Abstract
Purpose
We conducted ultrasound-guided single-shot supraclavicular blockade and investigated the analgesic effect of dexamethasone added to levobupivacaine. The aim of this study was to determine whether the addition of low-dose dexamethasone to levobupivacaine would prolong the duration of analgesia sufficiently to avoid additional intravenous analgesic use for the first 24 hours postoperatively.
Methods
This randomised controlled study assessed 70 patients undergoing upper-extremity surgery. Patients were eligible if there 18 years or over with American Society of Anaesthesiologists (ASA) physical status I, II or III. Patients were randomly assigned to receive 25 ml 0.5 % levobupivacaine plus four milligrams dexamethasone (group 1) or 25 ml 0.5 % levobupivacaine plus one millilitre saline (group 2). Pain scores, analgesic consumption and time estimation at which they perceived that sensory and motor blockade started and resolved were recorded.
Results
Duration of sensory (1,260 min. in group 1 vs 600 min. in group 2) and motor (1,200 min. in group 1 vs 700 min. in group 2) blockade were significantly longer in group 1 (P < 0.05). Postoperative pain levels in group 1 were significantly lower (P < 0.05) at all investigation times. Analgesia consumption was significantly lower (P < 0.05) in group 1; at six and 12 hours, no patient required additional analgesia, and at 24 hours, only two patients compared with 17 in the levobupivacaine group required additional analgesia.
Conclusion
Using single-shot low-dose dexamethasone in a mixture with levobupivacaine results in prolonged analgesia duration and less analgesic use compared with levobupivacaine alone.
Keywords: Supraclavicular block, Analgesia, Surgery, Dexamethasone, Levobupivacaine
Introduction
Postoperative pain management is an important part of perioperative care and if inadequate can lead to postoperative stress and the development of chronic pain syndromes [1, 2]. In an effort to improve analgesia, facilitate early mobilisation and bypass the post-anaesthesia care unit (PACU), regional anaesthesia is often preferred. Duration of a single injection of nerve blockade is often insufficient to bypass early intravenous analgesia administration. Continuous peripheral nerve blocks have been used to provide extended analgesia. However, these techniques have generally failed to gain popularity due to the need for technical proficiency and complications such as catheter migration, anaesthetic leakage and pump malfunction [3–6]. For single-shot techniques, various adjuvants have been used to improve the quality and increase the duration of the local anaesthetic action in different peripheral nerves and regional blockade techniques. The analgesic effects of spinal and systemic corticosteroids in combination with local anaesthetics have been approved in human studies, whereas dexamethasone microspheres have increased blockade duration in both human and animal studies [6–9]. Furthermore, dexamethasone has been shown to possess an anti-inflamatory action [10].
Why dexamethasone would prolong regional anaesthesia is a subject of debate. Steroids produce vasoconstriction, so they reduce local anaesthetic absorption. A more attractive theory holds that dexamethasone increases the activity of inhibitory potassium channels on nociceptive C fibres, decreasing their activity [11]. The addition of dexamethasone to local anaesthetic administration in order to prolong analgesia duration has recently been explored. Only one study, by Tandoc et al., has thus far investigated low-dose dexamethasone, but this was added to large dosages of bupivacaine for interscalene blockade [2]. No study has yet evaluated low-dose dexamethasone in conjunction with plain levobupivacaine for brachial plexus blockade at the supraclavicular level.
We therefore conducted ultrasound (US)-guided single-shot supraclavicular blockade in patients undergoing upper-extremity surgery and investigated the analgesic effect of dexamethasone added to levobupivacaine. The purpose of this study was to determine whether the addition of low-dose dexamethasone to levobupivacaine would prolong the duration of sensory analgesia enough to avoid additional IV administration of analgesics during the first 24 hours postoperatively.
Participants and methods
Design
The investigation was carried out with approval from the Ethics Committee of University Hospital Dubrava, Zagreb, Croatia, and an informed consent from all study participants. Also, the investigation was registered on ClinicalTrials.gov (NCT01739270).
Setting
The study included 70 patients undergoing upper-extremity surgery between October 2012 and March 2013.
Participants
Patients were eligible if they were 18 years or over and had American Society of Anaesthesiologists (ASA) physical status I, II or III. According to ASA preoperative classification, patients with ASA I are healthy, ASA II have mild systemic disease and ASA III have severe systemic disease that limits activity but is not incapacitating. Exclusion criteria were patient refusal to give informed consent, pre-existing coagulation disorders, local infection at the site of blockade, neuropathy, drug or alcohol abuse, known allergy to the study drug and operation time of over six hours.
Intervention
According to a computer-generated randomisation list, patients were randomly assigned to receive a mixture of 25 ml 0.5 % levobupivacaine (Chirocaine®, Abbott Laboratories) with four milligrams dexamethasone (Dexamethasone®, Krka) (group 1) or 25 ml 0.5 % levobupivacaine with one millilitre saline (group 2). Patients and the anaesthetists were blinded to group assignment. The injection solution in both groups was prepared by an independent anaesthetist not involved in other aspects of the investigation. Supraclavicular blockade was performed under US guidance with a nerve stimulator. With the patient in the supine position, the US probe was placed in the supraclavicular site. The 22-gauge needle (Stimuplex D®, B. Braun Melsungen AG) was connected to a nerve stimulator and positioned in a plane with the US probe and advanced near the subclavian artery. The injection fluid was slowly administered after muscle contraction under 0.5 mA electrical stimulation. Careful aspiration was performed before injection to exclude vascular puncture. Noninvasive blood pressure monitoring, pulse oximetry and electrocardiogram were recorded during the operation. After the operation and during the period of investigation, all patients were visited; data on pain scores, analgesic consumption and time estimation at which they perceived that the sensory and motor blockade had resolved were recorded. Data were based on pain, recovery of sensation and strength in the hand. Postoperative pain was evaluated by visual analogue scale (VAS) score at one, six, 12 and 24 postoperatively. At a complaint regarding pain, diclofenac was injected IV. Also, patients were evaluated for any complications, such as neurological defects, respiratory problems and vomiting.
Primary and secondary outcome measures
Primary outcome measure was analgesia duration. Secondary outcome measures included onset time of motor and sensory blockade, postoperative pain level, offset time of motor and sensory blockade and analgesic consumption.
Randomisation
A randomisation schedule was computer generated by a biostatistician (otherwise uninvolved in the study). Random function from Microsoft Excel was used to randomise patients.
Statistical methods
Statistical analysis was performed using the Mann–Whitney U test, and Fisher’s exact probability test was used for frequency comparisons. P < 0.05 indicated statistical significance. Calculated sample size was 23 patients per arm based on expected improvement of analgesia duration by 30 % at P < 0.05 and power goal of 90 %. Taking into account a dropout rate of 15 %, the total number of 35 patients in each arm was estimated as sufficient to close the study.
Results
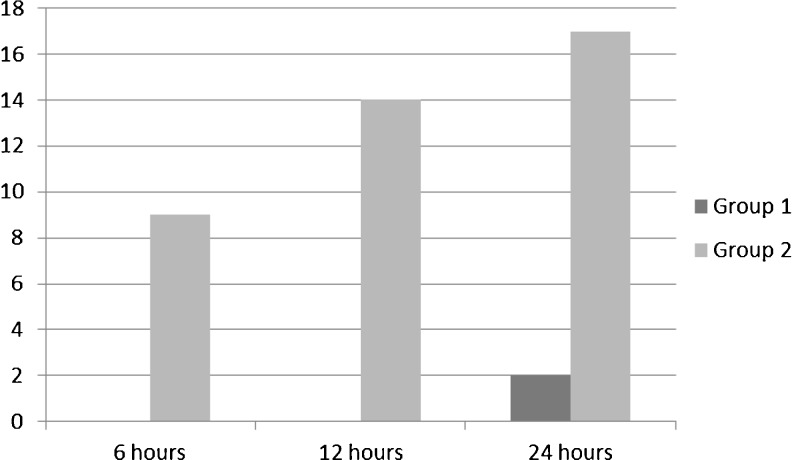
Of the 70 study participants, four were excluded because of unsuccessful blockade, three due to intraoperative changes in the surgical plan and conversion to general anaesthesia, and three because of prolonged operation time over six hours. A flow diagram of participants is presented in Fig. 1. There were no significant differences in age, body mass index (BMI) and surgery duration between groups. Also, there were no differences in pain level before supraclavicular blockade and sensory and motor onset time (Table 1). Duration of sensory (1,260 min. in group 1 vs 600 min. in group 2) and motor (1,200 min. in group 1 vs 700 min. in group 2) blockade were significantly longer in group 1 (P < 0.05). Also, postoperative pain levels in group 1 were significantly lower (P < 0.05) (Table 2) analgesia consumption differed significantly at all investigation times (P < 0.05); at six and 12 hours, no patient in group 1 received additional intravenous analgesia; at 24 hours, only two patients compared with 17 patients in group 2 received additional intravenous analgesia (Fig. 2).
Fig. 2.
Number of patients receiving analgesia. *P < 0.05
Table 1.
Comparison of patient demographics and clinical data
| Group 1 | Group 2 | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Median | Minimum | Maximum | No. | Median | Minimum | Maximum | ||
| Age (years) | 35 | 48 | 20 | 83 | 25 | 43 | 25 | 85 | 0.37 |
| BMI | 35 | 25 | 17 | 29 | 25 | 23 | 17 | 29 | 0.72 |
| VAS before blockade | 35 | 3 | 1 | 8 | 25 | 6 | 1 | 7 | 0.14 |
| TS onset (min) | 35 | 5 | 3 | 6 | 25 | 3 | 3 | 10 | 0.72 |
| TM onset (min) | 35 | 8 | 5 | 10 | 25 | 8 | 5 | 15 | 0.96 |
| Duration of surgery (min) | 35 | 70 | 30 | 120 | 25 | 55 | 20 | 90 | 0.05 |
BMI body mass index, VAS visual analogue scale, TS onset onset time of sensory blockade, TM onset onset time of motor blockade; P < 0.05
Table 2.
Comparison of postoperative pain level and analgesia duration
| Group 1 | Group 2 | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Median | Minimum | Maximum | No. | Median | Minimum | Maximum | ||
| VAS 1 h postop | 35 | 1 | 1 | 1 | 25 | 1 | 1 | 2 | 0.002 |
| VAS 6 h postop | 35 | 1 | 1 | 1 | 25 | 1 | 1 | 3 | 0.0001 |
| VAS 12 h postop | 35 | 1 | 1 | 1 | 25 | 2 | 1 | 5 | – |
| VAS 24 h postop | 35 | 1 | 1 | 1 | 25 | 3 | 1 | 5 | – |
| TM offset (min) | 35 | 1,200 | 690 | 1,800 | 25 | 700 | 420 | 1,140 | – |
| TS offset (min) | 35 | 1,260 | 930 | 1,600 | 25 | 600 | 360 | 1,200 | – |
| TA (min) | 35 | 1,260 | 930 | 1,600 | 25 | 600 | 360 | 1,200 | – |
VAS visual analogue scale, postop postoperative, TM offset offset time of motor blockade, TS offset offset time of sensory blockade, TA total analgesia; P < 0.05
Fig. 1.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram of participants
Discussion
Our results showed significantly prolonged analgesia effect when low-dose dexamethasone was added to levobupivacaine compared with levobupivacaine alone. This resulted in lower pain levels where, at 24 hours, only two patients in group 1 required additional IV administration of analgesics compared with 17 in group 2. Our findings generally correlate well with other recently published investigations, such as those by Tandoc et al. and Cummings et al., who reported that the addition of dexamethasone to bupivacaine significantly prolonged the analgesia duration following interscalene blockade [2, 11]. However, making direct comparisons is difficult because of the different local anaesthetic used and different blockades studied. We performed US-guided supraclavicular blockade using levobupivacaine and low-dose dexamethasone. Tandoc et al. investigated analgesia duration with a bupivacaine and dexamethasone mixture with an interscalene blockade. Cummings et al. investigated bupivacaine or ropivacaine in a mixture with high-dose dexamethasone for interscalene blockade. When performing supraclavicular blockade, Parrington et al. used mepivacaine with high-dose dexamethasone and observed prolonged analgesia (332 min. vs. 228 min.). This analgesia time is still too short to avoid IV administration of analgesics during the first 24 hours postoperatively [1]. Also, the technique used to perform the blockade in their study was different. We used US guidance with confirmation of nerve stimulation. The safety of perineural administration of dexamethasone still raises some concerns. In animal studies, dexamethasone reduced blood flow to normal nerves for four hours after topical application [12]. Intrafascicular injection of dexamethasone can produce a harmful effect on nerve fibres, but there were no reports of long-term local effects on peripheral nerves [13]. Future investigation for possible late-onset neuropathy needs to be done. In the light of current findings, we used low-dose dexamethasone in order to attenuate the possibility of neurological complications but to prolong analgesia for the first 24 hours.
A possible limitation of our study is that long-term follow-up was not performed. It is possible, however, for our patients to self-report any untoward reaction that can mimic late-onset neuropathy, but for future investigation, it will be advisable to establish continuous follow-up using survey questionnaires and periodic checking for a longer period.
On the basis of our results, we suggest a clear protocol for practice using our procedure. Major indications for this treatment include elective and trauma surgery of the upper arm, forearm, elbow and hand. US-guided single-shot supraclavicular blockade using a mixture of low-dose dexamethasone and levobupivacaine can be performed in the operative setting 30 minutes prior to surgery. During the first 24 hours postoperatively, the technique will achieve successful pain therapy and avoid the need for intravenous analgesic. If necessary, and according to patient postoperative pain scores after 24 hours, additional analgesics can be administered orally.
Acknowledgments
Conflict of interest
None.
References
- 1.Parrington SJ, O'Donnell D, Chan VW, Brown-Shreves D, Subramanyam R, Qu M, Brull R. Dexamethasone added to mepivacaine prolongs the duration of analgesia after supraclavicular brachial plexus blockade. Reg Anesth Pain Med. 2010;35:422–426. doi: 10.1097/AAP.0b013e3181e85eb9. [DOI] [PubMed] [Google Scholar]
- 2.Tandoc MN, Fan L, Kolesnikov S, Kruglov A, Nader ND. Adjuvant dexamethasone with bupivacaine prolongs the duration of interscalene block: a prospective randomized trial. J Anesth. 2011;25:704–709. doi: 10.1007/s00540-011-1180-x. [DOI] [PubMed] [Google Scholar]
- 3.Grossi P, Allegri M. Continuous peripheral nerve blocks: state of the art. Curr Opin Anaesthesiol. 2005;18:522–526. doi: 10.1097/01.aco.0000182562.40304.ac. [DOI] [PubMed] [Google Scholar]
- 4.Litz RJ, Vicent O, Wiessner D, Heller AR. Misplacement of the psoas compartment catheter in the subarachnoidal space. Reg Anesth Pain Med. 2004;29:60–64. doi: 10.1016/j.rapm.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesthesia. 2010;65:608–624. doi: 10.1111/j.1365-2044.2009.06231.x. [DOI] [PubMed] [Google Scholar]
- 6.Drager C, Benziger D, Gao F, Berde CB. Prolonged intercostal nerve blockade in sheep using controlled-release of bupivacaine and dexamethasone from polymer microspheres. Anesthesiology. 1998;89:969–979. doi: 10.1097/00000542-199810000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Glasser RS, Knego RS, Delashaw JB, Fessler RG. The perioperative use of corticosteroids and bupivacaine in the management of lumbar disc disease. J Neurosurg. 1993;78:383–387. doi: 10.3171/jns.1993.78.3.0383. [DOI] [PubMed] [Google Scholar]
- 8.Kopacz DJ, Lacouture PG, Wu D, Nandy P, Swanton R, Landau C. The dose response and effects of dexamethasone on bupivacaine microcapsules for intercostal blockade (T9 to T11) in healthy volunteers. Anesth Analg. 2003;96:576–582. doi: 10.1097/00000539-200302000-00050. [DOI] [PubMed] [Google Scholar]
- 9.Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–267. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 10.Kim YJ, Lee GY, Kim DY, Kim CH, Baik HJ, Heo S. Dexamathasone added to levobupivacaine improves postoperative analgesia in ultrasound guided interscalene brachial plexus blockade for arthroscopic shoulder surgery. Korean J Anesthesiol. 2012;62:130–134. doi: 10.4097/kjae.2012.62.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cummings KC, 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, Sessler DI. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011;107:446–453. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 12.Shishido H, Kikuchi S, Heckman H, Myers RR. Dexamethasone decreses blood flow in normal nerves and dorsal nerve ganglia. Spine. 2002;27:581–586. doi: 10.1097/00007632-200203150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Mackinnon SE, Hudson AR, Gentili F, Kline DG, Hunter D. Peripheral nerve injection injury with steroid agents. Plast Reconstr Surg. 1982;69:482–490. doi: 10.1097/00006534-198203000-00014. [DOI] [PubMed] [Google Scholar]