductions in neuromuscular function in this population (Carmeli et al. 2000). Interestingly, Macaluso et al. (2002) observed greater reductions in MQ in older compared to young women, suggesting a potential age-related neural impairment to explain the decreased MQ. Additionally, Delmonico et al. (2009), examining well-functioning women over 5 years, reported loss of knee extension strength two to five times greater than quadricep muscle mass loss, which suggests a decrease in MQ (11 %). Thus, the evaluation of MQ seems to be a suitable method to monitor neuromuscular function of the elderly, particularly in response to strength training.
Strength training (ST) is a potential intervention to counteract age-related sarcopenia and dynapenia (Doherty 2003; Hunter et al. 2004; Malafarina et al. 2012; Mitchell et al. 2012). In elderly women, studies ranging from 10 to 12 weeks, with two to three sessions per week, have resulted in significant strength gains (Bottaro et al. 2007; Correa et al. 2012a, 2012b). These strength improvements are the consequence of neural adaptations such as increases in maximal motor unit recruitment (Knight and Kamen 2001) and enhanced maximal motor unit firing rate (Kamen and Knight 2004) as well as increased muscle mass and thickness (Nogueira et al. 2009; Ahtiainen et al. 2010). However, in elderly women, the rate of hypertrophy induced by ST has been less (approximately 5–10 %) than the rate of increase in strength (approximately 35–50 %), as a result of neural adaptations, which supports the role of neural adaptations and its influence on MQ.
A positive relationship between power, strength, and functional performance in the elderly has been demonstrated by Pereira et al. (2012). In addition, muscle strength is a better predictor of physical performance than muscle mass (Latham et al. 2004; Kim et al. 2012). Thus, because ST can result in enhanced strength and, consequently, enhanced MQ, these improvements may affect functional outcomes, such as gait speed and chair-stand ability (Hunter et al. 1995; Granacher et al. 2009, 2012; Correa et al. 2012b). Despite numerous studies on the neuromuscular and functional adaptations induced by ST in the elderly, the effects of this type of exercise intervention on MQ and its association with functional performance in older individuals need to be investigated more, especially in women who may be at greater risk of loss of power, strength, and muscle mass (Caserotti et al. 2001). Moreover, to the best of the authors' knowledge, the effects of ST on muscle quality during early phases of training (i.e., less than 8 weeks) are poorly investigated. Therefore, the purpose of the study was to investigate changes in the knee extensor MQ induced by short-term strength training in elderly women. Furthermore, a second purpose was to investigate the association between MQ and functional capacity adaptations to ST. Our hypothesis is that 6 weeks of strength training would result in marked muscle thickness and muscle quality gains, and these adaptations would be associated with functional capacity gains.
Methods
Subjects
The volunteer sample comprised of 36 sedentary elderly women (age = 66.0 ± 8 years, height = 159.1 ± 9.2 cm, body mass = 68.3 ± 12.1 kg, body fat = 37.0 ± 4.2 %), who had not engaged in regular and systematic ST or aerobic training for at least 1 year prior to the study. Individuals with a history of severe endocrine, metabolic, and neuromuscular diseases were excluded. Individuals were selected by advertising in a large circulation daily newspaper. Subsequently, participants were randomly divided into two groups as follow: (1) the experimental group (EG; n = 19) or (2) the control group (CG; n = 17) by a blinded investigator. Each individual was informed about the methodological procedures of this study by reading an informed consent document, which was approved by the Institutional Ethics and Research Committee (Protocol No. 19322), with the ethical standards laid down in the 1964 Declaration of Helsinki. Body mass and height were measured using as ASImed (MG, Brazil) analog scale (resolution of 0.1 kg) and stadiometer (resolution of 1 mm), respectively. Body composition was assessed using a skinfold technique. A seven-site skinfold equation was used to estimate body density (Jackson and Pollock 1978), and body fat was, subsequently, calculated using the Siri equation (Siri 1993). The same technician obtained all anthropometric measurements on the right side of the body.
Experimental design
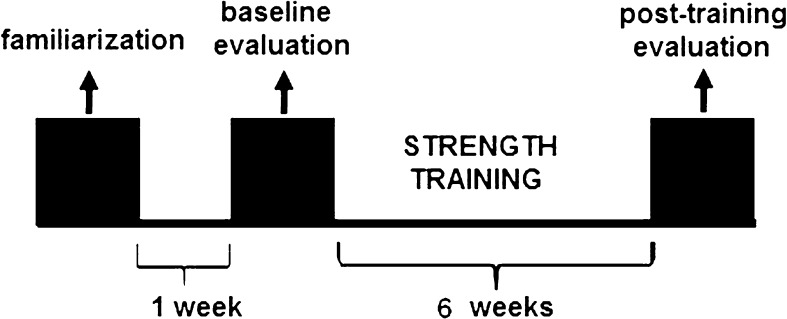
In order to investigate the effects of short-term ST on muscle quality and functional capacity in elderly women, maximal strength (one repetition maximum—1RM), muscle thickness (MT), and functional tests were performed pre and post 6 weeks of training (Fig. 1). Participants attended the laboratory on four different occasions before and after the training intervention because all tests were performed on separate days. On the first visit, each individual was informed about the methodological procedures of the study and signed the informed consent document. On the second visit, height, weight, body composition, and muscle thickness were assessed. On the third visit, maximal dynamic strength was assessed. Finally, in the fourth visit, subjects performed the functional tests. Testing at pre- and postintervention was conducted on the same equipment with identical subject/equipment positioning and at the same time of day and was overseen by the same investigator, who was blinded to the training group of the subjects. The ambient conditions were kept constant during all tests (temperature: 22–24 °C).
Fig. 1.
Experimental design
Strength training program
The ST program was performed twice a week for 6 weeks, with 48 h rest between training sessions and with linear and progressive intensity and volume. The intensity of training was controlled by repetition maximum (RM) (i.e., sets performed until concentric failure). The experimental group (EG) performed leg press, knee extension, and knee flexion exercises. During weeks 1–3, they performed two sets of 15–20 RM, and during weeks 4–6, they performed three sets of 12–15 RM, with 2-min rest interval between sets and exercises. All participants performed 12 ST sessions. One week prior to testing, all subjects were familiarized with the ST exercises and assessments on two different occasions.
Maximum dynamic strength (1RM)
Maximal knee extension strength was assessed in the dominant leg using the one-repetition maximum test (1RM) on a knee extension machine (World Sculptor, RS, Brazil). On the test day, the subjects warmed up for 5 min on a cycle ergometer, stretched all major muscle groups, and performed specific movements for the exercise test. Each subject's maximal load was determined with no more than five attempts with 4-min rest between attempts. The cadence during 1RM tests was controlled by an electronic metronome (Quartz, Torrance, CA, USA). Test–retest reliability (ICC) was 0.89 for this test.
Muscle Thickness
The knee extensors MT was measured though images obtained with a B-mode ultrasound device (Philips, MG, Brazil). Subjects lie supine with the dominant leg extended and relaxed for 10 min to restore the normal flow of body fluids. A 7.5-MHz linear array probe was positioned perpendicularly to the vastus lateralis (VL), vastus medialis (VM), vastus intermedius (VI), and rectus femoris (RF) muscles and a water-based gel was used to promote acoustic contact between the skin and the transducer. Measurement of the VL was taken at the midpoint between the greater trochanter and the lateral epicondyle of the femur (Kumagai et al. 2000), whereas the measurement for the VM was taken at 30 % of the distance from the lateral epicondyle of the femur to the greater trochanter; VI measurements were made at two thirds the distance from the greater trochanter of the femur to the lateral epicondyle and 3-cm lateral to the midline of the limb (Korhonen et al. 2009). The ultrasound muscular images were analyzed via ImageJ software (National Institute of Health, USA, version 1.37). The subcutaneous adipose tissue and bone tissue were identified, and the distance between them was defined as MT. All measurements were performed by the same experienced evaluator. Quadriceps femoris muscle thickness (QFMT) was considered as the sum of the four lower-body muscles MT (VL + VM + VI + RF). Test–retest reliability (ICC) was ≥0.97 for all measurements.
Muscle quality
MQ was expressed as force per unit of muscle mass and was calculated by dividing the 1RM knee extension value by the sum of the QFMT. Therefore, MQ was assessed according to the following equation:
 |
30-s sit to stand.
The test began with the participant seated in a chair (height: 43 cm) with the back straight and feet on a flat surface positioned about shoulder width apart, arms crossed at chest height, with hip and knee flexion of approximately 90°. At a verbal signal, the participant rose to a full upright position and then returned to the initial seated position. Subjects were encouraged to complete as many repetitions as possible within a 30-s period (Jones et al. 1999).
8 foot up and go
The test consisted of measuring the maximum time (in seconds) needed for the subject to rise from a seated position (same as the 30-s sit-to-stand test), walk forward 8 f and then return 8 f and resume a seated position as soon as possible. Subjects had three attempts with 4-min rest between attempts, and the fastest time was used for further analysis (Rikli and Jones 2013).
Statistical analyses
The SPSS statistical software package (version 17.0) was used to analyze all data. Normal distribution and homogeneity parameters were checked with Shapiro–Wilk and Levene test's, respectively. Results are reported as mean ± SD. The training-related effects were assessed using a two-way mixed factor analysis of variance (ANOVA) [group (experimental or control) × time (pre- and posttest)]. Sample size was calculated using G*Power software (version 3.0.1) and determined that a sample size of n = 13 subjects would provide a statistical power greater than 0.85 for all variables. Pearson's product moment correlation coefficient (r) was used to assess the relationship between MQ and functional tests. Significance was accepted when p < 0.05.
Results
Before the ST intervention, there were no significant differences between groups in any variables assessed. Following 6 weeks of ST, only the EG showed a significant increase in 1RM values (p < 0.05). In addition, all quadriceps femoris MT measurements (VL, VM, RF, and VI) increased significantly in the EG (p < 0.05), whereas no changes were observed in the CG (Table 1). Likewise, muscle quality (MQ) increased significantly (p < 0.001) in the EG but not in the CG (Table 1).
Table 1.
Values before and after the 6-week period of strength training and relative increments (∆%), expressed as means ± SD
| Variables | Experimental group, n = 19 | Control group, n = 17 | ||||
|---|---|---|---|---|---|---|
| Pre | Post | ∆% | Pre | Post | ∆% | |
| 1RM − knee extension (kg) | 42.5 ± 8.1 | 51.9 ± 9.9* | 23.5 ± 10.3 | 39.1 ± 8.3 | 38.8 ± 9.0 | −0.8 ± 14.0 |
| MT − VL (mm) | 16.1 ± 2.3 | 17.9 ± 2.1** | 10.5 ± 1.1 | 16.7 ± 2.9 | 16.1 ± 3.1 | −2.2 ± 2.1 |
| MT − VM (mm) | 14.0 ± 3.3 | 16.9 ± 2.2*** | 18.1 ± 1.7 | 14.4 ± 3.6 | 14.9 ± 3.4 | 3.0 ± 1.1 |
| MT − RF (mm) | 16.1 ± 2.9 | 18.7 ± 3.1** | 8.7 ± 2.6 | 16.8 ± 2.1 | 16.0 ± 2.0 | 2.2 ± 1.6 |
| MT − VI (mm) | 13.1 ± 4.1 | 15.5 ± 2.7*** | 13.2 ± 2.1 | 13.2 ± 3.8 | 14.1 ± 2.5 | 0.7 ± 1.4 |
| Muscle quality (kg/mm) | 0.6 ± 2.1 | 0.8 ± 1.9*** | 14.8 ± 10.2 | 0.6 ± 1.2 | 0.6 ± 2.2 | −0.3 ± 14.1 |
| 30-s chair-stand test (no.) | 14.1 ± 1.5 | 17.5 ± 1.8*** | 23.8 ± 10.5 | 15.7 ± 2.0 | 15.3 ± 2.0 | 0.1 ± 0.2 |
| 8 foot up-and-go test (s) | 4.9 ± 0.5 | 3.83 ± 0.35*** | −22.4 ± 8.7 | 4.64 ± 0.46 | 4.74 ± 0.59 | −0.1 ± 5.4 |
1RM one maximum repetition, MT muscle thickness, VL vastus lateralis, VM vastus medialis, RF rectus femoris, VI vastus intermedius
*Significant difference from pretraining values and from control group (p < 0.05)
**Significant difference from pretraining values and from control group (p < 0.01)
***Significant difference from pretraining values and from control group (p < 0.001)
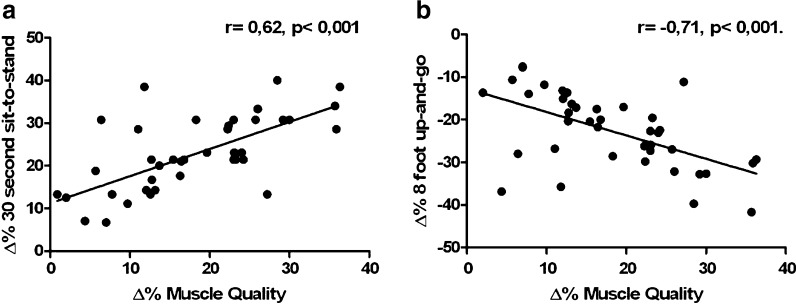
After training, the EG demonstrated significant changes in functional performance. The number of repetitions performed in the 30-s sit-to-stand test increased significantly as well as a significant reduction in time during the 8 foot up-and-go (p < 0.001). There were no significant changes in the functional tests in the CG (Table 1). There were significant positive associations between individual changes (∆%) observed in MQ with corresponding changes (∆%) in the 30-s sit-to-stand test (r = 0.62, p < 0.001) (Fig. 2a) and the 8 foot up-and-go test (r = −0.71, p < 0.001) (Fig. 2b).
Fig. 2.
Correlation between the increases (∆% muscle quality, 30-s chair-stand test and 8 foot up and go) observed during the training period. a ∆% muscle quality and ∆% 30-s chair-stand test. b ∆% muscle quality and ∆% 8 foot up and go
Discussion
The main finding of this study was a significant increase (~15 %) in MQ after only 6 weeks of strength training (ST) in older women. Likewise, it was observed that the increases in MQ (∆%) were positively correlated (r = 0.62, p < 0.001) with the 30-s sit-to-stand functional test and inversely correlated (r = −0.71, p < 0.001) with the 8 foot up-and-go test. Thus, the neuromuscular and morphological changes resulting from a short 6-week ST program represent significant improvements in functional tasks which older women perform daily.
Strength training programs have been shown to increase muscle strength and functional abilities in older women (Abe et al. 2000; Reeves et al. 2004; Correa et al. 2012a), whereas the ST adaptations during early phases of training (i.e., less than 8 weeks) is poorly investigated in this population. In one of the few studies in this perspective, Tracy et al. (1999) observed 30 % increments in 1RM knee extension after 9 weeks of ST. In the present study, the EG increased their 1RM knee extension by 23.5 % after only 6 weeks of ST (Table 1), which highlights the rapid initial force increments that occur in response to ST. The mechanisms that explain these changes are related to increased recruitment of motor units, firing rate, and inter- and intramuscular coordination (Frontera et al. 2000; Caserotti et al. 2008a; Granacher et al. 2009; Cadore et al. 2013).
Although neural adaptations explain initial increases in muscle strength observed with ST (Häkkinen et al. 1998; Lynch et al. 1999), morphological adaptations (i.e., muscle hypertrophy) also influence these changes to some degree. In our present study, MT increases observed in the whole quadriceps muscle group (VL, VM, VI, and RF) demonstrated these adaptations. Although changes in MT were less (8.7 to 18.1 %) than knee extension 1RM increases (23.5 %), these results suggest that structural changes in muscle also occur in the early phases of ST. In study of Able et al. (2000), morphological adaptations to ST were assessed using CT scans, and these authors did not demonstrate increases in the muscle mass in the initial periods of ST, probably because CT scans can only be used once every 6 months (Abe et al. 2000). In our study, morphological adaptations were measured by ultrasound, which can be performed more often and, thus, made it possible for us to observe muscle mass increases during the initial period of ST.
Decreases in MQ with the aging process have been described in previous studies (Metter et al. 1999; Misic et al. 2007; Frontera et al. 2008; Delmonico et al. 2009). Among the factors that may explain this phenomenon are the decline in the proportion of type II fibres, an increase in intramuscular connective tissue, an infiltration of adipose tissue, and changes in muscle metabolism. Because the reduction in the strength is more pronounced than the reduction in the muscle mass, muscle strength loss seems to affect MQ more than loss in muscle mass (Delmonico et al. 2009; Kim et al. 2012). Our results suggest that strength training is a quick and effective strategy to control the reduction in MQ of older women. Indeed, we found an increase of 14.8 % in MQ of the knee extensors in just 6 weeks of ST (Table 1), corroborating the 14 % reported by Tracy et al. (1999), in which women performed ST for 9 weeks.
The accelerated and progressive loss of muscle mass and strength, which results in reduced MQ, appears to be directly related to a decrease in functional capabilities and physical independence in the elderly population. However, muscle strength is a better predictor of physical performance than muscle mass (Latham et al. 2004; Kim et al. 2012). Thus, as ST can result in significant improvements in muscle strength, and consequently, in MQ, it may improve various functional aspects, such as gait speed and chair-stand ability (Hunter et al. 1995; Granacher et al. 2012; Correa et al. 2012b). It has been shown that the strength training may improve the strength and functional capacity even in oldest old (i.e., 90–97 years old) (Serra-Rexach et al. 2011). In the present study, although the subjects were 66 ± 8 years, the decline observed in the strength, muscle mass, and functional capacity during aging starts to be more accentuated after sixth decade of life. Thus, we believe that the enhancements in the strength and muscle quality observed in the present study are relevant and positively influenced the functional capacity parameters, such as the gait speed and chair-stand ability.
Functional status of the elderly has been evaluated using assessments such as the 30-s sit-to-stand and the 8 foot up-and-go tests (Bottaro et al. 2007; Rikli and Jones 2013), and the performance on these tests seems to be dependent on the capacity of the lower limbs muscles. Indeed, the increases in MQ observed in this study (~14.8 %) were associated to the increases in the performance of the 30-s sit-to-stand and the 8 foot up-and-go functional tests (24 and −22 %, respectively), which appear to have arisen from changes in the knee extensors muscle thickness (8.7–18.1 %) and increases in the 1RM (23.5 %). Therefore, these associations reinforce that ST can be a useful strategy to combat neural and morphological reductions associated with aging and, consequently, improve functional performance in elderly women.
In summary, a short-duration (6 weeks) strength training program was effective in increasing muscle quality (MQ) of the knee extensors in elderly women. Furthermore, this increase in MQ resulted in beneficial increases in functional capacity. These results are important, since lower body muscle strength is essential in executing activities of daily living in an elderly population.
References
- Aagaard P, Suetta C, Caserotti P, Magnusson SP, Kjaer M. Role of the nervous system in sarcopenia and muscle atrophy with aging: strength training as a countermeasure. Scand J Med Sci Sports. 2010;20:49–64. doi: 10.1111/j.1600-0838.2009.01084.x. [DOI] [PubMed] [Google Scholar]
- Abe T, DeHoyos DV, Pollock ML, Garzarella L. Time course for strength and muscle thickness changes following upper and lower body resistance training in men and women. Eur J Appl Physiol. 2000;81:174–180. doi: 10.1007/s004210050027. [DOI] [PubMed] [Google Scholar]
- Ahtiainen JP, Hoffren M, Hulmi JJ, Pietikäinen M, Mero AA, Avela J, Häkkinen K. Panoramic ultrasonography is a valid method to measure changes in skeletal muscle cross-sectional area. Eur J Appl Physiol. 2010;108:273–279. doi: 10.1007/s00421-009-1211-6. [DOI] [PubMed] [Google Scholar]
- Bottaro M, Machado SN, Nogueira W, Scales R, Veloso J. Effect of high versus low-velocity resistance training on muscular fitness and functional performance in older men. Eur J Appl Physiol. 2007;99:257–264. doi: 10.1007/s00421-006-0343-1. [DOI] [PubMed] [Google Scholar]
- Cadore EL, Izquierdo M, Alberton CL, Pinto RS, Conceição M, Cunha G, Radaelli R, Bottaro M, Trindade GT, Kruel LF. Strength prior to endurance intra-session exercise sequence optimizes neuromuscular and cardiovascular gains in elderly men. Exp Gerontol. 2012;47:164–169. doi: 10.1016/j.exger.2011.11.013. [DOI] [PubMed] [Google Scholar]
- Cadore EL, Izquierdo M, Pinto SS, Alberton CL, Pinto RS, Baroni BM, Vaz MA, Lanferdini FJ, Radaelli R, González-Izal M, Bottaro M, Kruel LF. Neuromuscular adaptations to concurrent training in the elderly: effects of intrasession exercise sequence. Age (Dordr) 2013;35:891–903. doi: 10.1007/s11357-012-9405-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmeli E, Reznick AZ, Coleman R, Carmeli V. Muscle strength and mass of lower extremities in relation to functional abilities in elderly adults. Gerontology. 2000;46:249–257. doi: 10.1159/000022168. [DOI] [PubMed] [Google Scholar]
- Caserotti P, Aagaard P, Simonsen EB, Puggaard L. Contraction-specific differences in maximal muscle power during stretch-shortening cycle movements in elderly males and females. Eur J Appl Physiol. 2001;84:206–212. doi: 10.1007/s004210170006. [DOI] [PubMed] [Google Scholar]
- Caserotti P, Aagaard P, Larsen JB, Puggaard L. Explosive heavy-resistance training in old and very old adults: changes in rapid muscle force, strength and power. Scand J Med Sci Sports. 2008;18:773–782. doi: 10.1111/j.1600-0838.2007.00732.x. [DOI] [PubMed] [Google Scholar]
- Clark BC, Manini TM. Sarcopenia=/=dynapenia. J Gerontol A Biol Sci Med Sci. 2008;63:829–834. doi: 10.1093/gerona/63.8.829. [DOI] [PubMed] [Google Scholar]
- Clark BC, Manini TM. What is dynapenia? Nutrition. 2012;28:495–503. doi: 10.1016/j.nut.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correa CS, Baroni BM, Radaelli R, Lanferdini FJ, Cunha GD, Reischak-Oliveira A, Vaz MA, Pinto RS (2012a) Effects of strength training and detraining on knee extensor strength, muscle volume and muscle quality in elderly women. Age (Dordr). [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- Correa CS, Laroche DP, Cadore EL, Reischak-Oliveira A, Bottaro M, Kruel LFM, Tartaruga MP, Radaelli R, Wilhelm EN, Lacerda FC, Gaya AR, Pinto RS. 3 types of strength training in older women. Int J Sports Med. 2012;33:962–969. doi: 10.1055/s-0032-1312648. [DOI] [PubMed] [Google Scholar]
- Delmonico MJ, Harris TB, Visser M, Park SW, Conroy MB, Velasquez-Mieyer P, Boudreau R, Manini TM, Nevitt M, Newman AB, Goodpaster BH. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90:1579–1585. doi: 10.3945/ajcn.2009.28047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty TJ. Invited review: aging and sarcopenia. J Appl Physiol. 2003;95:1717–1727. doi: 10.1152/japplphysiol.00347.2003. [DOI] [PubMed] [Google Scholar]
- Frontera WR, Reid KF, Phillips EM, Krivickas LS, Hughes VA, Roubenoff R, Fielding RA. Muscle fiber size and function in elderly humans: a longitudinal study. J Appl Physiol. 2008;105:637–642. doi: 10.1152/japplphysiol.90332.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera WR, Suh D, Krivickas LS, Hughes VA, Goldstein R, Roubenoff R. Skeletal muscle fiber quality in older men and women. Am J Physiol Cell Physiol. 2000;279:C611–C618. doi: 10.1152/ajpcell.2000.279.3.C611. [DOI] [PubMed] [Google Scholar]
- Granacher U, Gruber M, Gollhofer A. Resistance training and neuromuscular performance in seniors. Int J Sports Med. 2009;30:652–657. doi: 10.1055/s-0029-1224178. [DOI] [PubMed] [Google Scholar]
- Granacher U, Gruber M, Gollhofer A. Force production capacity and functional reflex activity in young and elderly men. Aging Clin Exp Res. 2012;22:374–382. doi: 10.1007/BF03337733. [DOI] [PubMed] [Google Scholar]
- Hakkinen K, Newton RU, Gordon SE, McCormick M, Volek JS, Nindl BC, Gotshalk LA, Campbell WW, Evans WJ, Hakkinen A, Humphries BJ, Kraemer WJ. Changes in muscle morphology, electromyographic activity, and force production characteristics during progressive strength training in young and older men. J Gerontol A Biol Sci Med Sci. 1998;53:B415–B423. doi: 10.1093/gerona/53A.6.B415. [DOI] [PubMed] [Google Scholar]
- Hunter GR, Treuth MS, Weinsier RL, Kekes-Szabo T, Kell SH, Roth DL, Nicholson C. The effects of strength conditioning on older women's ability to perform daily tasks. J Am Geriatr Soc. 1995;43:756–760. doi: 10.1111/j.1532-5415.1995.tb07045.x. [DOI] [PubMed] [Google Scholar]
- Hunter GR, McCarthy JP, Bamman MM. Effects of resistance training on older adults. Sports Med. 2004;34:329–348. doi: 10.2165/00007256-200434050-00005. [DOI] [PubMed] [Google Scholar]
- Ivey FM, Roth SM, Ferrell RE, Tracy BL, Lemmer JT, Hurlbut DE, Martel GF, Siegel EL, Fozard JL, Jeffrey Metter E, Fleg JL, Hurley BF. Effects of age, gender, and myostatin genotype on the hypertrophic response to heavy resistance strength training. J Gerontol A Biol Sci Med Sci. 2000;55:M641–M648. doi: 10.1093/gerona/55.11.M641. [DOI] [PubMed] [Google Scholar]
- Jackson AS, Pollock ML. Generalized equations for predicting body density of men. Brit J Nutr. 1978;40:497–504. doi: 10.1079/BJN19780152. [DOI] [PubMed] [Google Scholar]
- Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70:113–119. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]
- Kallman DA, Plato CC, Tobin JD. The role of muscle loss in the age-related decline of grip strength: cross-sectional and longitudinal perspectives. J Gerontol A Biol Sci Med Sci. 1990;45:M82–M88. doi: 10.1093/geronj/45.3.m82. [DOI] [PubMed] [Google Scholar]
- Kamen G, Knight CA. Training-related adaptations in motor unit discharge rate in young and older adults. J Gerontol A Biol Sci Med Sci. 2004;59:1334–1338. doi: 10.1093/gerona/59.12.1334. [DOI] [PubMed] [Google Scholar]
- Kim K, Jang S, Lim S, Park YJ, Paik N, Kim KW, Jang HC, Lim J. Relationship between muscle mass and physical performance: is it the same in older adults with weak muscle strength? Age and Ageing. 2012;41:799–803. doi: 10.1093/ageing/afs115. [DOI] [PubMed] [Google Scholar]
- Klass M, Baudry S, Duchateau J. Voluntary activation during maximal contraction with advancing age: a brief review. Eur J Appl Physiol. 2007;100:543–551. doi: 10.1007/s00421-006-0205-x. [DOI] [PubMed] [Google Scholar]
- Knight CA, Kamen G. Adaptations in muscle activation of the knee extensor muscle with strength training in young and older adults. J Electromyogr Kinesiol. 2001;11:405–412. doi: 10.1016/S1050-6411(01)00023-2. [DOI] [PubMed] [Google Scholar]
- Korhonen MT, Mero AA, Alen M, Sipila S, Hakkinen K, Liikavainio T, Viitasalo JT, Haverinen MT, Suominen H. Biomechanical and skeletal muscle determinants of maximum running speed with aging. Med Sci Sports Exerc. 2009;41:844–856. doi: 10.1249/MSS.0b013e3181998366. [DOI] [PubMed] [Google Scholar]
- Kumagai K, Abe T, Brechue WF, Ryushi T, Takano S, Mizuno M. Sprint performance is related with muscle fascicle length in male 100m-sprinters. J Appl Physiol. 2000;88:811–816. doi: 10.1152/jappl.2000.88.3.811. [DOI] [PubMed] [Google Scholar]
- Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59:48–61. doi: 10.1093/gerona/59.1.M48. [DOI] [PubMed] [Google Scholar]
- Lynch NA, Metter EJ, Lindle RS, Fozard JL, Tobin JD, Roy TA, Fleg JL, Hurley BF. Muscle quality I. Age-associated differences between arm and leg muscle groups. J Appl Physiol. 1999;86:188–194. doi: 10.1152/jappl.1999.86.1.188. [DOI] [PubMed] [Google Scholar]
- Macaluso A, Nimmo MA, Foster JE, Cockburn M, McMillan NC, De Vito G. Contractile muscle volume and agonist–antagonist coactivation account for differences in torque between young and older women. Muscle Nerve. 2002;25:858–863. doi: 10.1002/mus.10113. [DOI] [PubMed] [Google Scholar]
- Malafarina V, Uriz-Otano F, Iniesta R, Gil-Guerrero L. Sarcopenia in the elderly: diagnosis, physiopathology and treatment. Maturitas. 2012;71:109–114. doi: 10.1016/j.maturitas.2011.11.012. [DOI] [PubMed] [Google Scholar]
- Manini TM, Clark BC. Dynapenia and aging: an update J Gerontol A Biol Sci Med Sci. 2012;67:28–40. doi: 10.1093/gerona/glr010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metter EJ, Lynch N, Conwit R, Lindle R, Tobin J, Hurley B. Muscle quality and age: cross-sectional and longitudinal comparisons. J Gerontol A Biol Sci Med Sci. 1999;54:B207–B218. doi: 10.1093/gerona/54.5.B207. [DOI] [PubMed] [Google Scholar]
- Misic MM, Rosengren KS, Woods JA, Evans EM. Muscle quality, aerobic fitness and fat mass predict lower-extremity physical function in community-dwelling older adults. Gerontology. 2007;53:260–266. doi: 10.1159/000101826. [DOI] [PubMed] [Google Scholar]
- Mitchell WK, Williams J, Atherton P, Larvin M, Lund J, Narici M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front Physiol. 2012;3:1–18. doi: 10.3389/fphys.2012.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley J. Sarcopenia in the elderly. Fam Pract. 2012;29:i44–i48. doi: 10.1093/fampra/cmr063. [DOI] [PubMed] [Google Scholar]
- Nogueira W, Gentil P, Mello SN, Oliveira RJ, Bezerra AJ, Bottaro M. Effects of power training on muscle thickness of older men. Int J Sports Med. 2009;30:200–204. doi: 10.1055/s-0028-1104584. [DOI] [PubMed] [Google Scholar]
- Pereira A, Izquierdo M, Silva AJ, Costa AM, Bastos E, González-Badillo JJ, Marques MC. Effects of high-speed power training on functional capacity and muscle performance in older women. Exp Gerontol. 2012;47:250–255. doi: 10.1016/j.exger.2011.12.010. [DOI] [PubMed] [Google Scholar]
- Reeves ND, Narici MV, Maganaris CN. Effect of resistance training on skeletal muscle-specific force in elderly humans. J Appl Physiol. 2004;96:885–892. doi: 10.1152/japplphysiol.00688.2003. [DOI] [PubMed] [Google Scholar]
- Rikli RE, Jones CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53:255–267. doi: 10.1093/geront/gns071. [DOI] [PubMed] [Google Scholar]
- Serra-Rexach JA, Bustamante-Ara N, Hierro Villarán M, González Gil P, Sanz Ibáñez MJ, Blanco Sanz N, Ortega Santamaría V, Gutiérrez Sanz N, Marín Prada AB, Gallardo C, Rodríguez Romo G, Ruiz JR, Lucia A. Short-term, light- to moderate-intensity exercise training improves leg muscle strength in the oldest old: a randomized controlled trial. J Am Geriatr Soc. 2011;59:594–602. doi: 10.1111/j.1532-5415.2011.03356.x. [DOI] [PubMed] [Google Scholar]
- Siri WE. Body composition from fluid spaces and density: analysis of methods. Nutrition. 1993;9:480–491. [PubMed] [Google Scholar]
- Tracy BL, Ivey FM, Hurlbut D, Martel GF, Lemmer JT, Siegel EL, Metter EJ, Fozard JL, Fleg JL, Hurley BF. Muscle quality. II. Effects of strength training in 65- to 75-yr-old men and women. J Appl Physiol. 1999;86:195–201. doi: 10.1152/jappl.1999.86.1.195. [DOI] [PubMed] [Google Scholar]