Abstract
Background
Periacetabular osteotomy (PAO) enables correction of bony acetabular deficiency in the setting of hip dysplasia. Patients with insufficient acetabular coverage often have intraarticular pathology, but the degree of this pathology has been incompletely characterized. We have used arthroscopy as an adjunct to PAO to further delineate intraarticular pathology in patients with hip dysplasia with mechanical symptoms.
Questions/purposes
We documented the arthroscopic incidence of (1) femoral and acetabular chondral pathology, (2) femoral neck cam lesions, and (3) internal snapping or ligamentum teres pathology among patients having arthroscopy before PAO.
Methods
We reviewed all 16 patients (17 hips; mean age at surgery, 21 years; range, 12–33 years) with hip dysplasia who underwent PAOs and concomitant hip arthroscopy at our institutions from October 2010 to March 2012. During this period, 80 patients underwent PAOs, making the arthroscopic cohort 21% of the total cohort. Indications for concomitant hip arthroscopy were mechanical symptoms consistent with labral pathology identified on MRI. We documented pathology involving the labrum, chondral surface, ligamentum teres, cam deformity, and psoas tendon.
Results
Arthroscopy revealed significant intraarticular pathology in all patients. Fourteen hips had anterosuperior labral tears, and three hips had preoperative findings of internal snapping hip. Eleven hips had femoral cam-type lesions in addition to dysplasia, and 16 hips had articular chondral injury. Two hips had full-thickness ligamentum tears, and 13 hips had partial-thickness tears.
Conclusions
Intraarticular pathology at the time of PAO is common. Future studies are needed to rigorously address the use of arthroscopic intervention during PAO and the impact on clinical outcome compared to PAO alone.
Level of Evidence
Level IV, diagnostic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Developmental dysplasia of the hip (DDH) is one of the most common etiologies of osteoarthritis in adults, accounting for up to 20% to 40% in young adults [7, 8, 14, 25, 40, 45, 47]. DDH occurs when there is osseous undercoverage of the femoral head by the acetabulum. When the acetabulum is shallow, the labrum may become hypertrophied and can play a larger role in weightbearing and joint stability. The reduced area of the acetabular articular surface results in increased contact forces within the hip [8, 15, 28, 35]. Additionally, elongation of the ligamentum teres can accompany lateral subluxation of the femoral head within the acetabulum [3, 31]. These factors can lead to tears to the labrum and ligamentum teres and articular cartilage injury [29, 36]. Surgical realignment procedures can make the congruous dysplastic hip more stable and may reduce or eliminate symptoms. The Bernese periacetabular osteotomy (PAO) corrects the instability of the dysplastic hip with preservation of the integrity of the pelvic ring and improves abnormal hip mechanics [24]. Despite the effectiveness of the PAO in reducing or eliminating symptoms in most patients, medium-term clinical results show failure rates approaching 24% at 10 years [9, 10, 12, 13, 18, 44].
Several authors have reported a high incidence of labral tears associated with hip dysplasia [11, 16, 19, 22, 30, 41]. Failure in tension of the hypertrophied labrum seems the most common mode of labral injury in dysplasia, but inversion of the labrum can also occur, leading to tearing [5, 17]. Ross et al. [41] recently reported that more than 60% of patients undergoing PAO had concomitant intraarticular pathology (labral tears or chondral damage) by direct arthroscopic visualization. Byrd and Jones [4] reported on arthroscopic débridement of the labrum and articular cartilage in dysplastic hips with improved results at 1 year. However, a recent report by Parvizi et al. [38] reported minimal relief with labral débridement in the setting of dysplasia. Open labral débridement with an anterior arthrotomy at the time of PAO has also been reported with good results [21, 27]. In a study by Matheney et al. [34], 15 of 135 hips that had undergone PAO required arthroscopic intervention consisting of a labral débridement or chondroplasty for continued mechanical symptoms. We chose a subset of patients with hip dysplasia and mechanical symptoms who were undergoing PAO and performed arthroscopy as an adjunctive procedure before the PAO.
We therefore documented the arthroscopic incidence of (1) femoral and acetabular chondral pathology, (2) femoral neck CAM lesions, and (3) internal snapping or ligamentum teres pathology among patients having arthroscopy before PAO.
Patients and Methods
Patient Selection
After obtaining institutional approval, we reviewed our institution’s hip database to identify patients who underwent PAO with concomitant arthroscopy performed by the senior authors (BGD, JML, MBM, YMY) from October 2010 to March 2012. The decision to proceed with PAO was made by the senior authors based on history, physical examination, and radiographs consistent with symptomatic dysplasia. All patients had preoperative AP, false-profile, Dunn lateral, and Von Rosen radiographs for review. All patients had a lateral center-edge angle of 17° or less (Fig. 1). We obtained delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) on all patients to evaluate intraarticular pathology preoperatively and assess the extent of cartilage degeneration [23]. Patients with joint space narrowing or other radiographic evidence of arthritis changes (> Tönnis Grade 1) were not considered for PAO. We excluded patients with other secondary diagnoses such as Legg-Calvé-Perthes disease, slipped capital femoral epiphysis, or septic arthritis. Patients who had undergone previous open surgery were also excluded from this study. The decision to add a concomitant arthroscopy to the PAO was based on the physical examination findings of clicking, locking, or other mechanical symptoms and findings on dGEMRIC suggestive of labral pathology. We identified 16 patients who met our inclusion criteria. During this time period, a total of 80 patients underwent a PAO, making the arthroscopic cohort 21% of the total number of patients. There were 12 females and four males, with a mean age at the time of surgery of 21 years (range, 12–33 years) (Table 1). Two patients had previous arthroscopic surgery at another institution. Both previous arthroscopies included labral débridement; one patient also had a femoral osteoplasty, while the other had a labral repair and acetabular rim trimming. Both patients reported a short period of improvement after arthroscopy, followed by recurrence of their symptoms.
Fig. 1A–B.

(A) In a preoperative standing AP radiograph, the lateral center-edge angle measures 13°. (B) In a preoperative false-profile view, the anterior center-edge angle measures 11°.
Table 1.
Demographics and descriptions of intraarticular hip pathology and treatment
| Variable | Value |
|---|---|
| Number of patients/hips | 16/17 |
| Sex (number of patients) | |
| Female | 12 |
| Male | 4 |
| Age (years)* | 21 ± 6.7 (12–32) |
| Side (number of hips) | |
| Right | 11 |
| Left | 6 |
| Lateral center-edge angle (°)* | 11 ± 7.5 (10–17) |
| Anterior center-edge angle (°)* | 8 ± 11 (0–20) |
| Traction time (minutes)* | 39.3 ± 20.5 (15–72) |
| Preoperative dGEMRIC index* | 531 ± 90.1 (324–726) |
| Previous surgery (number of patients) | 2 |
| Labral tears (number of hips) | |
| Total | 14 |
| Seldes Type I | 8 |
| Seldes Type II | 5 |
| Combined | 1 |
| Position of clock face (hours)* | 2.3 ± 0.75 (1–3) |
| Chondral injury (number of hips) | |
| Total | 16 |
| Acetabular | 14 (6 abrasion chondroplasty; 2 microfracture) |
| Acetabular and femoral | 2 (2 abrasion chondroplasty) |
| Ligamentum tears (number of hips) | |
| Total | 15 |
| Low grade | 5 |
| High grade | 8 |
| Full thickness | 2 |
* Values are expressed as mean ± SD, with range in parentheses; dGEMRIC = delayed gadolinium-enhanced MRI of cartilage.
Data Collection
Preoperative and intraoperative findings were noted. Lateral and anterior center-edge angles were measured. Preoperative MRI was obtained and evaluated for the following: labral tears, chondral flaps, bony edema patterns, and dGEMRIC index. The dGEMRIC index refers to the longitudinal relaxation time after penetration of gadolinium and is reported as a value ranging from 50 to 1500 milliseconds, with lower scores indicating more disease. Intraoperatively, labral tears were described according to location (clock face), size, and Seldes classification [42]. Peripheral acetabular labral-articular disruption lesions were classified according to the acetabular labrum articular disruption (ALAD) classification [19]: softening of cartilage adjacent to the labrum (ALAD1), early peel back of the cartilage (ALAD2), large chondral flap (ALAD3), and complete loss of cartilage (ALAD4). Ligamentum teres pathology was classified as normal, a low-grade partial-thickness tear, a high-grade partial-thickness tear, or a full-thickness tear. Surgical traction was applied for the arthroscopy, and total traction time was recorded (Table 1). Peripheral arthroscopy was done to dynamically confirm cam deformity seen on preoperative radiographs.
Surgical Technique
Arthroscopy was performed in the supine position using anterolateral and midanterior portals. Muscular paralysis was employed with general endotracheal anesthesia for the arthroscopic portion of the procedure. The neuromuscular blockade was reversed for the PAO portion of the procedure. Initially, a full diagnostic arthroscopy of the central compartment was performed. Partial capsulotomy was employed as needed to enable subsequent arthroscopic procedures. The PAO was performed after the arthroscopy using a surgical technique described by Ganz as modified by Murphy et al. [33] with or without sparing of the rectus tendon (Fig. 2). There were no medical or surgical complications in this small cohort of patients at an average of 1.5 year of followup.
Fig. 2.
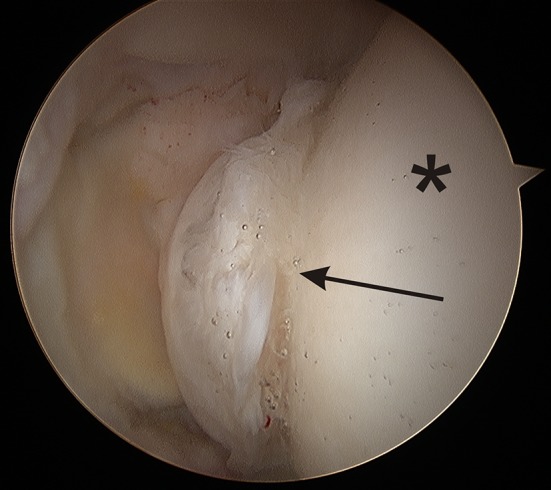
An arthroscopic view shows fraying of the ligamentum teres suggestive of microinstability (arrow). The asterisk is the articular surface of the femoral head.
Results
Arthroscopy revealed concomitant intraarticular pathology in all patients. Preoperative dGEMRIC diagnosed 16 of 17 hips with a labral tear. A total of 14 of 17 patients had labral tears identified arthroscopically (Table 1). Labral tears were located in the anterosuperior portion (Fig. 3). Mean tear size was 8 mm located at 2.3 hours on the clock face (range, 1–3 hours; SD = 0.75 hours). Tears were Seldes Type I in eight hips, Seldes Type II in five, and combined Seldes Types I and II in one. The Seldes Type II labral tears involving an intrasubstance split or fraying were treated with labral débridement while the Seldes Type I tears that were detached from the acetabulum required a labral repair (Fig. 4).
Fig. 3A–B.
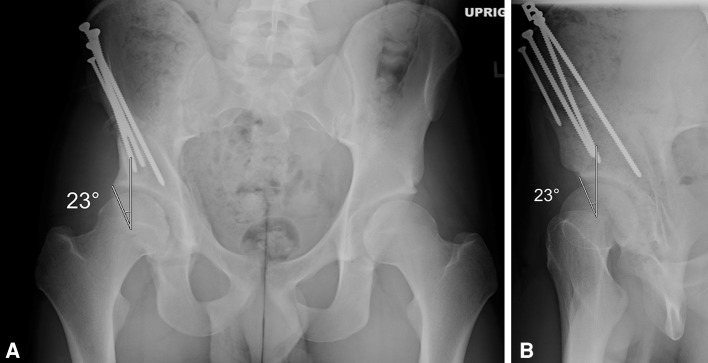
(A) In a postoperative AP radiograph, the lateral center-edge angle measures 23°. (B) In a postoperative false-profile view, the anterior center-edge angle measures 23°.
Fig. 4.
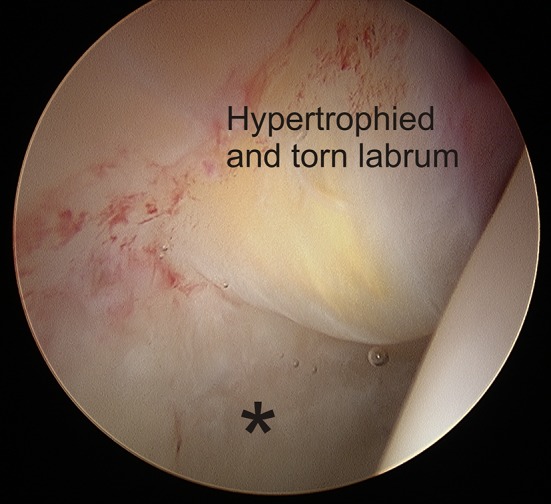
In an arthroscopic view, the labrum is hypertrophied and, under the yellowish area of degeneration, has separated from the acetabulum. The asterisk denotes the acetabular cartilage, which is softened.
Mean preoperative dGEMRIC index of the hips was 531 milliseconds (range, 324–726 milliseconds). Under arthroscopic visualization, 16 of 17 hips also had chondral injuries. Chondral damage was located on the acetabular side in 14 hips and was both femoral and acetabular in the remaining two. All acetabular lesions involved the periphery and acetabular rim. Five hips had ALAD1 lesions, eight had ALAD2 lesions, two had ALAD3 lesions, and one had an ALAD4 lesion. Eight hips underwent abrasion chondroplasty of the lesions, while two had microfracture chondroplasty for the lesions (Fig. 5).
Fig. 5.
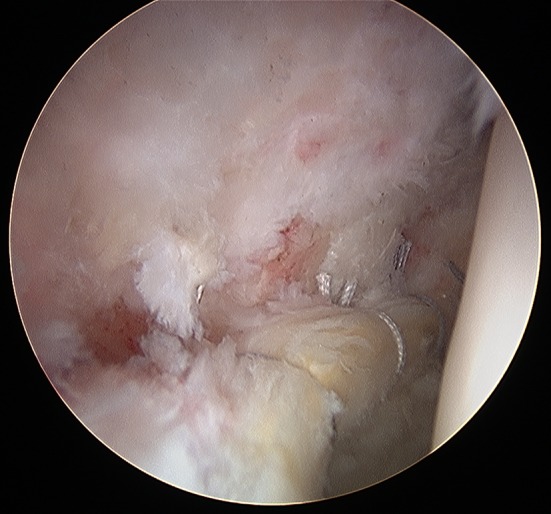
An arthroscopic view shows the repair of the torn labrum shown in Figure 4 using suture anchors to secure the tissue.
Ten hips were identified as having cam deformity by preoperative radiography. Arthroscopic evaluation revealed that 11 hips demonstrated cam-type deformities of the femoral neck. Three hips had preoperative findings of internal snapping hip. The ligamentum teres was probed and visualized during arthroscopy. We identified ligamentum pathology in 15 hips: five had low-grade partial-thickness tears, eight had high-grade partial thickness tears, and two had full-thickness tears.
Discussion
Over the past decade, the Bernese PAO has become a widely accepted treatment for symptomatic congruous acetabular dysplasia in the mature patient, with satisfactory results seen at short- and medium-term followup [13, 26]. However, despite adequate bony correction, some patients continue to experience pain and mechanical symptoms. Matheney et al. [34] noted that 15 of 135 hips required secondary arthroscopic intervention consisting of a labral débridement or chondroplasty at an average of 6.8 years after PAO. Eleven of those patients reported complete resolution of their pain and symptoms. Long-term followup of PAO shows that specific population subgroups are at a higher risk of failure. Patients with Tönnis Grade 2 and 3 changes tend to have worse outcomes [13, 43, 46]. Patients lacking a congruent joint have historically done worse and gone on to earlier failure [26]. The incidence of a labral tear and its effect on outcome after PAO are still controversial. Several authors reported worse long-term outcomes of PAO when a labral tear was found [43, 48]. Others studies have failed to show this association [26]. Accordingly, we described the frequency of different kinds of intraarticular pathology in dysplastic hips treated with concomitant arthroscopy and Bernese PAO.
Our study had a number of limitations. First, our patient sample was small and there was a significant selection bias within our study cohort. This group was selected based on preoperative mechanical symptoms and findings on dGEMRIC suggestive of labral pathology. Therefore, all patients were suspected of having intraarticular pathology. However, the degree of labral tearing, amount of chondral damage, presence of cam deformity, and amount of ligamentum teres damage were considerable. It is unclear from this study whether these same findings would be present in all patients who underwent PAO in the same time period. Second, our study was purely descriptive; we did not perform any clinical analysis or obtain outcome measures of the patients in this group. This severely limits the ability to interpret the usefulness of arthroscopy as an adjunct to PAO. However, intraarticular pathology was found in all patients, with multiple pathologies present in most patients.
Intraarticular pathology is quite common in the mature dysplastic hip and can include labral, articular cartilage, and ligamentum teres injury [11, 19, 21, 22, 30, 41]. The initial report by Klaue et al. [21] described addressing labral pathology at the time of surgery by intraarticular inspection and labral repair or débridement depending on the tear characteristics. Due to their short followup, they were unable to draw any conclusions relating to the effect of labral débridement or repair. In more recent series, labral tears were present in 49 of 72 [34] and 122 of 170 [29] patients, the majority of whom were surgically treated. In the series by Ross et al. [41], 93% of the labrum in dysplastic hips were either hypertrophic or torn; however, it is not known what type of labral tear occurred. In our study, the majority of labral tears were found to be Seldes I tears, which correlates to the increased stress concentration at the acetabular edge of a hypertrophied labrum. It is not known whether the labrum diminishes in size after PAO correction, although in patients treated with Chiari osteotomy, a massive labral tear was found in all seven patients treated with arthroscopy [16]. Recently, Parvizi et al. [38] cautioned against the use of arthroscopy in the treatment of hip dysplasia. They found that hip arthroscopy with isolated treatment of labral pathology may actually accelerate the arthritis process.
The acetabulum is affected in more than 60% of hips, and acetabular chondral lesions typically involve the anterosuperior and posterosuperior regions [11, 29, 41]. Evaluation by dGEMRIC also shows the acetabular cartilage is often diffusely thinned, even in the absence of any focal lesion in the dysplastic hip [20]. In our series, dGEMRIC index values of 500 milliseconds were corroborated by 15 of 16 hips that had anterosuperior chondral damage at the acetabular periphery. Arthroscopy offers the advantage of a more detailed examination of the articular surface with a magnified picture and the ability to clearly see chondral softening with an arthroscopic probe. We were able to classify ½ of the hips as having an ALAD1 articular softening. The pattern of chondral damage was diffuse, suggesting overload of the shallow acetabulum consistent with that seen by Ross et al. [41].
Within this small cohort, we identified a cam deformity in 10 of 16 hips. While dysplasia and femoroacetabular impingement are known to coexist, to our knowledge, there has only been one study documenting the dysplasia in the presence of FAI. Paliobeis and Villar [37] identified up to 47% of patients treated for femoroacetabular impingement had radiographic evidence of dysplasia. This number depended on the radiographic definition of dysplasia. Cam deformity was identified radiographically and confirmed with arthroscopic dynamic assessment of the femoral head-neck junction abutting against the labrum or acetabulum. It is unknown whether the presence of a cam deformity may have contributed to the intraarticular pathology seen in our patients.
The ligamentum teres can be elongated due to the lateral subluxation of the femoral head within the acetabulum [3, 31]. Instability of the hip due to the ligamentum teres is referred to as microinstability [2]. More recently, an MRI model showed that femoral head translation increased in vivo in dysplastic hips, suggesting microinstability as another cause of intraarticular damage [1]. Microinstability is exacerbated by sporting activities that require a lot of hip motion and torque, such as football and tennis, which leads to damage to the labrum and cartilage, explaining the high association among ligamentum tears, labral tears, and cartilage lesions [8, 32]. As shown by Botser et al. [2], hips with a low stability index (lateral center-edge angle − acetabular index), and therefore a lesser bony constraint, may be more dependent on the ligamentum as a secondary stabilizer. In this study, the ligamentum teres was at least partially torn or fully torn in almost all hips, suggesting that these dysplastic hips may have microinstability. This finding has not been seen as often in other series [19, 30, 41]. Pathology in the dysplastic hip can also affect the iliopsoas. In one series, two of eight patients who underwent an arthrotomy at the time of a PAO also required fractional psoas lengthening [6]. In our series, three of 17 hips had internal hip snapping and so underwent lengthening of the psoas.
We found that intraarticular pathology frequently coexists with dysplasia. Acetabular labral damage, chondral damage, and cam deformity are common, while ligamentum teres tears may suggest microinstability of the dysplastic joint. Extraarticular correction of the biomechanics by acetabular realignment osteotomy remains the conventional treatment for dysplasia. However, PAO provides limited access to intraarticular pathology. A concomitant arthroscopy at the time of a PAO allows more complete visualization of the hip than anterior arthrotomy, plus improved ability to address intraarticular pathology. There may be a role for hip arthroscopy to identify and treat intraarticular hip pathology in selected dysplastic hips at the time of PAO. However, further studies are needed to evaluate this role, to identify prognostic factors at arthroscopy, and to assess the value of arthroscopic intervention.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Boston Children’s Hospital (Boston, MA, USA) and the Hinsdale Hospital (Hinsdale, IL, USA).
References
- 1.Akiyama K, Sakai T, Koyanagi J, Yoshikawa H, Sugamoto K. Evaluation of translation in the normal and dysplastic hip using three-dimensional magnetic resonance imaging and voxel-based registration. Osteoarthritis Cartilage. 2011;19:700–710. doi: 10.1016/j.joca.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 2.Botser IB, Martin DE, Stout CE, Domb BG. Tears of the ligamentum teres: prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med. 2011;39(suppl):117S–125S. doi: 10.1177/0363546511413865. [DOI] [PubMed] [Google Scholar]
- 3.Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy. 1996;12:603–612. doi: 10.1016/S0749-8063(96)90201-7. [DOI] [PubMed] [Google Scholar]
- 4.Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055–1060. doi: 10.1016/j.arthro.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 5.Cerezal L, Arnaiz J, Canga A, Piedra T, Altonaga JR, Munafo R, Perez-Carro L. Emerging topics on the hip: ligamentum teres and hip microinstability. Eur J Radiol. 2011. [DOI] [PubMed]
- 6.Clohisy JC, St John LC, Nunley RM, Schutz AL, Schoenecker PL. Combined periacetabular and femoral osteotomies for severe hip deformities. Clin Orthop Relat Res. 2009;467:2221–2227. doi: 10.1007/s11999-009-0810-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooperman DR, Wallensten R, Stulberg SD. Post-reduction avascular necrosis in congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62:247–258. [PubMed] [Google Scholar]
- 8.Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;175:79–85. [PubMed] [Google Scholar]
- 9.Czubak J. Periacetabular Ganz osteotomy in the treatment of developmental dysplasia of the hip in adolescents and adults: surgical technique and early results. Ortop Traumatol Rehabil. 2004;6:51–59. [PubMed] [Google Scholar]
- 10.Czubak J. Periacetabular osteotomy in the treatment of developmental hip dysplasia in adolescents and adults. Ortop Traumatol Rehabil. 2006;8:12–15. [PubMed] [Google Scholar]
- 11.Fujii M, Nakashima Y, Jingushi S, Yamamoto T, Noguchi Y, Suenaga E, Iwamoto Y. Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:9–13. doi: 10.1097/BPO.0b013e318190a0be. [DOI] [PubMed] [Google Scholar]
- 12.Ganz R, Horowitz K, Leunig M. Algorithm for femoral and periacetabular osteotomies in complex hip deformities. Clin Orthop Relat Res. 2010;468:3168–3180. doi: 10.1007/s11999-010-1489-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garras DN, Crowder TT, Olson SA. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br. 2007;89:721–724. doi: 10.1302/0301-620X.89B6.18805. [DOI] [PubMed] [Google Scholar]
- 14.Gudmundsson G. Intertrochanteric displacement osteotomy for painful osteoarthritis of the hip. Acta Orthop Scand. 1970;41:91–109. doi: 10.3109/17453677008991981. [DOI] [PubMed] [Google Scholar]
- 15.Hadley NA, Brown TD, Weinstein SL. The effects of contact pressure elevations and aseptic necrosis on the long-term outcome of congenital hip dislocation. J Orthop Res. 1990;8:504–513. doi: 10.1002/jor.1100080406. [DOI] [PubMed] [Google Scholar]
- 16.Ilizaliturri VM, Jr, Chaidez PA, Valero FS, Aguilera JM. Hip arthroscopy after previous acetabular osteotomy for developmental dysplasia of the hip. Arthroscopy. 2005;21:176–181. doi: 10.1016/j.arthro.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 17.Ippolito E, Yoshiaki I, Ponseti I. Histologic, histochemical, and ultrastructural studies of the hip joint capsule and ligamentum teres in congenital dislocation of the hip. Clin Orthop Relat Res. 1980;146:246–258. [PubMed] [Google Scholar]
- 18.Katz DA, Kim YJ, Millis MB. Periacetabular osteotomy in patients with Down’s syndrome. J Bone Joint Surg Br. 2005;87:544–547. doi: 10.1302/0301-620X.87B4.15314. [DOI] [PubMed] [Google Scholar]
- 19.Kelly BT, Philippon M. Arthroscopic hip anatomy. In: Callaghan J, Rosenberg A, Rubash H, editors. The Adult Hip. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. pp. 78–79. [Google Scholar]
- 20.Kim YJ, Jaramillo D, Millis MB, Gray ML, Burstein D. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am. 2003;85:1987–1992. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 21.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 22.Klein SE, Morgan P, Schoenecker PL, Clohisy JC. Arthroscopic treatment of labral tears after a previous Pemberton osteotomy. J Pediatr Orthop. 2010;30:549–553. doi: 10.1097/BPO.0b013e3181e4f575. [DOI] [PubMed] [Google Scholar]
- 23.Ladner B, Nester K, Cascio B. Abdominal fluid extravasation during hip arthroscopy. Arthroscopy. 2010;26:131–135. doi: 10.1016/j.arthro.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Leunig M, Ganz R. The Bernese method of periacetabular osteotomy] [in German. Orthopade. 1998;27:743–750. doi: 10.1007/pl00003460. [DOI] [PubMed] [Google Scholar]
- 25.Mardam-Bey TH, MacEwen GD. Congenital hip dislocation after walking age. J Pediatr Orthop. 1982;2:478–486. doi: 10.1097/01241398-198212000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 27.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg Am. 2010;92(suppl 1 pt 2):115–129. doi: 10.2106/JBJS.J.00646. [DOI] [PubMed] [Google Scholar]
- 28.Maxian TA, Brown TD, Weinstein SL. Chronic stress tolerance levels for human articular cartilage: two nonuniform contact models applied to long-term follow-up of CDH. J Biomech. 1995;28:159–166. doi: 10.1016/0021-9290(94)00054-8. [DOI] [PubMed] [Google Scholar]
- 29.McCarthy JC, Lee JA. Acetabular dysplasia: a paradigm of arthroscopic examination of chondral injuries. Clin Orthop Relat Res. 2002;405:122–128. doi: 10.1097/00003086-200212000-00014. [DOI] [PubMed] [Google Scholar]
- 30.McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award. The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Michaels G, Matles AL. The role of the ligamentum teres in congenital dislocation of the hip. Clin Orthop Relat Res. 1970;71:199–201. doi: 10.1097/00003086-197007000-00023. [DOI] [PubMed] [Google Scholar]
- 32.Millis M, Kocher M. Hip, pelvis, femur: pediatric aspects. In: Koval K, editor. Orthopaedic Knowledge Update 7. Chicago, IL: American Academy of Orthopaedic Surgeons; 2002. pp. 387–394. [Google Scholar]
- 33.Murphy SB, Millis MB, Hall JE. Surgical correction of acetabular dysplasia in the adult: a Boston experience. Clin Orthop Relat Res. 1999;363:38–44. doi: 10.1097/00003086-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Nepple JJ, Carlisle JC, Nunley RM, Clohisy JC. Clinical and radiographic predictors of intra-articular hip disease in arthroscopy. Am J Sports Med. 2011;39:296–303. doi: 10.1177/0363546510384787. [DOI] [PubMed] [Google Scholar]
- 35.Nishii T, Sugano N, Tanaka H, Nakanishi K, Ohzono K, Yoshikawa H. Articular cartilage abnormalities in dysplastic hips without joint space narrowing. Clin Orthop Relat Res. 2001;383:183–190. doi: 10.1097/00003086-200102000-00020. [DOI] [PubMed] [Google Scholar]
- 36.Noguchi Y, Miura H, Takasugi S, Iwamoto Y. Cartilage and labrum degeneration in the dysplastic hip generally originates in the anterosuperior weight-bearing area: an arthroscopic observation. Arthroscopy. 1999;15:496–506. doi: 10.1053/ar.1999.v15.015049. [DOI] [PubMed] [Google Scholar]
- 37.Paliobeis CP, Villar RN. The prevalence of dysplasia in femoroacetabular impingement. Hip Int. 2011;21:141–145. doi: 10.5301/HIP.2011.7422. [DOI] [PubMed] [Google Scholar]
- 38.Parvizi J, Bican O, Bender B, Mortazavi SM, Purtill JJ, Erickson J, Peters C. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24:110–113. doi: 10.1016/j.arth.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 39.Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169–174. doi: 10.1016/j.arthro.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 40.Ranawat CS, Atkinson RE, Salvati EA, Wilson PD., Jr Conventional total hip arthroplasty for degenerative joint disease in patients between the ages of forty and sixty years. J Bone Joint Surg Am. 1984;66:745–752. [PubMed] [Google Scholar]
- 41.Ross JR, Zaltz I, Nepple JJ, Schoenecker PL, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011;39(suppl):72S–78S. doi: 10.1177/0363546511412320. [DOI] [PubMed] [Google Scholar]
- 42.Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH., Jr Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232–240. doi: 10.1097/00003086-200101000-00031. [DOI] [PubMed] [Google Scholar]
- 43.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed] [Google Scholar]
- 44.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. doi: 10.1097/00003086-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–183. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 46.Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85. doi: 10.2106/00004623-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 47.Wiberg G. Acetabular dysplasia and osteoarthritis. Acta Chir Scand. 1939;83(suppl 58):5–135. [Google Scholar]
- 48.Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006;88:1915–1919. doi: 10.2106/JBJS.E.00715. [DOI] [PubMed] [Google Scholar]


