I n this series, a clinician extemporaneously discusses the diagnostic approach (regular text) to sequentially presented clinical information (bold). Additional commentary on the diagnostic reasoning process (italics) is integrated throughout the discussion.
Clinical Information.A 35-year-old man presented to the emergency department with new acute lower back pain for the past 2 hours. The pain was abrupt in onset and awoke the patient from sleep. The pain was described as sharp, 10/10 on a 1–10 pain scale, constant, and midline with no radiation. He experienced numbness and lack of sensation in the lower portion of his back more on the right side than the left. The pain was exacerbated by any flexion, extension, or rotation of the spine, and by hip flexion. No maneuvers alleviated the pain, and 800 mg of ibuprofen was ineffective.
Clinician. The differential diagnosis for acute lower back pain includes acute back strain with muscle spasm, vertebral disk herniation, and compression fracture. Spondyloarthritis, degenerative joint disease, and facet syndrome are usually more indolent. The most concerning causes of low back pain, such as diskitis, epidural abscess, or malignancy, are typically indolent but can sometimes present acutely. Consideration of these conditions is frequently prioritized because of their potential morbidity and mortality and their potential for rapid neurologic compromise. Non-musculoskeletal causes of lower back pain include pyelonephritis, nephrolithiasis, aortic dissection or rupture, pancreatitis, or a retroperitoneal hemorrhage. The spontaneous onset and maximal pain at onset makes these important considerations. Exacerbation with vertebral rotation, flexion, or extension is more consistent with a musculoskeletal etiology, although the abrupt onset during sleep is unusual. The worsening with hip flexion could reflect irritation or involvement of the psoas muscle, e.g., psoas abscess. Mid-back “numbness” is a peculiar symptom, and it would be important to know if the patient is referring to paresthesias or lack of sensation.
Diagnostic Reasoning.The problem representation is a 35-year-old man with new, acute, severe, asymmetric bilateral lower back pain that started during sleep. This has triggered illness scripts for common musculoskeletal conditions and for acute retroperitoneal processes, with elements supporting both groups of conditions. The features that support a musculoskeletal cause are compelling, but given the mismatch between the prototypical low back pain illness script and some clinical features (abrupt onset during sleep and local neurologic symptoms), the discussant is considering systemic or emergent disorders as well.
The patient denied shortness of breath, abdominal pain, fevers, chills, nausea, vomiting or weakness. He denied any recent trauma or overuse. The patient lived in California and Oregon for his entire life and last traveled to Greece 6 years earlier. He had been a regular weight lifter for the past 15 years. 17 years ago, he sustained a traumatic fracture to the transverse processes of L1, L3, and L4. Since that time, he had experienced intermittent, 5/10, diffuse low back tightness every few months during intense physical activity or when seated for extended periods. His only other medical problem was seasonal affective disorder, for which he took bupropion. He denied use of anabolic steroids or illicit drugs. He took creatine and nitrogen dioxide (NO2) supplements three times per week to assist in workout recovery and accelerate muscle hypertrophy.
On physical exam, the patient was in significant discomfort. He was afebrile with a blood pressure of 124/63 mmHg, a pulse of 82 per minute, respiratory rate of 25 breaths per minute, and an oxygen saturation of 99% on ambient air. His neck was supple with no midline tenderness. Heart, lung, abdominal, and skin examination were all normal. He had marked paraspinal tenderness to palpation bilaterally around the inferior thoracic and superior lumbar spine with no midline tenderness. Muscle spasm was palpated in the right thoracolumbar paraspinal region with numbness limited to this area. He had an antalgic gait, but there were no other motor or strength deficits on examination.
The red flag features of acute lower back pain—including fever, weight loss, intravenous drug use, history of cancer or immunocompromise, and lower extremity neurologic deficits—are absent. It is unusual for musculoskeletal conditions, such as tendon, ligament, or muscle injury from weightlifting, to awaken a patient at night; if not immediate, they more typically manifest upon awakening the next day. A compression fracture would be unlikely given his age, gender, and lack of osteoporosis risk factors. His previous back injury may heighten his sensitivity or susceptibility to recurrent injury. Numbness extending across multiple vertebrae is unusual, and could be explained by local swelling, perhaps creating a mass effect on somatic cutaneous nerve endings overlying the palpable muscle area. I would also investigate any adverse reactions associated with creatine or NO2 (e.g., dystonia).
In analyzing the clinical features thus far, the discussant is borrowing from the illness script forlowerback pain, where most of his clinical experience and virtually all of the literature on acute back pain derives from. By using analogical reasoning (where knowledge about a known problem or issue is used to infer understanding of the new problem), the discussant has derived the red flags and differential diagnosis of thoracolumbar pain, although this could be an errant assumption. With this additional historical information and the physical exam, the discussant has found additional evidence that supports a musculoskeletal etiology, but he continues to mentally track the acute onset at night and numbness. This mental accounting of discordant features is a key method of avoiding confirmation bias and premature closure.
His pain decreased from 10/10 to 7/10 with intravenous hydromorphone and diazepam. He was discharged with analgesics and muscle relaxants. At home, he required frequent doses of acetaminophen/oxycodone, hydrocodone, and diazepam for pain and was confined to his bed for 3 weeks due to unrelenting pain and stiffness. At an outpatient visit with his primary care provider, a large palpable swelling overlying the right thoracolumbar paraspinal muscles was detected. Creatine kinase level, which was normal during the initial ED evaluation, was now 626 units/L (normal 44–196). He was prescribed metaxalone, hydrocodone, and ketorolac for persistent muscle strain. Review of the literature did not reveal adverse effects on skeletal muscle from his two supplements.
Most acute low back pain is idiopathic, and symptoms typically subside after 4 to 6 weeks with analgesia, rest, and progressive activity. The extreme immobility, progressive pain, local swelling, and substantial analgesic requirements at 3 weeks signal a more serious disorder that will likely require imaging to fully evaluate. His mild rhabdomyolysis likely results from local muscle injury rather than a systemic condition based on the physical exam.
At an orthopedic clinic appointment 2 weeks after the primary care provider evaluation (and 5 weeks since the onset of pain), he had erythema and edema from T12 to L2 on his right low back, with severe tenderness to palpation over the right lumbar paraspinous and gluteal muscle groups. The patient was afebrile and the neurologic exam was normal. Lumbar spine radiographs were normal.
The examination has progressed both in severity and distribution (extending to the buttocks). The cardinal signs of inflammation—pain, swelling, erythema—are present. Although he remains afebrile, the subacute inflammation and focality suggests an indolent infection. Acute trauma or hematoma in soft tissue can serve as a nidus for a bacterial infection. He lacks risk factors for reactivation of or recent exposure to tuberculosis or endemic fungal infections, but these must be considered along with a bacterial abscess. A non-infectious cause of inflammatory myositis is possible, although most myopathies from systemic diseases, medications, or toxic exposures are widespread. A soft tissue tumor, such as rhabdomyosarcoma, should be considered. Given the ongoing pain and advancing focal inflammation, an MRI is indicated.
Most descriptions of illness scripts in the literature emphasize diagnostic information. However, clinicians’ mental models of diseases also encapsulate the typical natural history and treatment course of diseases. Previously, the notable but equivocal mismatches between the patient’s presentation and prototypical acute musculoskeletal strain were not enough to divert the discussant or treating clinician’s suspicion of musculoskeletal injury. However, the marked discordance now between expected and actual clinical course has prompted consideration more serious etiologies including infection, malignancy, autoimmunity, and toxicity.
MRI revealed avid enhancement in the periphery of the right paraspinous muscles, compatible with muscle strain and concomitant compartment syndrome or rhabdomyolysis without evidence of infection or malignancy (Fig. 1). The orthopedic surgeon felt surgical decompression was unlikely to provide relief after 5 weeks of symptoms, but would pose a risk of renal injury, shock, and infection from the release of potentially necrotic tissue in the compartment. Compartment pressures were not measured. Analgesics and progressive physical therapy were prescribed. MRI 5 months later revealed marked interval reduction in the peripheral enhancement within the right paraspinous muscles, indicating decreased muscle mass and abnormal T1 signal in some of the multifidus and longissimus muscles at the level of L3 to L5 containing areas of rim enhancement, suggestive of necrosis(Fig. 2).
Figure 1.
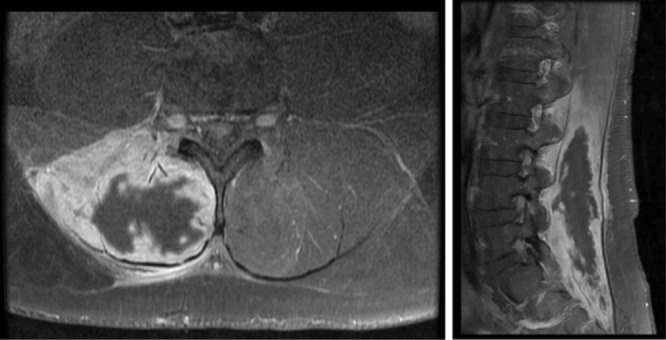
T1 axial (left) and sagittal (right) images 8 weeks after onset of symptoms. Avid enhancement in the periphery of the right paraspinous muscles, compatible with muscle strain and concomitant compartment syndrome.
Figure 2.
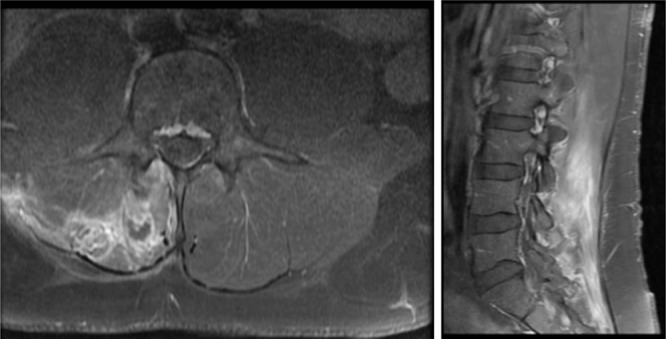
T1 axial (left) and sagittal (right) images 5 months after onset of symptoms. Interval reduction in the peripheral enhancement within the right paraspinous muscles indicating decreased muscle mass and possible areas of necrosis.
I was not aware of compartment syndrome of the back muscles, but in retrospect, all the signs make sense and the conclusion appears to be supported by the imaging, which I would re-review directly with the musculoskeletal radiologist. Given that this is an important decision with regards to functional outcome, but also is an infrequently encountered syndrome, I would want to know if the surgeon was making the decision to not operate based on evidence, personal experience with the condition, or extrapolation from experience with other compartment syndromes.
The discussant discloses that he did not have a pre-existing illness script for paraspinous compartment syndrome. Infrequently encountered and evidence-deficient scenarios can lead to suboptimal management judgments. In these situations a second or third opinion could optimize decision making by increasing the collective experience that is brought to bear on the decision.
The patient was advised to continue with medications for pain control and physical therapy. Two years later, the patient continues to struggle with chronic lower back pain and pain management issues, which have limited his previously active lifestyle.
COMMENTARY
Back pain is the third most common reason for seeing a physician in the United States.1 In 1998, total health care expenditures incurred by individuals with back pain in the United States reached $90.7 billion; the total incremental expenditures attributable to back pain were approximately $26.3 billion.2 This case illustrates an unusual and disabling cause of lower back pain that can be adequately treated when recognized early.
The clinical approach to many common, self-limited conditions like back pain, diarrhea, or red eye emphasizes the search for “red flag” symptoms and signs that alert the clinician to consider a more serious condition that requires addition testing or directed treatment. A red flag symptom or sign however rarely unequivocally signals a new serious disorder and rarely triggers a compulsory next step for the treating clinician. The presence of most red flags in low back pain only modestly decreases the probability that standard musculoskeletal injury is responsible. For instance, most patients with weight loss and back pain do not have cancer,3 and most patients who use IV drugs with back pain do not harbor an epidural abscess.
The variation in how clinicians react to the presence of red flags in acute back pain reveals differing diagnostic thresholds (e.g., to pursue MRI). One clinician may image all back pain in an intravenous drug user (citing the low specificity of fever or leukocytosis for example), while another clinician may set a higher threshold that requires fever with a neurologic deficit. The presence of red flag symptoms transforms the familiar cognitive task of evaluating low back pain into a more complex evaluation of diagnostic thresholds and resource utilization.
This case posed multiple cognitive barriers to a prompt diagnosis and treatment. The patient did not have classic red flag features endorsed in evidence-based guidelines for low back pain.4 He did have two unusual symptoms (acute nocturnal pain and focal back numbness) that caught the attention of the discussant and the treating clinicians, but these symptoms did not map to a familiar illness script or diagnostic rule, and therefore did not alter their threshold for MRI imaging. Nocturnal pain (chronic not acute) was listed as a red flag symptom in the 1994 AHRQ low back pain guidelines, but subsequent studies have shown that this symptom does not predict serious systemic causes of low back pain such as cancer, infection, or spondylarthroapthy.5,6 Second, a common complication of back pain—muscle spasm—provided a plausible explanation for his failure to improve quickly. In real time, it is very difficult for clinicians to know when to surrender their suspicion of an atypical manifestation of a common illnesses (e.g., muscle strain superimposed upon acute injury) to pursue the typical manifestation of an uncommon illness (e.g., paraspinous compartment syndrome), especially when clinical experience and medical education appropriately favors the former. Finally, the rarity of paraspinous compartment syndrome hampers early detection and treatment.
We present this case report in an effort to help mitigate this final factor for readers. Many of the classic signs of extremity compartment syndrome—severe pain with passive stretch, pallor, paralysis, pulselessness, and paresthesias—are not seen in paraspinous compartment syndrome, and therefore cannot serve as trigger to consider the diagnosis (see Clinical Teaching Points for clinical features). By the time the condition manifested with an overt mismatch with typical back pain, the surgeon felt the window for acute intervention had closed.
This case highlights the diagnostic challenge of promptly detecting unusual, but treatable, conditions concealed among myriad common presentations (the needle in the haystack phenomenon). The increased attention on diagnostic errors has generated potential solutions to this dilemma, including diagnostic checklists and computerized decision support. These measures may help the clinician consider and detect unusual syndromes, but there is a risk that these tools may increase sensitivity at the expense of decreased specificity and increased resource utilization (e.g., more MRI imaging every time the remote possibility of serious diagnoses is triggered). Such an outcome would be increasingly untenable as we adopt initiatives such as the American Board of Internal Medicine’s Choosing Wisely campaign, and adapt our training programs to make physicians better stewards of limited health careresources.7
CLINICAL TEACHING POINTS
Compartment syndrome is an acute rise in compartment pressure leading to reduced blood flow and tissue necrosis. It can occur in any muscular tissue that is encased by a fibro-osseous space, including the erector spinae (encased within the lumbodorsal fascia).
Compartment syndrome typically occurs after crush type injuries in the extremities, but can also develop following increased muscle exertion.
Previously described cases of paraspinous compartment syndrome have had the following features: men aged 24–37 years old with active lifestyles, previous low back injury, recent physical exertion, severe lumbosacral pain out of proportion to the examination, pain refractory to narcotics, and elevated serum creatine kinase levels (range 5,465–60,000 U/L).8–14
Key physical exam findings include loss of lordosis, pain exacerbated by straight leg raise, and sensory loss over the affected area.
Measurement of compartment pressure is the gold standard for diagnosis. Serum CK elevation and CT or MRI of the back are useful diagnostic adjuncts.
Fasciotomy is the definitive treatment.
Although nocturnal back pain is often cited as a red flag symptom based on 1994 guidelines, there is no strong evidence suggesting that nocturnal back pain predicts infection or malignancy in the spine.
Acknowledgements
Contributors
None besides the authors.
Funders
None.
Conflicts of Interest
There are no conflicts of interest related to this submission for any of the authors.
REFERENCES
- 1.St Sauver JL, Warner DO, Yawn BP, Jacobson DJ, McGree ME, Pankratz JJ, et al. Why patients visit their doctors: assessing the most prevalent conditions in a defined American population. Mayo Clinic proceedings. Mayo Clinic. 2013;88(1):56–67. doi: 10.1016/j.mayocp.2012.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine. 2004;29:79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 3.Deyo RA, Diehl AK. Cancer as a cause of back pain: frequency, clinical presentation, and diagnostic strategies. J Gen Intern Med. 1988;3(3):230–8. doi: 10.1007/BF02596337. [DOI] [PubMed] [Google Scholar]
- 4.Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. What’s New? What’s Different? Available at: http://guideline.gov/expert/printView.aspx?id=16452. Accessed March 20, 2013. [DOI] [PubMed]
- 5.Harding IJ, Davies E, Buchanan E, Fairbank JT. The symptom of night pain in a back pain triage clinic. Spine. 2005;30(17):1985–8. doi: 10.1097/01.brs.0000176313.02258.5e. [DOI] [PubMed] [Google Scholar]
- 6.Keeling SO, Majumdar SR, Conner-Spady B, Battie MC, Carroll LJ, Maksymowych WP. Preliminary validation of a self-reported screening questionnaire for inflammatory back pain. J Rheumatol. 2012;39(4):822–9. doi: 10.3899/jrheum.110537. [DOI] [PubMed] [Google Scholar]
- 7.Choosing Wisely campaign. Available at: http://www.abimfoundation.org/Initiatives/Choosing-Wisely.aspx. Accessed March 20, 2013.
- 8.Wik L, Patterson JM, Oswald AE. Exertional paraspinal muscle rhabdomyolysis and compartment syndrome: a cause of back pain not to be missed. Clin Rheumatol. 2010;29(7):803–5. doi: 10.1007/s10067-010-1391-9. [DOI] [PubMed] [Google Scholar]
- 9.Carr D, Gilbertson L, Frymoyer J, Krag M, Pope M. Lumbar paraspinal compartment syndrome. A case report with physiologic and anatomic studies. Spine. 1985;10(9):816–20. doi: 10.1097/00007632-198511000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Kitajima I, Tachibana S, Hirota Y, Nakamichi K. Acute paraspinal muscle compartment syndrome treated with surgical decompression: a case report. Am J Sports Med. 2002;30(2):283–5. doi: 10.1177/03635465020300022301. [DOI] [PubMed] [Google Scholar]
- 11.Minnema BJ, Neligan PC, Quraishi NA, Fehlings MG, Prakash S. A case of occult compartment syndrome and nonresolving rhabdomyolysis. J Gen Intern Med. 2008;23(6):871–4. doi: 10.1007/s11606-008-0569-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paryavi E, Jobin CM, Ludwig SC, Zahiri H, Cushman J. Acute exertional lumbar paraspinal compartment syndrome. Spine. 2010;35(25):E1529–33. doi: 10.1097/BRS.0b013e3181ec4023. [DOI] [PubMed] [Google Scholar]
- 13.Stock KW, Helwig A. MRI of acute exertional rhabdomyolysis–in the paraspinal compartment. J Comput Assist Tomogr. 1996;20(5):834–6. doi: 10.1097/00004728-199609000-00033. [DOI] [PubMed] [Google Scholar]
- 14.DiFazio FA, Barth RA, Frymoyer JW. Acute lumbar paraspinal compartment syndrome. A case report. J Bone Joint Surg Am. 1991;73(7):1101–3. [PubMed] [Google Scholar]


