Abstract
Purpose
This study was designed to evaluate whether the mechanical axis deviation (MAD) of the leg correlates with an increased hip alpha angle as described by Nötzli, which is associated with femoroacetabular impingement (FAI).
Methods
In a retrospective analysis, standing full-length anteroposterior radiographs were analysed in patients who suffered from symptomatic leg alignment. The study included 85 radiographs of 80 patients with an average age of 43.11 years (range 18–60 years). Five patients underwent a bilateral long-leg X-ray examination. All radiographs were transferred as Digital Imaging and Communications in Medicine data files from the Picture Archiving and Communications System into the OrthoPlanner software version 2.3.2. The radiographs were measured by one orthopaedic surgeon and one independent radiologist.
Results
The mean value of the alpha angle of Nötzli was 61.43° (49.07–74.04°). A total of 57 (67 %) radiographs showed a varus deviation, 25 (29.5 %) had a valgus malalignment and three (3.5 %) a straight leg axis. Of 82 radiographs, 40 (48.8 %) had a moderate axis deviation with a MAD <15 or > − 15 mm and a mean alpha angle of 57.81°, and 42 (51.2 %) with extended axis deviation of a MAD > 15 or < − 15 mm had a mean alpha angle of 62.93°; 40 (95.2 %) of these 42 showed an alpha angle > 55°. The alpha angle was significantly increased in extended axis deviation compared to moderate axis deviation (P = 0.001).
Conclusions
This study confirmed that increased alpha angles were found significantly at higher degrees of axis deviation on the full-length radiograph. In cases of a MAD >15 or < − 15 mm and symptomatic coxalgia, diagnostic tests must be pursued for FAI.
Keywords: Alpha angle of Nötzli, Full-length radiograph, Mechanical axis deviation, Femoroacetabular impingement, Hip arthrosis
Introduction
Hip osteoarthritis is one of the major challenges affecting our aging population [1]. Health services will have to face increasing economic costs due to hip osteoarthritis in the coming years [1]. Femoroacetabular impingement (FAI) represents a novel approach to the mechanical aetiology of hip osteoarthritis [2, 3]. A large proportion of idiopathic hip osteoarthritides can be traced back to FAI; thus early diagnosis is very important [4, 5]. In the pathogenesis of FAI, an anatomical deformity at the proximal end of the femur or the acetabulum or in both structures is essential. An acetabular type of FAI (pincer impingement) is anatomically distinguished from the femoral type (cam impingement) [6]. Pincer impingement is caused by an immoderate acetabular cover of the femoral head and is linked with acetabular retroversion [7], coxa profunda or protrusio acetabuli [8]. Cam impingement results from a prominence at the anterolateral femoral head-neck junction [9]. Causes for cam impingement are aspheric deformity of the femoral head, late closure of the femoral epiphysis, slipped capital femoral epiphysis and Legg-Calvé-Perthes disease [10–12].
X-ray of the hips is the first choice of imaging diagnostics after anamnesis and clinical examination. For the diagnostics of FAI, an anteroposterior (AP) pelvic radiograph and a second lateral or oblique view are necessary. Clohisy et al. [13] showed that the pathological alpha angle of Nötzli [9] is detected in a standing AP view. The alpha angle of Nötzli is defined as an angle between the femoral neck axis and a line connecting the head centre with the point of beginning asphericity of the head-neck outline [9]. The measurement of the alpha angle is an adequate parameter to assess the degree of femoral deformity and femoral head asphericity to evaluate the value of FAI [9, 14].
In a computed tomography (CT)-based study, Siebenrock et al. [15] showed that hips with coxa valga had a higher prevalence of impingement. Thus, it was tempting to investigate whether the mechanical axis deviation (MAD) of the leg affects the morphology of the hip, particularly concerning FAI. The purpose of our study was to investigate if the MAD correlated with a radiologically increased alpha angle in standing full-length AP radiographs and thus indicated the risk of FAI.
Materials and methods
Patients
This study follows the principles of the Declaration of Helsinki. In Germany, where this study was conducted, retrospective epidemiological studies without personally identifiable data do not need to be approved by the Ethics Committee. Between January 2010 and December 2012, 85 standing full-length radiographs of 80 patients (32 women and 48 men) were included in the study. Five patients underwent a bilateral long-leg X-ray examination. We analysed 41 (48.2 %) left and 44 (51.8 %) right radiographs. The full-leg radiographs had been performed previously to evaluate the mechanical axis for further conservative or surgical treatment of the knee (arthroscopy, cartilage surgery, osteotomy, total knee replacements, Table 1). Radiographs of patients with any previous kind of bone surgery (arthroplasty, osteotomy and osteosynthesis) for the lower limbs which could influence the mechanical axis were excluded from the study. The radiographs were divided into three groups based on the positive or negative extent of the MAD. In varus alignment of the mechanical axis, the MAD was defined as a positive value in millimeters (group 1, Fig. 1a, b). In cases of valgus position, the MAD was determined as a negative value (group 2, Fig. 2a, b). With a straight mechanical axis, the MAD was defined as a zero value (group 3, Fig. 3a, b). Table 2 details the group division.
Table 1.
Baseline demographics for 80 patients (85 radiographs)
| Variables | |
|---|---|
| Mean age, years (range) | 43.1 (18–60) |
| Gender, n (%) | |
| Male | 48 (60) |
| Female | 32 (40) |
| Side, n (%) | |
| Left | 41 (48.2) |
| Right | 44 (51.8) |
| Diagnosis, n (%) | |
| Medial OA | 35 (42.1) |
| Cartilage lesions | 15 (17.6) |
| Patellofemoral instability | 14 (16.1) |
| OA | 9 (10.5) |
| Lateral OA | 6 (7) |
| Meniscal tears | 6 (7) |
OA osteoarthritis
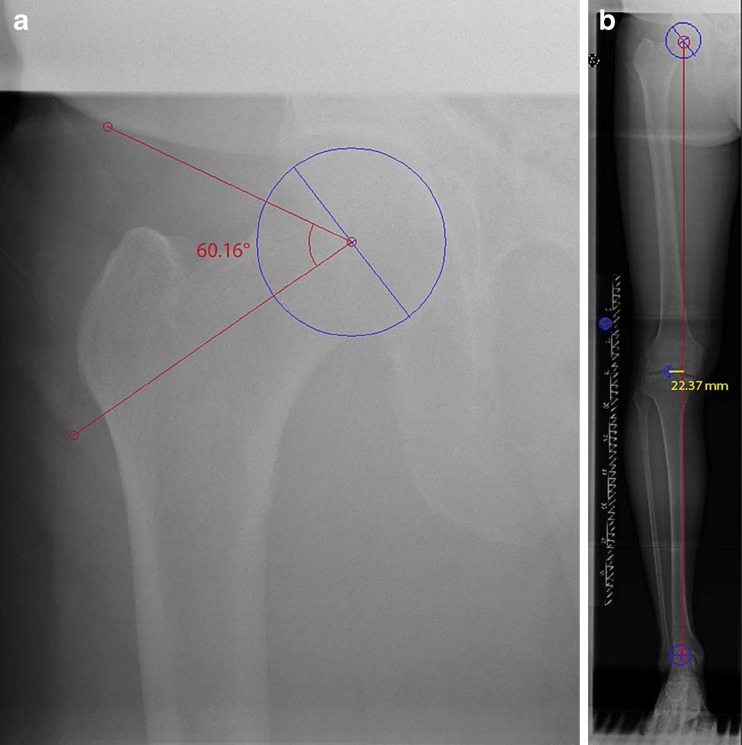
Fig. 1.
The alpha angle is formed by the connecting lines (red lines) between the longitudinal mid-axis of the femoral neck and the axis which marked the lateral departure of the radius of the femoral head (blue circle). The alpha angle was 60.16° in this example (a). The weight-bearing line (WBL) is defined as the connecting line (red line) between the femoral head centre and the centre of the ankle. The MAD was measured as a distance in millimetres, as an alignment from the centre of the knee to the vertical line of the WBL (yellow line). The MAD was 22.37 mm (b)
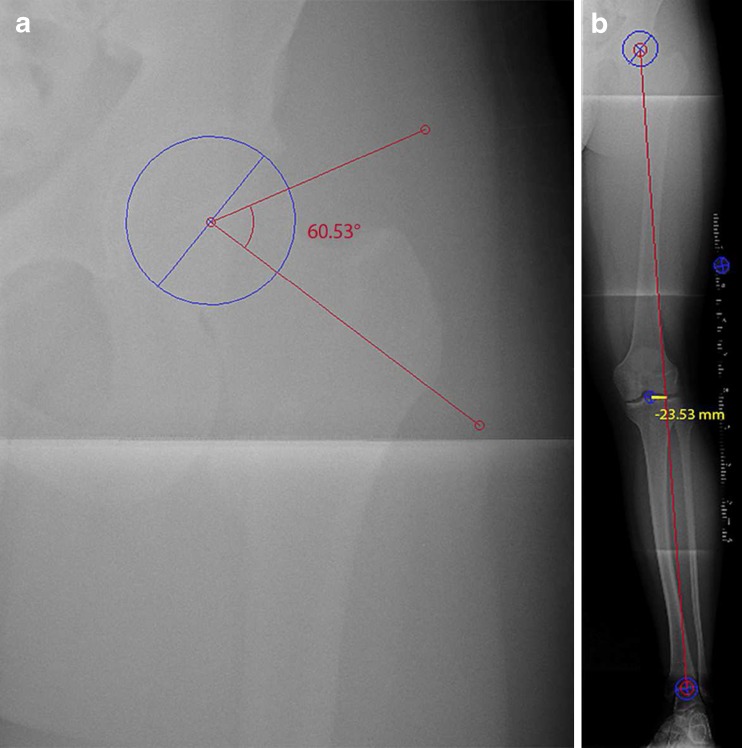
Fig. 2.
A radiograph of group 2. The alpha angle of the left hip was 60.53° in this example (a). The WBL was in valgus alignment and the MAD comprised −23.53 mm (b)
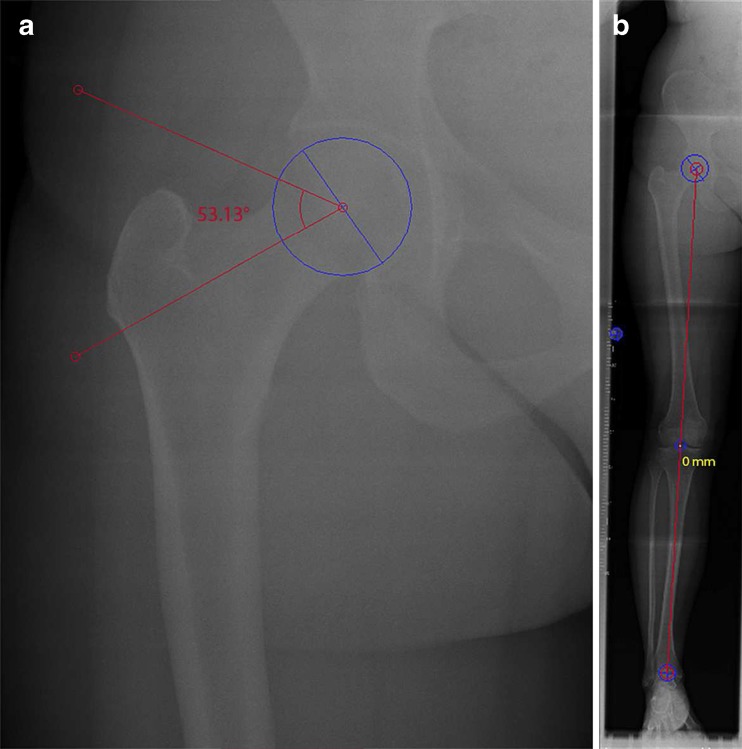
Fig. 3.
A radiograph of group 3. The alpha angle of the right hip was 53.13° in this example (a). The right leg showed a straight mechanical axis. The MAD was 0 mm (b)
Table 2.
Group division according to the extent of the MAD and proportion of radiographs in the subgroups
| Group division | Radiographs, n (%) | Mean ± SD (mm) | Mechanical axis |
|---|---|---|---|
| Group 1 | 57 (67) | 21.63 ± 18.18 (1.49–83.64) | Varus alignment |
| Group 2 | 25 (29.5) | −15.6 ± 11.62 (−48.66 to −1.29) | Valgus alignment |
| Group 3 | 3 (3.5) | 0 (0) | Neutral alignment |
Radiological examination
A standing AP radiograph was carried out with the patient facing the radiographic tube and the patellae pointing anteriorly. The patients loaded equally on both lower limbs. According to protocol, the radiographs were performed under free exposure to a tube voltage of 81 kV with an exposure value of 25 mAS and a focus film distance (FFD) of 180 cm. Source-to-leg and leg-to-film were continuous in all radiograms. For the calibration of the X-ray images, a spherical radiographic marker was placed in the middle of the lateral femur. The marker in the form of a ball is shown on the X-ray photographs as a circle with a specified overall diameter of 25 mm. All radiographs were transferred as Digital Imaging and Communications in Medicine (DICOM) data files from the Picture Archiving and Communications System (PACS version 3.0, VISUS, Bochum, Germany) into the OrthoPlanner software version 2.3.2 (LOCALITE Biomedical Visualization Systems, St. Augustin, Germany).
Radiological analysis
After transferring the files into the OrthoPlanner, a calibration of the transferred radiographs was performed by measuring the standardised marker. The calibration allows an accurate measurement of the dimension of the specific radiological anatomy. An orthopaedic surgeon (M.L.) and an independent radiologist (N.L.J.), both experienced in orthopaedic diagnostics, determined each radiograph for the following measuring points: (1) femoral head centre, by placing two marks at the superior and inferior zones of the femoral head to draw a circle (Figs. 1a, 2a and 3a); (2) longitudinal mid-axis of the femoral neck, by connecting to the centre of the femoral head from the femoral neck; (3) anterior point, where the distance from the centre transcended the radius of the subchondral surface of the femoral head; (4) weight-bearing line (WBL) is defined as the connecting line between the femoral head centre and the centre of the ankle (Figs. 1b, 2b and 3b), [16]; (5) MAD was evaluated as a distance in millimetres, as an alignment from the centre of the knee to the vertical line of the WBL. The alpha angle is formed by the mid-axis and the connecting line between the femoral head and the anterior point and was measured using the method described by Nötzli et al. [9]. Medial deviation with a MAD < 15 mm was defined as moderate varus malalignment and as extended deviation in MAD >15 mm (Fig. 1a, b). Lateral deviation with a MAD > − 15 mm of the WBL was defined as moderate valgus malalignment and as extended deviation in MAD < − 15 mm (Fig. 2a, b). In cases of a straight mechanical axis, the MAD was defined as a zero value (Fig. 3a, b).
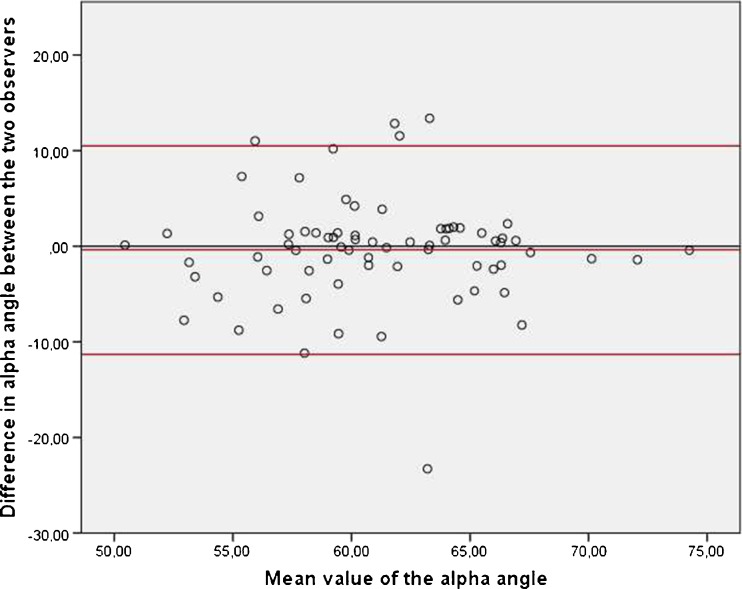
Statistical analysis
All examination results were recorded on a case report form. The selected patient cohort was grouped in an Excel file (version 2003, Microsoft Corporation, Seattle, WA, USA). Distribution of data was assessed by the D’Agostino-Pearson test. The arithmetic mean value, SD and 95 % confidence intervals (CI) were calculated for the variables above and measured with Microsoft Excel. The values were recorded in IBM SPSS Statistics 14 (PASW 14, SPSS Inc., Chicago, IL, USA). The measurements on the alpha angles and the MAD were compared using Student’s t test. Statistical significance was defined as a P value <0.05. An analysis of variance (ANOVA) was used to exclude a significant difference between the different groups (P = 0.014); the inhomogeneity of variance was excluded by the Levene test (P = 0.775). Bland-Altman plots were performed to illustrate a visual assessment of the alpha angle between the two observers (Fig. 4). For comparing the three groups, we performed Scheffé’s procedure due to the unequal group quantity. Validity between the two observers was calculated for comparing the alpha angle values and the MAD using Spearman’s correlation coefficient. We did a post hoc power analysis for comparing the alpha angles of the moderate with the extended axis deviation.
Fig. 4.
The Bland-Altman plot demonstrated the extent of accordance between the two observers
Results
Descriptive analysis
No significance difference of the arithmetic mean could be detected in the measurements of the alpha angles and the MAD by the two observers (M.L, J.L.J.). The mean value of the MAD was 8.51 ± 24.05 mm (−46.31 to 83.64 mm). A total of 57 (67 %) radiographs had a varus deviation, 25 (29.5 %) had a valgus malalignment and three (3.5 %) a straight leg axis (Table 2). Group 1 showed a mean MAD value of 21.63 ±18.18 mm (1.49–83.64 mm). Group 2 offered a mean MAD of −15.60 ± 11.62 mm (−48.66 to −1.29 mm). Of 82 radiographs, 40 (48.8 %) had a moderate axis deviation with a MAD <15 or > − 15 mm, and 42 (51.2 %) showed an extended axis deviation with a MAD >15 or < − 15 mm.
Comparison
In our study, the mean value of the alpha angle of Nötzli was 61.43 ± 5.33° (49.07–74.04°). Divided by gender, the mean alpha angle was 61.91 ± 5.59° (50.86–74.84) in men and 58.84 ± 3.37° (49.07–67.19°) in women. The highest values of alpha angle were detected in patients with extended varus or valgus alignment with a MAD >15 or < − 15 mm; 42 (51.2 %) radiographs with extended axis deviation had a mean alpha angle of 62.93 ± 4.43° (49.07–74.04°), and 40 (95.2 %) of these 42 radiographs showed an alpha angle >55° with a mean alpha angle of 63.42 ± 3.90° (51.70–71.35°). Of 82 radiographs with moderate axis deviation, 40 (48.8 %) had an alpha angle of 57.81 ± 5.04° (51.82–71.35°). The alpha angle was significantly increased in extended axis deviation compared to moderate axis deviation (P = 0.001). A power of 99.8 % was achieved in the post hoc analysis. Divided by groups of varus, valgus or straight alignment, the mean value of the alpha angle was 62.04 ± 5.02° (50.86–74.46°) in group 1. In group 2, the mean alpha angle was 59.43 ± 5.55° (49.07–74.84°). In comparison of the three groups, the lowest mean value of the alpha angle was 54.17 ± 4.86° (50.51–60.09°) in the cohort of patients with straight mechanical axis. The evaluation of the Bland-Altman plot demonstrated a sufficient symmetrical distribution of the mean values of the alpha angle (Fig. 4). The dotted lines demonstrate the two SDs and the majority of the measured alpha angles are located inside the lines. The alpha angles in group 1 were significantly higher than in group 3 (P = 0.045, Table 3). A significant difference could not be stated between groups 2 and 3 due to the low number of cases in group 3 and the low difference of the mean value (5.3 vs 7.9). The low mean difference (2.6 vs 7.9) between groups 1 and 2 was responsible for the non-existent statistical significance. The result of Scheffé’s procedure is presented in Table 3.
Table 3.
Comparison of the three groups
| Group (a) | Group (b) | Mean difference (a-b) | Standard error | P value | 95 % CI | |
|---|---|---|---|---|---|---|
| Minimum level | Maximum level | |||||
| 1 | 2 | 2.6146 | 1.3399 | 0.157 | −0.738 | 5.967 |
| 3 | 7.8726 | 3.0887 | 0.045 | 0.145 | 15.600 | |
| 2 | 1 | −2.6146 | 1.3399 | 0.157 | −5.967 | 0.738 |
| 3 | 5.2580 | 3.1922 | 0.264 | −2.728 | 13.244 | |
| 3 | 1 | −7.8726 | 3.0887 | 0.045 | −15.6 | −0.145 |
| 2 | −5.2580 | 3.1922 | 0.264 | −13.244 | 2.728 | |
Results of Scheffé’s procedure
Validity
In group 1, Spearman’s correlation coefficient was r = 0.403 between the alpha angle values and the MAD values (P = 0.01). In group 2, Spearman’s correlation coefficient was measured as r = −0.503 (P = 0.01). In group 3, the correlation coefficient could not be determined due to the small size of the group.
Discussion
The most important finding of this study is that the axis deviation in higher degrees correlates with increased hip alpha angles and could be a risk factor for FAI. The alpha angle in our radiographs with straight leg axis resembled the alpha angles found in AP pelvis radiographs of 1,055 symptomless men in the study of Gosvig et al. [17]. The authors showed that the alpha angles remained variable with ascending position of 20° internal and external rotation of the femur in a geometrical radiological analysis to a gradual measuring. However, the authors argued that in well-placed standardised AP radiographs a false-negative evaluation of the femoral head-neck junction was tolerable when excessive tilt of the pelvis and the hip was avoided.
Hack et al. [18] showed a prevalence of 14 % hips with increased alpha angles and cam morphology in 200 asymptomatic volunteers. The interesting part of our study is that we detected a higher proportion of elevated alpha angles in patients with varus or valgus alignment. In almost half of the cases, an increase in alpha angles >55° was identified in cases of MAD.
Asymptomatic patients without FAI have an alpha angle between 45 and 55° [19, 20]. An alpha angle >55° can be described as radiologically noticeable and an angle >55° is associated with FAI [9, 14, 20]. Symptomatic FAI can be treated by arthroscopy or open surgery [21]. Although the alpha angle was originally described from oblique axial sequences from magnetic resonance imaging (MRI) [9], an X-ray is known as an efficient diagnostic imaging procedure [13]. Therefore, the quality management of the radiographs plays an important role for the accurate image analysis. In the realisation of the standing full-length radiograph, the correct position of the leg is important for accurate measurement of the mechanical axis [22, 23]. The position of the femur is determined on the position of the minor trochanter. In cases of an internal axial rotation of the femur, the minor trochanter disappears behind the femoral cortical bone. In standing full-length radiographs, the patella should always be centred on the level of the knee joint [22].
Clohisy et al. [13] measured the alpha angle in the frog-leg lateral radiographic view, compared with the AP and cross-table views for identifying the cam-type femoral impingement deformation. Despite the high reliability of the frog-leg lateral view for detecting the cam-type impingement, the AP view is likewise adequate for measuring the alpha angle to detect an aspheric femoral head. The AP pelvic radiograph was done with patients standing with the foot in a neutrally aligned position. In our study, the standing full-length radiograph was also performed with straight anteriorly positioned legs, whereby the AP view in the study of Clohisy et al. [13] is comparable to the standing full-length radiographs relating to measurement of the alpha angle.
AP radiographs are a good screening tool for measuring alpha angles. For specific analysis of the femoral head-neck zone, a frog-leg view is more suitable and should succeed AP radiographs when suspected [13, 24]. When the alpha angle is symptomatically increased in radiographs, ultrasound, MRI and CT should be performed [24, 25]. Due to the multiplanar capability, MRI and CT are more suitable than plain radiography for detecting cam impingement because only the outlines of the bone are clearly visualised in conventional radiographs [26–28].
The aim of our study was to clarify whether there was a relation between the specificity of the alpha angle value and an axis deviation. To the best of our knowledge, the correlation between alpha angle and MAD has not yet been examined in the literature. The full-length radiograph is capable as a screening tool in a routine clinical setting for the assessment of the alpha angle and mechanical axis. Especially, alpha angle and leg axis can be measured quickly and easily in clinical practice with the aid of PACS.
The results of the study must be interpreted in light of its limitations. Our group with neutral mechanical axis was relatively small because a full-length X-ray was only performed in patients with suspected axis deviation. Nevertheless, we achieved a strong power in the post hoc analysis comparing the alpha angles of the moderate with the extended axis deviation; therefore, the number of participants was sufficient for our study. An increased angle does not necessary include clinical symptoms of FAI; however, the risk for the development of symptoms is certainly increased. Clinical examination and oblique sagittal MR sequences should succeed increased alpha angles in radiographs and especially in extended varus or valgus malalignment.
Nevertheless, our study was the first investigation in the literature which examined the relation between the mechanical leg axis and FAI and we can state a correlation between alpha angle and the MAD. In conclusion, although there are diverse causes for the development of FAI, axis deviation can be identified carefully as a risk factor. In cases of a MAD >15 or < − 15 mm and symptomatic coxalgia, FAI must be ruled out by further diagnostic tests.
Acknowledgments
The authors thank Dr. Nina Lahner for linguistic support and preparation of the manuscript.
References
- 1.Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012;380(9855):1768–1777. doi: 10.1016/S0140-6736(12)60607-2. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leunig M, Ganz R. Femoroacetabular impingement. A common cause of hip complaints leading to arthrosis. Unfallchirurg. 2005;108(1):9–10. doi: 10.1007/s00113-004-0902-z. [DOI] [PubMed] [Google Scholar]
- 5.Imam S, Khanduja V. Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop. 2011;35(10):1427–1435. doi: 10.1007/s00264-011-1278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 7.Kim WY, Hutchinson CE, Andrew JG, Allen PD. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. 2006;88(6):727–729. doi: 10.1302/0301-620X.88B6.17430. [DOI] [PubMed] [Google Scholar]
- 8.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 10.Siebenrock KA, Wahab KH, Werlen S, Kalhor M, Leunig M, Ganz R. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;418:54–60. doi: 10.1097/00003086-200401000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Leunig M, Casillas MM, Hamlet M, Hersche O, Nötzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370–375. doi: 10.1080/000164700317393367. [DOI] [PubMed] [Google Scholar]
- 12.Snow SW, Keret D, Scarangella S, Bowen JR. Anterior impingement of the femoral head: a late phenomenon of Legg-Calvé-Perthes’ disease. J Pediatr Orthop. 1993;13:286–289. doi: 10.1097/01241398-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 14.Kassarjian A, Yoon LS, Belzile E, Connolly SA, Millis MB, Palmer WE. Triad of MR arthrographic findings in patients with cam-type femoroacetabular impingement. Radiology. 2005;236(2):588–592. doi: 10.1148/radiol.2362041987. [DOI] [PubMed] [Google Scholar]
- 15.Siebenrock KA, Steppacher SD, Haefeli PC, Schwab JM, Tannast M (2013) Valgus hip with high antetorsion causes pain through posterior extraarticular FAI. Clin Orthop Relat Res Mar 6 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 16.Brown G, Amendola A. Radiographic evaluation and preoperative planning for high tibial osteotomies. Oper Tech Sports Med. 2000;8:2–14. doi: 10.1016/S1060-1872(00)80018-0. [DOI] [Google Scholar]
- 17.Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br. 2007;89(10):1309–1316. doi: 10.1302/0301-620X.89B10.19405. [DOI] [PubMed] [Google Scholar]
- 18.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2344. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 19.Pollard TC, Villar RN, Norton MR, Fern ED, Williams MR, Murray DW, Carr AJ. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Joint Surg Br. 2010;92(2):209–216. doi: 10.1302/0301-620X.92B2.22850. [DOI] [PubMed] [Google Scholar]
- 20.Reichenbach S, Jüni P, Werlen S, Nüesch E, Pfirmann CW, Trelle S, Odermatt A, Hofstetter W, Ganz R, Leunig M. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res (Hoboken) 2010;62(9):1319–1327. doi: 10.1002/acr.20198. [DOI] [PubMed] [Google Scholar]
- 21.Papalia R, Del Buono A, Franceschi F, Marinozzi A, Maffulli N, Denaro V. Femoroacetabular impingement syndrome management: arthroscopy or open surgery? Int Orthop. 2012;36(5):903–914. doi: 10.1007/s00264-011-1443-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coventry MB. Upper tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1985;67:1136–1140. [PubMed] [Google Scholar]
- 23.Pape D, Seil R, Adam F, Rupp S, Kohn D, Lobenhoffer P. Imaging and preoperative planning of osteotomy of tibial head osteotomy. Orthopade. 2004;33(2):122–134. doi: 10.1007/s00132-003-0585-0. [DOI] [PubMed] [Google Scholar]
- 24.Barton C, Salineros MJ, Rakhra KS, Beaulé PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469(2):464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lerch S, Kasperczyk A, Warnecke J, Berndt T, Rühmann O. Evaluation of Cam-type femoroacetabular impingement by ultrasound. Int Orthop. 2013;37(5):783–788. doi: 10.1007/s00264-013-1844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beaulé PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23(6):1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 27.Dudda M, Albers C, Mamisch TC, Werlen S, Beck M. Do normal radiographs exclude asphericity of the femoral head-neck junction? Clin Orthop Relat Res. 2009;467(3):651–659. doi: 10.1007/s11999-008-0617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rakhra KS, Sheikh AM, Allen D, Beaulé PE. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res. 2009;467(3):660–665. doi: 10.1007/s11999-008-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]