Abstract
Laparoscopic Roux-en-Y gastric bypass (LRYGBP) reduces appetite and induces significant and sustainable weight loss. Circulating gut hormones changes engendered by LRYGBP are implicated in mediating these beneficial effects. Laparoscopic sleeve gastrectomy (LSG) is advocated as an alternative to LRYGBP, with comparable short-term weight loss and metabolic outcomes. LRYGBP and LSG are anatomically distinct procedures causing differential entero-endocrine cell nutrient exposure and thus potentially different gut hormone changes. Studies reporting the comparative effects of LRYGBP and LSG on appetite and circulating gut hormones are controversial, with no data to date on the effects of LSG on circulating peptide YY3-36 (PYY3-36) levels, the specific PYY anorectic isoform. In this study, we prospectively investigated appetite and gut hormone changes in response to LRYGBP and LSG in adiposity-matched non-diabetic patients. Anthropometric indices, leptin, fasted and nutrient-stimulated acyl-ghrelin, active glucagon-like peptide-1 (GLP-1), PYY3-36 levels and appetite were determined pre-operatively and at 6 and 12 weeks post-operatively in obese, non-diabetic females, with ten undergoing LRYGBP and eight adiposity-matched females undergoing LSG. LRYGBP and LSG comparably reduced adiposity. LSG decreased fasting and post-prandial plasma acyl-ghrelin compared to pre-surgery and to LRYGBP. Nutrient-stimulated PYY3-36 and active GLP-1 concentrations increased post-operatively in both groups. However, LRYGBP induced greater, more sustained PYY3-36 and active GLP-1 increments compared to LSG. LRYGBP suppressed fasting hunger compared to LSG. A similar increase in post-prandial fullness was observed post-surgery following both procedures. LRYGBP and LSG produced comparable enhanced satiety and weight loss. However, LSG and LRYGBP differentially altered gut hormone profiles.
Keywords: Laparoscopic Roux-en-Y gastric bypass (LRYGBP), Laparoscopic sleeve gastrectomy (LSG), Appetite, Acyl-ghrelin, Peptide YY3-36 (PYY3-36), Active glucagon-like petide-1 (GLP-1)
Introduction
Obesity is a leading cause of morbidity and mortality, placing growing demands on healthcare systems. Bariatric surgery induces significant long-lasting weight loss, ameliorates obesity-associated co-morbidities and reduces mortality [1]. Laparoscopic Roux-en-Y gastric bypass (LRYGBP) is the ‘gold standard’ procedure, resulting in 65–80 % excess bodyweight loss, decreased appetite, and rapid weight-independent amelioration of type-2 diabetes mellitus (T2DM) [2–5]. LRYGBP is cost-effective, but technically challenging with associated mortality—albeit low ∼0.09 % [6]—and micronutrient deficiencies risks, necessitating lifelong follow-up. Laparoscopic sleeve gastrectomy (LSG) (originally undertaken as a first-step in super-obese patients with subsequent conversion to a hybrid restrictive–malabsorptive procedure) is technically less complex, with lower complications and nutritional deficiencies rates than LRYGBP [2]. In light of reports of comparable weight loss and metabolic outcomes to LRYGBP, LSG is increasingly undertaken as a stand-alone procedure [7–10]. However, its long-term efficacy for weight loss and metabolic benefit remains unclear [8, 10].
Understanding the mechanisms mediating the weight loss and metabolic effects of bariatric surgery is key for developing less invasive procedures and medical obesity treatments. Post-operative changes in circulating gut hormones, including ghrelin, peptide YY (PYY) and glucagon-like peptide-1 (GLP-1), are thought to play a key role to the beneficial outcomes of bariatric surgery [2].
Ghrelin is produced by X/A-like cells predominantly located in the stomach fundus and proximal small intestine. Its circulating levels increase with fasting and decrease post-prandially. Acyl-ghrelin, the bioactive form, exerts orexigenic properties and is produced by ghrelin octanoylation in serine-3 mediated by ghrelin-O-acyl transferase (GOAT). Acyl-ghrelin is rapidly converted by endogenous esterases to the main circulating form, des-acyl-ghrelin [11]. Moreover, ghrelin is labile, with highest stability in acidic states [12]. Thus, plasma acyl-ghrelin assessment requires specific sample processing by addition of esterase inhibitor and plasma acidification [13].
GLP-1 and PYY are released post-prandially by distal gut entero-endocrine L-cells [2]. Bioactive forms of GLP-1 augment glucose-dependent insulin release and decrease appetite [2]. Active GLP-1 is rapidly inactivated by the protease di-peptidyl-peptidase-4 (DPP-4). PYY3-36 reduces appetite, bodyweight and adiposity and is produced by truncation of the full-length PYY1-36 by DPP-4 [14]. The effects of PYY1-36 on appetite and feeding are less clear. In rodents, central PYY1-36 administration stimulates feeding [15], whereas equipotent or weaker anorexigenic effects to PYY3-36 have been attributed to peripheral PYY1-36 administration [16, 17]. However, to date, there is no evidence that systemically administered PYY1-36 alters human appetite [18]. Accurate assessment of plasma active GLP-1 and PYY3-36 requires rapid addition of DPP4-inhibitor to samples [13]. Diet-induced weight loss increases ghrelin and reduces PYY, but has little effect on GLP-1 [4, 19, 20], whilst in post-LRYGBP despite the weight loss, ghrelin decreases and marked, weight-independent, increments in nutrient-stimulated plasma PYY and GLP-1 occur [2–5, 21–24].
LRYGBP and LSG differentially alter gastrointestinal anatomy. LRYGBP reduces stomach volume and bypasses the majority of the stomach, duodenum and proximal jejunum, with direct nutrient delivery to the distal gut [2]. In LSG, the gastric fundus (the major source of ghrelin source) is excised, and this accelerates gastric emptying and intestinal transit post-operatively resulting in rapid nutrient delivery to the duodenum and hindgut [25–27]. Thus, LSG and LRYGBP produce differential nutrient exposure of entero-endocrine cells, and as such would be anticipated to differentially alter circulating gut hormones. Most studies comparing the two procedures report larger decreases in circulating fasting and/or meal-stimulated ghrelin after LSG versus LRYGBP [21, 28–30]; however, findings of their effects on hindgut hormones have been inconsistent, reporting either comparable increases in GLP-1 and/or total-PYY [8, 21, 28, 29, 31]; or superior total-PYY [32] and GLP-1 [30] increases post-LRYGBP versus LSG. Technical procedural variations, differences in hormonal isoforms assessed, time-lapse from surgery, subjects’ HOMA-IR and glycaemic status, and differences in subject standardization and sample processing may account for these discrepancies.
Several studies have measured total-ghrelin, total-GLP-1 and/or total-PYY post-surgery, which depict hormone production, but may not necessarily reflect circulating levels of their respective bioactive forms. In support of this, DPP-4 activity declines after LRYGBP [33], whereas GOAT expression is altered by caloric restriction and plasma GOAT is BMI-dependent and thus may change post-bariatric surgery [34–36]. Moreover, the effects of LSG on the anorectic PYY-isoform, PYY3-36, are unknown. Therefore, we prospectively compared the effects of LSG and LRYGBP on anthropometric indices, leptin, acyl-ghrelin, active GLP-1, PYY3-36, and appetite in non-diabetic patients using our established subject standardisation and stringent sample-processing protocols.
Materials and Methods
Subjects
Ten obese non-diabetic females undergoing LRYGBP (age = 46.8 ± 1.5 years, body mass index [BMI] = 45 ± 1.5 kg/m2) and eight adiposity-matched non-diabetic females undergoing LSG (age = 41.4 ± 3.4 years, BMI = 44 ± 1.6 kg/m2) were recruited. Inclusion criteria were female sex (for purpose of sex matching), BMI = 40–50 kg/m2, aged 18–60 years, and undergoing their first bariatric procedure. Exclusion criteria were T2DM, smoking, alcohol consumption >20units/week and intra-operative/ early post-operative complications. Subjects gave written consent, and approval was obtained from University College London Hospitals Ethics Committee (project 09/H0715/65).
Surgical Procedures
LRYGBP included an antecolic–antegastric Roux-en-Y construction with 120-cm alimentary/80-cm biliopancreatic limbs and a small vertical gastric pouch. LSG was performed as previously described [37] and calibrated tightly with a 32-Ch bougie with stapling commenced 5 cm from the pylorus.
Study Protocol
Patients attended for a 500-kcal test meal (43 % carbohydrate/18 % protein/39 % fat) within 2 weeks pre-surgery and at 6 and 12 weeks (6w and 12w) post-operatively. Subjects maintained similar food intake, refrained from alcohol 24 h prior to each study day, fasted from 9 p.m. and drank only water. At ∼9 a.m. on study days, a peripheral cannula was inserted, and 1 h was allowed for recovery/habituation [13]. At t0 min, a baseline visual analogue scale (VAS) [13] and a blood sample were collected. Subjects consumed the test meal (250 ml Resource2.0 + fibre, Nestle Nutrition, Croydon, UK) within 15 min, with blood drawn at t15, t30 and every 30 min thereafter until t180 min post-meal. Coincident with blood sampling, subjects completed appetite VAS [13]. Samples were processed by previously described stringent protocols [13].
Anthropometric Phenotyping
Height was determined by a wall-mounted stadiometer (242 Measuring Rod, Seca, UK), and body composition by multifrequency bioimpedance (InBody_720, Biospace, Derwent Healthcare, UK). Excess weight (EW) was calculated by subtracting ideal bodyweight (based on BMI = 25 kg/m2) from pre-operative bodyweight. Percent excess weight loss (%EWL) was calculated as: [100 × (bodyweight pre-surgery − current bodyweight)/excess weight].
Hormone Assays
To limit inter-assays’ variability, samples were processed simultaneously. Plasma insulin, PYY3-36 and acyl-ghrelin were assayed by radioimmunoassay (assays’ characteristics, respectively: sensitivity 2 μU/mL, 20 pg/mL, 7.8 pg/ml; inter-assay variability, 3.8, 6.6, and 6.8 %; intra-assay variability, 2.6, 4.5, and 5 %). Plasma leptin and active GLP-1 were assayed by ELISA (respectively: sensitivity 0.5 ng/mL, 2 pM; inter-assay variability N/A, 7.5 %; intra-assay variability, 3.2 and 5.2 %) (radioimmunoassays and ELISAs by Millipore, Watford, UK). Plasma glucose was determined by enzymatic colorimetric assay, Infinity™ Glucose Oxidase Reagent (sensitivity 3.3 mmol/L; ThermoFisher, Loughborough, UK). Insulin resistance was calculated using the homeostasis model assessment for insulin resistance, HOMA-IR [38].
Statistical Analysis
Results are expressed as mean ± standard error of the mean. Normal distribution was assessed by D’Agostino-Pearson omnibus normality test. Integrated area-under-the-curve (AUC) t0–t180 for appetite and hormone concentrations versus time was calculated using the trapezoid rule. Non-paired student’s t test was used for between-groups comparisons, and paired student’s t test and repeated measures one-way ANOVA with Bonferroni post-hoc for within-groups’ analysis. p < 0.05 was considered significant.
Results
Preoperative Patient Characteristics
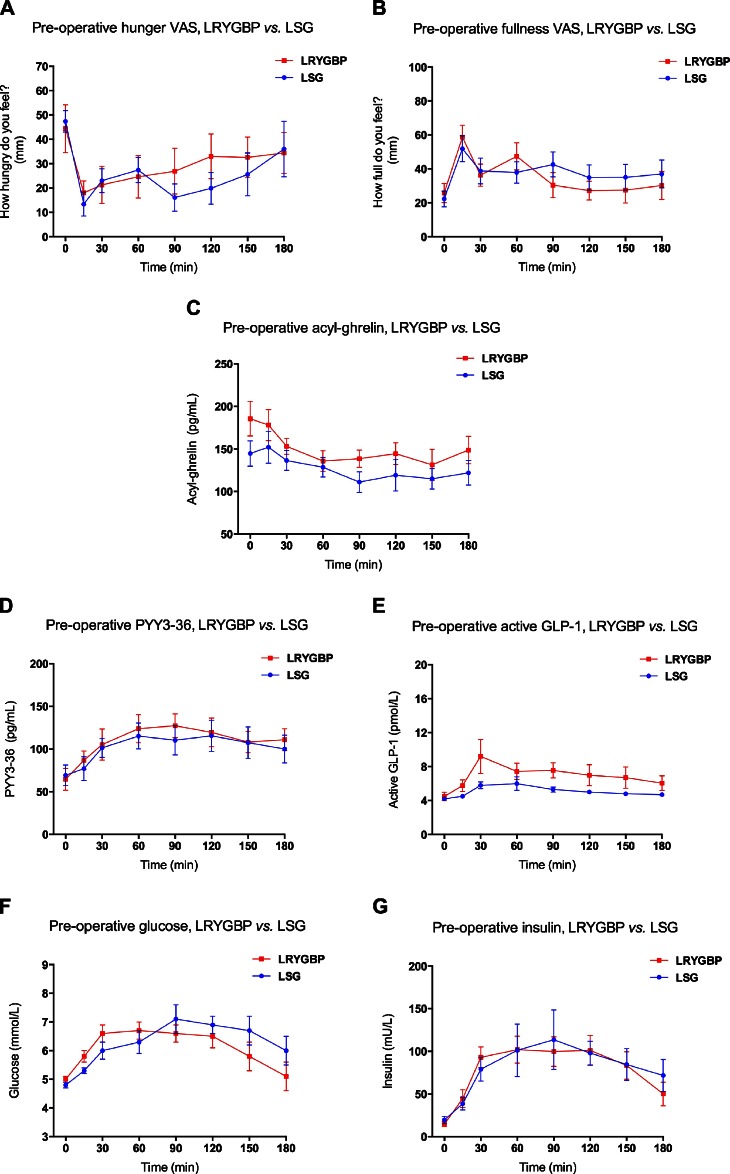
The two groups had comparable age, BMI and adiposity and exhibited similar circulating fasting leptin, acyl-ghrelin, PYY3-36, active GLP-1, glucose, insulin levels and HOMA-IR at baseline (Fig. 1, Tables 1 and 2). In response to the test meal, we observed decreases in hunger and acyl-ghrelin and increases in perceived satiety and in plasma PYY3-36, active GLP-1, glucose, and insulin, with no between-groups differences (Fig. 1, Tables 1 and 2).
Fig. 1.
Fasting and nutrient-stimulated appetite, gut hormones, glucose and insulin for the LRYGBP and LSG groups pre-operatively. (A) Temporal hunger visual analogue scales (VAS) ratings for the LRYGBP (red, filled squares) and LSG (blue, filled circles). (B) Temporal fullness VAS for the LRYGBP (red, filled squares) and LSG (blue, filled circles) groups. (C) Plasma acyl-ghrelin temporal profile for the LRYGBP (red, filled squares) and LSG (blue, filled circles) groups. (D) Plasma PYY3-36 temporal profile for the LRYGBP (red, filled squares) and LSG (blue, filled circles) groups. (E) Plasma active GLP-1 temporal profile for the LRYGBP (red, filled squares) and LSG (blue, filled circles) groups. (F) Plasma glucose temporal profile for the LRYGBP (red, filled squares) and LSG (blue, filled circles) groups. (G) Plasma insulin temporal profile for the LRYGBP (red, filled squares) and LSG (blue, filled circles) groups. Results are expressed as mean ± SEM
Table 1.
Anthropometric characteristics and appetite VAS for the LRYGBP and LSG groups pre-operatively and at 6 and 12 weeks post-surgery (mean ± SEM)
| LRYGBP | LSG | P (between groups) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-operatively | 6 Weeks | 12 Weeks | Pre-operatively | 6 Weeks | 12 Weeks | ||||||||
| Mean ± SEM | Mean ± SEM | p a | Mean ± SEM | p b | Mean ± SEM | p c | Mean ± SEM | p d | p e | p f | p g | ||
| Age | 46.8 ± 1.5 (40–53) | 41.4 ± 3.4 (28–57) | 0.13 | ||||||||||
| Anthropometrics | |||||||||||||
| BMI (kg/m2) | 45 ± 1.5 | 40.2 ± 1.7 | <0.0001 | 37.9 ± 1.6 | <0.0001 | 44 ± 1.6 | 39.6 ± 1.7 | <0.0001 | 37.4 ± 1.7 | <0.0001 | 0.66 | 0.81 | 0.84 |
| Weight loss (kg) | N/A | 12.6 ± 0.8 | N/A | 18.7 ± 0.8 | N/A | N/A | 13.9 ± 2.2 | N/A | 19.9 ± 3.0 | N/A | N/A | 0.56 | 0.67 |
| %EWL (%) | N/A | 27.1 ± 3.6 | N/A | 39.4 ± 3.8 | N/A | N/A | 28.9 ± 5.1 | N/A | 37.8 ± 5.3 | N/A | N/A | 0.77 | 0.81 |
| WHR | 1.13 ± 0.02 | 1.08 ± 0.02 | <0.0001 | 1.05 ± 0.02 | <0.0001 | 1.10 ± 0.02 | 1.05 ± 0.02 | <0.01 | 1.02 ± 0.0 | <0.0001 | 0.30 | 0.37 | 0.22 |
| Total fat mass (kg) | 62 ± 3.3 | 53.7 ± 3.1 | <0.0001 | 49.3 ± 3.2 | <0.0001 | 62.1 ± 3.0 | 54 ± 3.3 | <0.0001 | 49 ± 3.2 | <0.0001 | 0.99 | 0.95 | 0.95 |
| VFA (cm2) | 245 ± 12.1 | 207 ± 10.9 | <0.0001 | 188 ± 11 | <0.0001 | 231 ± 11.8 | 195 ± 13.6 | <0.0001 | 180 ± 13 | <0.0001 | 0.45 | 0.49 | 0.63 |
| Appetite VAS | |||||||||||||
| Fasting hunger (mm) | 44.4 ± 9.8 | 13.4 ± 3.5 | 0.008 | 19.1 ± 8.3 | 0.009 | 47.4 ± 4.4 | 34 ± 11.7 | 0.40 | 53.1 ± 12.3 | 0.70 | 0.80 | 0.08 | 0.03 |
| Hunger AUC0-180 (mm × min) | 5,109 ± 1,335 | 1,385 ± 328 | < 0.05 | 2,588 ± 1033 | 0.07 | 4,282 ± 914 | 1,818 ± 287 | <0.05 | 2,645 ± 388 | 0.06 | 0.63 | 0.35 | 0.96 |
| Fasting fullness (mm) | 26 ± 5.6 | 47 ± 9.6 | 0.06 | 30 ± 9.6 | 0.7 | 22 ± 5.1 | 34 ± 11.6 | 0.47 | 25 ± 9.0 | 0.81 | 0.66 | 0.40 | 0.72 |
| Fullness AUC0-180 (mm × min) | 6,315 ± 729 | 12,592 ± 1050 | <0.01 | 1,102 ± 1,677 | <0.05 | 6,883 ± 1,214 | 13,917 ± 546 | <0.01 | 13,116 ± 546 | <0.001 | 0.68 | 0.32 | 0.31 |
LRYGBP proximal gastric bypass, LSG sleeve gastrectomy, BMI body mass index, EWL excess weight loss, WHR waist to hip ratio, VFA visceral fat area, AUC area-under-the-curve
aSignifies LRYGBP 6w post-surgery versus pre-operatively
bLRYGBP 12w post-surgery versus pre-operatively
cSignifies LSG 6w post-surgery versus pre-operatively
dLSG 12w post-surgery versus pre-operatively
eSignifies LRYGBP versus LSG at pre-surgery
fLRYGBP versus LSG at 6w post-surgery
gLRYGBP versus LSG at 12w post-surgery
Table 2.
Gut hormones and glycaemia indices for the LRYGBP and LSG groups (mean ± SEM)
| LRYGBP | LSG | p (between groups) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-operatively | 6 weeks | 12 weeks | Pre-operatively | 6 weeks | 12 weeks | ||||||||
| Mean ± SEM | Mean ± SEM | p a | Mean ± SEM | p b | Mean ± SEM | Mean ± SEM | p c | Mean ± SEM | p d | p e | p f | p g | |
| Fasting leptin (ng/mL) | 63.3 ± 5.6 | 38.3 ± 4.6 | <0.01 | 33.4 ± 3.6 | <0.001 | 62.4 ± 6.9 | 38.9 ± 5.0 | <0.01 33.4 | ±4.9 | <0.01 | 0.92 | 0.93 | 0.93 |
| Acyl-ghrelin | |||||||||||||
| Fasting acyl-ghrelin (pg/mL) | 186 ± 20.2 | 139 ± 9.0 | 0.06 | 179 ± 16.6 | 0.74 | 145 ± 14.9 | 110 ± 6.3 | <0.05 | 100 ± 6.5 | <0.01 | 0.14 | 0.02 | 0.001 |
| Acyl-ghrelin AUC0-180 (pg × min/mL) | 25,853 ± 2,242 | 23,842 ± 1,104 | 0.38 | 25,144 ± 1,457 | 0.72 | 22,485 ± 2,231 | 18,725 ± 1,275 | 0.08 | 18,234 ± 1,087 | 0.09 | 0.31 | 0.008 | 0.002 |
| PYY3-36 | |||||||||||||
| Fasting PYY3-36 (pg/mL) | 64.6 ± 12.8 | 91.3 ± 12.4 | 0.11 | 90.2 ± 9.2 | 0.11 | 69.4 ± 12 | 74.2 ± 11.3 | 0.57 | 87.8 ± 10.7 | 0.09 | 0.79 | 0.34 | 0.87 |
| PYY3-36 AUC0-180 (pg × min/mL) | 19,794 ± 2,273 | 46,864 ± 3,677 | <0.0001 | 42,177 ± 3,709 | <0.001 | 18,917 ± 2,656 | 30,771 ± 3,528 | <0.01 | 30,186 ± 4,233 | <0.05 | 0.80 | 0.007 | 0.05 |
| Active GLP-1 | |||||||||||||
| Fasting active GLP-1 (pmol/L) | 4.5 ± 0.5 | 5.6 ± 0.9 | 0.18 | 5.8 ± 1.2 | 0.21 | 4.2 ± 0.1 | 4.2 ± .01 | 0.97 | 4.2 ± .01 | 0.88 | 0.62 | 0.20 | 0.25 |
| Active GLP-1 AUC0-180 (pmol × min/L) | 1,279 ± 188 | 6,037 ± 801 | <0.0001 | 5,832 ± 583 | <0.0001 | 933 ± 40 | 2,804 ± 443 | <0.01 | 2,255 ± 328 | <0.05 | 0.13 | 0.005 | 0.0001 |
| Glucose | |||||||||||||
| Fasting glucose (mmol/L) | 5 ± 0.1 | 4.8 ± 0.1 | 0.26 | ||||||||||
| Glucose AUC0-180 (mmol × min/L) | 1,116 ± 44.6 | 1,152 ± 45.9 | 0.58 | ||||||||||
| Insulin | |||||||||||||
| Fasting Insulin (mU/L) | 14.8 ± 2.7 | 19.6 ± 4.3 | 0.34 | ||||||||||
| Insulin AUC0-180 (mU × min/L) | 15,221 ± 2,206 | 15,508 ± 3,324 | 0.94 | ||||||||||
| HOMA-IR | 3.3 ± 0.6 | 4.3 ± 1 | 0.41 | ||||||||||
LRYGBP proximal gastric bypass, LSG sleeve gastrectomy, PYY peptide YY, GLP-1 glucagon-like peptide-1, AUC area-under-the-curve
aSignifies LRYGBP 6w post-surgery versus pre-operatively
bLRYGBP 12w post-surgery versus pre-operatively
cSignifies LSG 6w post-surgery versus pre-operatively
dLSG 12w post-surgery versus pre-operatively
eSignifies LRYGBP versus LSG at pre-surgery
fLRYGBP versus LSG at 6w post-surgery
gLRYGBP versus LSG at 12w post-surgery
Post-surgery Changes in Adiposity and Plasma Leptin
Both procedures induced comparable, marked reductions in BMI, fat mass, visceral fat area (VFA) and fasting leptin, with similar BMI and %EWL observed at 6w and 12w post-surgery (Tables 1 and 2).
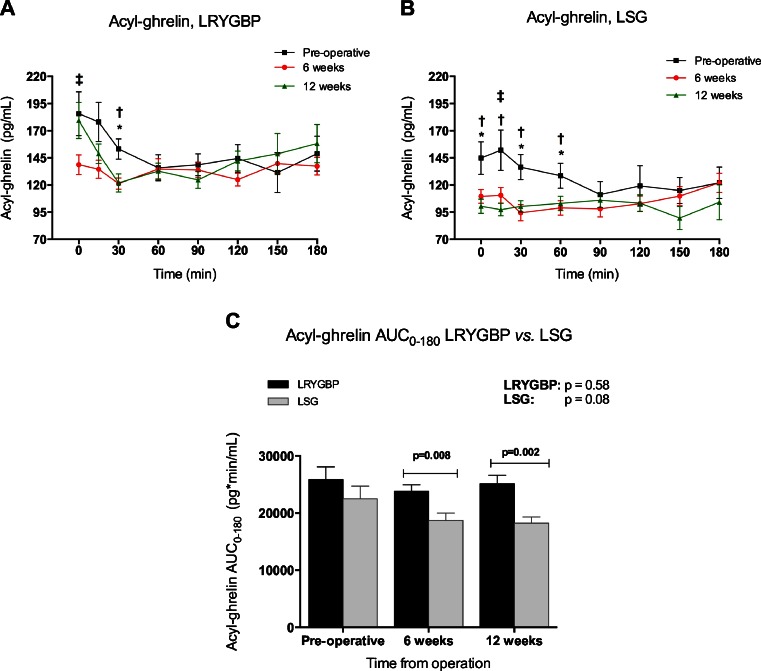
Post-operative Fasting and Nutrient-Stimulated Plasma Acyl-ghrelin Levels
Post-LRYGBP fasting acyl-ghrelin non-significantly decreased at 6w (p = 0.06), but rose towards pre-surgery values by 12w (p = 0.74). Post-meal, plasma acyl-ghrelin levels were reduced compared to pre-surgery at t30 at 6w and 12w post-operatively, whereas acyl-ghrelinAUC0-180 remained unaltered (Fig. 2, Table 2). At both post-LSG visits, lower fasting acyl-ghrelin levels and nutrient-stimulated levels at t30 and t60 were observed, with a trend towards decreased acyl-ghrelinAUC0-180 (p < 0.1) compared to pre-surgery (Table 2). Fasting acyl-ghrelin and acyl-ghrelinAUC0-180 were significantly lower post-LSG versus post-LRYGBP (Fig. 2, Table 2).
Fig. 2.
The effects of LRYGBP and LSG on plasma fasting, meal-stimulated acyl-ghrelin and acyl-ghrelinAUC0–180. Plasma acyl-ghrelin temporal profile in response to the test-meal for LRYGBP (a) and LSG (b) groups at pre-surgery (black, solid squares), and at 6w and 12w post-operatively (red, solid circles and green, solid triangles, respectively). c Acyl-ghrelinAUC0–180 for LRYGBP (black, solid columns) and LSG groups (grey, solid columns) at pre-surgery and at 6w and 12w post-operatively. Results are expressed as mean ± SEM. *p < 0.05, within-group at 6w post-operatively compared to pre-surgery; † p < 0.05, within-group comparisons at 12w post-operatively versus pre-surgery; ‡ p < 0.05, within-group 6w versus 12w comparison. The p values at the right upper corner of c indicate one-way ANOVA within-group analysis. Within-group Bonferroni post hoc and between-group t test significance is indicated over the corresponding bars
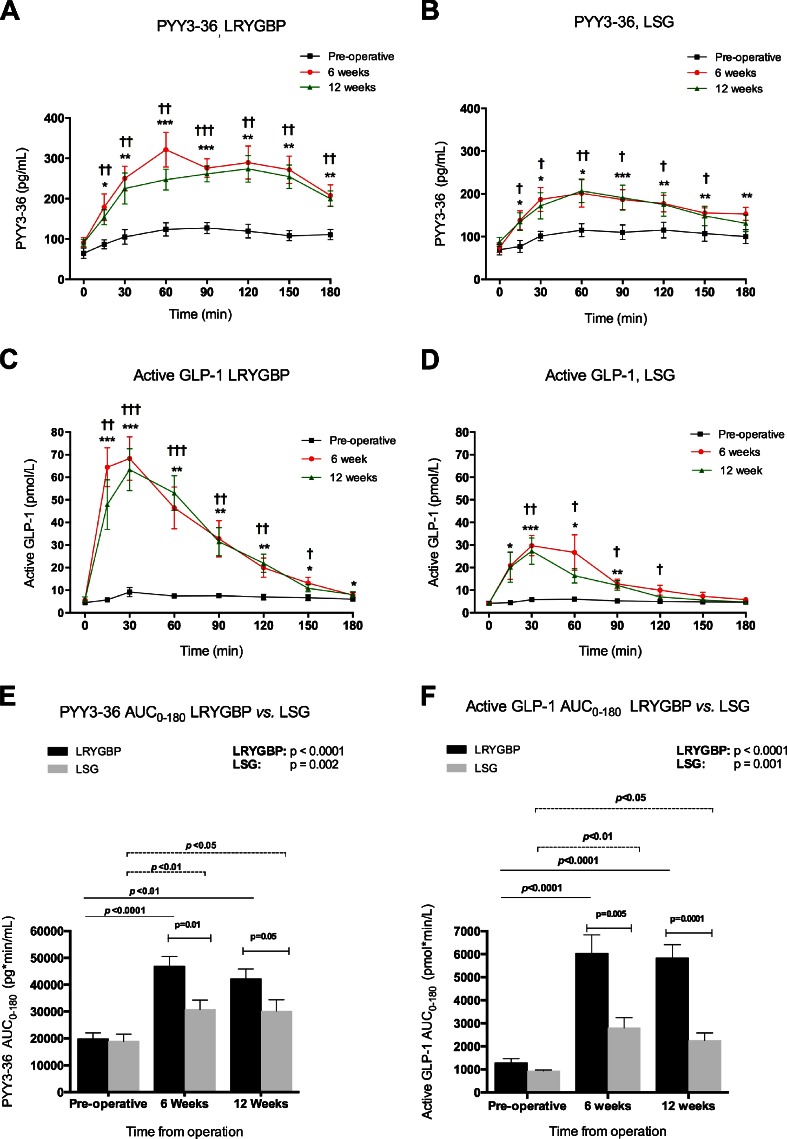
Post-operative Fasting and Nutrient-Stimulated Plasma PYY3-36 and Active GLP-1 Levels
Fasting PYY3-36 and active GLP-1 did not significantly change following either procedure (Fig. 3, Table 2). However, marked augmentation of nutrient-stimulated PYY3-36 and active GLP-1 occurred post-operatively (Fig. 3) (LRYGBP: PYY3-36 6w and 12w: t15–t180, active GLP-1 6w: t15–t180, 12w: t15–t150; LSG: PYY3-36 6w: t15–t180, 12w: t15–t150, active GLP-1 6w: t15–t90, 12w: t30–t120), with associated increases in PYY3-36AUC0-180 and active GLP-1AUC0-180 (Fig. 3, Table 2) (LRYGBP: PYY3-36AUC0–180 6w = ↑2.5 ± 0.2-fold, 12w = ↑2.3 ± 0.3-fold, active GLP-1AUC0–180: 6w&12w = ↑5.1 ± 0.8-fold; LSG: PYY3-36AUC0–180 6w and 12w = ↑1.7 ± 0.2-fold, active GLP-1AUC0–180: 6w = ↑3.1 ± 0.4-fold, 12w = ↑2.4 ± 0.3-fold). The LRYGBP group exhibited significantly higher PYY3-36AUC0-180 and active GLP-1AUC0-180, with higher meal-stimulated levels versus LSG (PYY3-36, 6w: t90–t150, 12w: t120–150; active GLP-1 6w: t15–t30, 12w: t30–t180) (Fig. 3, Table 2).
Fig. 3.
The effects of LRYGBP and LSG on fasting, meal-stimulated plasma concentrations and area-under-the curve (AUC0–180) for PYY3–36 and active GLP-1. Plasma PYY3-36 temporal profile in response to the test-meal for LRYGBP (a) and LSG (b) groups at pre-surgery (black, solid squares) and at 6w and 12w post-operatively (red, solid circles and green, solid triangles, respectively). Plasma active GLP-1 temporal profile in response to the test-meal for LRYGBP (c) and LSG (d) groups at pre-surgery (black, solid squares) and at 6w and 12w post-operatively (red, solid circles and green, solid triangles, respectively). PYY3-36AUC0-180 (e) and active GLP-1AUC0-180 (f) for LRYGBP (black, solid columns) and LSG groups (grey, solid columns) at pre-surgery and at 6w and 12w post-operatively. Results are expressed as mean ± SEM. *p < 0.05, **p < 0.01 and ***p < 0.001 within-group at 6w post-operatively compared to pre-surgery. † p < 0.05, †† p < 0.01 and ††† p < 0.001 for within-group comparisons at 12w post-operatively versus pre-surgery. The p values at the right upper corner of e and f indicate one-way ANOVA within-group analysis. Within-group Bonferroni post hoc and between-group t test significance is indicated over the corresponding bars
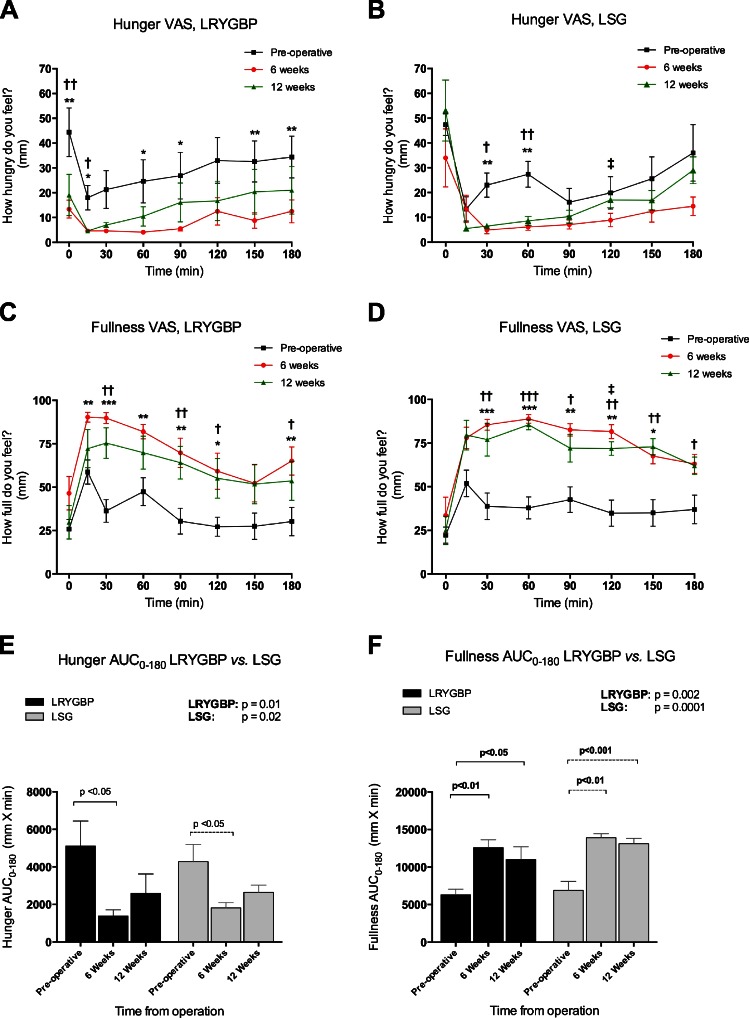
Post-operative Subjective Hunger and Satiety Scores
Fasting hunger significantly decreased post-LRYGBP, but remained unchanged post-LSG. Both procedures comparably reduced hungerAUC0-180 in response to the standard test meal (Fig. 4, Table 2). At 12w, fasting hunger was lower post-LRYGBP versus LSG, with no other between-groups differences in hunger (Fig. 4, Table 2).
Fig. 4.
The effects of LRYGBP and LSG on fasting, meal-stimulated and area-under the curve (AUC0–180) for subjective hunger and fullness VAS ratings. Hunger VAS temporal profile in response to the test-meal for LRYGBP (a) and LSG (b) groups at pre-surgery (black, solid squares), and at 6w and 12w post-operatively (red, solid circles and green, solid triangles, respectively). Fullness VAS temporal profile in response to the test-meal for LRYGBP (c) and LSG (d) groups at pre-surgery (black, solid squares) and at 6w and 12w post-operatively (red, solid circles and green, solid triangles, respectively). HungerAUC0-180 (e) and fullnessAUC0-180 (f) for LRYGBP (black, solid columns) and LSG groups (grey, solid columns) at pre-surgery and at 6w and 12w post-operatively. Results are expressed as mean ± sem. *p < 0.05, **p < 0.01 and ***p < 0.001 within-group at 6w post-operatively compared to pre-surgery. † p < 0.05, †† p < 0.01 and ††† p < 0.001 for within-group comparisons at 12w post-operatively versus pre-surgery. The p values at the right upper corner e and f indicate one-way ANOVA within-group analysis. Within-group Bonferroni post hoc and between-group t test significance is indicated over the corresponding bars
Fasting fullness non-significantly declined at 6w (p = 0.06), but returned to baseline by 12w post-LRYGBP, whereas remained unchanged post-LSG. Both procedures comparably enhanced postprandial fullness (Fig. 4, Table 2).
Discussion
LRYGBP and LSG reduced BMI, excess weight, adiposity and plasma leptin at 6w and 12w post-operatively to a similar extent. Hence, the observed differences in appetite and gut hormones were not attributable to differences in weight loss and more likely reflect differences in the surgical procedures per se.
Our study reports the first comparison of plasma acyl-ghrelin in non-diabetic patients’ post-LRYGBP and LSG. These procedures produce differential nutrient contact with ghrelin-producing X/A-like cells. Post-LRYGBP, X/A-like cells in the gastric fundus and duodenum remain in situ but are excluded from nutrient contact. Diet-induced weight loss increases ghrelin [19]. Yet, despite marked weight loss, post-LRYGBP fasting acyl-ghrelin non-significantly decreased at 6w but rose towards baseline values by 12w, whereas at t30 post-meal declined from pre-surgery at 6w and 12w. Our results suggest that stomach fundus and duodenal ghrelin-producing cells contribute to circulating ghrelin post-LRYGBP despite their exclusion from nutrient contact and that mechanisms independent from X/A-like cell nutrient-sensing, for example the vagus nerve [39], may signal meal-induced ghrelin suppression. Chronaiou et al. provided direct evidence that fundus ghrelin-producing cells remain active post-LRYGBP by demonstrating superior decreases in ghrelin post-LRYGBP + fundus resection versus LRYGBP with fundus preservation [23]. Interestingly Barazzoni et al. reported no change in total ghrelin, but significantly increased acyl-ghrelin at 1, 3, 6 and 12 months post-LRYGBP [24]. Substantial differences in sample handling by addition of esterase inhibitor and plasma acidification in our study may underlie these discrepant findings.
LSG removes gastric fundus ghrelin-producing cells and accelerates nutrient delivery to duodenal ghrelin-producing cells by increasing gastric emptying [25–27]. After LSG, 40–50 % decreases in fasting total-ghrelin have been reported, sustained for up to 5 years post-surgery, with reductions in post-meal circulating ghrelin levels [21, 28, 40]. We also observed reductions in fasting acyl-ghrelin and acyl-ghrelinAUC0-180 post-LSG. Moreover, as anticipated in view of the stomach fundus excision, LSG induced superior acyl-ghrelin reductions than LRYGBP. Interestingly, despite removing the majority of the gastric fundus, fasting acyl-ghrelin and acyl-ghrelinAUC0-180 declined by only ∼20–30 % post-LSG. A possible explanation is that although the majority of ghrelin-producing cells are in the stomach fundus, circulating acyl-ghrelin may primarily originate from the duodenum. Alternatively, plasma acyl-ghrelin is highly regulated, and compensatory up-regulation of duodenal ghrelin-production may occur.
PYY and GLP-1 are released from distal gut L-cells. Post-meal their levels rapidly rise, implicating a yet unknown neural and/or humoral mechanism to this initial release. Subsequent PYY and GLP-1 release results from L-cell nutrient-contact. LRYGBP and LSG increase gastric emptying [25–27, 41] but have different effects on gut nutrient-passage. LRYGBP excludes nutrients from foregut contact and expedites nutrient delivery to distal gut L-cells, which is suggested to augment hindgut hormone release; the ‘hindgut theory’. LSG accelerates gastric emptying, reduces acid production and rapidly transits nutrients into the duodenum and proximal intestine, enhancing foregut stimulation [2]. Few studies have examined the effects of LRYGBP on circulating PYY3-36, the anorectic PYY-isoform. This is the first report of plasma PYY3-36 post-LSG. LRYGBP and LSG markedly enhanced nutrient-stimulated PYY3-36, with, however, greater, more sustained post-prandial PYY3-36 release post-LRYGBP. These findings are in keeping with the procedural anatomical differences and suggest that factors originating from foregut and hindgut regulate PYY3-36 levels. Our findings of superior PYY3-36 enhancement post-LRYGBP versus LSG are in accord with those of Valderas et al. for total-PYY [32]. However, they are at odds with reports of comparable post-prandial total-PYY following LRYGBP and LSG [21, 29, 31]. Differences in PYY-isoforms assessed, sampling time-points, subject standardization, sample handling and in subjects’ HOMA-IR pre-surgery may account for these discrepancies.
Similarly to PYY3-36, both procedures augmented nutrient-stimulated active GLP-1 levels, with again greater, more sustained release observed post-LRYGBP. These findings are at odds with reports by Chambers et al. of similar increases in nutrient-stimulated active GLP-1 post-sleeve gastrectomy and gastric bypass in rats [8]. These discrepancies may be accounted for by structural inter-species rodent-human stomach differences, which potentially affect gastric emptying post-surgery and hence gut hormone responses. Moreover, Chambers and colleagues measured active GLP-1 5 months post-surgery in weight-stable rats, whilst our studies were undertaken during the acute weight-loss phase. Peterli et al. have reported greater meal-stimulated active GLP-1 responses at 1 week and non-significant increases 12 weeks post-LRYGBP versus LSG [21]. In another study, they showed non-significantly greater active GLP-1 peak and active GLP-1AUC following LRYGBP [29]. Again, methodological and subject-related differences may underlie these discrepancies.
Despite greater reductions in the ‘hunger hormone’ acyl-ghrelin post-LSG versus post-LRYGBP, paradoxically the LRYGBP group exhibited lower fasting hunger; post-prandial hunger was reduced comparably by both procedures. We also observed similar post-operative increments in nutrient-stimulated fullness perception in both groups. These findings again are slightly at odds with the accepted notion that PYY3-36 and active GLP-1 mediate satiety, as LRYGBP induced superior increases of these anorectic peptides and thus would be expected to result in greater satiety perception. These findings highlight that additional factors to active GLP-1 and PYY3-36 regulate satiety.
The novel finding of our study is the characterisation for the first time of the effects of LSG on circulating levels of the anorectic PYY-isoform, PYY3-36. Moreover, our study is the first to simultaneously measure bioactive forms of ghrelin, PYY and GLP-1 in the same patient cohort, while concurrently undertaking parallel appetite assessment. The main strength of our study is the use of validated subject-standardisation protocols, stringent sample processing [13], and tight group-matching pre-operatively for the gut hormone confounders age [42], sex [43] and adiposity [44]. Furthermore, we studied patients without T2DM, dissecting out confounding effects of T2DM on the incretin effect [45], circulating PYY3-36 [5] and ghrelin [46]. The limitations of our study are our small sample sizes, non-randomization and limited follow-up. We studied females only as these represent the majority of patients undergoing bariatric surgical procedures in the UK, and future studies are needed to assess whether gender differences exist in post-operative gut hormone changes. Moreover, studies in patients with T2DM are required to examine whether their inferior weight-loss outcome post-bariatric surgery [47] results from altered/aberrant gut hormone responses. Future larger, randomised studies with longitudinal assessment of gut hormones, intestinal transit, glycaemic and anthropometric indices are required to further elucidate the mechanisms underlying the beneficial effects of LRYGBP and LSG in an attempt to develop novel, less invasive surgical and non-surgical T2DM and obesity treatments.
Acknowledgments
We are indebted to our patients who participated in this study. We thank all the members of the UCLH Bariatric Group, past and present. This work was supported by the Rosetrees Trust, Medical Research Council, UCLH Charities and UCL/UCLH Comprehensive Biomedical Research Centre who received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centres funding scheme
Conflict of Interest
All authors declare no conflict of interest.
Footnotes
Ahmed Yousseif and Julian Emmanuel contributed equally.
References
- 1.Sjostrom L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65. doi: 10.1001/jama.2011.1914. [DOI] [PubMed] [Google Scholar]
- 2.Scott WR, Batterham RL. Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: understanding weight loss and improvements in type 2 diabetes after bariatric surgery. Am J Physiol Regul Integr Comp Physiol. 2011;301:R15–R27. doi: 10.1152/ajpregu.00038.2011. [DOI] [PubMed] [Google Scholar]
- 3.Morinigo R, Moize V, Musri M, et al. Glucagon-like peptide-1, peptide YY, hunger, and satiety after gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab. 2006;91:1735–1740. doi: 10.1210/jc.2005-0904. [DOI] [PubMed] [Google Scholar]
- 4.Laferrere B. Effect of gastric bypass surgery on the incretins. Diabetes Metab. 2009;35:513–517. doi: 10.1016/S1262-3636(09)73458-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olivan B, Teixeira J, Bose M, et al. Effect of weight loss by diet or gastric bypass surgery on peptide YY3-36 levels. Ann Surg. 2009;249:948–953. doi: 10.1097/SLA.0b013e3181a6cdb0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gould JC, Kent KC, Wan Y, et al. Perioperative safety and volume: outcomes relationships in bariatric surgery: a study of 32,000 patients. J Am Coll Surg. 2011;213:771–777. doi: 10.1016/j.jamcollsurg.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Deitel M, Gagner M, Erickson AL, et al. Third international summit: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:749–759. doi: 10.1016/j.soard.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Chambers AP, Jessen L, Ryan KK, et al. Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141:950–958. doi: 10.1053/j.gastro.2011.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paluszkiewicz R, Kalinowski P, Wroblewski T, et al. Prospective randomized clinical trial of laparoscopic sleeve gastrectomy versus open Roux-en-Y gastric bypass for the management of patients with morbid obesity. Wideochir Inne Tech Malo Inwazyjne. 2012;7:225–232. doi: 10.5114/wiitm.2012.32384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vidal P, Ramon JM, Goday A, et al. Laparoscopic gastric bypass versus laparoscopic sleeve gastrectomy as a definitive surgical procedure for morbid obesity. Mid-term results, Obes Surg. 2013;23:292–299. doi: 10.1007/s11695-012-0828-4. [DOI] [PubMed] [Google Scholar]
- 11.Hillman JB, Tong J, Tschop M. Ghrelin biology and its role in weight-related disorders. Discov Med. 2011;11:521–528. [PubMed] [Google Scholar]
- 12.Hosoda H, Doi K, Nagaya N, et al. Optimum collection and storage conditions for ghrelin measurements: octanoyl modification of ghrelin is rapidly hydrolyzed to desacyl ghrelin in blood samples. Clin Chem. 2004;50:1077–1080. doi: 10.1373/clinchem.2003.025841. [DOI] [PubMed] [Google Scholar]
- 13.Chandarana K, Drew ME, Emmanuel J, et al. Subject standardization, acclimatization, and sample processing affect gut hormone levels and appetite in humans. Gastroenterology. 2009;136:2115–2126. doi: 10.1053/j.gastro.2009.02.047. [DOI] [PubMed] [Google Scholar]
- 14.Batterham RL, Heffron H, Kapoor S, et al. Critical role for peptide YY in protein-mediated satiation and body-weight regulation. Cell Metab. 2006;4:223–233. doi: 10.1016/j.cmet.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Batterham RL, Bloom SR. The gut hormone peptide YY regulates appetite. Ann N Y Acad Sci. 2003;994:162–168. doi: 10.1111/j.1749-6632.2003.tb03176.x. [DOI] [PubMed] [Google Scholar]
- 16.Nadkarni PP, Costanzo RM, Sakagami M. Pulmonary delivery of peptide YY for food intake suppression and reduced body weight gain in rats. Diabetes Obes Metab. 2011;13:408–417. doi: 10.1111/j.1463-1326.2011.01363.x. [DOI] [PubMed] [Google Scholar]
- 17.Chelikani PK, Haver AC, Reidelberger RD. Intravenous infusion of peptide YY(3-36) potently inhibits food intake in rats. Endocrinology. 2005;146:879–888. doi: 10.1210/en.2004-1138. [DOI] [PubMed] [Google Scholar]
- 18.Sloth B, Holst JJ, Flint A, et al. Effects of PYY1-36 and PYY3-36 on appetite, energy intake, energy expenditure, glucose and fat metabolism in obese and lean subjects. Am J Physiol Endocrinol Metab. 2007;292:E1062–E1068. doi: 10.1152/ajpendo.00450.2006. [DOI] [PubMed] [Google Scholar]
- 19.Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597–1604. doi: 10.1056/NEJMoa1105816. [DOI] [PubMed] [Google Scholar]
- 20.Valderas JP, Irribarra V, Rubio L, et al. Effects of sleeve gastrectomy and medical treatment for obesity on glucagon-like peptide 1 levels and glucose homeostasis in non-diabetic subjects. Obes Surg. 2011;21:902–909. doi: 10.1007/s11695-011-0375-4. [DOI] [PubMed] [Google Scholar]
- 21.Peterli R, Wolnerhanssen B, Peters T, et al. Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a prospective randomized trial. Ann Surg. 2009;250:234–241. doi: 10.1097/SLA.0b013e3181ae32e3. [DOI] [PubMed] [Google Scholar]
- 22.Morinigo R, Vidal J, Lacy AM, et al. Circulating peptide YY, weight loss, and glucose homeostasis after gastric bypass surgery in morbidly obese subjects. Ann Surg. 2008;247:270–275. doi: 10.1097/SLA.0b013e31815f6e77. [DOI] [PubMed] [Google Scholar]
- 23.Chronaiou A, Tsoli M, Kehagias I, et al. Lower ghrelin levels and exaggerated postprandial peptide-YY, glucagon-like peptide-1, and insulin responses, after gastric fundus resection, in patients undergoing Roux-en-Y gastric bypass: a randomized clinical trial. Obes Surg. 2012;22:1761–1770. doi: 10.1007/s11695-012-0738-5. [DOI] [PubMed] [Google Scholar]
- 24.R. Barazzoni, A. Semolic, M.R. Cattin, M. Zanetti, G. Guarnieri. Acylated ghrelin limits fat accumulation and improves redox state and inflammation markers in the liver of high-fat-fed rats. Obesity (Silver Spring). 2013. [DOI] [PubMed]
- 25.Melissas J, Daskalakis M, Koukouraki S, et al. Sleeve gastrectomy-a “food limiting” operation. Obes Surg. 2008;18:1251–1256. doi: 10.1007/s11695-008-9634-4. [DOI] [PubMed] [Google Scholar]
- 26.Baumann T, Kuesters S, Grueneberger J, et al. Time-resolved MRI after ingestion of liquids reveals motility changes after laparoscopic sleeve gastrectomy–preliminary results. Obes Surg. 2011;21:95–101. doi: 10.1007/s11695-010-0317-6. [DOI] [PubMed] [Google Scholar]
- 27.J. Melissas, A. Leventi, I. Klinaki, et al. Alterations of global gastrointestinal motility after sleeve gastrectomy: a prospective study. Annals of Surgery. 2012. [DOI] [PubMed]
- 28.Karamanakos SN, Vagenas K, Kalfarentzos F, et al. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247:401–407. doi: 10.1097/SLA.0b013e318156f012. [DOI] [PubMed] [Google Scholar]
- 29.Peterli R, Steinert RE, Woelnerhanssen B, et al. Metabolic and Hormonal Changes After Laparoscopic Roux-en-Y Gastric Bypass and Sleeve Gastrectomy: a Randomized. Obes Surg: Prospective Trial; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramon JM, Salvans S, Crous X, et al. Effect of Roux-en-Y gastric bypass vs sleeve gastrectomy on glucose and gut hormones: a prospective randomised trial. J Gastrointest Surg. 2012;16:1116–1122. doi: 10.1007/s11605-012-1855-0. [DOI] [PubMed] [Google Scholar]
- 31.F. Romero, J. Nicolau, L. Flores, R. Casamitjana, A. Ibarzabal, A. Lacy, J. Vidal, Comparable early changes in gastrointestinal hormones after sleeve gastrectomy and Roux-En-Y gastric bypass surgery for morbidly obese type 2 diabetic subjects, Surg Endosc, (2012) [DOI] [PubMed]
- 32.Valderas JP, Irribarra V, Boza C, et al. Medical and surgical treatments for obesity have opposite effects on peptide YY and appetite: a prospective study controlled for weight loss. J Clin Endocrinol Metab. 2010;95:1069–1075. doi: 10.1210/jc.2009-0983. [DOI] [PubMed] [Google Scholar]
- 33.Alam ML, Van der Schueren BJ, Ahren B, et al. Gastric bypass surgery, but not caloric restriction, decreases dipeptidyl peptidase-4 activity in obese patients with type 2 diabetes. Diabetes Obes Metab. 2011;13:378–381. doi: 10.1111/j.1463-1326.2011.01358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirchner H, Gutierrez JA, Solenberg PJ, et al. GOAT links dietary lipids with the endocrine control of energy balance. Nat Med. 2009;15:741–745. doi: 10.1038/nm.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonzalez CR, Vazquez MJ, Lopez M, et al. Influence of chronic undernutrition and leptin on GOAT mRNA levels in rat stomach mucosa. J Mol Endocrinol. 2008;41:415–421. doi: 10.1677/JME-08-0102. [DOI] [PubMed] [Google Scholar]
- 36.Goebel-Stengel M, Hofmann T, Elbelt U, et al. The ghrelin activating enzyme ghrelin-O-acyltransferase (GOAT) is present in human plasma and expressed dependent on body mass index. Peptides. 2013;43:13–19. doi: 10.1016/j.peptides.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 37.Gagner M, Deitel M, Kalberer TL, et al. The second international consensus summit for sleeve gastrectomy. Surg Obes Relat Dis. 2009;5:476–485. doi: 10.1016/j.soard.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 38.Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 39.Sundbom M, Holdstock C, Engstrom BE, et al. Early changes in ghrelin following Roux-en-Y gastric bypass: influence of vagal nerve functionality? Obes Surg. 2007;17:304–310. doi: 10.1007/s11695-007-9056-8. [DOI] [PubMed] [Google Scholar]
- 40.Bohdjalian A, Langer FB, Shakeri-Leidenmuhler S, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20:535–540. doi: 10.1007/s11695-009-0066-6. [DOI] [PubMed] [Google Scholar]
- 41.Falken Y, Hellstrom PM, Holst JJ, et al. Changes in glucose homeostasis after Roux-en-Y gastric bypass surgery for obesity at day three, two months, and one year after surgery: role of gut peptides. J Clin Endocrinol Metab. 2011;96:2227–2235. doi: 10.1210/jc.2010-2876. [DOI] [PubMed] [Google Scholar]
- 42.Rigamonti AE, Agosti F, Compri E, et al. Anorexigenic postprandial responses of PYY and GLP1 to slow ice cream consumption: preservation in obese adolescents, but not in obese adults. Eur J Endocrinol. 2013;168:429–436. doi: 10.1530/EJE-12-0867. [DOI] [PubMed] [Google Scholar]
- 43.Kim BJ, Carlson OD, Jang HJ, et al. Peptide YY is secreted after oral glucose administration in a gender-specific manner. J Clin Endocrinol Metab. 2005;90:6665–6671. doi: 10.1210/jc.2005-0409. [DOI] [PubMed] [Google Scholar]
- 44.Neary MT, Batterham RL. Gut hormones: implications for the treatment of obesity. Pharmacol Ther. 2009;124:44–56. doi: 10.1016/j.pharmthera.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 45.Nauck M, Stockmann F, Ebert R, et al. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia. 1986;29:46–52. doi: 10.1007/BF02427280. [DOI] [PubMed] [Google Scholar]
- 46.Katsuki A, Urakawa H, Gabazza EC, et al. Circulating levels of active ghrelin is associated with abdominal adiposity, hyperinsulinemia and insulin resistance in patients with type 2 diabetes mellitus. Eur J Endocrinol. 2004;151:573–577. doi: 10.1530/eje.0.1510573. [DOI] [PubMed] [Google Scholar]
- 47.Campos GM, Rabl C, Mulligan K, et al. Factors associated with weight loss after gastric bypass. Arch Surg. 2008;143:877–883. doi: 10.1001/archsurg.143.9.877. [DOI] [PMC free article] [PubMed] [Google Scholar]