ABSTRACT
BACKGROUND
Inequity in cancer outcomes for minorities and vulnerable populations has been linked to delays in cancer care that arise from barriers to accessing care. Social service barriers represent those obstacles related to meeting life’s most basic needs, like housing and income, which are often supported by public policy, regulation and services.
OBJECTIVE
To examine the association between social service barriers and timely diagnostic resolution after a cancer screening abnormality.
DESIGN
Secondary analysis of the intervention arm of Boston Patient Navigation Research Program (2007–2008) conducted across six urban community health centers. Subjects with no barriers, other barriers, and social service barriers were compared on their time to diagnostic resolution.
SUBJECTS
Women ≥ 18 years of age with a breast or cervical cancer screening abnormality.
MAIN MEASURES
Social service barriers included: income supports, housing and utilities, education and employment, and personal/family stability and safety. Time to event analyses compared across five groups: those with no barriers, one barrier (other), one barrier (social service), two or more barriers (all other), and two or more barriers (at least one social service).
KEY RESULTS
1,481 navigated women; 31 % Hispanic, 27 % Black, 32 % White; 37 % non-English speakers and 28 % had private health insurance. Eighty-eight women (6 %) had social service barriers. Compared to those without social service barriers, those with were more likely to be Hispanic, younger, have public/no health insurance, and have multiple barriers. Those with two or more barriers (at least one social service barrier), had the longest time to resolution compared to the other four groups (aHR resolution < 60 days = 0.27, ≥ 60 days = 0.37).
CONCLUSION
Vulnerable women with multiple barriers, when at least one is a social service barrier, have delays in care despite navigation. The impact of patient navigation may never be fully realized if social service barriers persist without being identified or addressed.
KEY WORDS: access to care, cancer, disparities, vulnerable populations
INTRODUCTION
Inequity in cancer outcomes for racial/ethnic minorities and socioeconomically disadvantaged populations has been increasingly linked to delays in the delivery of quality cancer care.1,2 These inequities are attributable to the social determinants of health; the environmental conditions in which people live that affect a wide array of health, functioning, and life outcomes.3 These social determinants of health, such as safe and affordable housing, access to education and employment, and personal safety, culminate in a wide range of financial, structural, and personal obstacles to completing cancer care.4 These obstacles to health care are the driving force behind public policy, regulation, and social services that exist to ameliorate their health impact.
Despite regulations and programs to support individuals experiencing barriers to care, evidence suggests that vulnerable populations don’t fully utilize and access these resources, nor are health providers adequately equipped to address them. A LegalHealth study found that many cancer survivors were knowledgeable about resources available to them, but were unable to access them or were delayed in their application process.5 According to a recent study by the Robert Wood Johnson Foundation, over 80 % of physicians acknowledged the importance of addressing social needs, yet did not feel confident in their ability to address them.6
In recognition of the role barriers may have on health outcomes, patient navigation was designed as a patient-centered7–8model to address barriers to care.9–11 Patient navigation has been defined as the logistic and emotional support needed to achieve timely and quality diagnostic and treatment care.12 Patient navigators are trained to help patients negotiate a complex health care system and identify and overcome barriers to care in a culturally sensitive manner.12While there is evidence that navigation improves timely care for many,9,13,14 the impact of specific barriers to care remains largely unknown. Specifically, it is unknown whether patient navigators have the training or resources available to address social service barriers.
In order to assess the impact of social service barriers on cancer health disparities, we conducted an exploratory analysis of data collected in the Boston Patient Navigation Research Program, one of ten sites of the National Patient Navigation Research Program.12Our goal was to understand the impact that social service barriers have on time to diagnostic resolution after a cancer screening abnormality.
METHODS
Study Design
We conducted a secondary analysis of the intervention arm of the Boston Patient Navigation Research Program (PNRP), a quasi-experimental patient navigation intervention across six inner-city community health center sites for women with breast and cervical cancer screening abnormalities (2007–2010).9 The Boston University Institutional Review Board approved this study.
Navigation Intervention
Patient navigators were paid employees of the community health centers, imbedded in the clinical practices, with the goal of reducing delays in diagnostic care after abnormal cancer screening. Patient navigators were intentionally selected from the community in which they served, with the notion that they may have an increased ability to elicit barriers and build rapport with patients. Navigators contacted subjects by telephone to initiate navigation after a clinician had informed the subject of an abnormal test result. Navigators completed national trainings on identifying barriers to completing clinical care and employing culturally appropriate resources and strategies to address such barriers.
Study Population
Eligible women were over 18 years of age and had a breast (mammography or abnormal clinical examination) or cervical (Pap test) cancer screening abnormality performed at any of the six intervention sites during 2007–2008. Abnormal mammograms included Breast Imaging Reporting and Data System (BI-RADS) scores indicating need for follow-up (BI-RADS 0, 3, 4, and 5). Eligible Pap tests included cellular abnormalities indicating need for follow-up: atypical squamous cells of undetermined significance positive for human papillomavirus (ASCUS/HPV+), low-grade squamous intraepithelial lesion (LGSIL), or high-grade squamous intraepithelial lesions (HGSIL). Control subjects were excluded from this analysis since barrier data was only collected for intervention subjects.
Data Collection
All data were captured through the electronic medical record (EMR) at each health center. Data was collected by automated electronic reporting and manual abstraction. First, patient electronic charts recorded all screening studies and their results, enabling us to capture sociodemographics (age, race/ethnicity, primary spoken language and primary health insurance) and screening abnormalities. Barriers to care were captured by electronic reporting from navigator logs developed for the research study. During subject encounters, navigators identified barriers to care and recorded them in a log within the chart, which included 20 prespecified barrier categories (Table 1) and one open field “other” category.12 Barriers were defined by whether the patient reported that the issue was affecting or delaying their care. For example, the lack of health insurance was not recorded as a barrier to care until the subject perceived that the lack of insurance delayed her access to timely care.
Table 1.
Barriers in the Boston Patient Navigation Research Program: Categorized as Social Service and Other Barriers
| Social service barriers | Other barriers |
|---|---|
| • Insurance | • Transportation |
| • Financial Problems | • Social/Practical Support |
| • Housing | • Language |
| • Employment Issues | • Literacy |
| • Childcare Issues | • Location of Health Care Facility |
| • Adult Care | • Communication Concerns with Medical Personnel |
| • Fear | |
| • Medical & Mental Health Comorbidity | |
| • Patient Disability | |
| • Out of Town/Country | |
| • Perceptions/Beliefs about Tests/Treatment | |
| • System Problems with Scheduling Care | |
| • Attitudes Towards Providers | |
| • Other |
Study Measures
For the purposes of this analysis, we categorized the barrier data into two categories: barriers that correspond to social service barriers and other (or non-social service) barriers (Table 1). Social service barriers fit within the construct of social determinants of health, and were conceptualized according to a framework utilized by Medical-Legal Partnership commonly referred to by the acronym I-HELP. I-HELP represents the five common social service barrier domains that Medical–Legal Partnership programs address in the healthcare setting through legal advocacy. In this study, we define social service barriers by the following: health insurance and financial problems barriers (Income supports & Insurance) housing barriers (Housing & Utilities), employment issues (Employment & Education), and adult care and childcare (Personal and Family Stability and Safety).15 There was no corresponding barrier category in the navigator log relating to Legal Status. Each I-HELP category reflects basic life needs that, if not met, may affect health and be amenable to legal advocacy or service intervention should initial efforts to satisfy these needs fail. All other documented barriers were categorized as other (non-social service) barriers. Other barriers included medical or mental health comorbidities, patient perceptions, problems with scheduling, fear, or attitudes towards providers. These barriers have solutions outside of the social service or legal advocacy sector. Each unique barrier was counted once per subject, even if recorded on multiple encounters; however, subjects could have multiple barriers.
The first outcome of interest was whether diagnostic resolution of the screening abnormality was achieved within 365 days of the initial screening abnormality. The second outcome was time to diagnostic resolution, defined as the number of days from the initial screening abnormality to when the final definitive diagnostic test or evaluation was completed.9 For BI-RADS 4/5 lesions,16 this time point was the date of biopsy, or date in which additional imaging redesignated the image as BI-RADS 1 or 2. For BI-RADS 3 imaging, where serial 6-month imaging for up to 2 years is recommended, we confirmed when the next imaging was completed. We subtracted 180 days from the diagnostic evaluation time, which allowed us to compare all abnormalities in a similar time frame. If the BI-RADS 3 was addressed in less than 180 days, we used 0.5 days for the time to diagnostic resolution. For BI-RADS 0 lesions, resolution was defined as either follow-up imaging designated BI-RADS 1/2, or completion of diagnostic testing recommended by the healthcare provider. For cervical abnormalities, diagnostic resolution was usually colposcopy with biopsy diagnosis.
Data Analysis
Due to a limited sample size, breast and cervical subjects were combined for all analyses. Bi-variate analyses were conducted to compare subjects with no barriers, other barriers, and social service barriers, using analysis of variance (ANOVA) for means of measurement variables, the Kruskall–Wallis test for median time to resolution, and chi-square for categorical variables. Descriptive statistics examined the distribution and frequency of barrier categories and whether an action was taken.
Because of potential confounding by the presence of multiple barriers, we conducted our time to event analyses comparing across five groups: those with no barriers, one barrier (other), one barrier (social service), multiple barriers (other), and multiple barriers (at least one social service). We plotted Kaplan–Meier curves to examine the effect of the type and number of barriers on time to diagnostic resolution across groups, and compared time to resolution through log-rank tests. Proportional hazards regression models compared time to resolution across the five groups, controlling for site of care, age, race/ethnicity, primary language, and insurance. We included interaction terms with the time to diagnostic resolution variable where proportional hazards assumptions were violated. Adjusted hazard ratios less than 1.0 indicate longer time to resolution. Statistical significance was defined at p < 0.05 and all analyses were conducted in SAS.
RESULTS
Among 1,493 subjects enrolled in the navigation arm, 1,481 subjects (760 breast and 721 cervical) had complete data and were included in analyses. The sample represented a diverse group of women: 31 % were Hispanic, 27 % African-American, one-third were non-English speakers, and the majority had public or no health insurance. Table 2 displays subject characteristics by type of barrier (no barrier, other barrier, social service barrier). Half the subjects had one or more barriers documented by patient navigators (44 % with other barriers and 6 % with social service barriers). Eighty-eight subjects (52 cervical and 36 breast) had one or more social service barrier. Compared to those with no barriers and other barriers, subjects with social service barriers were more likely to be Hispanic, younger, and uninsured. Subjects with no barriers were largely white and English-speaking.
Table 2.
Subject Characteristics by Type of Barrier (N = 1481) Boston Patient Navigation Research Program
| Total N (%) | No barriers N (%) | Other barriers* N (%) | Social service barriers† N (%) | p | ||
|---|---|---|---|---|---|---|
| Total (%) | N = 1481 | 736 (50) | 657 (44) | 88 (6) | ||
| Race/Ethnicity | < 0.0001 | |||||
| White | 468 (32) | 296 (40) | 149 (23) | 23 (26) | ||
| African-American | 405 (27) | 202 (27) | 181 (28) | 22 (25) | ||
| Hispanic | 460 (31) | 197 (27) | 227 (34) | 36 (41) | ||
| Other | 148 (10) | 41 (6) | 100 (15) | 7 (8) | ||
| Age Category | < 0.0001 | |||||
| 18–29 | 486 (33) | 262 (35) | 184 (28) | 40 (45) | ||
| 30–39 | 245 (16) | 145 (20) | 89 (13) | 11 (12) | ||
| 40–49 | 396 (27) | 177 (24) | 190 (29) | 29 (33) | ||
| 50+ | 354 (24) | 152 (21) | 194 (30) | 8 (9) | ||
| Language | < 0.0001 | |||||
| English | 925 (63) | 520 (71) | 349 (53) | 56 (64) | ||
| Spanish | 317 (21) | 126 (17) | 167 (25) | 24 (27) | ||
| Other | 239 (16) | 90 (12) | 141 (21) | 8 (9) | ||
| Insurance | < 0.0001 | |||||
| Private | 410 (28) | 254 (35) | 142 (21) | 14 (16) | ||
| Public‡ | 657 (44) | 287 (39) | 327 (50) | 43 (49) | ||
| No insurance | 414 (28) | 195 (26) | 188 (29) | 31 (35) |
*Other Barriers: Transportation, social/practical support, language, literacy, location of health care facility, communication concern with medical personnel, fear, medical & mental health comorbidity, patient disability, out of town/country, perceptions/beliefs about tests/treatment, system problems with scheduling care, and attitudes towards providers
†Social Service Barriers: Health insurance, financial barriers, housing barriers, employment issues, adult care, and childcare
‡Public insurance: Medicaid, Medicare and Massachusetts subsidized health plans for those with incomes less than 300 % federal poverty level
Of the 88 subjects with social service barriers, 96 unique social service barriers were documented, with six subjects reporting more than one social service barrier. We assessed the distribution of social service barriers across I-HELP categories. The most common social service barrier documented was employment (N = 52), followed by income supports (N = 25). There were fewer documented barriers related to personal and family safety and stability (N = 13) and housing issues (N = 6).
We examined the association between type of barrier (social service versus other) and number of unique barriers present for each subject. Those with a social service barrier were more likely to have multiple barriers compared to those with only other barriers (59 % versus 23 %, p < 0.0001).
We measured the unadjusted timeliness outcomes by barrier type. Compared to subjects with no barriers and other barriers, the social service barrier group had the smallest proportion reaching diagnostic resolution by 365 days (94 % and 88 % versus 81 %, p < 0.0001) and the longest median days to resolution (50 days and 53 days versus 95 days, p < 0.0001).
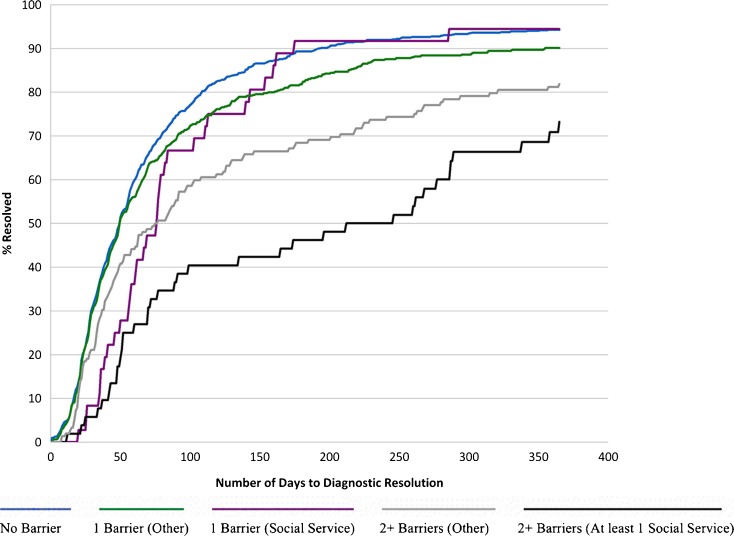
Figure 1 displays the Kaplan–Meier curves for time to diagnostic resolution (y- axis represents the proportion achieving diagnostic resolution) across five barrier groups. For no barrier and one other barrier, the curves appear superimposed until 60 days, when subjects with one other barrier are less likely to achieve timely diagnostic resolution (p = 0.010). Those with two or more barriers (other and at least one social service) diverge almost immediately, such that they are each less likely to achieve diagnostic resolution compared to those with no or one other barrier. Those with two or more barriers (at least one social service) were least likely to achieve timely resolution compared to those with no barrier (p < 0.001), those with one other barrier (p = 0.001), and those with two or more other barriers (p = 0.014).
Figure 1.
Kaplan–Meier survival curves of time to diagnostic resolution by barrier category.
Table 3 presents the adjusted Hazard Ratios (aHR) for reaching diagnostic resolution by type of barrier after controlling for age, race/ethnicity, language, insurance, and adjusting for site of care by cluster. Since there were violations in proportional hazards assumptions for the subgroups with social service barriers, we present aHRs for diagnostic resolution before and after 60 days. Relative to subjects with no identified barriers to care, all women with barriers had less timely diagnostic resolution (indicated by aHR < 1.0, where an aHR greater than 1.0 indicates more timely resolution). The hazards ratios indicate that once stratifying for number of barriers, women with multiple barriers (including at least one social service barrier) had the least timely diagnostic resolution (< 60 days aHR = 0.27 [0.15–0.46], ≥ 60 days aHR = 0.37 [0.24–0.57]).
Table 3.
Adjusted Cox Proportional Hazards Models Predicting Time to Diagnostic Resolution Boston Patient Navigation Research Program
| Barrier category | Adjusted HR (95 % CI)* | p |
|---|---|---|
| No Barrier | 1.0 (reference) | |
| 1 Barrier (Other†) | 0.77 (0.68–0.88) | < 0.0001 |
| 1 Barrier (Social Service‡) | ||
| Resolution < 60 days | 0.47 (0.27–0.81) | 0.007 |
| Resolution ≥60 days | 1.16 (0.74–1.82) | 0.43 |
| 2+ Barriers (Other) | 0.45 (0.37–0.56) | < 0.0001 |
| 2+ Barriers (At least 1 Social Service) | ||
| Resolution < 60 days | 0.27 (0.15–0.46) | < 0.0001 |
| Resolution ≥ 60 days | 0.37 (0.24–0.57) | < 0.0001 |
*Cox proportional analysis adjusted for age, race/ethnicity, language, insurance, site of care
aHR > 1.0 indicates shorter time to diagnostic resolution than the reference group
†Other Barriers: Transportation, social/practical support, language, literacy, location of health care facility, communication concern with medical personnel, fear, medical & mental health comorbidity, patient disability, out of town/country, perceptions/beliefs about tests/treatment, system problems with scheduling care, and attitudes towards providers
‡Social Service Barriers: Health insurance, financial problems, housing, employment issues, adult care, and childcare issues
DISCUSSION
This study describes the impact of social service barriers on delays in care among a vulnerable population of women in need of diagnostic cancer care. We have defined a set of social services barriers that reflect some aspect of the social determinants of health and may be ameliorated by programs and policies that have been developed to promote the health of the population. We found that those subjects with social service barriers are among the most vulnerable populations (Hispanic, younger, and uninsured), and are also more likely to have multiple barriers to care. When conducting stratified analyses by barrier number with adjusted Cox models to address potential confounding by demographic factors, we found significant delays in care among women with social services barriers.
While our main analysis of the Boston Patient Navigation Research Program (PNRP) demonstrated an overall improvement in timeliness of diagnostic care after abnormal cancer screening in the navigation intervention arm compared to the control condition,9 these findings suggest that a subset of subjects did not benefit equally. Navigated subjects with social service barriers had greater delays in care compared to those without. This may be due in part to the inherent differences between social service barriers and other non-social service barriers to care. First, our findings suggest that the presence of social service barriers is a marker for a high burden of other more traditional barriers to care. It is also conceivable that social service barriers are more complex and require intervention beyond the scope of work of a patient navigator. Traditional training of patient navigators does not include education around public policy and regulation, an area typically covered by social work. While there were varying degrees of social work support across health center sites in this study, our data suggests that navigation in its current form may not adequately identify social service needs, which would ideally prompt a social work consultation to address those needs.
Because of mounting evidence documenting the benefits of patient navigation on the delivery of timely cancer care,9,14,17,18 some professional organizations10,11 now recommend navigation as a standard service requirement for cancer care programs. To improve the health of vulnerable populations like the one in this study, navigation programs must first identify those barriers most likely to interfere with care delivery. Our study suggests that an increased emphasis on social service barriers may be necessary to identify and address these types of obstacles to cancer care. Patient navigation programs may consider this as they work to develop standardized training curricula,19 as competency in the ability to identify relevant obstacles to care is a critical step to connecting vulnerable patients to existing resources.
While social workers are one resource to address social service barriers to care, there has been a recent movement to include legal advocacy into medical teams serving the most vulnerable populations, to ensure that public policy and regulation are enforced. Medical–Legal Partnerships nationwide20–22 seek to address social service barriers through collaboration of legal advocates within the medical team. Social service barriers may have a legal dimension to the extent that a patient has sought resources or assistance from an agency/authority and has been denied that support, evidently in violation of legal rights. Likewise, for patient navigators and oncology social workers, access to legal advocacy may allow them to improve their capacity to support patients by addressing barriers that threaten their ability to complete cancer care.
Through capacity building within the healthcare team, these programs advocate for access and utilization of public programs and policies and/or enforce existing laws that protect patients, especially those that ensure access to basic social needs. The American Bar Association (ABA) uses a similar model to examine these basic needs and labels them as legal needs. National studies by the ABA show that low-income Americans typically have two to three legal needs in areas related to health, including housing, disability supports, family stability/safety and access to disability accommodations in work and school.20 Another study among cancer patients found that 61 % of patients reported two or more legal barriers, while only 20 % reported that they had their barrier addressed.5 By screening, identifying, and resolving unmet social needs before they develop into true barriers and legal emergencies, Medical–Legal Partnership programs have shown the ability to improve care delivery for pediatric populations.22,23 This has important implications for cancer care delivery in safety net settings caring for similar vulnerable populations. While LegalHealth (New York, NY), the first legal services program serving people with cancer, has documented patient benefits through several case studies,5 more rigorous studies are needed targeting the most vulnerable populations.
We recognize several limitations of our findings. Our current study was a secondary analysis, and was not designed to specifically identify social service barriers. Navigators were trained to identify and document barriers from a pre-set list, which we later used to categorize social service barriers. We cannot know if a barrier categorized as social service in nature truly represents a barrier with public policy solutions. We were limited in our ability to discern the impact of the specific types of social service barriers due to the small sample size of those with social service barriers (n = 88). Finally, confounding by indication was possible, since delays in care allowed for more navigator encounters and thus more opportunity to identify barriers. While possible, there was likely minimal impact of such confounding, given that the majority of barriers were identified in the first encounter.
CONCLUSIONS
We demonstrate that the presence of a social service barrier, especially in women with multiple barriers to care, is associated with delays in diagnostic resolution after an abnormal cancer screening, even in the presence of navigation services. This study supports the need to better understand the burden of such obstacles to care, as existing services to address social service barriers may lead to improved outcomes. Partnerships that integrate legal services and advocacy into the health care team have the potential to expand the capacity of existing patient navigation programs to identify and address social service barriers. Just as a physician refers a patient to a pulmonologist for asthma that standard treatment cannot control, a navigator may refer patients to on-site legal advocates when an underlying social circumstance impairs access to cancer services and demands resources and solutions beyond the expertise of the medical team.
Acknowledgements
Our sincere appreciation to the Boston Patient Navigation Research Program (The National Cancer Institute NCI U01CA116892) for providing the data necessary to complete these analyses, and to MLP|Boston for their collaboration on this research. This research was supported by a training grant from Susan G. Komen for the Cure (KG101421). Preliminary findings from this study were previously presented at the American Association for Cancer Research (AACR) Conference on The Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved (October 2012), and at the American Public Health Association Annual Meeting (October 2012).
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.American Cancer Society. Cancer Facts & Figures 2012. Atlanta: American Cancer Society.
- 2.Shavers VL, Brown ML. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst. 2002;94(5):334–57. doi: 10.1093/jnci/94.5.334. [DOI] [PubMed] [Google Scholar]
- 3.Healthy People 2020. 2013 social determinants of health. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39. Accessed August 20, 2013.
- 4.American Cancer Society. Cancer Facts & Figures 2012. Atlanta: American Cancer Society, 2012. Available at: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf. Accessed August 20, 2013.
- 5.Retkin RBJ, Bacich C. Impact of legal interventions on cancer survivors. Legal Health 2007. Available at: http://legalhealth.org/wp-content/uploads/2012/07/FinalReportImpactofLegalInterventionsoncancersurvivors.pdf
- 6.The Robert Wood Johnson Foundation. Health Care’s blindside: The overlooked connection between social needs and good health: summary of findings from a survey of America’s physicians. Dec. 2011. Available at: http://www.rwjf.org/content/dam/farm/reports/surveys_and_polls/2011/rwjf71795. Accessed August 20, 2013.
- 7.Rittenhouse DR, Shortell SM. The patient-centered medical home: will it stand the test of health reform? JAMA. 2009;301(19):2038–40. doi: 10.1001/jama.2009.691. [DOI] [PubMed] [Google Scholar]
- 8.Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient-centered health care. Health Aff (Millwood). 29(8):1489–95. [DOI] [PubMed]
- 9.Battaglia TA, Bak SM, Heeren T, et al. Boston patient navigation research program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 21(10):1645–54. [DOI] [PMC free article] [PubMed]
- 10.American College of Surgeons. Commission on Cancer. Cancer Program Standards 2012: Ensuring patient centered care. Available at: http://www.sgmc.org/sites/www/Uploads/COC%20Program%20Stds%202012.pdf. Accessed August 20, 2013.
- 11.American College of Surgeons. National accreditation program for breast centers; 2011 [cited 2011 Mar 28]. Available at: http://accreditedbreastcenters.org/accreditation/application.html. Accessed August 20, 2013.
- 12.Freund KM, Battaglia TA, Calhoun E, et al. National cancer institute patient navigation research program: methods, protocol, and measures. Cancer. 2008;113(12):3391–9. doi: 10.1002/cncr.23960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ell K, Vourlekis B, Lee PJ, Xie B. Patient navigation and case management following an abnormal mammogram: a randomized clinical trial. Prev Med. 2007;44(1):26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Raich PC, Whitley EM, Thorland W, Valverde P, Fairclough D. Patient navigation improves cancer diagnostic resolution: an individually randomized clinical trial in an underserved population. Cancer Epidemiol Biomarkers Prev. 21(10):1629–38. [DOI] [PMC free article] [PubMed]
- 15.Kenyon C, Sandel M, Silverstein M, Shakir A, Zuckerman B. Revisiting the social history for child health. Pediatrics. 2007;120(3):e734–8. doi: 10.1542/peds.2006-2495. [DOI] [PubMed] [Google Scholar]
- 16.American College of Radiology (ACR). Illustrated breast imaging reporting and data System (BI-RADS). 4th ed. Reston VA: American College of Radiology; 2003.
- 17.Paskett ED, Katz ML, Post DM, et al. The Ohio Patient Navigation Research Program: does the American Cancer Society patient navigation model improve time to resolution in patients with abnormal screening tests? Cancer Epidemiol Biomarkers Prev. 21(10):1620–8. [DOI] [PMC free article] [PubMed]
- 18.Hoffman HJ, LaVerda NL, Young HA, et al. Patient navigation significantly reduces delays in breast cancer diagnosis in the District of Columbia. Cancer Epidemiol Biomarkers Prev. 21(10):1655–63. [DOI] [PMC free article] [PubMed]
- 19.National Patient Navigation Consortium. Available at: http://nationalpatientnavigationconsortium.com/. Accessed August 20, 2013.
- 20.National Center for Medical Legal Partnership. MLP Network. (2012) Available at: http://www.medical-legalpartnership.org/. Accessed August 20, 2013.
- 21.Medical Legal Partnership Boston. (2013) Available at: http://www.mlpboston.org/. Accessed August 20, 2013.
- 22.Zuckerman B, Sandel M, Smith L, Lawton E. Why pediatricians need lawyers to keep children healthy. Pediatrics. 2004;114(1):224–8. doi: 10.1542/peds.114.1.224. [DOI] [PubMed] [Google Scholar]
- 23.Weintraub D, Rodgers MA, Botcheva L, et al. Pilot study of medical-legal partnership to address social and legal needs of patients. J Health Care Poor Underserved. 21(2 Suppl):157–68. [DOI] [PubMed]