Abstract
Objectives
We previously developed a model for projection of heat-related mortality attributable to climate change. The objective of this paper is to improve the fit and precision of and examine the robustness of the model.
Methods
We obtained daily data for number of deaths and maximum temperature from respective governmental organizations of Japan, Korea, Taiwan, the USA, and European countries. For future projection, we used the Bergen climate model 2 (BCM2) general circulation model, the Special Report on Emissions Scenarios (SRES) A1B socioeconomic scenario, and the mortality projection for the 65+-year-old age group developed by the World Health Organization (WHO). The heat-related excess mortality was defined as follows: The temperature–mortality relation forms a V-shaped curve, and the temperature at which mortality becomes lowest is called the optimum temperature (OT). The difference in mortality between the OT and a temperature beyond the OT is the excess mortality. To develop the model for projection, we used Japanese 47-prefecture data from 1972 to 2008. Using a distributed lag nonlinear model (two-dimensional nonparametric regression of temperature and its lag effect), we included the lag effect of temperature up to 15 days, and created a risk function curve on which the projection is based. As an example, we perform a future projection using the above-mentioned risk function. In the projection, we used 1961–1990 temperature as the baseline, and temperatures in the 2030s and 2050s were projected using the BCM2 global circulation model, SRES A1B scenario, and WHO-provided annual mortality. Here, we used the “counterfactual method” to evaluate the climate change impact; For example, baseline temperature and 2030 mortality were used to determine the baseline excess, and compared with the 2030 excess, for which we used 2030 temperature and 2030 mortality. In terms of adaptation to warmer climate, we assumed 0 % adaptation when the OT as of the current climate is used and 100 % adaptation when the OT as of the future climate is used. The midpoint of the OTs of the two types of adaptation was set to be the OT for 50 % adaptation.
Results
We calculated heat-related excess mortality for 2030 and 2050.
Conclusions
Our new model is considered to be better fit, and more precise and robust compared with the previous model.
Keywords: Heat-related mortality, Excess deaths, Climate change, Projection, Adaptation
Introduction
In 2002, the World Health Organization reported for the first time the health impact of climate change [1]. In the report, however, heat-related impact was not included in the final aggregate total number, because it was not easy to model the relationship between ambient temperature and mortality for projecting future impact of climate change.
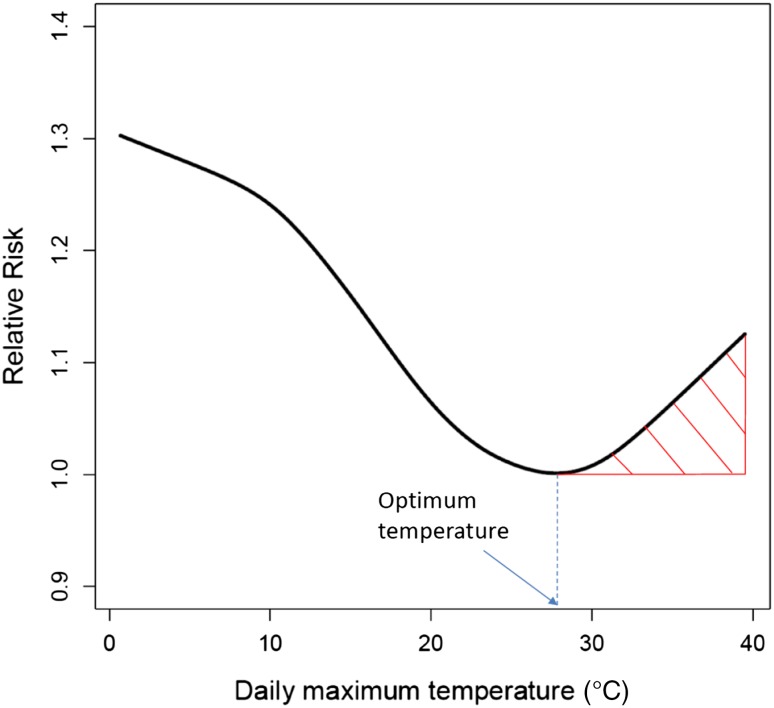
One of the reasons for not being able to construct the model was as follows: In many places of the world, a V-shaped temperature–mortality relation was observed [2, 3]. Using this relation, heat-related excess mortality can be defined as the shaded area in Fig. 1 (where the V-shaped relation was constructed from data for Tokyo from 1972 to 2008). So, if we can identify the optimum temperature (OT), at which the mortality risk becomes smallest, we should be able to estimate the excess mortality with some additional information (as described later). Although the OT level was found to be higher for warmer areas [4, 5], no good index to estimate the OT had been available.
Fig. 1.
Heat-related excess mortality, considered as the shaded area; the figure shows an example using data for Tokyo Prefecture for 1972–2008
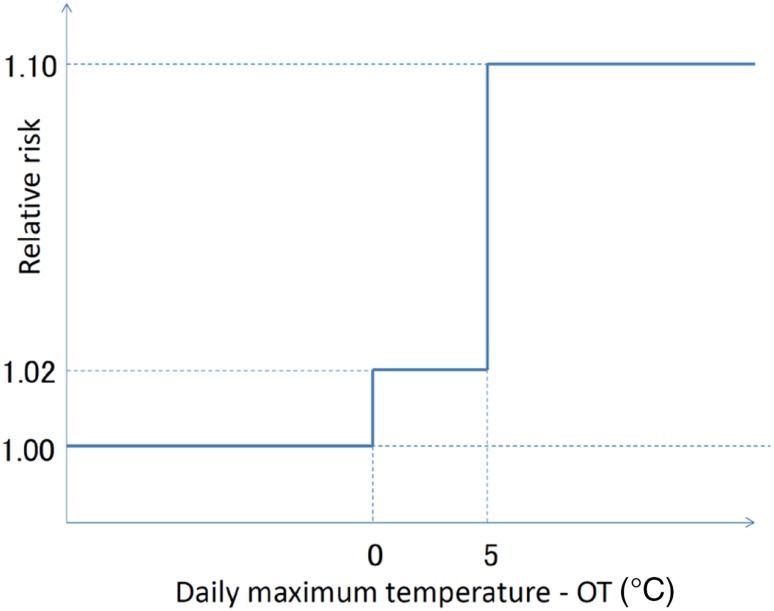
In 2007, we found that the optimum temperature can be estimated using the 80–85th percentile of daily maximum temperature based on 47 prefectures in Japan [6]. Using this estimation method and a risk function model, we projected excess mortality due to heat [7]. The projection method can be summarized as follows: The observation period was 24 years (1972–1995), and we used males and females with all ages combined. The OT was the 85th percentile value of daily maximum temperature. Although the risk function of excess mortality due to heat is nonlinear as shown in Fig. 1, we used the categorical function shown in Fig. 2. In this projection, we do not even show a confidence interval.
Fig. 2.
Risk function of excess mortality due to heat used in the previous projection
Although the above projection was one of the first projections of climate change impact on heat-related mortality, there were some weaknesses to the method, including (1) the applicability of the OT estimation method to other regions of the world, and (2) that the risk function was categorical. In this paper, we solve problem (2) by using a nonparametric risk function. This should be a substantial improvement, because the average of the temperatures in the highest temperature category was actually very close to the lower boundary of the category and huge underestimation was expected for the risk of this category. Regarding problem (1), we examine in this paper the applicability using cities in Korea, Taiwan, Europe, and the USA as well as 47 Japanese prefectures.
Another concern is the temporal pattern of exposure–mortality effects. This can be regarded in two ways [8]. One is the carry-over effect (lag effect), and the other is mortality displacement or harvesting. The former effect has been considered not to last long for heat-related mortality. In the latter case, heat just kills people who would die in a very short period of time anyway, and avoiding heat would extend the lives of people for only a short period of time. In the case of the 2003 heat wave in Europe, however, there was little evidence of mortality displacement [9]. Here, we address this lag effect using a distributed lag nonlinear model developed by Armstrong [8].
Materials and methods
Meteorological data and mortality data were obtained from respective governmental organizations of Japan, Korea, Taiwan, and European countries. For the USA, we downloaded the National Morbidity, Mortality, and Air Pollution Study (NMMAPS) files (which used to be downloadable at http://www.ihapss.jhsph.edu/data/data.htm, but are no longer available) [10]. Some descriptive information for the mortality data is presented in Table 1; because heat-related impact in occupational setting was also included in the new WHO project, we restricted mortality to 65+ years of age.
Table 1.
Description of mortality data by country
| Country/region | Observation period | Age category | Note |
|---|---|---|---|
| Japan | 1972–2008 | 65+ | 47 prefectures, 1973–2008 for Okinawa |
| Korea | 1992–2010 | 65+ | 6 cities |
| Taiwan | 1994–2007 | 65+ | 3 cities |
| USA | 1987–2000 | 65+ | 20 cities |
| Spain | 1992–2000 | All ages | Barcelona |
| France | 1991–1998 | All ages | Paris |
| Italy | 1992–2000 | All ages | Rome |
A set of mortality projections for the 2030s and 2050s was developed for this project by the World Health Organization. The approach built upon previous methods developed by Mathers and Loncar [11]. The method uses a series of regression equations that quantify the current and historical relationships between mortality and a set of independent variables. The major independent variables that were shown to be structurally related to mortality were (i) gross domestic product (GDP)/capita, (ii) years of education, and (iii) time, which is assumed to be a proxy for health benefits arising from technological developments. In addition, specific assumptions are made regarding future patterns of human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), tuberculosis, malaria, smoking, and body mass index (BMI).
Development of the new risk function
We developed the risk function based on all 47 prefectures in Japan. Then, we examined the applicability of the assumptions in combining these 47 prefectures described below. For this purpose, we used the data for the selected cities in Korea, Taiwan, the USA, and Europe. We did not include data other than from Japan, because, although these cities somewhat represent large cities in each region, the data are not systematically collected and are not suitable for calculating average values.
Applicability of OT estimation method
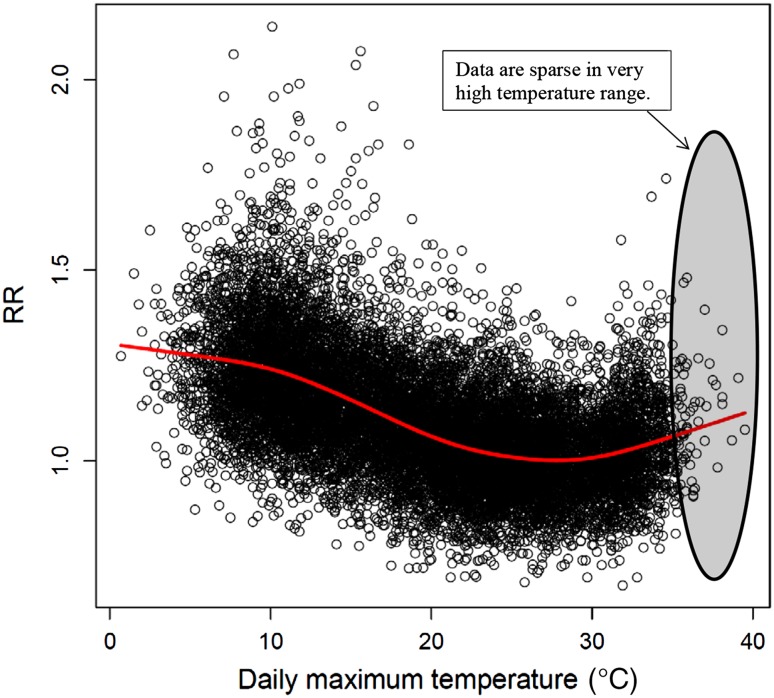
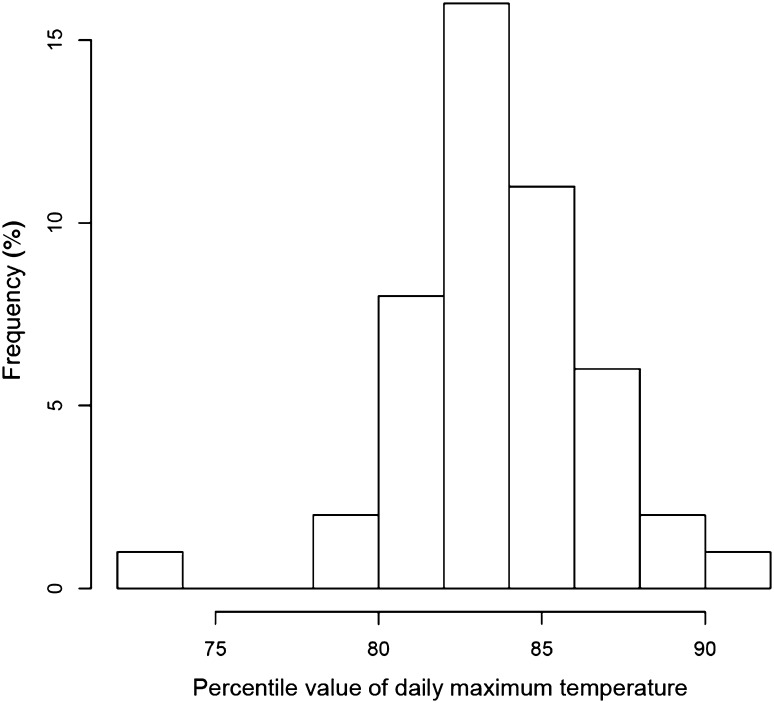
We obtained OT estimates for 47 prefectures in Japan using a smoothing spline with six degrees of freedom. As shown in Fig. 3, data points in the very hot range, especially beyond 35 °C, are sparse. Figure 4 shows the distribution of percentile values that correspond to the OT. In most cases, the value was around the 84th percentile. The mean of all the 47 prefectures was the 83.6th percentile, and we used this value to estimate the OT.
Fig. 3.
Relation between daily maximum temperature and relative risk (RR) in Tokyo, 1972–2008
Fig. 4.
Distribution of optimum temperature (expressed as percentile value of daily maximum temperature) in Japan
Table 2 presents the OT and 84th percentile value of daily maximum temperature in the cities of the other countries examined in this study. The OTs and 84th percentile values were close to each other in a majority of the cities. There were 3 US cities (Dallas/Fort Worth, Houston, and San Diego) that did not show a V-shaped relation. These 3 cities are located in the south, and it is possible to speculate that air-conditioned houses are very popular in these hot cities such that residents of these cities have adapted to heat exposure. However, other southern cities showed a V-shaped relation, even when the OT was higher than 40 °C. Also, in many mid- to southern Japanese prefectures, more than 90 % of households are equipped with air-conditioners (based on the 2009 National Survey of Family Income and Expenditure, for example), but these prefectures still showed V-shaped temperature–mortality relations. Hence, these 3 US cities may be exceptions due to statistical variation. From this multicountry examination, we concluded that OT can be estimated by the 83.6th percentile value of daily maximum temperature.
Table 2.
OT, 84th percentile of T max, and ratio of RMOT over RMav
| Country | City | OT | 84th percentile of T max | Ratio |
|---|---|---|---|---|
| Taiwan | Taipei | 33.4 | 33.9 | 0.95 |
| Taichung | 33.0 | 33.0 | 0.94 | |
| Kaohsiung | 31.2 | 32.5 | 0.96 | |
| Korea | Seoul | 27.8 | 28.1 | 0.93 |
| Busan | 28.7 | 26.6 | 0.93 | |
| Daegu | 29.9 | 29.5 | 0.93 | |
| Incheon | 27.5 | 26.9 | 0.94 | |
| Gwangju | 29.1 | 28.8 | 0.92 | |
| Daejeon | 29.6 | 28.4 | 0.91 | |
| USA | Los Angeles | 30.0 | 28.3 | 0.95 |
| New York | 26.7 | 28.3 | 0.92 | |
| Chicago | 26.1 | 27.8 | 0.94 | |
| Dallas/Fort Worthb | 37.2 | 34.4 | 0.93 | |
| Houstonb | 41.7 | 33.9 | 0.93 | |
| Phoenix | 41.7 | 40.0 | 0.89 | |
| Santa Ana/Anaheim | 33.3 | 31.1 | 0.94 | |
| San Diegob | 41.7 | 24.4 | 0.95 | |
| Miami | 31.7 | 32.2 | 0.96 | |
| Detroit | 25.0 | 27.2 | 0.93 | |
| Seattle | 22.2 | 23.3 | 0.93 | |
| San Bernardino | 39.4 | 38.9 | 0.91 | |
| San Jose | 30.6 | 31.7 | 0.91 | |
| Minneapolis/St. Paul | 26.7 | 26.7 | 0.92 | |
| Riverside | 44.4 | 42.8 | 0.91 | |
| Philadelphia | 27.8 | 29.4 | 0.92 | |
| Atlanta | 31.7 | 31.1 | 0.93 | |
| Oakland | 32.8 | 33.9 | 0.90 | |
| Denver | 33.3 | 32.2 | 0.92 | |
| Cleveland | 26.1 | 26.7 | 0.94 | |
| Spain | Barcelona | 27.9 | 29.4 | 0.88a |
| France | Paris | 22.8 | 23.6 | 0.92a |
| Italy | Rome | 25.0 | 26.8 | 0.89a |
aTarget population is all ages combined
bOptimum temperature was not observed; the lowest mortality was observed at the highest end of the temperature
Precision improvement
To improve precision, use of long-term data and combining area-specific data are effective, provided that the chronological trend is well controlled and the heterogeneity among areas is reasonably small.
To control for chronological trend and population size, we introduced relative risk. The reference mortality for each year is the average number of deaths during the days with daily maximum temperature from the 75th to 85th percentile for each year. We chose this reference because this reference temperature range usually covers the OT, and because this reference is less affected by influenza epidemic than the annual average daily number of deaths or adding time trend in regression models as a nonparametric term.
Lag effect inclusion
As explained earlier, lag effect should be controlled for to obtain the overall heat-related effect. For this purpose, we used a distributed lag nonlinear model [8]. In the actual calculation, we used the dlnm package developed by Gasparrini [12] in R 2.15.1 [13]. In their paper, they describe dlnm as “a modelling framework that can simultaneously represent non-linear exposure–response dependencies and delayed effects. This methodology is based on the definition of a ‘cross-basis’, a bi-dimensional space of functions that describes simultaneously the shape of the relationship along both the space of the predictor and the lag dimension of its occurrence.” In our model, we used OT-offset daily maximum temperature (expressed as “Tmax − OT”) as the temperature index. Another choice would be the percentile value of daily maximum temperature, because most prefectures have OT close to the 84th percentile value. However, the range of daily maximum temperature is very wide in northern prefectures, whereas that in southern prefectures is narrow, so a one-unit increase of the percentile corresponds to a different increase in temperature.
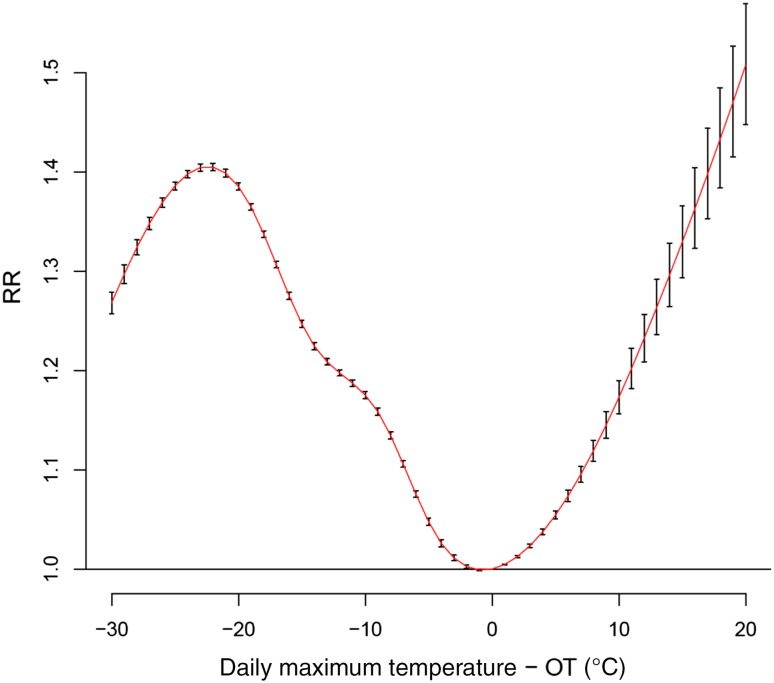
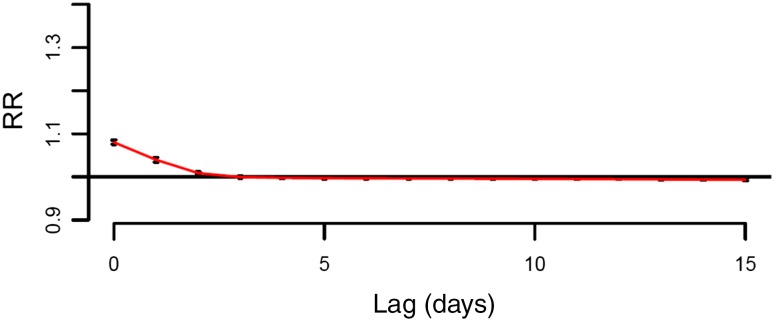
The parameter setting of the dlnm model is as follows: For both OT-offset daily maximum temperature and its lag (from 0 to 15 days), we used natural cubic splines with degree of freedom 6. OT-offset daily maximum temperature = 0, i.e., the mortality level at OT, was used as a reference. Since we used relative mortality, quasi-Poisson distribution was assumed. Figure 5 shows the dlnm result. This curve shows the result of adding up the lag effect. Figure 6 shows the lag pattern for the situation when the daily maximum temperature is 5 °C higher than OT. Lag 0 days had the highest risk, followed by lag 1 day. These risks, including slightly negative risk up to lag 15 days, were added up to construct Fig. 5. As observed, heat-related mortality increases monotonically above OT. On the other hand, below OT there is a complex relationship between mortality and temperature.
Fig. 5.
Risk function of excess mortality due to heat (for 47 prefectures in Japan, 1972–2008). Note: Lag effects up to 15 days were added to construct this curve
Fig. 6.
Lag structure of the heat-related relative risk when the daily maximum temperature is 5 °C higher than OT. Note: Lag structure when T max − OT was 5
From relative risk to excess number of deaths
The above risk function curve used the relative risk, and we need to estimate the excess number of deaths using this relative risk. Because the reference of the relative risk is the risk at OT, we can convert the relative risks if we can calculate the number of deaths when the temperature is the OT (NDOT). For this purpose, considering that the available information is the annual number of deaths (NAN), we need the following formula:
 |
where RMOT is the relative risk at OT and RMav is the average daily relative risk. (NAN/365.25) yields the daily average number of deaths. We obtained both RMOT and RMav using the Japanese dataset. Based on the Japanese dataset, the average and standard deviation of RMOT/RMav were 0.88 and 0.014, respectively.
To examine the robustness of the above index, we used selected data from cities in Korea, Taiwan, the USA, and Europe. Table 2 presents the values of this ratio in these countries selected for this manuscript. Although cities in Korea, Taiwan, and the USA showed a higher ratio than Japanese prefectures, two European countries showed a lower ratio. Considering that the European data are for all ages combined, the ratios for the 65+-year-old age group is expected to be even lower, because <65-year-old age groups are usually more resistant to heat; heat-related relative risk is lower for younger age groups. Based on this observation, we decided to use the Japanese ratio, 0.88, for global projection.
Projection of future impact of climate change on heat-related mortality
We need the daily maximum temperature distribution for risk estimation. So, we chose NCC (= NCEP Corrected by CRU, where NCEP stands for National Centers for Environmental Prediction, USA, and CRU stands for Climate Research Unit, University of East Anglia) daily data [14] as the baseline climate data. For the future climates, we used one of the general circulation models provided by the WHO Global Burden of Diseases project, i.e., BCM2. Here, we added the monthly average difference between the current climate and the future climate from models to each of the baseline daily maximum temperatures within the same month. The grid resolution is 1°. As the socioeconomic scenario, we used SRES A1B.
Adaptation is another concern. When the OT is estimated as the 83.6th percentile value of daily maximum temperature as of the current climate, we assume no adaptation (0 % adaptation). If the future climate is used for OT estimation, we assume 100 % adaptation. The midpoint of the 0 and 100 % adaptation OTs is assumed to be the OT for 50 % adaptation. V-shape flattening is another possible type of adaptation, but our preliminary analyses showed no evidence of flattening (this will be published in another paper), and we did not include this type of adaptation in this manuscript.
Because there are excess deaths due to heat even at present, the excess number of deaths attributable to climate change is calculated using the “counterfactual method.” The idea is that, with identical annual mortality rate, what is the difference between the number of excess deaths in the baseline case and that in the altered climate case? The actual procedure for 2030 is as follows: The calculation was done for each 1° × 1° grid of the globe. We used the annual number of deaths (provided by the WHO) in 2030 for both the baseline and altered climate case. Then, for the baseline case, we applied the temperature distribution of the current climate (1961–1990) to the risk functions (based on 47 prefectures of Japan) for 0, 50, and 100 % adaptation; for the altered climate case, we applied the temperature distribution of the projected 2030 climate obtained using BCM2 instead of the current climate. The difference in the number of excess deaths between these two cases is considered to be the climate-attributable excess number of deaths. These grid-specific numbers of deaths were summed up for each WHO region (Table 3). Likewise, the 2050 climate-attributable excess number of deaths was calculated.
Table 3.
WHO regions
| WHO_REG_NEW | GBDname |
|---|---|
| AP_HI | Asia Pacific, High Income |
| As_C | Asia, Central |
| As_E | Asia, East |
| As_S | Asia, South |
| As_SE | Asia, Southeast |
| Au | Australasia |
| Ca | Caribbean |
| Eu_C | Europe, Central |
| Eu_E | Europe, Eastern |
| Eu_W | Europe, Western |
| LA_A | Latin America, Andean |
| LA_C | Latin America, Central |
| LA_S | Latin America, Southern |
| LA_T | Latin America, Tropical |
| NA_HI | North America, High Income |
| NA_ME | North Africa/Middle East |
| Oc | Oceania |
| SSA_C | Sub-Saharan Africa, Central |
| SSA_E | Sub-Saharan Africa, East |
| SSA_S | Sub-Saharan Africa, Southern |
| SSA_W | Sub-Saharan Africa, West |
Results
Table 4 presents the projected excess heat-related deaths by WHO region. Asian regions are vulnerable to climate change impact.
Table 4.
Projection of heat-related excess deaths
| Region | 2030 | 2050 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Populationa | Baseline | 0 %b | 50 %b | 100 %b | Populationa | Baseline | 0 %b | 50 %b | 100 %b | |
| AP_HI | 177,053 | 2,427 | 4,802 | 3,635 | 2,598 | 162,307 | 2,528 | 6,866 | 4,395 | 2,588 |
| As_C | 9,529 | 611 | 1,458 | 975 | 598 | 103,588 | 947 | 3,797 | 2,024 | 854 |
| As_E | 1,428,481 | 5,343 | 18,423 | 11,053 | 5,837 | 1,332,115 | 7,050 | 36,739 | 18,612 | 7,184 |
| As_S | 2,033,885 | 10,692 | 26,666 | 18,022 | 11,296 | 2,284,943 | 17,429 | 65,562 | 37,524 | 18,489 |
| As_SE | 723,970 | 1,449 | 5,718 | 3,078 | 1,594 | 777,181 | 2,487 | 19,662 | 8,371 | 2,549 |
| Au | 32,982 | 119 | 370 | 230 | 125 | 37,063 | 156 | 837 | 424 | 174 |
| Ca | 48,633 | 2 | 195 | 75 | 2 | 49,792 | 3 | 553 | 261 | 3 |
| Eu_C | 115,732 | 988 | 3,123 | 1,955 | 1,090 | 107,099 | 1,058 | 5,396 | 2,998 | 1,417 |
| Eu_E | 195,411 | 1,708 | 6,350 | 3,647 | 1,860 | 178,872 | 1,732 | 10,471 | 4,845 | 1,721 |
| Eu_W | 441,260 | 3,570 | 6,214 | 4,722 | 3,485 | 446,713 | 4,425 | 13,367 | 8,334 | 4,677 |
| LA_A | 66,776 | 41 | 372 | 160 | 40 | 75,150 | 71 | 1,760 | 548 | 78 |
| LA_C | 287,206 | 700 | 2,181 | 1,239 | 711 | 318,626 | 1,226 | 7,364 | 3,363 | 1,249 |
| LA_S | 69,901 | 234 | 924 | 537 | 263 | 74,285 | 301 | 2,069 | 925 | 289 |
| LA_T | 229,162 | 364 | 2,050 | 1,066 | 432 | 233,166 | 563 | 6,546 | 2,545 | 694 |
| NA_HI | 401,536 | 2,408 | 7,394 | 4,704 | 2,702 | 446,749 | 2,953 | 15,441 | 7,877 | 3,235 |
| NA_ME | 584,318 | 1,596 | 4,780 | 2,977 | 1,683 | 681,137 | 3,209 | 15,331 | 7,940 | 3,302 |
| Oc | 14,113 | 4 | 47 | 14 | 3 | 18,172 | 8 | 195 | 68 | 7 |
| SSA_C | 152,539 | 201 | 918 | 482 | 221 | 212,327 | 438 | 4,007 | 1,645 | 485 |
| SSA_E | 574,918 | 858 | 3,686 | 1,923 | 857 | 848,878 | 1,679 | 14,734 | 6,060 | 1,776 |
| SSA_S | 81,752 | 156 | 539 | 319 | 165 | 87,940 | 246 | 1,737 | 798 | 300 |
| SSA_W | 543,556 | 775 | 2,491 | 1,486 | 785 | 809,872 | 1,578 | 9,468 | 4,465 | 1,679 |
aIn thousands. Based on United Nations 2010 revision, medium estimates
b0, 50, and 100 % represent adaptation level
In some regions, the heat-related excess deaths constitute up to 0.6 % of deaths, and some high-income regions also suffer a 0.1–0.4 % excess.
Discussion
Because this manuscript aims at developing a better projection model for heat-related excess deaths, the problems and their solutions were already addressed in “Materials and methods” section. Here, we evaluate how our goal was achieved, i.e., how much the fit, precision, and robustness of the proposed model have been improved from the previous projection [7]. As shown in Figs. 2 and 5, it is obvious that the fit is much better for the present model. To show the improvement of precision, we used the present model and applied it to the observation period of the previous model, i.e., 1972–1995. As an example, when the temperature was 10 °C higher than OT, the risk estimate (95 % confidence interval) of this calculation was 1.241 (1.218–1.265), whereas the present calculation gave 1.173 (1.156–1.189); the range of the confidence interval was 30 % smaller. As for the robustness, Table 2 clearly shows the similarity of the OT and the ratio of RMOT over RMav across a wide range of areas, including Asia, the USA, and Europe. Hence, our model that sets OT to be around the 84th percentile value of daily maximum temperature can be generalizable to all over the world. One additional concern may be the applicability of our OT estimation to tropical areas, where the annual temperature difference is very small. Our analyses covered very cold areas to subtropical areas, but did not cover tropical areas or countries in the Southern Hemisphere. In this regard, McMichael and coworkers’ report [15] is worth mentioning, because they observed the heat-related effect for 12 cities including cities in tropical countries and those in the Southern Hemisphere. Their model used a different method from ours; For example, they used daily mean temperature instead of daily maximum temperature, and they averaged out lag effect for lag 0–1 day and for lag 0–13 days. Still, the relation of the 0–1 averaged lag model was V-shaped for the majority of the cities. Considering that the 84th percentile value is roughly equal to the summer mean temperature, we tried to identify summer average temperature and optimum temperature from the graphs they provided. Among the cities with a V-shaped relation, most of the cities, including a tropical city (Bangkok, Thailand), had optimum temperature similar to their respective summer average temperature. Although this procedure is not accurate, at least use of the 84th percentile value in predicting OT cannot be falsified even by observations of cities in tropical zones or in the Southern Hemisphere. Another supporting report is the 4th Assessment Report of the Intergovernmental Panel on Climate Change [16]; temperature rise in tropical areas is expected to be less prominent compared with temperate areas and high-latitude areas. Hence, our projection would not be wide of the mark.
Compared with our previous projection, this new projection has advantages in terms of fit, precision, and robustness. Also, we included lag effect, which addresses mortality displacement. This implies that, although there may be some mortality displacement effect, the overall risk exists and climate change would increase the burden due to heat-related mortality.
Because the purpose of this paper is to show how we have improved the model for the global projection, we showed the projection results using only one global circulation model. However, the model described in this paper was adopted in the new WHO Global Burden of Diseases attributable to climate change, which will appear somewhere soon, and several models will be used and compared.
Compared with the total number of deaths, the proportion of deaths due to heat-related mortality attributable to climate change appears small. However, considering that even huge cyclones do not kill many people nowadays in high-income countries, heat waves are a major environmental hazard. Of course, we need to compare the heat-related impact and cold-related impact to obtain the net impact of global warming. However, new papers have warned that we should not naively apply the V-shaped temperature–mortality relation to projections for future cold-related excess deaths [17, 18]. We will try to develop our model for cold-related excess mortality after taking into account the points these papers raised in the near future.
Acknowledgments
This study was supported by the Environment Research and Technology Development Fund (S-8 & S10) of the Ministry of the Environment, Japan, and the Global Research Laboratory (grant K21004000001-10A0500-00710) through the National Research Foundation of Korea (NRF), funded by the Ministry of Education, Science, and Technology, Korea.
Conflict of interest
All authors have no conflicts of interest.
References
- 1.The World Health Report 2002-reducing risks, promoting healthy life. Geneva: WHO; 2002. [DOI] [PubMed] [Google Scholar]
- 2.Kunst AE, Looman CW, Mackenbach JP. Outdoor air temperature and mortality in the Netherlands: a time-series analysis. Am J Epidemiol. 1993;137:331–341. doi: 10.1093/oxfordjournals.aje.a116680. [DOI] [PubMed] [Google Scholar]
- 3.El-Zein A, Tewtel-Salem M, Nehme G. A time-series analysis of mortality and air temperature in Greater Beirut. Sci Total Environ. 2004;330:71–80. doi: 10.1016/j.scitotenv.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 4.Honda Y, Ono M, Sasaki A, Uchiyama I. Shift of the short-term temperature mortality relationship by a climate factor—some evidence necessary to take account of in estimating the health effect of global warming. J Risk Res. 1998;1:209–220. doi: 10.1080/136698798377132. [DOI] [Google Scholar]
- 5.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz J a. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- 6.Honda Y, Kabuto M, Ono M, Uchiyama I. Determination of optimum daily maximum temperature using climate data. Environ Health Prev Med. 2007;12:209–216. doi: 10.1265/ehpm.12.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takahashi K, Honda Y, Emori S. Assessing mortality risk from heat stress due to global warming. J Risk Res. 2007;10:339–354. doi: 10.1080/13669870701217375. [DOI] [Google Scholar]
- 8.Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology. 2006;17:624–631. doi: 10.1097/01.ede.0000239732.50999.8f. [DOI] [PubMed] [Google Scholar]
- 9.Fouillet A, Rey G, Laurent F, Pavillon G, Bellec S, Guihenneuc-Jouyaux C, et al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006;80:16–24. doi: 10.1007/s00420-006-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bell ML, Dominici F, Samet JM. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology. 2005;16:436–445. doi: 10.1097/01.ede.0000165817.40152.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Stat Med. 2010;29:2224–2234. doi: 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ihaka R, Gentleman RR. A language for data analysis and graphics. J Comput Graph Stat. 1996;5:299–314. [Google Scholar]
- 14.Ngo-Duc T. A 53-year forcing data set for land surface models. J Geophys Res. 2005;110:D06116. [Google Scholar]
- 15.McMichael AJ, Wilkinson P, Kovats RS, Pattenden S, Hajat S, Armstrong B, et al. International study of temperature, heat and urban mortality: the “ISOTHURM” project. Int J Epidemiol. 2008;37:1121–1131. doi: 10.1093/ije/dyn086. [DOI] [PubMed] [Google Scholar]
- 16.Solomon S, Qin D, Manning M, Chen Z, Marquis M, Ave KB. IPCC. Summary for Policymakers. In: Climate Change 2007. The physical science basis contribution of working group I to the fourth assessment report of the intergovernmental panel on climate change. Cambridge, UK and New York, USA: Cambridge University Press; 2007. p 18.
- 17.Kinney PL, Pascal M, Vautard R, Laaidi K. Winter mortality in a changing climate: will it go down? Bull Epidémiol Hebd. 2012;12–13:148–151. [Google Scholar]
- 18.Ebi KL, Mills D. Winter mortality in a warming climate: a reassessment. WIRES Climate Change. 2013;4:203–212. doi: 10.1002/wcc.211. [DOI] [Google Scholar]