Introduction
Mesohepatectomy is derived from the Greek word Meso = Middle. Hence it is also called by various names as Central Hepatectomy, Central bi-trisegmentectomy, Middle Lobectomy and Middle Hepatic Resection [1]. It is undoubtedly a rare procedure [2] that was, historically, restricted to the resection of hilar cholangiocarcinomas (in order to obtain surgical margins) and for the treatment of biliary strictures [3]. Of late, this technique of mesohepatectomy is being increasingly used for surgical removal of centrally located hepatocellular carcinomas and gall bladder cancers [3]. Mesohepatectomy involves removal of liver segments that are drained by the middle hepatic vein i.e. segments IV, V and VIII.
Case Details
A 54-year old man, non-alcoholic and non-smoker, presented with complaints of pain abdomen since the last 6 months; the pain was in the right upper abdomen, continuous dull aching pain with no relation to food or posture. It was also associated with abdominal distension since 2 months. There was no history of fever, jaundice, vomiting, loose stools or melena.
Examination revealed hepatomegaly 8 cm from the right costal margin, firm in consistency, mildly tender. The liver span was 25 cm. There was no evidence of free fluid in the abdomen. Rest of the examination was found to be normal.
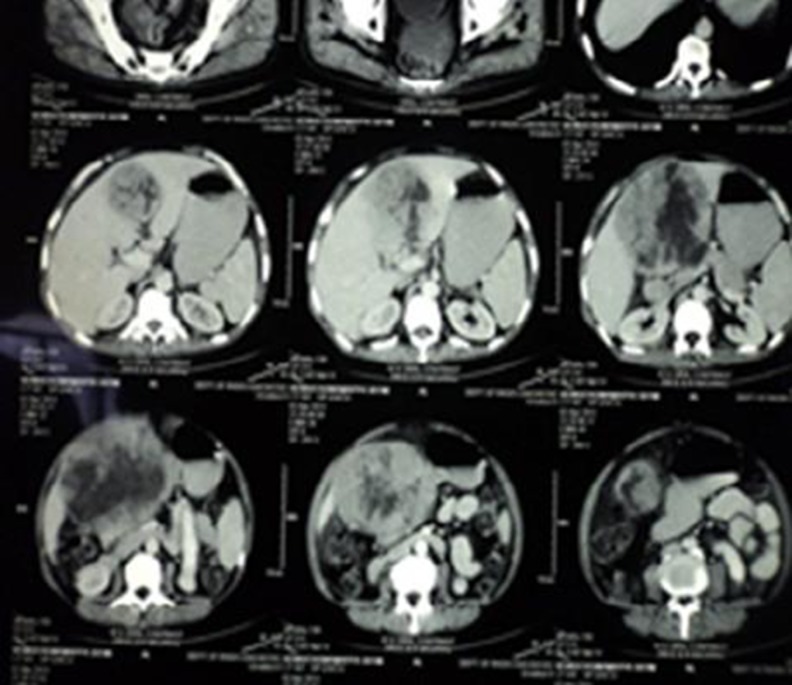
Basic blood investigations were within normal limits. Serum alpha fetoprotein (AFP) was raised measuring 32,300 IU/L. Ultrasound showed moderate hepatomegaly with a heterogeneous mass lesion in the right lobe measuring 11 × 9.8 × 11.5 cm. CT abdomen revealed a large, well defined heterogeneously enhancing mass lesion occupying segments IV, V and VIII of the liver with non-enhancing hypodense areas within it suggestive of necrosis (Fig. 1).
Fig. 1.
CT abdomen showing large necrotic tumor in the liver
A diagnosis of a large centrally located hepatocellular carcinoma was thus made with Child-Pugh grade A.
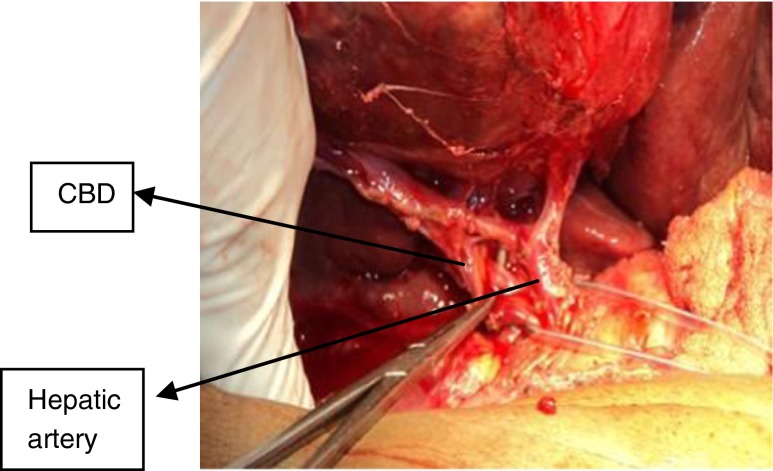
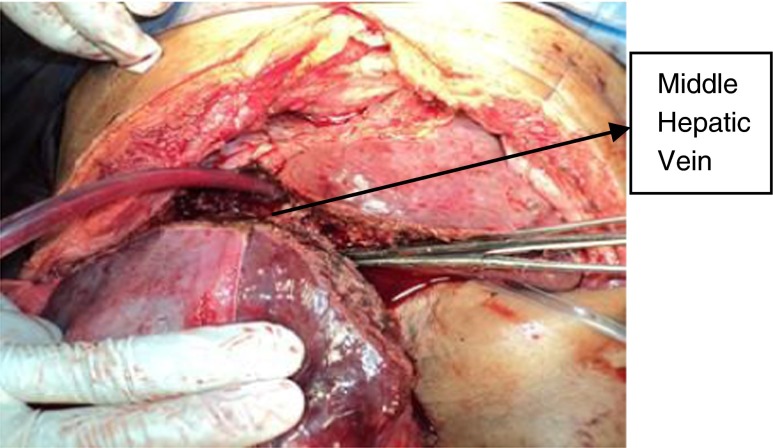
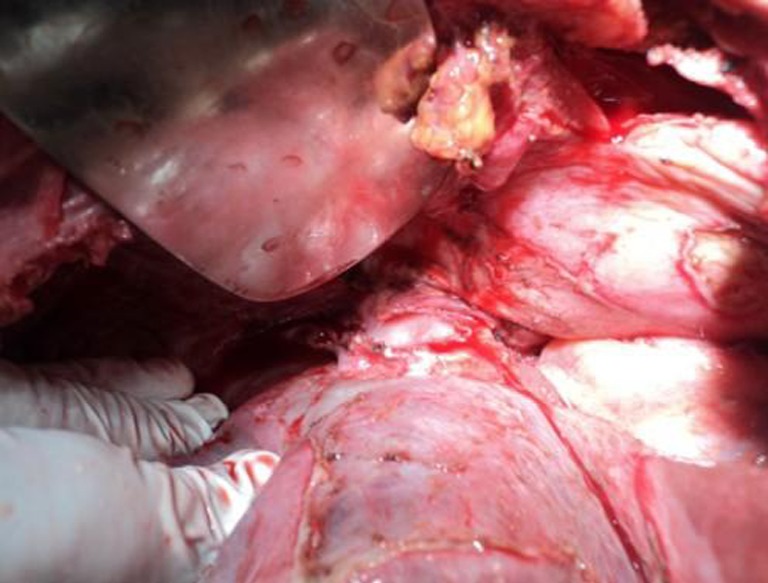
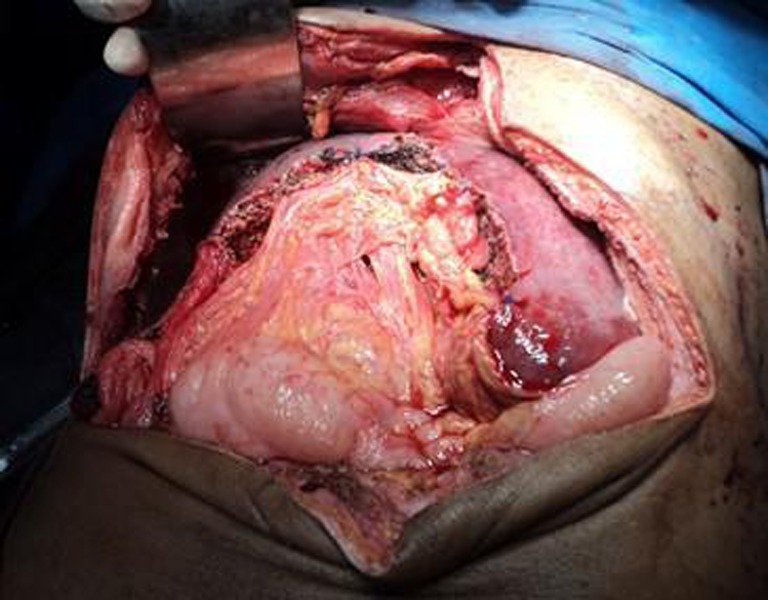
After obtaining the pre-operative fitness, the patient was posted for surgery. The abdomen was opened through a Mercedes Benz incision. Intra-operatively, a large tumour was seen arising from segments IV, V and VIII (Fig. 2). There was no evidence of free fluid in the abdomen. The falciform ligament was divided from the abdominal wall. The liver was mobilized by dividing the coronary and triangular ligaments. The hilum was carefully identified and dissected (Fig. 3). The inflow control was obtained by using intermittent Pringle manoeuvre- 5 min for every 20 min. The supra hepatic inferior vena cava was identified and dissected till the point where the hepatic veins emptied into it (Fig. 4). The middle hepatic vein was dissected and ligated intraparenchymally. In our case, we didn’t use intra-operative ultrasound guidance to isolate the middle hepatic vein. The tumour was removed by a 1 cm margin using Kelly clamps as haemostats (Figs. 5 and 6). The raw area in the liver so created (Fig. 7) was covered by omentum (Fig. 8). Drains were placed and abdomen was closed in layers.
Fig. 2.

Tumour noted in the liver
Fig. 3.
Hilar dissection
Fig. 4.
Supra hepatic IVC exposed
Fig. 5.

Parenchymal transection
Fig. 6.
Middle hepatic vein isolated and divided intra-parenchymally
Fig. 7.

Remnant liver
Fig. 8.
Omental coverage
Post-operative period was uneventful except for a small bile leak which lasted for 5 days and was managed conservatively. The patient was discharged on the tenth post-operative day.
Details
The technique of mesohepatectomy was first described by McBride and Wallace in 1972 [4]. An anatomic mesohepatectomy is performed by the en bloc resection of segments IV, V and VIII while preserving the right posterior and left lateral sectors as well as the caudate lobe (segment I) [4]. This involves resection of hepatic tissue supplied by both the right and left portal pedicles after dividing the middle hepatic vein. The caudate lobe forms the posterior margin of resection [2]. The right and the left hepatic veins are preserved. Then the parenchymal transection begins from either ends until the two planes meet posteriorly in front of the inferior vena cava [2]. Mesohepatectomy has been used as an alternative to extended liver resections because with these resections, the volume of the resected liver accounts for more than 85 % of the whole functioning liver [4].
There are a number of advantages and disadvantages of this technique. The advantages [1, 3–5] include a) parenchymal loss with mesohepatectomy is up to 35 % less than those of extended resections which improves both the functional and anatomical outcomes b) it is oncologically equivalent to extended resections c) it may be combined with hepatic arterial reconstruction d) it is associated with lower rates of complications and shorter post-operative recovery time e) it also increases the chances for a second hepatic resection in case of an isolated recurrent intra hepatic tumour. The disadvantages [1, 4, 6] include a) technically demanding procedure b) the complexity is based on dissection of the hepatic pedicles, double area of raw surface of the liver, proximity to the main hepatic veins and the necessity of preserving the portal pedicles to the remaining segments c) increased risk of bleeding and bile leaks especially for large tumours d) longer liver parenchymal transection time e) the need for biliary reconstruction in selected cases f) in rare case of congenital absence or hypoplasia of the left branch of the portal vein, the technique is not possible g) this technique cannot be recommended when there is inferior vena cava invasion by the tumour.
Of late, mesohepatectomy has been safely performed laparoscopically in selected patients by those who are experienced in both liver surgeries and minimally invasive techniques [7]. Table 1 showing the published studies on Mesohepatectomy is given below.
Table 1.
Studies on mesohepatectomy
| Sl. No | Authors | Journal | Year | Name of study | Numbers |
|---|---|---|---|---|---|
| 1 | Wang Chang-Ming, Song Shi-Bing, Jiang Bin, Jia Yi-Mu, Xiu Dian-Rong, Zhang Tong-Lin | Chinese J Hepatobiliary Surg | 2010 | Mesohepatectomy for treatment of Central Liver Tumors | 3 (Dec 2007–Mar 2009) |
| 2 | Scudamore CH, Buczkowski AK, Shayan H, Ho SGF, Legiehn GM, Chung SW | Am J Surg | 2000 | Mesohepatectomy | 18 |
| 3 | Herman P, Machado MA | Rev. Col. Bras Cir | 2005 | Mesohepatectomy-An alternative to extended liver surgery | 3 |
| 4 | Zhao Hong-Chian, Geng Xiao-Ping, Liu Fu-bao | J Hepatobiliary Surg | 2008 | Clinical study of Mesohepatectomy | 12 (Aug 06–Apr 08) |
| 5 | Lang H, Sotiropoulos GC, Fruhauf NR, RadHce A, Malago M, Broelsch Ch E | Zeitschrift fur alle Gebiete der operative Medizen | 2009 | Mesohepatectomy-An alternative to extended hepatectomy in treatment of central liver tumours | 7 |
| 6 | Mehrabi A, Mood ZA Mood Z | J Am Coll Surg | 2008 | Mesohepatectomy as an option for treatment of central liver tumours | 48 |
| 7 | Takacs I, Furka A, Kovdcs G, Szentkereszty Z, Vagvdlgy A | Hepatogastroenterology | 2007 | Mesohepatectomy without hilar dissection in the treatment of malignant focal liver diseases | 8 (2000–2002) |
| 8 | Xiao-Ping Chen, Fa-Zu Qiu, Wan-Yee Lan, Bi Xiang Zhang, Yi-Fa Chen | Int J of Colorectal Dis | 2008 | Mesohepatectomy for hepatocellular carcinomas | 256 (1996–2005) |
| 9 | Wei-Dong Dai, Ji-Xiong Hu, Xiong-Ying Miao, De-Wu Zhong, Yu-Wen, Sfiou-Zhi Xiong | Hepatogastroenterology | 2008 | Intrahepatic Glissonian Access for Mesohepatectomy in Cirrhotic patients | 17 (Jan 2005–Sep 07) |
Conclusions
Mesohepatectomy is an emerging technique that is found to be efficacious in well circumscribed centrally located tumours of the liver with the added advantage of avoiding unnecessary resection of functioning liver tissue.
References
- 1.Mehrabi A, Mood Z, Fonouni H, Muller S, et al. Mesohepatectomy as an option for the treatment of central liver tumours. J Am Coll Surg. 2008;207:499–509. doi: 10.1016/j.jamcollsurg.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 2.Liau KH, Blumgart LH, Dematteo RP. Segment oriented approach to liver resection. Surg Clin N Am. 2004;84:543–561. doi: 10.1016/j.suc.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 3.LaQuaglia M, Shoster N, Blumgart LH. Central hepatic resection for pediatric tumours. J Pediatr Surg. 2002;37(7):986–989. doi: 10.1053/jpsu.2002.33825. [DOI] [PubMed] [Google Scholar]
- 4.Machado MA, Herman P, Machado MC. Intrahepatic Glissonian approach for pedicle control during anatomic mesohepatectomy. Surgery. 2007;141:533–537. doi: 10.1016/j.surg.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 5.Schudamore CH, Buczkowski AK, Legiehn GM, et al. Mesohepatectomy. Am J Surg. 2000;179:356–360. doi: 10.1016/S0002-9610(00)00374-3. [DOI] [PubMed] [Google Scholar]
- 6.Wu CC, Yeh DC, Yu CL, Cheng SB, et al. Occlusion of hepatic blood inflow for complex central liver resections in cirrhotic patients. Arch Surg. 2002;137:1369–1376. doi: 10.1001/archsurg.137.12.1369. [DOI] [PubMed] [Google Scholar]
- 7.Machado MA, Kalil AN. Glissonian approach for laparoscopic mesohepatectomy. Surg Endosc. 2011;25(6):2020–2022. doi: 10.1007/s00464-010-1483-2. [DOI] [PubMed] [Google Scholar]