Abstract
Purpose
The aim of this study was to analyse the clinical and radiological outcomes of unilateral versus bilateral instrumented TLIF in two-level degenerative lumbar disorders.
Methods
A prospective randomised clinical study was performed from January 2008 to May 2011. Sixty-eight consecutive patients with severe low back pain and radicular pain were divided randomly into the unilateral (n = 33) or bilateral (n = 35) pedicle screw fixation group based on a random number list. Operative time, blood loss, duration of hospital stay, fusion rate, complication rate and implant costs were recorded and analysed statistically. Visual analog scale (VAS) scores, Oswestry Disability Index (ODI), and SF-36 were used to assess the preoperative and postoperative clinical results in the two groups.
Results
No differences were observed between the two groups with respect to demographic data. The patients of the two groups had significant improvement in functional outcome compared to preoperatively. There was no significant difference comparing fusion rate, complication rate and duration of hospital stay between the two groups at postoperative follow-up (P > 0.05). However, compared with the bilateral pedicle screw group, a significant decrease occurred in operative time, blood loss and implant costs in the unilateral group.
Conclusion
Two-level unilateral instrumented TLIF is an effective and safe method with reduced operative time and blood loss for multiple-level lumbar diseases. But it is imperative that the larger cage should be appropriately positioned to support the contralateral part of the anterior column by crossing the midline of the vertebral body.
Keywords: Unilateral or bilateral transforaminal lumbar interbody fusion, Two level lumbar disease, Prospective, Randomised
Introduction
Spinal-fusion surgery for the treatment of instability and deformity is considered to be effective for some degenerative spine disorders, such as spondylolisthesis, spinal stenosis associated with deformities or discogenic pain identified by provocative discography [1]. Advantages of restoring disk height, immobilising the unstable segment and restoring load bearing to anterior structures can be achieved by lumbar interbody fusion [2]. Nowadays, TLIF is a popular lumbar interbody fusion technique to perform anterior interbody fusion with less neural retraction through a single unilateral approach [3–5]. Pedicle screws and intervertebral cage devices, which can provide initial stability, have been developed to correct deformity, improve the rate of fusion and speed the recovery of patients after surgery. Patients with greater numbers of implants, however, had a higher rate of implant-related complications, more extensive dissection, greater blood loss and a longer operative time involving greater costs [1, 6]. Traditionally, an open approach is required, using bilateral pedicle screw/rod fixation to provide stability as the gold standard. However, the increased stiffness of the fused segments will reduce the bone mineral content in adjacent vertebrae, and biomechanical studies have indicated that increased stress at the levels adjacent to the fusion may increase adjacent segment pathology (ASP) [7–10]. Therefore, unilateral pedicle screw fixation had been considered as a means to decrease the stiffness of the instrumented segment.
Suk et al. and Fernandez-Fairen et al. concluded that no difference exists in long-term radiographic or clinical outcome between bilateral and unilateral instrumentation in posterolateral fusion [11, 12]. More recently, bilateral and unilateral pedicle screw fixation techniques have been used in minimally invasive surgery (MIS) [6]. In view of the disadvantages in relation to posterior spinal instrumentation, it might be reasonable to decrease the stiffness of the implant and achieve reliable fusion with fewer pedicle screws [13]. In addition, the cost-effectiveness of this approach is worthy of attention [14–16]. Recently, researchers have shown that unilateral instrumented spinal fusion provides comparable results and is as effective as bilateral fixation. However, these studies are mainly case reports in one-segment lumbar interbody fusion. Although several reports of two-level unilateral instrumented lumbar interbody fusion have been described in various studies, they were mixed with one-level cases and fewer cases were involved.
To our knowledge, few prospective randomised studies comparing unilateral versus bilateral instrumented TLIF in two-level lumbar degenerative diseases have been reported. The rationale for this research is based on the one-level unilateral instrumentation providing sufficient stability for a good fusion environment. The purpose of this prospective randomised study was to compare clinical and radiographic outcomes in a series of patients with two-level lumbar degenerative diseases treated with unilateral or bilateral pedicle screw instrumented TLIF.
Materials and methods
This study was approved by the Committee of Medical Ethics and the institutional review boards of our hospital. Sixty-eight consecutive patients with severe low back pain and radicular pain having undergone at least six months of non-operative management were divided randomly into the unilateral or bilateral pedicle screw fixation groups based on a random number list from January 2008 to May 2011. Thirty-three were randomly enrolled in the unilateral fixation group and 35 were assigned to the bilateral fixation group. A single surgeon (J. Zhao) performed the surgeries and was blinded to the group until the beginning of the surgery.
The demographic data and procedure data of the patients are listed in Table 1. Indications for surgery were: (1) severe spinal stenosis with degenerative disc disease combined with instability, (2) one-level spondylolisthesis (grade I) and adjacent spinal stenosis requiring facetectomy and fusion, (3) previous spinal surgery needing surgical revision, such as recurrent lumbar disc herniation and symptomatic adjacent segment pathology. Patients who had active infection, metabolic disease, severe osteoporosis, gross obesity and symptomatic vascular disease were not included in our study.
Table 1.
Patient characteristics
| Parameter | Unilateral fixation group | Bilateral fixation group | P |
|---|---|---|---|
| No. of patients | 33 | 35 | |
| Age (years)a | 59.4 ± 10.2 | 55.7 ± 11.6 | 0.171 |
| Sex (F/M)b | 19/14 | 25/10 | 0.232 |
| Symptom duration | 8.5 months to 12 years | 11 months to 18 years | NS |
| Diagnosisb | |||
| Spinal stenosis | 11 | 16 | 0.297 |
| Symptomatic DDD | 13 | 9 | 0.228 |
| Spondylolisthesis | 5 | 7 | 0.600 |
| Failed back surgery | 4 | 3 | 0.705 |
| Operated level, No.b | |||
| L4-S1 | 20 | 23 | 0.662 |
| L3-L5 | 12 | 10 | 0.492 |
| L2-L4 | 1 | 2 | 1.00 |
| Operation time (min)a | 208 (126–275) | 257 (158–300) | 0.000 |
| Blood loss (ml)a | 391 (230–780) | 546 (310–980) | 0.000 |
| Hospital stay(days)a | 12.5 (7–21) | 13.7 (8–18) | 0.134 |
M male, F female, DDD degenerative disk disease, NS not significant
a Data were compared by t test
b Data were compared by chi-square test
Surgical techniques
The patient was placed in the prone position and general anaesthesia was used. The location of the interbody level was identified using a C-arm image intensifier. The local autograft and Capstone cages (Medtronic Sofamor Danek, Memphis, Tennessee) and pedicle screws (Legacy; Medtronic Sofamor Danek) were used in the surgery.
Unilateral fixation group
The soft tissues on the symptomatic side were split and unilateral laminectomy and facetectomy were mainly performed. Adequate decompression could be accomplished simultaneously. If necessary, bilateral decompression could be performed through the laminectomy window. Multiaxial screws and rod were used unilaterally, and then the discectomy and endplate preparation were performed. The original disk space height was restored as much as possible by sequentially distracting the disk space, and the distracted space was maintained using ipsilateral pedicle screws. The disc space was filled with morsellised bone from the facetectomy and laminectomy, after the cage was inserted obliquely.
Bilateral fixation group
A standard technique was carried out with bilateral pedicle screw fixation and cages. Decompression was mainly performed on the symptomatic side. The contralateral facet joint was exposed in a standard Wiltse muscle splitting approach and pedicle screws were placed.
Assessment of results including clinical and radiological outcomes
Perioperative parameters including sex, age, operative time, blood loss, duration of hospital stay, complication rate and implant costs were recorded and compared between the unilateral or bilateral fixation groups. The patients were asked to return for follow-up at three, six, and 12 months after operation and annually thereafter. VAS, ODI, and SF-36 scores were used to assess the clinical and radiological outcomes in the two groups preoperatively and postoperatively.
Radiological assessments were used to evaluate fusion status, screw failure, and other complications. X-ray films (anteroposterior and lateral flexion-extension) were used to evaluate fusion status. Bone bridging the disk space without lucency and less than 4° of angular motion on flexion-extension views between the fused segments were considered as solid fusion [20, 21]. Three-dimensional CT scan radiographs were used to more accurately evaluate the fusion status every year postoperatively. All images were independently measured by at least two experienced radiologists.
Statistical analysis
Statistical analysis was performed using SPSS 17.0 (SPSS Inc, Chicago, IL). Demographic data (gender, preoperative index diagnosis, degenerated segment, and level of fusion) were compared by chi-square test. Patient age, operative time, blood loss, hospital stay and implant costs were compared by Student’s t test. Functional outcomes (VAS, ODI, and SF-36) were compared before and after treatment by an unpaired t test. Fusion rates and complication rates were compared by chi-square and Fisher’s exact tests. A P-value <0.05 was considered to be significant.
Results
All patients were followed up for an average 25.6 months (range, 18–36 months). There were no significant differences between the two groups in patient demographics. The unilateral fixation group had a shorter operative time and less blood loss than the bilateral fixation group (P < 0.01) (Table 1). Implant costs in the unilateral fixation group were lower than those in the bilateral fixation group ($5,848.7 ± 19.5 vs $8,568.8 ± 70.5).
There was a significant difference comparing preoperative and postoperative VAS, ODI and SF-36 scores in both groups (P < 0.05). There was no significant difference comparing VAS, ODI and SF-36 scores between the two groups at postoperative follow-up (P > 0.05) (Table 2).
Table 2.
VAS (back and leg pain), ODI and SF-36 test results
| Test | Preoperative | 6 months | 12 months | 24 months |
|---|---|---|---|---|
| VAS back | ||||
| Unilateral | 7.8 ± 0.8 | 2.3 ± 0.9 | 2.1 ± 1.8 | 2.1 ± 0.8 |
| Bilateral | 8.1 ± 0.7 | 2.3 ± 0.7 | 2.4 ± 2.6 | 2.0 ± 1.8 |
| VAS leg | ||||
| Unilateral | 7.4 ± 2.8 | 2.1 ± 1.7 | 2.2 ± 1.1 | 1.9 ± 1.4 |
| Bilateral | 7.1 ± 1.3 | 2.2 ± 0.9 | 2.0 ± 1.5 | 2.0 ± 1.3 |
| ODI | ||||
| Unilateral | 42.4 ± 16 | 20.6 ± 15.1 | 18.6 ± 5.7 | 18.8 ± 3.2 |
| Bilateral | 44.3 ± 18.2 | 21.8 ± 16.4 | 19.8 ± 8.3 | 17.9 ± 7.6 |
| SF-36 | ||||
| PF | ||||
| Unilateral | 16.7 ± 6.2 | – | 45.6 ± 9.0 | 47.2 ± 15.2 |
| Bilateral | 15.8 ± 2.5 | – | 44.1 ± 11.0 | 46.1 ± 12.7 |
| GH | ||||
| Unilateral | 49.6 ± 13.4 | – | 58.4 ± 10.4 | 57.8 ± 16.5 |
| Bilateral | 51.8 ± 8.3 | – | 57.6 ± 11.0 | 58 ± 13.3 |
| MH | ||||
| Unilateral | 51.3 ± 16.2 | – | 69.1 ± 15.5 | 71.5 ± 18 |
| Bilateral | 50.4 ± 11.8 | – | 69.9 ± 17.4 | 72.6 ± 21.2 |
PF physical function, GH general health, MH mental health
Data presented as mean±SD. Difference significant (P < 0.01) pre- and postoperatively in both groups. Difference not significant between outcomes at 12- and 24-months follow-up for each subscale
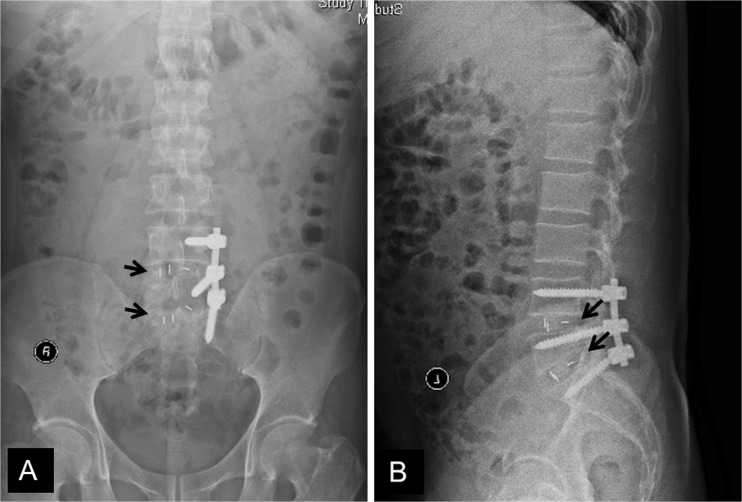
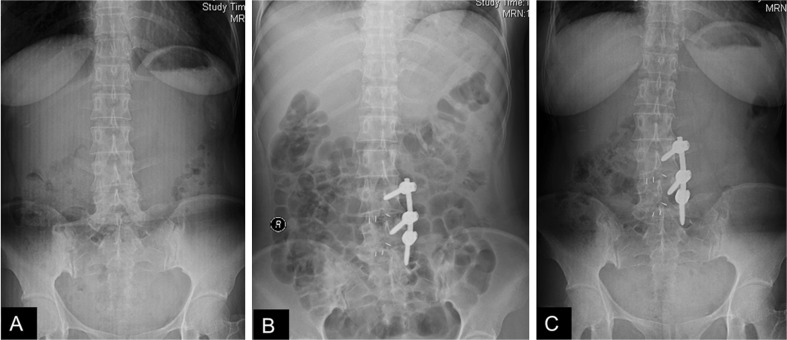
Radiological assessment (Fig. 1) showed that there was no significant difference in fusion rate, respectively 90.91 % (unilateral fixation group) vs 94.29 % (bilateral fixation group) (p > 0.05). Screw malposition was found in one case in the bilateral fixation group by CT examination but the patient had no symptoms of nerve compression. No other device-related complications, such as hardware loosening or breakage, or fusion cage migration, occurred in either group. Proximal scoliosis was found in one case postoperatively in the unilateral fixation group (Fig. 2). Neither group showed screw breakages. No significant difference in general complications was found between the two groups (P > 0.05). Two cases suffered from superficial wound infection in the bilateral group and one case in the unilateral group. There was one case of laceration of the dural sac in each group.
Fig. 1.
Follow-up anteroposterior and lateral radiographs of a 41-year-old man with L4-L5-S1 lumbar stenosis treated with decompression, interbody fusion, and unilateral pedicle screw fixation
Fig. 2.
A 73-year-old woman with L4-L5-S1 lumbar stenosis was found with proximal scoliosis three months after operation
Discussion
Spinal fusion surgery is an effective treatment in the management of painful degenerative lumbar disc diseases. Spinal instrumentation, such as pedicle screw and cage, play an important role by achieving a higher fusion rate. However, there are some disadvantages such as a larger surgical exposure, greater blood loss, a higher likelihood of reoperation, nerve injury, etc. [17–19]. Some clinical and biomechanical studies on the suitability of unilateral pedicle screw fixation have demonstrated that reliable fusion with fewer pedicle screws can be achieved [11–13, 20–23]. Therefore, the need for unilateral or bilateral instrumentation is a matter for debate.
Unilateral pedicle screw fixation has been previously studied biomechanically and clinically. Some biomechanical studies using cadaver specimens have indicated that the unilateral instrumented TLIF procedure provides less rotational stability and stiffness than bilateral pedicle screw fixation, but whether the more rigid fixation is needed was controversial [8, 23]. Encouraging results can be achieved by unilateral fixation with an anterior supporting device such as an interbody cage [23]. Several randomised controlled clinical trials have shown that there is no clinical benefit from bilateral over unilateral instrumentation in posterolateral fusion alone. The main benefits of unilateral fixation seem to be less blood loss and muscle dissection, shorter operative time and hospital stay, lower medical cost, and fewer complications related to implants [12, 20, 21, 24]. These results were also observed in our study. Functional outcomes including VAS, ODI and SF-36 scores after operation also showed significant improvement. Our previous prospective randomised study showed that the effect of unilateral pedicle screw fixation is comparable to that of bilateral pedicle screw fixation in one- or two-level interbody fusion with one cage for lumbar degenerative diseases without major instability. This study revealed that unilateral instrumented TLIF in two-level degenerative lumbar disorders is effective and safe.
Some studies have suggested that unilateral instrumentation should not be applied in multilevel fusion because of its inadequate fixation strength. Some authors have reported two-level unilateral instrumented spinal fusion. Suk reported 15 cases (15/47) with two-level posterolateral fusion, but the fusion rate was not clearly recorded [11]. In a prospective randomised study of posterolateral arthrodesis, the failed fusion rate of two-level fusion was 18.75 (3/16) in the unilateral group, whereas it was 18.18 (2/11) in the bilateral group [12].
That conclusion was based on studies using unilateral pedicle screw fixation without anterior support devices and specimens with extensive destruction of soft tissue structures. That is to say, they did not study the efficacy of anterior support devices such as interbody cages. It should be emphasised that interbody techniques for this situation play an important role. The cage itself distracts the intervertebral space as an anterior support device. Recently, a study of unilateral versus bilateral instrumented TLIF in degenerative lumbar diseases has revealed that the fusion rates of double-level fusion in the unilateral and bilateral group were 87.5 % (7/8) and 91.2 % (11/12), respectively [21]. Thus, we performed discectomy and an interbody device to improve the biomechanical soundness of unilateral fixation. In our previous and present study, we obtained identical radiographic and clinical results between the two groups. Unilateral fixation can therefore provide adequate stability for a good fusion environment in a double-level process. Taking into account the published articles and our study, we suggest that unilateral pedicle screw fixation with reliable anterior support can be used in two-level lumbar disease. Placing fewer screws is possible with somewhat favourable results regarding reduced operative time, blood loss, implant cost and screw-related complications.
Lumbar interbody fusion can reach almost 100 % fusions, whereas the fusion rate of posterolateral arthrodesis with unilateral fusion ranges between 90 % and 97 %, especially with a lower rate in two-level fusion [11–13, 25]. In this study, we found that the fusion rate of two-level fusion in the unilateral fixation group was similar to that in the bilateral fixation group (90.91 % vs 94.29 %).
In addition, the unilateral approach only dissected one side of the paravertebral muscles and it was not necessary to expose the contralateral bone structure. Therefore, less soft tissue and bone damage allows the patient to achieve early recovery and rehabilitation. Furthermore the operative time and blood loss are reduced.
This study has several important limitations. Considering different diagnoses in the two groups, the sample size in this study was relatively small, which may limit the comparability and outcomes. Furthermore, less rigid unilateral fixation is considered to reduce the possibility of adjacent segment pathology, but no radiological signs of adjacent segment pathology existed in either group. A possible reason was that follow-up periods were not long enough to confirm the results. Further multicentre studies with more patients and longer follow-up should be performed.
Conclusion
Unilateral instrumented TLIF with cages is an effective and safe method of treating two-level lumbar disease, which can take less operative time, reducing blood loss and hospital stay and implant costs. But it should be kept in mind that the larger cage should be appropriately positioned to support the contralateral part of the anterior column by crossing the midline of the vertebral body. Further well-designed prospective randomized studies and a longer period of follow-up are needed to confirm this conclusion.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (grant no. 81071453, 81071503), Program for Innovative Research Team of Shanghai Municipal Education Commission (Phase II).
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Drs. Zhang Kai and Sun Wei contributed equally to this study.
References
- 1.Deyo RA, Nachemson A, Mirza SK. Spinal-fusion surgery - the case for restraint. N Engl J Med. 2004;350:722–726. doi: 10.1056/NEJMsb031771. [DOI] [PubMed] [Google Scholar]
- 2.Zdeblick TA, Phillips FM. Interbody cage devices. Spine (Phila Pa 1976) 2003;28:S2–S7. doi: 10.1097/01.BRS.0000076841.93570.78. [DOI] [PubMed] [Google Scholar]
- 3.Lowe TG, Tahernia AD, O’Brien MF, Smith DA. Unilateral transforaminal posterior lumbar interbody fusion (TLIF): indications, technique, and 2-year results. J Spinal Disord Tech. 2002;15:31–38. doi: 10.1097/00024720-200202000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J. 2005;14:551–558. doi: 10.1007/s00586-004-0830-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lowe TG, Tahernia AD (2002) Unilateral transforaminal posterior lumbar interbody fusion. Clin Orthop Relat Res 394:64–72 [DOI] [PubMed]
- 6.Kim CW, Siemionow K, Anderson DG, Phillips FM. The current state of minimally invasive spine surgery. J Bone Joint Surg. 2011;93:582–596. [PubMed] [Google Scholar]
- 7.Lee MJ, Dettori JR, Standaert CJ, Ely CG, Chapman JR. Indication for spinal fusion and the risk of adjacent segment pathology: does reason for fusion affect risk? A systematic review. Spine (Phila Pa 1976) 2012;37:S40–S51. doi: 10.1097/BRS.0b013e31826ca9b1. [DOI] [PubMed] [Google Scholar]
- 8.Goel VK, Lim TH, Gwon J, Chen JY, Winterbottom JM, Park JB, Weinstein JN, Ahn JY. Effects of rigidity of an internal fixation device. A comprehensive biomechanical investigation. Spine (Phila Pa 1976) 1991;16:S155–S161. doi: 10.1097/00007632-199103001-00023. [DOI] [PubMed] [Google Scholar]
- 9.Nagata H, Schendel MJ, Transfeldt EE, Lewis JL. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976) 1993;18:2471–2479. doi: 10.1097/00007632-199312000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Shono Y, Kaneda K, Abumi K, McAfee PC, Cunningham BW. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine (Phila Pa 1976) 1998;23:1550–1558. doi: 10.1097/00007632-199807150-00009. [DOI] [PubMed] [Google Scholar]
- 11.Suk KS, Lee HM, Kim NH, Ha JW. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine (Phila Pa 1976) 2000;25:1843–1847. doi: 10.1097/00007632-200007150-00017. [DOI] [PubMed] [Google Scholar]
- 12.Fernandez-Fairen M, Sala P, Ramirez H, Gil J. A prospective randomized study of unilateral versus bilateral instrumented posterolateral lumbar fusion in degenerative spondylolisthesis. Spine (Phila Pa 1976) 2007;32:395–401. doi: 10.1097/01.brs.0000255023.56466.44. [DOI] [PubMed] [Google Scholar]
- 13.Kabins MB, Weinstein JN, Spratt KF, Found EM, Goel VK, Woody J, Sayre HA. Isolated L4-L5 fusions using the variable screw placement system: unilateral versus bilateral. J Spinal Disord. 1992;5:39–49. doi: 10.1097/00002517-199203000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Fritzell P, Hagg O, Jonsson D, Nordwall A. Cost-effectiveness of lumbar fusion and nonsurgical treatment for chronic low back pain in the Swedish Lumbar Spine Study: a multicenter, randomized, controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 2004;29:421–434. doi: 10.1097/01.BRS.0000102681.61791.12. [DOI] [PubMed] [Google Scholar]
- 15.Cahill KS, Wang MY. Cost effectiveness of lumbar fusion improves with time. Neurosurgery. 2012;70:N21. doi: 10.1227/01.neu.0000410938.46452.b6. [DOI] [PubMed] [Google Scholar]
- 16.Andres TM, Park JJ, Ricart Hoffiz PA, McHugh BJ, Warren DT, Errico TJ. Cost analysis of anterior-posterior circumferential fusion and transforaminal lumbar interbody fusion. Spine J. 2013;13:651–656. doi: 10.1016/j.spinee.2012.11.055. [DOI] [PubMed] [Google Scholar]
- 17.Bridwell KH, Sedgewick TA, O’Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993;6:461–472. doi: 10.1097/00002517-199306060-00001. [DOI] [PubMed] [Google Scholar]
- 18.Zhao J, Hou T, Wang X, Ma S. Posterior lumbar interbody fusion using one diagonal fusion cage with transpedicular screw/rod fixation. Eur Spine J. 2003;12:173–177. doi: 10.1007/s00586-001-0376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fritzell P, Hagg O, Wessberg P, Nordwall A. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 2001;26:2521–2532. doi: 10.1097/00007632-200112010-00002. [DOI] [PubMed] [Google Scholar]
- 20.Xie Y, Ma H, Li H, Ding W, Zhao C, Zhang P, Zhao J. Comparative study of unilateral and bilateral pedicle screw fixation in posterior lumbar interbody fusion. Orthopedics. 2012;35:e1517–e1523. doi: 10.3928/01477447-20120919-22. [DOI] [PubMed] [Google Scholar]
- 21.Xue H, Tu Y, Cai M. Comparison of unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in degenerative lumbar diseases. Spine J. 2012;12:209–215. doi: 10.1016/j.spinee.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 22.Cunningham BW, Polly DW Jr (2002) The use of interbody cage devices for spinal deformity: a biomechanical perspective. Clin Orthop Relat Res 394:73–83 [DOI] [PubMed]
- 23.Chen HH, Cheung HH, Wang WK, Li A, Li KC. Biomechanical analysis of unilateral fixation with interbody cages. Spine (Phila Pa 1976) 2005;30:E92–E96. doi: 10.1097/01.brs.0000153703.80747.16. [DOI] [PubMed] [Google Scholar]
- 24.Rihn JA. Commentary: is bilateral pedicle screw fixation necessary when performing a transforaminal lumbar interbody fusion? An analysis of clinical outcomes, radiographic outcomes, and cost. Spine J. 2012;12:216–217. doi: 10.1016/j.spinee.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Beringer WF, Mobasser JP. Unilateral pedicle screw instrumentation for minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus. 2006;20:E4. [PubMed] [Google Scholar]