Dear Editor,
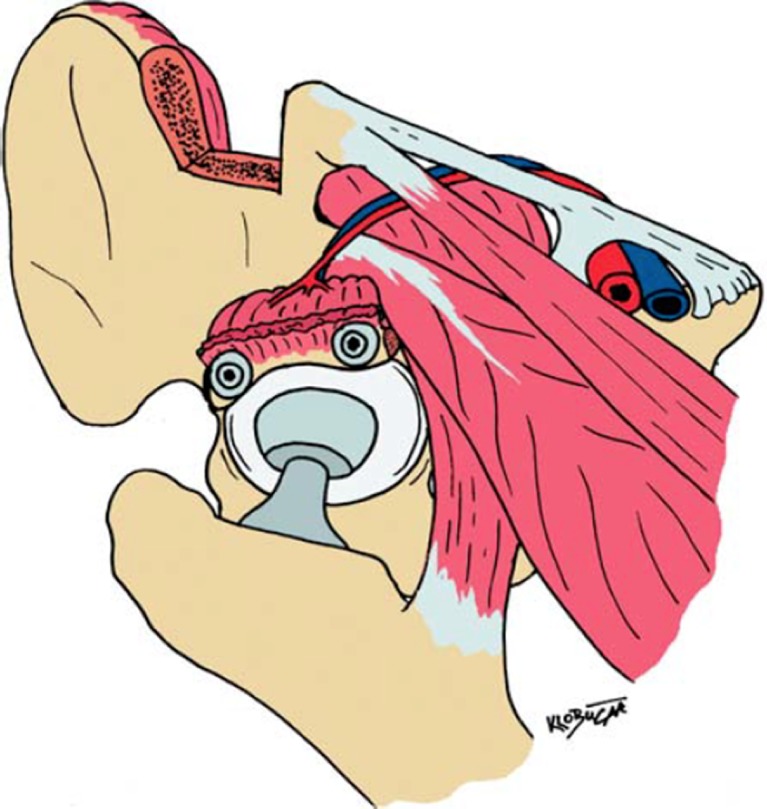
We would like to present ten years follow-up of the previously published original technique for reconstruction of the acetabular roof in patients with severe hip dysplasia. In the article “Acetabular roof reconstruction with pedicled iliac graft” published in International Orthopaedics [1] we presented a new method for acetabular superolateral rim reconstruction using a pedicled iliac graft (Fig. 1). The method was designed and developed in order to allow optimal acetabular component placement during total hip replacement procedures in patients with combined hip dysplasia and deficient bone stock where some kind of acetabular reconstruction is often required. Various bone grafting techniques for acetabular reconstruction have been reported so far; the majority of them have shown good early results, but mid- and long-term results showed relatively high revision rates—between 30 and 50 % after the first four to eight years [2]. Furthermore, according to our previous results, optimal placement of the acetabular component should be in the ideal centre of rotation, but if that is not feasible then as far medially as possible [3]. Therefore, we developed a new bone grafting method with several predefined primary goals such as: (1) to ensure good primary stability of the acetabular component, (2) to provide local bone remodelling and (3) to provide adequate incorporation under load. Our method was based on the use of a pedicled iliac graft because of its strong mechanical properties coupled with its preserved circulation, i.e. high healing and remodelling potential [4].
Fig. 1.
Vascularised iliac graft based on deep circumflex pedicle [1]
The feasibility of our method was first tested on ten cadavers where a pedicled structural graft appeared to be suitable to achieve any desired position of the acetabular roof without requiring any microvascular anastomosis [1]. Later on, we presented our early clinical experience of acetabular roof reconstruction with a pedicled iliac graft based on the deep circumflex artery and vein performed on two patients [5]. Early clinical outcome showed that use of such a pedicled bulk structural graft provides good primary stability combined with good potential for bone formation and incorporation under load. However, mid- and long-term follow-up is crucial for proper evaluation of final outcome after any reconstruction procedure.
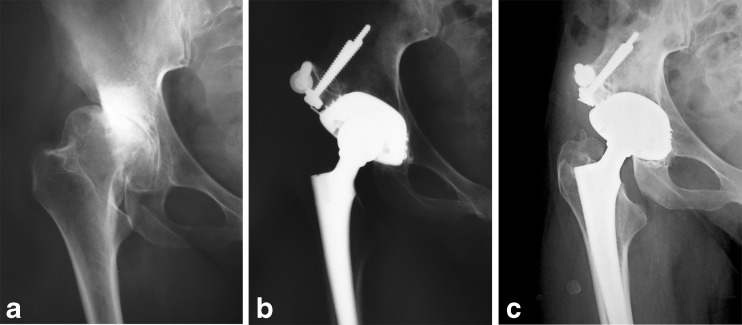
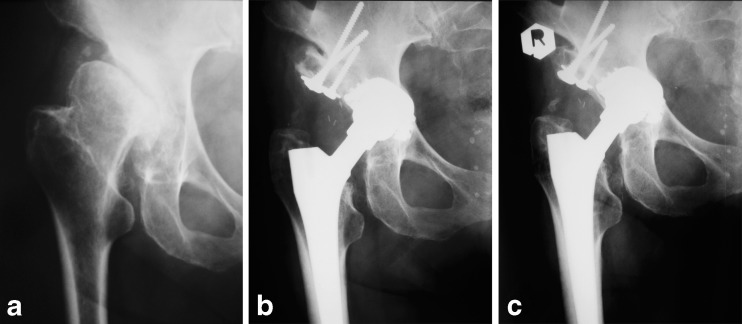
Therefore, here we report long-term follow-up results ten years after the primary procedure in the same two patients where acetabular reconstruction using a pedicled iliac graft was performed [5]. The patients, both female, now 47 and 70 years of age had the procedure 10.5 and 11 years ago. Both patients, now ten years after the primary procedure, have equal leg lengths, show excellent endoprosthesis function and no donor site morbidity. The patients report no pain at rest or during physical activity; both have satisfactory walking distance (more than 30 minutes) and have no symptoms during any everyday activity. Radiographs documented on follow-up examinations showed excellent bone healing and remodelling as well as incorporation under load as soon as one year after surgery and even more so ten years after (Figs. 2 and 3). Long-term follow-up results presented here demonstrate our method as a valuable procedure fulfilling all the primary goals set out above, finally resulting in good functional outcome and high patient comfort.
Fig. 2.
Radiographs of the female patient V. P., 37 years of age at the time of grafting: preoperatively (a), 1 year post-operatively (b) and 10 years post-operatively (c). The acetabular component was placed adequately with the use of a pedicled iliac graft. Graft incorporation is visible at both time points, 1 and 10 years after surgery
Fig. 3.
Radiographs of the female patient B. B., 60 years of age at the time of grafting: preoperatively (a), 1 year post-operatively (b) and 10 years post-operatively (c). Graft incorporation is clearly visible at both post-operative time points together with clearly visible signs of bone remodelling within the graft
Therefore, the method of acetabular roof reconstruction with a pedicled iliac graft based on deep circumflex artery and vein might serve as a method of choice in patients with combined hip dysplasia and deficient bone stock that need to undergo total hip replacement.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Domagoj Delimar, Email: domagoj.delimar@kbc-zagreb.hr.
Ivan Bohacek, Email: ivan.bohacek@gmail.com.
Marko Pecina, Email: marko.pecina@zg.t-com.hr.
Goran Bicanic, Phone: +385-1-2368911, FAX: +385-1-2379913, Email: goran.bicanic@zg.t-com.hr.
References
- 1.Delimar D, Čičak N, Klobučar H, Pećina M, Koržinek K. Acetabular roof reconstruction with pedicled iliac graft. Int Orthop. 2002;26:344–348. doi: 10.1007/s00264-002-0381-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwong LM, Jastry M, Harris WH. High failure rate of bulk femoral allografts in total hip acetabular reconstructions at 10 years. J Arthroplasty. 1993;8:341–346. doi: 10.1016/S0883-5403(06)80032-X. [DOI] [PubMed] [Google Scholar]
- 3.Bicanic G, Delimar D, Delimar M, Pecina M. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop. 2009;33:397–402. doi: 10.1007/s00264-008-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leung PC. Pedicled iliac graft—twenty years experience. Int Orthop. 2003;27:323–325. doi: 10.1007/s00264-003-0487-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delimar D, Bićanić G, Pećina M, Koržinek K. Acetabular roof reconstruction with pedicled iliac graft: early clinical experience. Int Orthop. 2004;28:319–320. doi: 10.1007/s00264-004-0555-0. [DOI] [PMC free article] [PubMed] [Google Scholar]