Abstract
Purpose
The combined anteversion (CA) technique is a method in which the cup is placed according to the stem anteversion in total hip arthroplasty (THA). We examined whether the CA technique reduced the dislocation rate, and the distribution of CA with the manual placement of the cup.
Methods
We retrospectively reviewed 634 hips in 579 patients with primary cementless THA. In 230 hips using the CA technique [CA(+)], a CA of 50 ± 10° was the aim. In the remaining 404 hips [CA(−)], the cup was first placed targeting 20° of anteversion. The post-operative CA was measured using the computed tomography (CT) images in 111 hips.
Results
One hip (0.4 %) had a dislocation in the CA(+) group, whereas ten hips (2.5 %) had a dislocation in the CA(−) group. A multivariate analysis showed that primary diagnosis, head size and CA technique significantly influenced the dislocation rate. Patients in the CA(−) group were 5.8 times more likely to have a dislocation compared to the CA(+) group. In the 111 hips with CT images, 81 hips (73.0 %) achieved the intended CA.
Conclusions
Although the manual placement of the cup resulted in 27 % of outliers from the intended CA, the CA technique significantly reduced the dislocation after primary THA.
Keywords: Total hip arthroplasty, Dislocation, Combined anteversion technique, Stem anteversion
Introduction
Accurate component placement has been considered to be a prerequisite for successful total hip arthroplasty (THA), as implant malposition influences impingement, dislocation, wear and aseptic loosening [1–6]. Although the Lewinnek safe zone for cup placement (anteversion 15 ± 10°) is a gold standard in THA [7], this is sometimes not applicable to cases with abnormal femoral anteversion such as seen in dysplastic hips [8–10]. Combined anteversion (CA), the sum of the cup and stem anteversion, should be considered in these cases [9, 11–13].
The generally accepted CA has been reported to range from 30 to 60° to avoid impingement and maximise hip range of motion [11, 14, 15]. The dislocation risk was reportedly 6.9 times greater if the CA fell outside the range of 40–60° [15]. Other reports recommended the CA to be between 25 and 35° in men and up to 45° in women [11]. To achieve an appropriate CA for each case, the method of adjusting cup anteversion according to stem anteversion, the so-called CA technique, has been recommended by Dorr et al. in cementless THA [14] as a cementless stem has less adjustability in the femoral canal compared to the cemented stem [1, 16]. Although the CA technique has become more relevant [17], there is little evidence that the CA technique has lowered the dislocation rate. This technique has been adopted as a routine procedure in primary THA since 2006 by one of us (YN).
Therefore, we investigated whether the CA technique reduced the rate of dislocation in THA and also examined the distribution of CA with the manual placement of the cup with an attempt to achieve a CA of 50 ± 10°.
Materials and methods
Patients
This retrospective study was approved by the Institutional Review Board. Between 2006 and 2011, a total of 651 hips in 596 patients underwent primary cementless THA. Among them, five hips in five patients and 12 hips in 12 patients were excluded because of patient death unrelated to THA and loss to follow-up, respectively. The remaining 634 hips in 579 patients followed up for at least one year were included in this study (Table 1). The mean age of the patients at surgery was 63.4 years old (22–92 years) and the mean duration of follow-up was 30.2 months (12–71 months). There were 533 hips in women and 101 hips in men. The most common indication for THA was hip osteoarthritis (OA) in 556 hips in 508 patients including 360 hips with developmental dysplasia of the hip (DDH). DDH was diagnosed when the hip had a centre-edge angle less than 20° [18]. Other indications included osteonecrosis of the femoral head (ONFH) in 67 hips in 61 patients and rheumatoid arthritis (RA) in 11 hips in ten patients. Among them, pre- and post-operative computed tomography (CT) was performed in 111 hips in 101 patients between 2010 and 2011 (Table 2).
Table 1.
Patient characteristics
| Total, 634 hips in 579 cases | CA(+) technique, 230 hips in 207 cases | CA(−) technique, 404 hips in 372 cases | p value | ||
|---|---|---|---|---|---|
| Age at THAa (years) | 63.4 ± 11.2 (22–92) | 63.5 ± 10.0 | 63.0 ± 11.2 | 0.7771 | |
| BMIa (kg/m2) | 23.7 ± 3.7 (15.0–45.2) | 23.6 ± 4.0 | 23.5 ± 3.6 | 0.8167 | |
| Gender (hips/cases) | Male | 101/97 | 39/39 | 62/58 | 0.9701 |
| Female | 533/482 | 191/168 | 342/314 | ||
| Diagnosis (hips/cases) | OA | 556/508 | 197/180 | 359/328 | 0.1409 |
| RA | 11/10 | 7/6 | 4/4 | ||
| ONFH | 67/61 | 26/21 | 41/40 | ||
Comparison was performed between the patients with and without the CA technique
CA combined anteversion, BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH osteonecrosis of the femoral head
aValues are given as mean ± SD (range)
Table 2.
Patient characteristics with pre- and post-operative CT (n = 111)
| Characteristic | ||
|---|---|---|
| Total number of hips | 111 hips in 101 patients | |
| Age at THAa (years) | 64.2 ± 8.3 (42–78) | |
| BMIa (kg/m2) | 24.5 ± 3.8 (15.1–36.9) | |
| Gender (male/female) | 18/93 hips | |
| Diagnosis | OA | 105 hips |
| DDH | 76 hips | |
| Non-DDH | 29 hips | |
| RA | 3 hips | |
| ONFH | 3 hips | |
| Native anteversiona | 23.9 ± 10.7° (1.3–49.7) | |
| Stem anteversiona | 33.5 ± 10.8° (8.9–59.9) | |
| Cup anteversiona | 18.0 ± 10.4° (−8.8–41.1) | |
| CAa | 51.4 ± 10.4° (20.1–73.4) | |
BMI body mass index, OA osteoarthritis, DDH developmental dysplasia of the hip, RA rheumatoid arthritis, ONFH osteonecrosis of the femoral head, CA combined anteversion
aValues are given as mean ± SD (range)
The CA technique was adopted in 2006 by one of our study authors (YN). Since then, 230 THAs have been performed routinely using the CA technique [CA(+) group]. The other surgeons continued to place the cup prior to the stem preparation. In total, 404 THAs were performed without the CA technique [CA(−) group]. No significant differences related to the baseline patient characteristics were noted between the groups (Table 1). The CA technique was used in all 111 hips with CT images. All patients were followed up prospectively. They visited our clinic for examination two months, six months and one year after THA and yearly thereafter. When patients could not visit the clinic, they were interviewed over the phone and questioned about the presence or absence of dislocation.
Implants
Cementless THA (AMS cup and PerFix910 stem, Kyocera, Osaka, Japan) was used in all hips [19]. Femoral offset was changed according to the case. A standard offset was used in 127 hips and +4 mm offset was used in 507 hips. The head size was changed depending on the periods, 26 mm in 465 hips and 32 mm in 169 hips.
Surgical technique
All THAs were performed using the common posterior approach [20]. In cases using the CA technique, the preparation of the femur was performed first so that the anteversion of the femur was known prior to the cup placement [14]. The anteversion of the final broach was measured as the angle between the lower leg axis and trial stem axis by flexing the knee and placing the tibia in a vertical position using a manual goniometer (Fig. 1). Then the cup was placed according to the stem anteversion so that the combined anteversion ranged from 40 to 60° [15]. Cup anteversion was defined as the operative anteversion following the method of Murray [21]. The cup was placed with 20° anteversion first using the manufacturer’s cup inserter which aimed at 20° operative anteversion and 45° abduction by aligning the jig to the longitudinal axis of the body. Cup anteversion was then adjusted to achieve the intended anteversion. When 30° of cup anteversion was the aim, 10° more anteversion was added manually to the jig of the cup inserter. If the stem anteversion was more than 60°, a cup anteversion of 5° was attempted to avoid a retroverted cup. In cases without the CA technique, the cup was placed first with a goal of 20° anteversion and the stem preparation was started. The posterior soft tissues were routinely repaired [22].
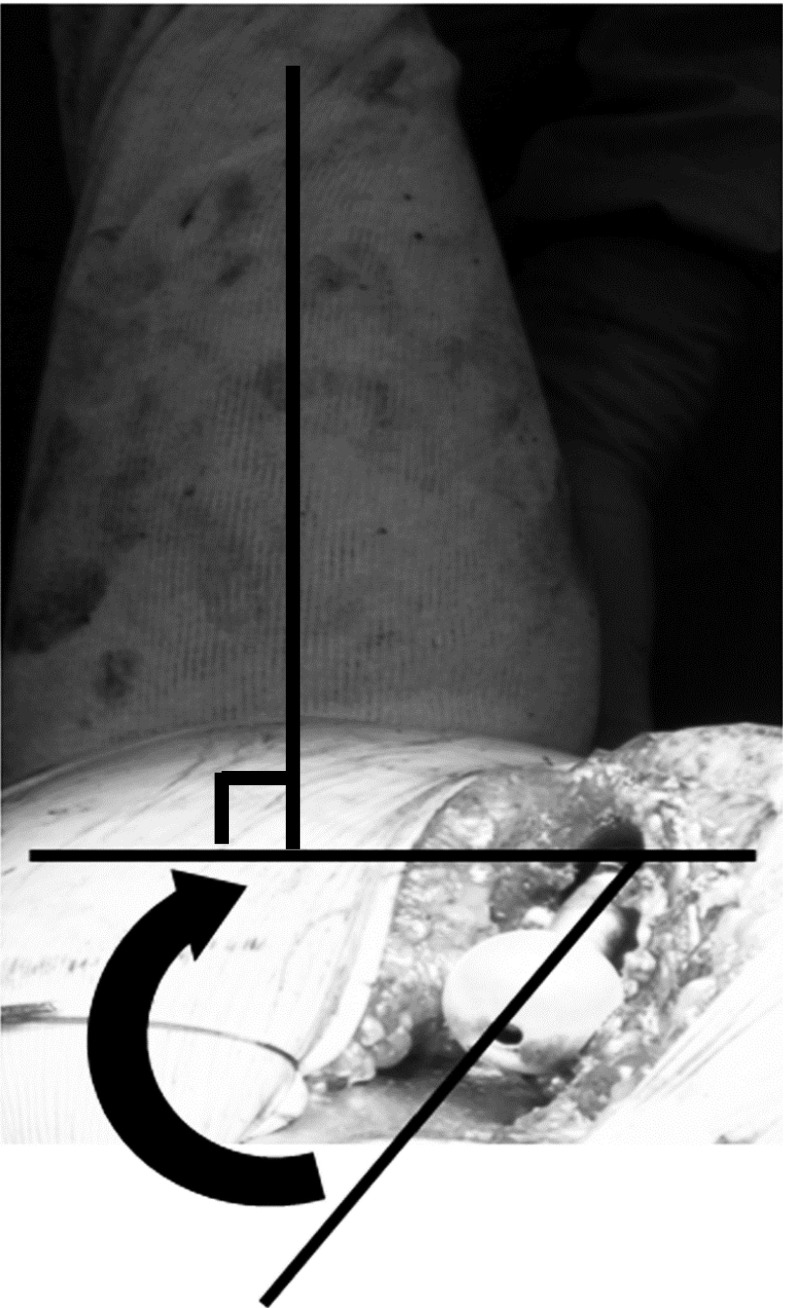
Fig. 1.
Intraoperative measurement of stem anteversion (left hip). The anteversion of the final broach was measured using a goniometer as the angle between the axis of the lower leg and the trial stem by flexing the knee and placing the tibia in a vertical position
Radiographic assessment
The cup inclination was measured as an abduction angle using the inter-teardrop line as the baseline. In cases with pre- and post-operative CT data, native femoral anteversion, stem and cup anteversion were measured (Fig. 2). Briefly, the femoral neck axis was calculated as a best-fit line connecting slices taken through a central segment of the neck. Then native femoral anteversion was defined as the angle between the neck axis and epicondylar line [23]. Stem anteversion was calculated as the angle of the prosthetic femoral neck relative to the epicondylar line (Fig. 2a). Cup anteversion was measured as the operative anteversion (Fig. 2c).
Fig. 2.
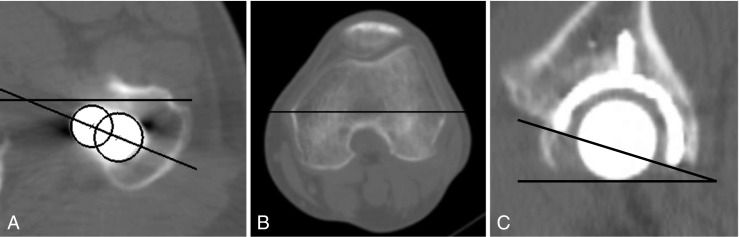
Measurements of stem and cup anteversion. Stem anteversion (a) was calculated as the angle of the prosthetic femoral neck relative to the epicondylar line (b). Cup anteversion (c) was defined as the operative anteversion and measured on the sagittal plane
Statistical analyses
Factors examined included age, gender, body mass index (BMI), primary diagnosis, head size, neck geometry, cup position and CA technique. The chi-square test was used to compare categorical parameters and the Wilcoxon rank sum test was used to compare continuous parameters between the groups. The Tukey-Kramer HSD test was used for multiple comparisons. The univariate Cox model was applied to each possible risk factor to separately screen for significant factors affecting dislocation. The significant risk factors were then examined together using a multivariate Cox model to determine their contribution to dislocation. Differences were defined as significant when the p value was < 0.05. Statistical analyses were performed using JMP Software (SAS Institute, Cary, NC, USA).
Results
Dislocations occurred in 11 hips (1.74 %). Univariate analysis indicated four significant risk factors for dislocation: gender, the primary diagnosis for THA, head size and CA technique (Table 3). Male patients and the hips with ONFH resulted in a significantly higher incidence of dislocation compared to female patients and other diseases, respectively. The larger head size significantly reduced the dislocation rate, 2.3 % with 26 mm and 0 % with 32 mm. Multivariate analysis demonstrated that ONFH (p = 0.0173), 32 mm head size (p = 0.0078) and CA technique (p = 0.0383) were significantly associated with dislocation (Table 4). Among the CA(+) group, only one hip with ONFH and 26 mm head (0.4 %) experienced a dislocation, whereas ten hips (2.5 %) dislocated in the CA(−) group, showing the significantly lower rate of dislocation in the CA(+) group with an odds ratio of 5.8. Namely, the CA(−) group was 5.8 times more likely to dislocate compared to the CA(+) group.
Table 3.
Univariate analysis of the factors for dislocation
| Factors | Dislocation (+), 11 hips in 11 cases | Dislocation (−), 623 hips in 568 cases | p value |
|---|---|---|---|
| Age at THAa (years) | 59.9 ± 16.1 | 63.4 ± 10.9 | 0.6025 |
| BMIa (kg/m2) | 25.0 ± 5.8 | 23.7 ± 3.7 | 0.7002 |
| Gender (hips) | Male: 4.95 % (5/101) | Male: 95.0 % (96/101) | 0.0079 |
| Female: 1.16 % (6/533) | Female: 98.8 % (527/533) | ||
| Primary diagnosis (hips) | OA: 1.1 % (6/556) | OA: 98.9 % (550/556) | 0.0006 |
| RA: 0 % (0/11) | RA: 100 % (11/11) | ||
| ONFH: 7.4 % (5/67) | ONFH: 92.5 % (62/67) | ||
| Head size (hips) | 26 mm: 2.3 % (11/465) | 26 mm: 97.7 % (454/465) | 0.0423 |
| 32 mm: 0.0 % (0/169) | 32 mm: 100 % (169/169) | ||
| Stem offset (hips) | Standard: 1.5 % (2/127) | Standard: 98.5 % (125/127) | 0.8362 |
| +4 mm offset: 1.7 % (9/507) | +4 mm offset: 97.9 % (498/507) | ||
| Cup abductiona (°) | 41.0 ± 7.92 | 39.4 ± 6.50 | 0.6337 |
| CA technique | CA(+): 0.43 % (1/230) | CA(+): 99.6 % (229/230) | 0.0334 |
| CA(−): 2.48 % (10/404) | CA(−): 97.5 % (394/404) |
BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH osteonecrosis of the femoral head, CA combined anteversion
aValues are given as mean ± SD
Table 4.
Multivariate analysis of the factors for dislocation
| Factors | Odds ratio | χ2 | 95 % confidence interval | p value |
|---|---|---|---|---|
| Age | 1.00 | 0.00 | 0.9489–1.0552 | 0.9752 |
| BMI | 0.95 | 0.49 | 0.8138–1.1101 | 0.4860 |
| Gender (M:F) | 2.63 | 0.15 | 0.5439–11.558 | 0.2194 |
| Primary diagnosis | ||||
| OA/RA | 1.51 | 5.83 | 0–47.209 | 0.7150 |
| OA/ONFH | 6.36 | 5.83 | 1.40666–28.1162 | 0.0173 |
| Head size (26:32) | 3.35 | 7.08 | 0–0.47125 | 0.0078 |
| Stem offset | 0.86 | 0.86 | 0.12103–4.03841 | 0.8593 |
| Cup abduction | 0.99 | 0.01 | 0.88801–1.10777 | 0.9061 |
| CA technique | 5.79 | 6.23 | 1.08845–118.4604 | 0.0383 |
BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH osteonecrosis of the femoral head, CA combined anteversion
In the analysis of the 111 hips with pre- and post-operative CT scans, the mean anteversion of the cup and stem was 18.0 ± 10.4° and 33.5 ± 10.8°, respectively (Table 2). The resulting CA was 51.4 ± 10.4° on average ranging from 20.1 to 73.4°. There were 81 hips (73.0 %) within 40–60° of CA, 21 hips (18.9 %) with more than 60° and nine hips (8.1 %) with less than 40° (Table 5). The mean stem anteversion of hips with CA of more than 60° was 43.4 ± 7.9° and the primary diagnosis of all these hips was OA due to DDH. As for the cases with CA less than 40°, the stem anteversion was 21.9 ± 8.1° and the mean cup anteversion was 8.0°. No dislocations were observed by the time of the latest follow-up in these 111 hips.
Table 5.
CA measured by post-operative CT (n = 111)
| 40-60° CA | 81 hips (73.0 %) |
| Stem anteversion | 32.3 ± 9.7° (10.7–59.9) |
| Cup anteversion | 18.0 ± 9.9° (−6.5–41.1) |
| CA | 50.3 ± 6.2° (40–60) |
| CA > 60 | 21 hips (18.9 %) |
| Stem anteversion | 43.4 ± 7.9° (33.1–57.3) |
| Cup anteversion | 22.0 ± 9.4° (7.1–41) |
| CA | 65.5 ± 4.0° (61.2–73.4) |
| CA < 40 | 9 hips (8.1 %) |
| Stem anteversion | 21.9 ± 8.1° (8.9–36.6) |
| Cup anteversion | 8.0 ± 10.8° (−8.8–26.4) |
| CA | 30.0 ± 5.3° (20.1–38.6) |
All the values are given as mean ± SD (range)
Discussion
In addition to the other influencing factors, the CA technique significantly reduced the dislocation rate. One hip (0.4 %) dislocated in the CA(+) group, whereas ten hips (2.5 %) dislocated in the CA(−) group. A multivariate analysis showed that the CA(−) group was 6.4 times more likely to have a dislocation compared to the CA(+) group. As shown in this study, the stem version was highly variable ranging from 0 to 60°, possibly leading to the implant malposition with the cup first technique. This accords with previous reports; Maruyama et al. showed the range of stem anteversion as 17° retroversion to 28° anteversion in cementless femoral stems [9]. Other studies using post-operative CT scans showed a wider range, 30° retroversion to 45° anteversion in both cemented and cementless stems [24, 25]. Cemented stems can be rotated to correct the stem anteversion. However, cementless stems of any geometry are limited by native femoral anteversion to achieve the initial stability. Widmer and Zurfluh showed that the safe zone of cup placement varied depending on stem anteversion using a mathematical model [12]. The safe range of cup anteversion dramatically decreased with an abnormal stem anteversion compared to a stem anteversion of 15 ± 10°. These findings indicate the necessity of understanding stem anteversion before placing the cup.
This study has several limitations. First, we examined only the effects of attempting to achieve a CA of 50 ± 10°. Thus, the CA(+) group did not always satisfy the intended CA. As shown with CT measurements, 27 % of the hips were outliers due to the large stem anteversion and possibly surgeon error in the manual cup placement. However, the CA technique significantly reduced the dislocation rate compared to methods where the cup was placed first. Therefore, it is meaningful to show the importance of confirming stem anteversion prior to cup placement. Second, the patients in this study were retrospectively reviewed and not randomised; therefore the exact effect of CA on the dislocation must be further determined by a randomised controlled study. Third, only the posterior approach was used, therefore limiting results to only that approach. As the posterior approach has been associated with higher rates of dislocation [26, 27], we assumed that the posterior approach was the best to examine our research question. Lastly, the effect of CA technique in the cases with larger head size (32 mm) was not determined, as no dislocation has been noted so far in them. The larger head size has consistently shown the advantage of preventing dislocation in many studies [27–29] and may compensate for the possible instability due to implant malposition to a certain extent. Because the number of patients and the follow-up periods were less in cases with 32 mm head compared to those with 26 mm head, this topic needs further clarification.
Preoperative planning using CT helps to achieve the appropriate CA and may compensate for the disadvantages of the cup first placement [30]; however, stem anteversion is not always parallel to the native femoral anteversion. Emerson showed an increased stem anteversion of 8° compared to the native femoral anteversion [16]. The stem version is also affected by stem alignment. Müller et al. showed that an anteriorly tiled stem tended to have decreased anteversion [31]. These inconsistencies between stem and native anteversion suggested a theoretical advantage of the CA technique.
The goal range of CA in this study was from 40 to 60°, which was relatively larger than in other reports [11, 12]. As many DDH cases in which the large stem anteversion was expected were included in this study, we set this range of CA following Jolles et al. [15]. Despite attempts, 30 hips (27 %) among the cases with CT measurement failed to achieve the intended CA. Two reasons were thought to contribute to these deviations. First, even with a higher upper limit (60°), the greater stem anteversion in DDH cases tended to result in the larger CA with 21 hips (18.9 %) having more than 60°. The hips with CA over 60° had a stem anteversion of 43.4° on average, which was significantly larger than 32.3° in the hips with 40 to 60°. Second, inaccuracy of the cup anteversion by manual cup placement was thought to lead to the outliers. Manual placement is reportedly often less accurate than expected [32]. Jolles et al. showed that the standard deviation of manual placement was three times larger than that using computer navigation. Fortunately there have been no dislocations in these cases so far; however, the existence of outliers suggested the importance of careful cup placement. The CA technique might compensate for the unexpected CA by confirming stem anteversion prior to cup placement.
In conclusion, the CA technique significantly reduced dislocations with an odds ratio of 5.8. The cementless stem anteversion varied widely; therefore, the CA technique is useful to reduce the incidence of dislocation in cementless THA.
Acknowledgments
This work was supported by Grant-in-Aid for Scientific Research from Japan Society for the Promotion of Science (No. 24592268).
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 2.Sato T, Nakashima Y, Akiyama M, et al. Wear resistant performance of highly cross-linked and annealed ultra-high molecular weight polyethylene against ceramic femoral heads in total hip arthroplasty. J Orthop Res. 2012;30:2031–2037. doi: 10.1002/jor.22148. [DOI] [PubMed] [Google Scholar]
- 3.Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008;23:51–56. doi: 10.1016/j.arth.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Hernigou P, Ratte L, Roubineau F, et al. The risk of dislocation after total hip arthroplasty for fractures is decreased with retentive cups. Int Orthop. 2013;37(7):1219–1223. doi: 10.1007/s00264-013-1911-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33(4):927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosker BH, Ettema HB, Verheyen CC, Castelein RM. Acetabular augmentation ring for recurrent dislocation of total hip arthroplasty: 60% stability rate after an average follow-up of 74 months. Int Orthop. 2009;33(1):49–52. doi: 10.1007/s00264-007-0456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 8.Akiyama M, Nakashima Y, Fujii M, et al. Femoral anteversion is correlated with acetabular version and coverage in Asian woman with anterior and global deficient subgroups of hip dysplasia: a CT study. Skeletal Radiol. 2012;41:1411–1418. doi: 10.1007/s00256-012-1368-7. [DOI] [PubMed] [Google Scholar]
- 9.Maruyama M, Feinberg JR, Capello WN, D’Antonio JA. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;393:52–65. doi: 10.1097/00003086-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Matsushita A, Nakashima Y, Fujii M, Sato T, Iwamoto Y. Modular necks improve the range of hip motion in cases with excessively anteverted or retroverted femurs in THA. Clin Orthop Relat Res. 2010;468:3342–3347. doi: 10.1007/s11999-010-1385-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ranawat CS, Maynard MJ. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17–25. doi: 10.1097/00013611-199109000-00004. [DOI] [Google Scholar]
- 12.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, Nunoda D. Study of hip joint dislocation after total hip arthroplasty. Int Orthop. 2006;30(1):26–30. doi: 10.1007/s00264-005-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467:119–127. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 16.Emerson RH., Jr Increased anteversion of press-fit femoral stems compared with anatomic femur. Clin Orthop Relat Res. 2012;470:477–481. doi: 10.1007/s11999-011-1993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Renkawitz T, Hamerl M, Dohmen L, et al. Minimally invasive computer-navigated total hip arthroplasty, following the concept of femur first and combined anteversion: design of a blinded randomized controlled trial. BMC Musculoskelet Disord. 2011;12:192. doi: 10.1186/1471-2474-12-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(Suppl 58):5–135. [Google Scholar]
- 19.Nakashima Y, Hayashi K, Inadome T, Uenoyama K, Hara T, Kanemaru T, Sugioka Y, Noda I. Hydroxyapatite-coating on titanium arc sprayed titanium implants. J Biomed Mater Res. 1997;35:287–298. doi: 10.1002/(SICI)1097-4636(19970605)35:3<287::AID-JBM3>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 20.Inaba Y, Dorr LD, Wan Z, Sirianni L, Boutary M. Operative and patient care techniques for posterior mini-incision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:104–114. doi: 10.1097/01.blo.0000193811.23706.3a. [DOI] [PubMed] [Google Scholar]
- 21.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Tang Y, Zhang C, Zhao X, Xie Y, Xu S. Modified posterior soft tissue repair for the prevention of early postoperative dislocation in total hip arthroplasty. Int Orthop. 2013;37(6):1039–1044. doi: 10.1007/s00264-013-1874-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22:610–614. doi: 10.1097/00004728-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Pierchon F, Pasquier G, Cotten A, Fontaine C, Clarisse J, Duquennoy A. Causes of dislocation of total hip arthroplasty. CT study of component alignment. J Bone Joint Surg Br. 1994;76:45–48. [PubMed] [Google Scholar]
- 25.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Ji HM, Kim KC, Lee YK, Ha YC, Koo KH. Dislocation after total hip arthroplasty: a randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplasty. 2012;27:378–385. doi: 10.1016/j.arth.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 27.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 28.Matsushita A, Nakashima Y, Jingushi S, Yamamoto T, Kuraoka A, Iwamoto Y. Effects of the femoral offset and the head size on the safe range of motion in total hip arthroplasty. J Arthroplasty. 2009;24:646–651. doi: 10.1016/j.arth.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 29.Boyer B, Philippot R, Geringer J, Farizon F. Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop. 2012;36(3):511–518. doi: 10.1007/s00264-011-1289-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DiGioia AM, 3rd, Jaramaz B, Plakseychuk AY, et al. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364. doi: 10.1054/arth.2002.30411. [DOI] [PubMed] [Google Scholar]
- 31.Müller M, Crucius D, Perka C, Tohtz S. The association between the sagittal femoral stem alignment and the resulting femoral head centre in total hip arthroplasty. Int Orthop. 2011;35:981–987. doi: 10.1007/s00264-010-1047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179. doi: 10.1097/01.blo.0000141903.08075.83. [DOI] [PubMed] [Google Scholar]