Abstract
Purpose
Fractures of the femur associated with total hip arthroplasty are a significant concern in orthopaedic and trauma surgery. However, little is known about the different biomechanical properties of internal fixation systems in combination with periprosthetic fractures. In this study two new internal fixation systems for periprosthetic fractures are investigated using a cadaver fracture model simulating a Vancouver B1 periprosthetic femur fracture.
Methods
Nine pairs of fresh-frozen cadaver femurs were scanned by dual X-ray absorptiometry. Cementless total hip prostheses were implanted and a periprosthetic femur fracture was simulated. Fractures were randomly fixed either with the fixed angle locking attachment plate (LAP®, Depuy Synthes®, Solothurn, Switzerland) or the variable angle non-contact bridging plate (NCB®, Zimmer GmbH, Winterthur, Switzerland). Each construct was cyclically loaded to failure in axial compression.
Results
Axial stiffness and cycles to failure were significantly higher in the NCB group. Both systems were able to be fixed well around the femoral stem.
Conclusion
The two different internal fixation systems for periprosthetic fractures differed significantly in our setup. The non-contact bridging plate system revealed significantly higher failure load and may be the preferred option where high stability and load capacity is needed right after operation.
Keywords: Periprosthetic, Vancouver B1 fracture, Cadaver, Biomechanics, Fixation
Introduction
Periprosthetic fractures of the femur are a serious concern in orthopaedic and trauma surgery. Due to an increasing number of total hip arthroplasties (THA) the incidence of periprosthetic fractures continuously rises [1–3]. The main goals in the management are fracture union, a stabilized prosthesis, and a functional limb suitable for ambulation. The management of those fractures is based upon fracture location and implant stability.
Treatment of periprosthetic fractures remains difficult due to the combination of fractured bone and prosthesis with further complications like osteoporotic bone and cement used for prosthesis fixation. Therefore, biomechanical conditions differ from a fracture of a femur without THA. Common treatment methods are open reduction and internal fixation, revision arthroplasty or a combination of both [4–6], depending on the stability of the prosthesis.
Numerous biomechanical studies investigated different techniques of periprosthetic fracture fixation [7–12], although as yet, not all types of these fractures or fixation methods have been comprehensively evaluated and new tools for fixation are on the way.
Various osteosynthetic devices have been developed over recent years to increase stability around the prosthesis [5, 11, 13]. New anatomically pre-shaped devices using angular stability may help to improve the outcome of those complicated fractures. There are several competing systems on the market using diverse types of fixation which differ in size of implants, type of fixation or material. Locked plating seems to be beneficial to increase stability in an osteoporotic bone, however, it still remains controversial whether fixed or variable angled screws are preferable to provide the best stability. Little is known about the biomechanical properties of those different internal fixation systems, especially in combination with periprosthetic fractures and compared to each other. The purpose of this study was to investigate the currently two most popular internal fixation plate systems especially designed for periprosthetic femoral fractures: the fixed angle locking attachment plate (LAP®, Depuy Synthes®, Solothurn, Switzerland) and the variable angle non-contact bridging plate (NCB®, Zimmer GmbH, Winterthur, Switzerland).
The biomechanical properties of these two internal fixation systems were evaluated in combination with THA using a cadaver fracture model simulating a Vancouver B1 periprosthetic femur fracture to determine load to failure and mode of failure.
Material and method
Bone samples
Institutional review board approval was obtained. In this study nine pairs of fresh frozen femora were used. The mean age was 81 years (range 67–90; six female, three male). Before mechanical testing bone mineral density was measured in the femoral head and the trochanter region using pQCT scan. The mean trabecular value of these regions was used for further evaluation.
Implants
A cementless standard straight stem (Alloclassic® Zweymüller® Schaft SL, Zimmer GmbH, Switzerland) was implanted according to the manufacture’s guidelines.
We used two different angular stable plates in this study. For a pairwise comparison, specimens were randomly assigned to either group I (LAP—Locking Attachment Plate, Synthes, Solothurn, Switzerland, n = 9) or group II (NCB PP—Non-Contact Bridging Periprosthetic Proximal Femur Plate, Zimmer GmbH, Winterthur, Switzerland, n = 9).
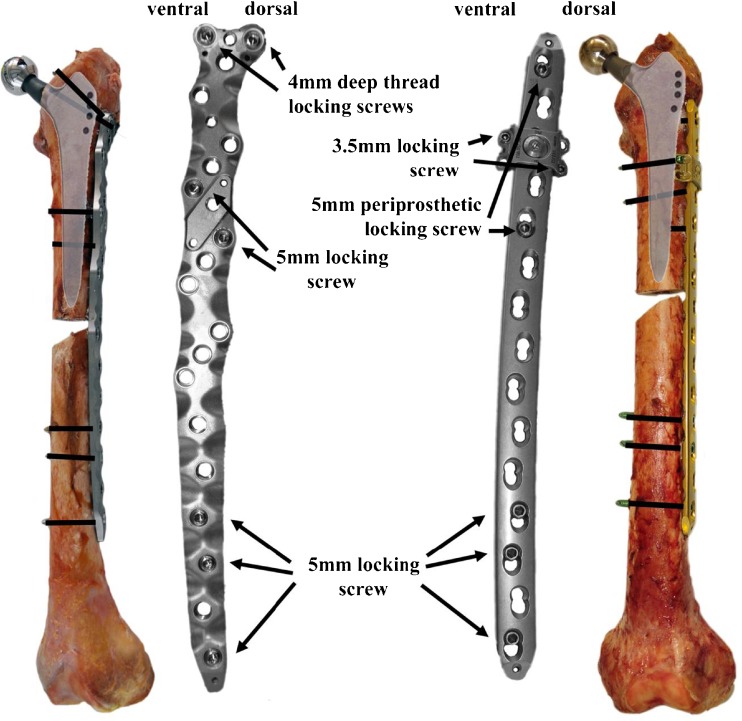
The LAP is an add-on plate designed for the treatment of periprosthetic femoral fractures to allow screw placement passing the shaft component of the femoral stem. In our study the four-hole locking attachment plate was used in combination with a broad curved 15-hole locking compression plate (LCP; length 282 mm, Synthes, Solothurn, Switzerland). Both implants are made of titanium alloy and were used with corresponding 5-mm fixed angle locking screws for distal locking, 5-mm periprosthetic fixed angle locking screws proximal and 3.5-mm fixed angle locking screws for the LAP.
The NCB Periprothetic Femur System is made of titanium alloy (Protasul®-64). We used the 12-hole proximal femoral plate (length 285 mm). This system allows a variety on screw positions as well as different screw options. Additionally, all screws can be placed in a variable angel of 15° in each direction. We used 5-mm screws and 4-mm deep thread screws proximally. All screws were angular stable locked by locking caps.
Distally, both groups were locked by three 5-mm bicortical locking screws. In the LAP group two short 5-mm periprosthetic fixed angle locking screws were placed proximally through the LCP and two 3.5-mm fixed angle locking screws bicortically through the LAP. In the NCB group two 4-mm variable angle screws were placed proximally passing the prosthesis and two 5-mm variable angle screws passing the stem. The screw placement is visualized in Fig. 1.
Fig. 1.
Implants used in this study (NCB left, LAP+LCP right) and the screw configurations of the plate constructs
Instrumentation
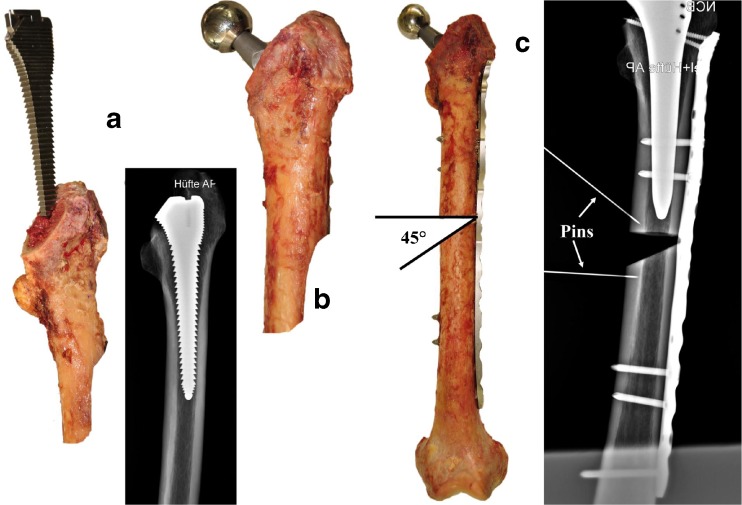
Before instrumentation the size of the stem was evaluated using the TraumaCad-software (Voyant Health, Munich, Germany). Stem implantation was performed by an experienced orthopedic surgeon (R.S.). The shaft was reamed using the appropriate rasps until the correct size was reached and the stem was implanted (Fig. 2a, b). This step was controlled using X-rays (Fig. 2a).
Fig. 2.
Process of implantation (from left to right) and the osteotomy representing a Vancouver B1 fracture without medial support. Pins were placed to measure displacement radiographically
Instrumentation of both systems followed the manufacturer’s guidelines. Three distal 5-mm bicortical locking screws were placed.
In the NCB constructs the two most proximal screws were placed using 4-mm screws with deep thread. Finally, two 5-mm locking screws were placed in the middle passing the prosthesis stem.
In the LAP group the two 5-mm periprosthetic screws were placed in monocortical manner followed by the two 3.5-mm bicortical locking screws in the LAP. These screws were placed after bending the LAP to allow bicortical screw placement.
After the plates were fixed to the bone, an X-ray was taken to control implant position and plan the osteotomy. The osteotomy was planned 5 mm below the hip shaft stem with a horizontal cut in the proximal part and a 45° cut in the distal part (Fig. 2c).
Test setup/biomechanical testing
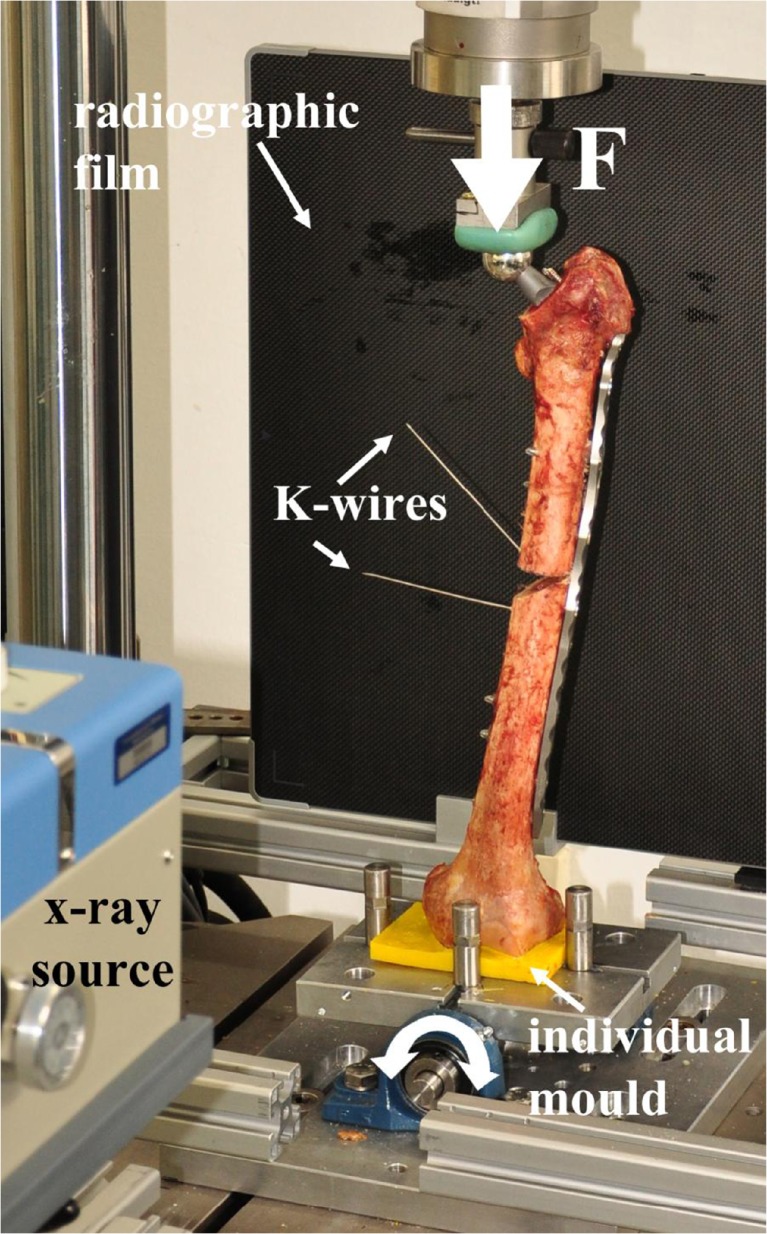
For this study we modified the test setup used in previous studies of our group [14, 15]. The specimens were anatomically loaded via the femoral head. The femoral head was placed under a pre-shaped mould and thus attached mobile to the machine actuator. The distal femur was also placed in an individually shaped mould (made of Technovit 4000, Heraeus, Hanau, Germany) on a plate able to tilt medially and laterally. Testing was performed using a servo-hydraulic testing machine (Instron 8874) equipped with a 10 kN load cell (Fig. 3). Cyclic sinusoidal axial loading was performed at 2 Hz until failure of the construct. Starting at 750 N peak load, the load was continuously increased at 0.1 N/cycle. The base load was kept constant at 100 N throughout the test. Every 250 cycles the machine stopped at 100 N until X-ray was performed.
Fig. 3.
Test setup with the specimen proximally placed under a custom made shell and distally on a custom made mould on a table able to tilt medially and laterally. This picture also shows the X-ray machine and the X-ray film placed in AP direction
Data acquisition and evaluation
Time, number of cycles, axial load and axial displacement were recorded from the test system’s transducers at a frequency of 64 Hz. Axial stiffness was calculated from the load displacement curves for cycle 10 to 19; further statistics was performed with the mean value.
Two 1.5-mm K-wires were attached to the medial femoral shaft proximally and distally to the fracture to serve as landmarks for X-ray data evaluation. In this way varus collapse, plate bending and prosthesis migration could be detected by the change of angle between the wires, change of distance between screw tips, screw and prosthesis tip. Fluoroscopic imaging was performed in the anteroposterior direction using a digital radiograph system (EXAMION, Fellbach, Germany) every 250 cycles (Fig. 4). X-ray evaluation was performed by means of a custom-made software routine (Matlab 7.9 R2009b, Image processing Toolbox, The MathWorks GmbH, Ismaning, Germany). The number of cycles to 5° and 10° varus collapse with respect to the initial X-ray was identified for all specimens.
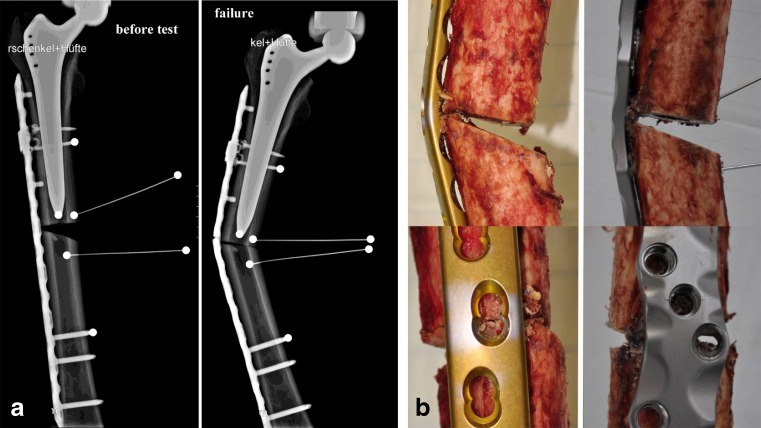
Fig. 4.
Two exemplary X-rays before testing (a left) and after failure (a right) the white dots mark the points for X-ray evaluation. Mode of failure with plate bending in the LAP group (b left row) and blade bending with cracks nest to the screw hole for the non-contact bridging plate (b right row)
After assuring normal distribution of the test data (Shapiro-Wilk test), paired t-tests were carried out to identify differences between study groups with regard to BMD, stiffness and cycles to failure. Pearson’s correlation coefficient R was calculated for BMD and cycles to failure. The software package SPSS 21.0 (SPSS Inc., Chicago, USA) was used for all statistical evaluations. Level of significance was p ≤0.05.
Results
Bone mineral density
The mean overall bone mineral density (BMD) was 79,7 mgHA/ccm (SD 46). The BMD in the NCB group was 80.2 mgHA/ccm (SD 44) and in the LAP group 79.2 mgHA/ccm (SD 51.5). This difference was statistically not significant (p = 0.866).
Axial stiffness
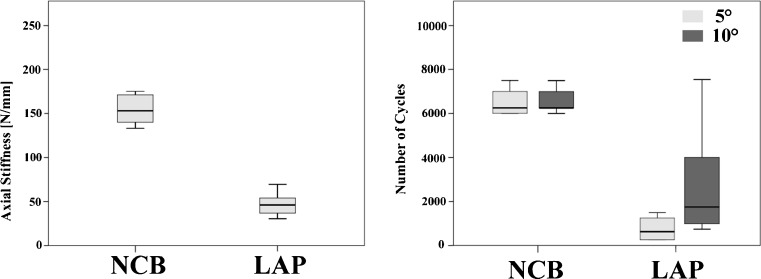
The mean axial stiffness was 163 N/mm (SD 29) in the NCB and 47 N/mm (SD 12) in the LAP group. This difference was statistically significant (p < 0.01). The NCB constructs showed a 3.4 times higher axial stiffness compared to the LAP group (Fig. 5).
Fig. 5.
Axial stiffness (left graph) and the number of cycles until failure (right graph) for the NCB and LAP group
Cycles to 5° varus collapse and failure (10° varus), failure load and failure mode
The mean number of cycles until 5° varus collapse was 6,475 cycles (SD 1,325) for the NCB group and 750 cycles (SD 500) in the LAP group. The mean number of cycles until failure (10° varus) was 6,500 (SD 1,318) for the NCB and 2,505 (SD 2,121) for the LAP group. The difference was statistically significant for both conditions with p < 0.01 (Fig. 5).
The average load to failure was 1,400 N (SD 132) for the NCB and 1,001 N (SD 212) for the LAP group. Thus, the NCB group showed a 40 % higher failure load. The difference was statistically significant (p < 0.01).
Additionally, the patterns of failure in both configurations differed tremendously. The LAP group showed early deformity of the construct. In the NCB specimens the plate system retained its shape for a long time before failing by plate breakage (Fig. 4).
Correlation BMD–failure
There was no correlation between the number of cycles to failure and the bone mineral density for both groups (NCB: R2 = 0.12; LAP: R2 = 0.03).
Discussion
Internal fixation systems especially adjusted for periprosthetic femoral fractures have been gaining in importance in the treatment of those challenging fractures [7, 16, 17]. In the present study, the non-contact bridging plate (NCB®) and the locking attachment plate with LCP (LAP-LCP®) [18, 19] were compared for the first time in a cadaver matched pair approach to determine load to failure and mode of failure. Using different technical approaches for fracture fixation around the prosthesis the two internal fixation systems differed significantly in our study. Both systems could be fixed well around the femoral stem. The LAP-LCP allowed different applications around the stem but was less stable due to the less rigid main plate. The variable angle locking screw system of the NCB revealed significantly higher stiffness and cycles to failure.
The NCB was the first plate system for periprosthetic fractures that provided a variable angle screw positioning. This system allows conventional screw placement up to a 15° variable angle to the plate axis allowing bicortical screw positioning passing the intramedullary stem. The screws are, subsequently, locked in position with screw caps. Konstantinidis et al. showed in a former model of this plate, that those variable angle screws were able to provide similar stability in a periprosthetic scenario as fixed angle screws. They demonstrated that operative stabilization of periprosthetic femoral fractures can be successfully and equally well achieved with both the LISS plate with periprosthetic monocortical screws and the NCB plate with variable angle placed bicortical locking screws. However, the NCB system was not superior to the LIS-system by Synthes in that study, despite better bilateral screw anchoring [7]. Other studies revealed a safe option in treatment of complex and periprosthetic femoral fractures in geriatric patients at a low complication rate with the NCB [19].
The NCB plate has been modified over recent years to provide more possibilities to provide stability around the stem. This newly designed second generation plate system has shown promising results so far [20]; however, it has not been evaluated biomechanically in a periprosthetic fracture situation yet. Compared to the first model for distal femur application, there are now three variants of the plate for proximal, diaphyseal and distal femur fractures. Additional offset plate holes allow bicortical screw fixation around the stem of the implanted prosthesis. During biomechanical testing the NCB plate system retained its shape for a long time before failing by plate breakage. The construct showed significantly higher axial stiffness and number of cycles compared to the LAP group, most probably caused by the stiffer and heavier plate itself compared to the LCP. A typical failure mode of the NCB plate was the cracking along the plate itself and of the bone around the screws, due to the high rigidity of the NCB construct also described by Erhardt and others [16, 17].
The locking attachment plate (LAP), a clamp-on plate attached to a conventional locking compression plate (LCP), provides lateral arms for bicortical offset screw placement beside the prosthesis stem. Lenz et al. demonstrated in a biomechanical study on synthetic bone that the LAP construct provided an improved mechanical stability and strength compared to a cerclage construct, exhibiting generally less relative movements at the plate-femur interface in all registered modalities [18]. In a first clinical study, Kammerlander et al. described no surgical complications or implant loosening in eight patients [21]. In our study the LAP-LCP group showed early deformity of the construct at the LC-plate. The locking attachment plate itself kept its stability. Construct collapse appeared by early bending of the LCP around the fracture gap due to the inferior size and rigidity of the LCP compared to the NCB. A possible solution might be the use of an additional perpendicular plate at the fracture side to provide more stability [22].
The Synthes system might serve as an example for “conventional” locking screw systems without variable angle position when comparing other implant systems for periprosthetic fractures to our results. One might expect that these systems reveal the same results as the system tested here.
The Zweymueller stem was chosen in our study because of its popularity and good results [23]. Due to its rectangular cross section design the Alloclassic stem allows screw placement parallel to the stem in our setup. This might be more difficult with other stem designs such as round shaped or oval which fill out the intramedullary canal and provide less space for screw placement around the stem. The LAP construct might be beneficial for fractures around those implants due to its variable shape and screw hole design, which can be adjusted to the bone.
Limitations of our study are the relatively small number of samples. However, the bone models used and both groups were characterized by a very small variability. In addition, the matched pair approach investigated both fixation devices in the same “patient” with the same bone quality leading to a good comparability of the results. The average age of cadavers was quite high, characteristic of the type of population sustaining periprosthetic fractures; thus bone quality is not comparable to younger patient cohorts.
Furthermore, this is an in vitro biomechanical study with limitations in the loading conditions and missing muscle forces due to the use of nonliving tissue as well as failure to account for soft tissue contributions to stability. Cadaveric femurs allow for optimal plate fixation because they are free of soft tissue that might hinder sufficient exposure. Since we used non cemented implants, our results should be implemented to these types of fixation. However, implant fixation around cemented prostheses should follow similar principles in terms of type of failure.
The osteotomy gap simulated a comminuted fracture where compression may not be attainable. This was done to limit the effect of compressive load sharing of the bone ends and look at the isolated effect of the proximal fixation on stability.
Conclusion
We compared the biomechanical performance of two locking plate constructs for internal fixation of periprosthetic fractures. Using different technical approaches both fixation systems were able to be fixed around the investigated femoral stem but differed significantly in our setup. The locking attachment plate was less stable due to the less rigid main plate. The non-contact bridging plate revealed significantly higher stiffness and cycles to failure and may be the preferred option where high stability and load capacity is needed right after operation.
Further in vivo analysis is necessary to evaluate the appropriate stiffness required for optimal fracture union and to determine appropriate concepts and clinical significance of locking plate and screw constructs in the management of periprosthetic femur fractures associated with THAs.
Acknowledgments
Conflict of interest
The authors were not compensated; benefits were received in support of the research material described in this article from Zimmer GmbH (Winterthur, Switzerland).
References
- 1.Lindahl H, Malchau H, Oden A, Garellick G. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br. 2006;88(1):26–30. doi: 10.1302/0301-620X.88B1.17029. [DOI] [PubMed] [Google Scholar]
- 2.Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011;93(1):96–101. doi: 10.1302/0301-620X.93B1.25087. [DOI] [PubMed] [Google Scholar]
- 3.Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007;38(6):651–654. doi: 10.1016/j.injury.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 4.Garbuz DS, Masri BA, Duncan CP. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect. 1998;47:237–242. [PubMed] [Google Scholar]
- 5.Pike J, Davidson D, Garbuz D, Duncan CP, O’Brien PJ, Masri BA. Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg. 2009;17(11):677–688. doi: 10.5435/00124635-200911000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Giannoudis PV, Kanakaris NK, Tsiridis E. Principles of internal fixation and selection of implants for periprosthetic femoral fractures. Injury. 2007;38(6):669–687. doi: 10.1016/j.injury.2007.02.050. [DOI] [PubMed] [Google Scholar]
- 7.Konstantinidis L, Hauschild O, Beckmann NA, Hirschmuller A, Sudkamp NP, Helwig P. Treatment of periprosthetic femoral fractures with two different minimal invasive angle-stable plates: biomechanical comparison studies on cadaveric bones. Injury. 2010;41(12):1256–1261. doi: 10.1016/j.injury.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Lever JP, Zdero R, Nousiainen MT, Waddell JP, Schemitsch EH. The biomechanical analysis of three plating fixation systems for periprosthetic femoral fracture near the tip of a total hip arthroplasty. J Orthop Surg Res. 2010;5:45. doi: 10.1186/1749-799X-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pletka JD, Marsland D, Belkoff SM, Mears SC, Kates SL. Biomechanical comparison of 2 different locking plate fixation methods in Vancouver b1 periprosthetic femur fractures. Geriatr Orthop Surg Rehabil. 2011;2(2):51–55. doi: 10.1177/2151458510397609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Demos HA, Briones MS, White PH, Hogan KA, Barfield WR. A biomechanical comparison of periprosthetic femoral fracture fixation in normal and osteoporotic cadaveric bone. J Arthroplasty. 2012;27(5):783–788. doi: 10.1016/j.arth.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 11.Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE. Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty. 2000;15(4):523–528. doi: 10.1054/arth.2000.4339. [DOI] [PubMed] [Google Scholar]
- 12.Lehmann W, Rupprecht M, Nuechtern J, Melzner D, Sellenschloh K, Kolb J, Fensky F, Hoffmann M, Puschel K, Morlock M, Rueger JM. What is the risk of stress risers for interprosthetic fractures of the femur? A biomechanical analysis. Int Orthop. 2012;36(12):2441–2446. doi: 10.1007/s00264-012-1697-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Corten K, Vanrykel F, Bellemans J, Frederix PR, Simon JP, Broos PL. An algorithm for the surgical treatment of periprosthetic fractures of the femur around a well-fixed femoral component. J Bone Joint Surg Br. 2009;91(11):1424–1430. doi: 10.1302/0301-620X.91B11.22292. [DOI] [PubMed] [Google Scholar]
- 14.Wahnert D, Hoffmeier K, Frober R, Hofmann GO, Muckley T. Distal femur fractures of the elderly-different treatment options in a biomechanical comparison. Injury. 2011;42(7):655–659. doi: 10.1016/j.injury.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Wahnert D, Lange JH, Schulze M, Lenschow S, Stange R, Raschke MJ. The potential of implant augmentation in the treatment of osteoporotic distal femur fractures: a biomechanical study. Injury. 2013;44(6):808–812. doi: 10.1016/j.injury.2012.08.053. [DOI] [PubMed] [Google Scholar]
- 16.Buttaro MA, Farfalli G, Paredes Nunez M, Comba F, Piccaluga F. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am. 2007;89(9):1964–1969. doi: 10.2106/JBJS.F.01224. [DOI] [PubMed] [Google Scholar]
- 17.Erhardt JB, Grob K, Roderer G, Hoffmann A, Forster TN, Kuster MS. Treatment of periprosthetic femur fractures with the non-contact bridging plate: a new angular stable implant. Arch Orthop Trauma Surg. 2008;128(4):409–416. doi: 10.1007/s00402-007-0396-6. [DOI] [PubMed] [Google Scholar]
- 18.Lenz M, Windolf M, Muckley T, Hofmann GO, Wagner M, Richards RG, Schwieger K, Gueorguiev B. The locking attachment plate for proximal fixation of periprosthetic femur fractures—a biomechanical comparison of two techniques. Int Orthop. 2012;36(9):1915–1921. doi: 10.1007/s00264-012-1574-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El-Zayat BF, Ruchholtz S, Efe T, Fuchs-Winkelmann S, Kruger A, Kreslo D, Zettl R. NCB-plating in the treatment of geriatric and periprosthetic femoral fractures. Orthop Traumatol Surg Res. 2012;98(7):765–772. doi: 10.1016/j.otsr.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Ruchholtz S, El-Zayat B, Kreslo D, Bucking B, Lewan U, Kruger A, Zettl R. Less invasive polyaxial locking plate fixation in periprosthetic and peri-implant fractures of the femur—A prospective study of 41 patients. Injury. 2013;44(2):239–248. doi: 10.1016/j.injury.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 21.Kammerlander C, Kates SL, Wagner M, Roth T. Blauth M (2013) Minimally invasive periprosthetic plate osteosynthesis using the locking attachment plate. Oper Orthop Traumatol. 2013;25(4):398–410. doi: 10.1007/s00064-011-0091-1. [DOI] [PubMed] [Google Scholar]
- 22.Choi JK, Gardner TR, Yoon E, Morrison TA, Macaulay WB, Geller JA. The effect of fixation technique on the stiffness of comminuted Vancouver B1 periprosthetic femur fractures. J Arthroplasty. 2010;25(6 Suppl):124–128. doi: 10.1016/j.arth.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymuller Alloclassic system. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 2003;85-A(2):296–303. doi: 10.2106/00004623-200302000-00017. [DOI] [PubMed] [Google Scholar]