Abstract
Background
Femoroacetabular impingement (FAI) has been recognized as a common cause of hip pain as well as a cause of hip arthritis, yet despite this, little is known about the etiology of the cam morphology or possible risk factors associated with its development.
Questions/purposes
The purposes of our study were to determine when the cam morphology associated with FAI developed in a cross-sectional cohort study of pediatric patients pre- and postphyseal closure using MRI and whether increased activity level during the period of physeal closure is associated with an increased likelihood that the cam deformity will develop.
Methods
Alpha angles were measured at the 3 o’clock (anterior head-neck junction) and 1:30 (anterosuperior head-neck junction) positions in both hips with a cam deformity defined as an alpha angle ≥ 50.5° at the 3 o’clock position. Forty-four volunteers (88 hips) were studied: 23 with open physes (12 females, mean age 9.7 years; 11 males, age 11.7 years) and 21 with closed physes (five females, age 15.2 years; 16 males, age 16.2 years). Daily activity level using the validated Habitual Activity Estimation Scale was compared for patients in whom cam morphology did and did not develop.
Results
None of the 23 (0%) patients prephyseal closure had cam morphology, whereas three of 21 (14%, p = 0.02; all males) postclosure had at least one hip with cam morphology. Daily activity level was higher (p = 0.02) for patients with the cam morphology (7.1 hours versus 2.9 hours). Mean alpha angles at the 3 o’clock head-neck position were 38° (95% confidence interval [CI], 37.2°–39.1°) in the open physes group and 42° (95% CI, 40.16°–43.90°) in the closed physes group; at the 1:30 head-neck position, they were 45° (95% CI, 44.0°–46.4°) in the open physes group and 50° (47.9°–52.3°) in the closed physes group.
Conclusions
The fact that cam morphology was present exclusively in the closed physeal group strongly supports its development during the period of physeal closure with increased activity level as a possible risk factor.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Over the last decade, femoroacetabular impingement (FAI) has become an active clinical and investigational area in both the diagnosis and treatment of the young adult with hip pain as well as in our understanding of the degenerative process within the hip [1]. As early as the 1960s, Murray and Duncan [18] identified a structural abnormality of the femoral head-neck junction as a potential cause of hip arthritis, which was later coined the pistol grip deformity and defined as cam-type FAI leading to “outside-in” mechanical damage of the acetabular cartilage [3, 6, 12, 22, 29, 31]. FAI has become of significant interest as a result of its high prevalence in athletes and active young adults [14] as well as in patients with groin and/or hip pain and labral pathology [16]. However, very little is currently known about the natural history of cam-type FAI before the onset of symptoms nor about the etiology of the deformity. Recent work has established the prevalence of cam-type FAI in the general adult population to be 10% to 15% [17]. Hack et al. [9] found the prevalence of cam deformity to be significantly higher in males than females, 24.7% versus 5.4%. In another study in male patients only, a prevalence of 24% was also found [25]. However, it is still unclear why and when the deformity first appears. Some have proposed that the deformity develops as a response to strenuous physical activities during childhood [18, 27], whereas others have argued that it develops in response to increased loading of the hip and is an adaptive rather than a pathologic process [20, 21]. Finally, other hypotheses have included the deformity reflecting a subclinical slipped capital femoral epiphyseal injury [5, 7, 13] or another form of unrecognized childhood disorder or disease process [28].
The purposes of this study were to determine when the cam morphology associated with FAI developed in a cross-sectional cohort of pediatric patients pre- and postphyseal closure using MRI and whether increased activity level during the period of physeal closure is associated with an increased likelihood that the cam deformity will develop.
Patients and Methods
The study was reviewed and approved by the research ethics board at the Children’s Hospital of Eastern Ontario. The study was designed as a prospective cross-sectional analysis, comparing the radiological morphology of hips before and after physeal closure of the proximal femur. For open physes subjects, inclusion criteria included males between the ages of 10 and 12 years and females between the ages of 8 and 10 years. For closed physes subjects, inclusion criteria were males between the ages of 15 and 18 years and females between the ages of 14 and 18 years. Age ranges were chosen to reflect age spans where under normal circumstances (ie, no previous injury or infection to physis and no systemic or physeal developmental diseases), the growth plate would be reliably either open or functionally “closed” (beyond the peak growth period) [1, 4]. Study volunteers did not have radiographic bone age assessed, because there was no clinical indication for radiographs. Bone-age radiographs were not approved by our research ethics board to avoid clinically unnecessary radiation. Exclusion criteria for both groups were a history of more than one previous fracture or vertebral fracture, any history of lower extremity pathology or surgery, any hip or knee pain, any form of arthritis, or any known congenital or developmental musculoskeletal disorder.
Volunteer study subjects were recruited from the fracture clinic at the Children’s Hospital of Eastern Ontario. Subjects and/or their parents or guardians gave informed consent for the study. Patient demographic information was recorded, including body mass index, ethnicity, and family history of hip arthritis. In addition, a validated pediatric activity score was administered: the Habitual Activity Estimation Scale (HAES) [11]. Depending on age, the HAES is either self-reported or parent-reported and quantifies the duration, in hours, of four levels of activity ranging from very inactive (lying down, napping), somewhat inactive (sitting, reading, watching television, playing video games), somewhat active (walking, light chores), to very active (running, bicycling, activities leading to sweating or breathing hard) over a complete waking day. The HAES is typically administered for both a typical weekday and a Saturday and can be used from infancy through adolescence. It has been shown to be both a valid and reliable form of quantifying levels of physical activity in various pediatric populations [10, 30].
Each subject underwent MRI of bilateral hips and a focused clinical hip examination by a single observer (SC) using a goniometer. Participants were supine with internal rotation measured with the hip in 90° of hip flexion. No sedation or contrast was used. The examinations were carried out on a 1.5-T MRI scanner (GE HDxt v15 1.5 Tesla MRI; GE Healthcare, Little Chalfont, Buckinghamshire, UK) with a phased array surface coil placed anteriorly over the pelvis and with spine phased array coils situated posteriorly. Subjects were supine with their feet held in neutral position. The MRI sequence was an axially acquired, three-dimensional isotropic, T1-weighted spoiled gradient with the following parameters: field of view 40 cm, slice thickness 1 mm, acquisition matrix 384 × 256, TR/TE/flip angle = 11.4 ms/4.0 ms/205°, 1 average. Multiplanar reformation (MPR) was carried out to generate radial images, using the center of the femoral neck as the axis of rotation, with 2-mm thick images generated at 30° intervals. Acquisition and MPR images were sent to PACS (PACS system Siemens Syngo Workflow version 30B; Siemens AG, Erlangen, Germany) for review. MR images were read in a blinded fashion by a fellowship-trained musculoskeletal radiologist (KR). The alpha angle of Notzli et al. was measured at two positions along the femoral head-neck junction, anterior and anterosuperior denoted the 3:00 and 1:30 clock face locations, respectively, as per Pfirrmann et al. [23] and Rakhra et al. [24]. A best-fit circle was drawn around the perimeter of the femoral head. The first arm of the angle is the long axis of the femoral neck, defined as a line drawn between the center of the femoral neck at its narrowest point and the center of the circle. The second arm of the angle was drawn from the center of the circle anteriorly to the point where the femoral head extended beyond the margin of the circle. Previous research studies have reported a value of greater than or equal to 50.5° at the 3 o’clock position as indicative of an abnormal head-neck junction consistent with a cam deformity [2, 23, 24].
Body mass index (BMI) was calculated as body mass in kilograms divided by height in meters squared. Statistical analyses were performed with significance set at 0.05 and included chi square testing as well as the Student’s t-test. Multivariate subgroup analyses and analyses of variance were also performed, including controls for age (or physeal status) and sex. In assessing physical activity, both sex and age were important to control given their different established norms [10, 30].
A total of 44 volunteers were recruited with a mean age of 13.1 years (range, 8–18 years) and included 27 boys and 17 girls with a mean BMI of 20.9 kg/m2 (range, 13.7–34 kg/m2) (Table 1). There were 23 in the open physes group with 11 boys and 12 girls who had mean ages of 11.7 years (range, 10–12 years) and 9.7 years (range, 8–10 years), respectively. There were 21 in the closed physes group with 16 girls and five boys; these subjects had mean ages of 16.2 years (range, 15–17 years) and 15.2 years (range, 14–15 years) (Table 2), respectively.
Table 1.
Demographics: pre- versus postphyseal closure groups
| Variable | Open physes (n = 23) | Closed physes (n = 21) | p value |
|---|---|---|---|
| Sex (male/female) | 11/12 | 16/5 | 0.07 |
| Age (years) | 10.5 (1.4) | 15.9 (0.9) | < 0.001 |
| Height (cm) | 145.2 (11.5) | 171.5 (7.0) | < 0.001 |
| Weight (kg) | 42.8 (15.5) | 64.8 (11.4) | < 0.001 |
| Body mass index (kg/m2) | 19.8 (4.3) | 22.0 (3.6) | < 0.001 |
Table 2.
Alpha angle by physeal closure at the 3:00 and 1:30 positions
| Position | Mean alpha angle | SD | Range | 95% CI |
|---|---|---|---|---|
| Open physes (n = 46) | ||||
| Anterior (3:00) | 38.11 | 3.23 | 32.00–48.80 | 37.15–39.07 |
| Anterosuperior (1:30) | 45.20 | 4.08 | 37.80–57.00 | 43.99–46.42 |
| p < 0.001 | ||||
| Closed physes (n = 42) | ||||
| Anterior (3:00) | 42.04 | 6.03 | 32.00–58.30 | 40.16–43.90 |
| Anterosuperior (1:30) | 50.05 | 7.05 | 39.90–64.60 | 47.85–52.25 |
| p < 0.001 |
CI = confidence interval.
Results
MRI of Hips
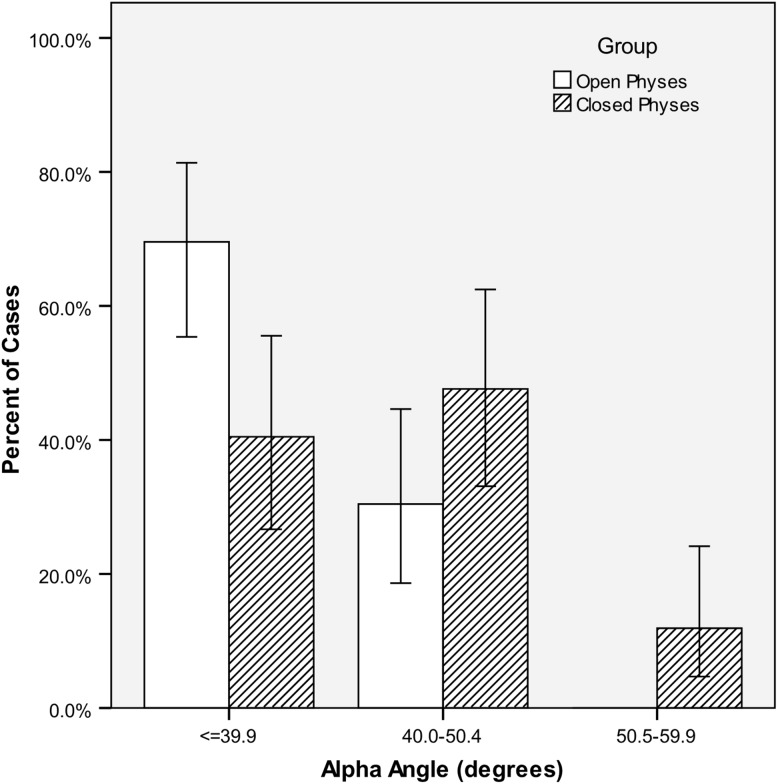
The cam morphology was only seen in in the closed group, which also had overall different head/neck morphology compared with the open physes group quantified by the alpha angle at both the 3 o’clock and 1:30 positions (Fig. 1). For the 46 hips with open physes, the mean alpha angle at the 3 o’clock and 1:30 positions were 38º and 45º, respectively (p < 0.001), whereas for the 42 hips with closed physes, the mean alpha angle at the 3 o’clock and 1:30 positions were 42º and 50º (p < 0.001), respectively (Table 2). Representative images from the 1:30 radial position can be found of a patient with an open physis (Fig. 2) and of a patient with a closed physis (Fig. 3). When comparing the closed and open physes groups, the mean alpha angles were significantly higher in the closed physes group compared with the open physes at both the 3 o’clock position (42.0º ± 6.0 SD versus 38.1º ± 3.2 SD, p < 0.001) and at the 1:30 position (50.1º ± 4.08 SD versus 45.2º ± 7.05 SD, p < 0.001). Using a cutoff value of ≥ 50.5° at the 3 o’clock position, no hips had cam-type morphology in the open physes group, whereas five of 42 hips (12%) had cam morphology (chi square = 5.81, p = 0.02) with two patients having bilateral deformities. This corresponded with three of 21 (14%) of postclosure volunteers having at least one cam morphology. All hips with cam-type morphology were males, although the difference between male and female rates did not achieve statistical significance (chi-square = 3.34, p = 0.15).
Fig. 1.
Comparison of the open physes and closed physes groups with respect to alpha angle results at the 3:00 position. Closed physes hips showed greater alpha angles.
Fig. 2.
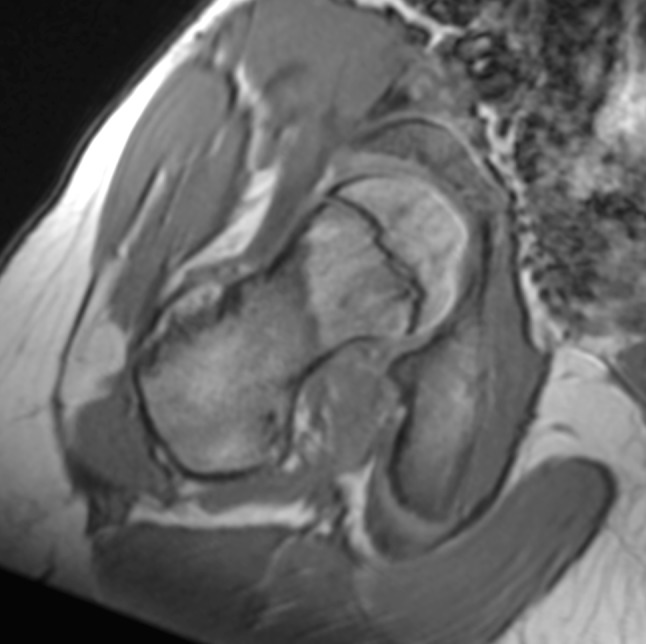
Representative MRI of a 12-year-old boy with an alpha angle of 49° at the 1:30 position. Note the open physis but normal head-neck contour.
Fig. 3.
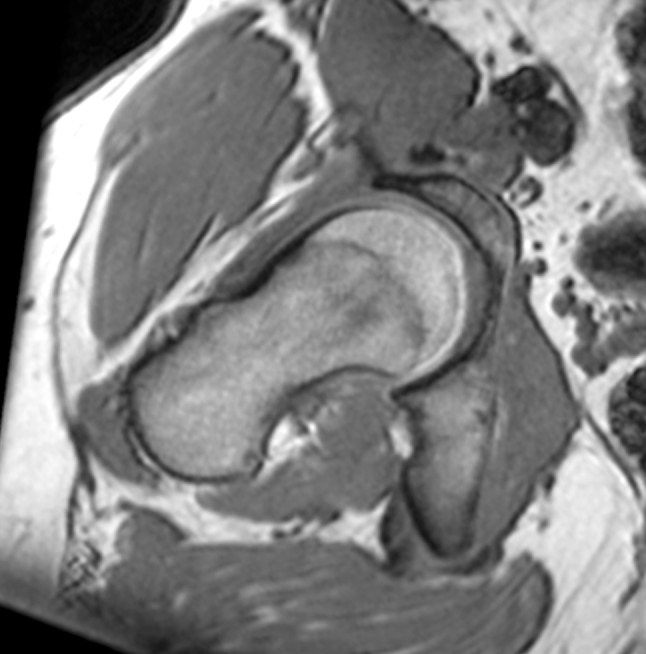
MRI of a 16-year-old boy with an alpha angle of 63° at the 1:30 position with typical cam morphology.
A significant difference was found between sexes in the closed physes group. Boys had a significantly higher mean alpha angle in the closed physes group at the 3:00 position (43.4º ± 6.0 SD versus 37.8º ± 4.0 SD, p = 0.009). The difference at the 1:30 position (51.2º ± 7.5 SD versus 46.4º ± 3.5 SD, p = 0.056) was not quite statistically significant.
Physical Examination Findings Before and After Physeal Closure
Physical examination of the hips of all subjects found no positive impingement signs, but patients with closed physes and cam morphology had less internal rotation than those without that radiographic finding (21º ± 4.2 SD versus 38º ± 10.3 SD; p = 0.001). Results of testing of internal rotation of the hip showed a mean of 55º ± 14.5 SD in the open physes group and 36º ± 11.2 SD (p < 0.001, t-test) in the closed physes group.
Habitual Activity Estimation Scale
Males within the closed physes group who had cam morphology on MRI had significantly higher levels of activity on HAES. When the closed physes group was subdivided and HAES results of only the males were examined, analyses of variance controlled for age showed the mean “very active” hours on Saturdays was 7.1 (± 1.59 SE) in those with at least one hip with an alpha angle ≥ 50.5º (subjects positive for cam morphology) compared with 2.9 hours (± 0.51 SE) in those with alpha angles < 50.5º (p = 0.02). “Somewhat active” hours during weekdays were 6.6 (± 1.00 SE) in those positive for cam morphology versus 4.4 hours (± 0.32 SE) in those without (p = 0.056) (Table 3). Two-way analyses of variance by group (open/closed) and sex uncovered no significant differences for total active hours on either weekdays or Saturdays. Mean active hours in the open physes group were 7.3 (± 2.34 SD) during weekdays and 8.2 (± 2.65 SD) on Saturdays; mean active hours in the closed physes group were 7.2 (± 3.17 SD) during weekdays and 7.4 (± 2.99 SD) on Saturdays. The closed physes group had significantly higher (p < 0.037) hours of inactivity than the open physes group on weekdays (8.1 versus 6.4). However, with the numbers available, this finding was not significant after controlling for age. Mean hours of inactivity in the open physes group were 6.5 (± 2.07 SD) during weekdays and 5.9 (± 3.02 SD) on Saturdays; mean hours of inactivity in the closed physes group were 8.0 (± 3.34 SD) during weekdays and 6.3 (± 2.33 SD) on Saturdays. Two-way analyses of variance for age and sex demonstrated a significantly higher (p < 0.039) BMI among the closed group (21.9 versus 19.4 kg/m2) (Fig. 3).
Table 3.
Habitual Activity Estimation Score (HAES), analysis of variance: boys in the closed physes group comparing those with versus without cam morphology of the hip
| Hours | SE | p value | F ratio | |
|---|---|---|---|---|
| Somewhat active weekday | ||||
| Cam morphology (3) | 6.56 | 1.00 | 0.056 | 3.93 |
| No cam (29) | 4.43 | 0.32 | ||
| Very active Saturday | ||||
| Cam morphology (3) | 7.06 | 1.59 | 0.02 | 5.92 |
| No cam (29) | 2.94 | 0.51 | ||
Discussion
Asphericity of the femoral head-neck junction known as cam-type FAI, without a history of Perthes [15] or slipped capital femoral epiphysis [5, 13], has been recently recognized in young adults as an important source of hip pain and cause of cartilage damage predisposing to degenerative arthritis [18]. Understanding how the femoral head-neck morphology develops during skeletal growth may provide insight into the etiology of the cam deformity as well as the potential for early screening and even intervention. Based on recent studies, the prevalence of cam morphology in the adult population is between 14% and 15% [9] with males having a significantly higher prevalence than females (9.6%–24% versus 5%) [8, 9, 26]. More importantly, the morphology of the femoral head-neck junction is such that the alpha angle measurements are significantly higher at the anterosuperior femoral head-neck position (1:30 radial position) compared with the anterior position (3:00 radial position). In our study, the cam deformity was only observed in subjects who were postphyseal closure, consistent with the theory that the deformity is a developmental phenomenon. The fact that the deformity was more frequently observed in males is consistent with adult studies with greater alpha angles being measured at the anterosuperior position compared with the anterior position. Level of activity, measured with the validated HAES score, was higher in the subjects positive for cam morphology as compared with group- and sex-matched comparators. This lends further support to the hypothesis that physical activity is somehow related to the development of cam morphology.
There are a number of limitations with our study. One of them is the lack of radiological bone age of patients declined by our ethics board as a result of concerns of radiation exposure. On the other hand, we ensured at the time of recruitment that the patient age groups would be quite distinct to provide some validity to our determination of open versus closed physes, and the volunteers were all healthy with no predisposing factors that would be expected to affect bone age and therefore their chronological and bone ages would be expected to be consistent [1, 4]. Another limitation is that this study was a cross-sectional analysis and not a prospective longitudinal study; as such, we only observed the subjects at a single time point, limiting our findings to one of prevalence and not of incidence. However, the main purpose of our study was to determine when the cam morphology associated with FAI developed in a cohort of pediatric patients as well as executing the MRIs in a research context to determine the prevalence of cam deformity as well as morphology of the femoral head-neck junction pre- and postphyseal closure. Although we recruited a smaller number of patients in each arm compared with adult studies, our findings are in line with what has been published in the literature in regard to both prevalence and femoral head-neck morphology providing some certainty to our results. In addition, the individuals with a cam deformity had significantly less internal rotation (IR) than those without a cam deformity (21° versus 38°), which again is consistent with the clinical presentation of patients with cam FAI [9]. Interestingly, the group prephyseal closure also exhibited greater ROM in IR than the overall postphyseal closure group (55° versus 36°) further supporting the correlation between femoral head-neck morphology (ie, clearance) and hip ROM. Further study will be necessary in better identifying risk factors other than male sex for developing cam-type deformities and in better delineating the role of intensity of physical activity.
The published prevalence of cam-type FAI morphology in asymptomatic adults in the largest published data set showed a general prevalence of 14.0% [9]. This compares very well with our finding of 14% of closed physis individuals having a cam-type morphology. When looking at males, the published prevalence is 24.7% [9], whereas in our group of 16 closed physis males, we had three positive for FAI morphology, amounting to a prevalence of 19%. In women the prevalence was 5.4% [9], whereas we did not have any females with cam morphology but this may be the result of our relatively small number of females in our closed physeal group (five). The only other study that evaluated the prevalence of cam FAI morphology in the pediatric population is that of Siebenrock et al. [27] in which they retrospectively matched athletic individuals (ie, playing basketball) during their growth spurt with a group of children with a normal activity level. They reported a cam morphology prevalence of 8.3% in the closed physes group, whereas they saw no cam morphology in the open physes or transitional groups. Having said that, it is unclear why they choose basketball as an at risk activity because activities like football and hockey also are commonly associated with this deformity [14, 19]. This could have introduced patient selection bias. In contrast, our study used a validated pediatric activity score, which also quantifies periods of inactivity making a more sensitive and descriptive tool. These results highlight the strong association between activity level and the development of proximal femoral head-neck morphology and is consistent with the initial hypothesis of Murray and Duncan in 1971 [18] of the association of the tilt deformity and activity level. However, how this translates into which sporting intensity level results into abnormal head-neck morphology is unclear because type of sporting activity was not recorded and needs to be better understood to better counsel parents and schools in regard to activities.
The impact of physiological loading on the physes’ development has long been suspected with silent slipped capital femoral epiphysis being associated with early arthritic changes [5, 13]. If clear evidence were to show a direct link between even mild slipped capital femoral epiphysis with FAI, it might have an effect on our treatment decision for clinical slipped capital femoral epiphysis (ie, to reduce or plan for deformity correction after healing). The hypothesis that the cam deformity may be a normal physiological response to loading forces [21] is in fact not in opposition to the other etiological theories. Ng and Ellis [21] highlighted that when a physis or portion thereof is disrupted through abnormal loading, biomechanics, vascularity, or trauma, this can have significant effects on the morphological development of the hip. Our study group did also show significant differences in activity levels of boys in the closed physes group between those with and without cam morphology despite a small sample size of cam morphology-positive hips. Because we did not select our cohorts based on activity level, our data can be considered quite representative of the general population. Further studies should include larger patient cohorts with a wide variety of activity levels to better understand the at-risk activities.
Deciding on the optimal plane of measurement for the alpha angle is still evolving from Notzli’s [22] original description of the alpha angle using oblique axial cuts to the current standard of radial imaging. This represents a logical evolution because Ito et al’s [12] original description of the deficient femoral head-neck offset in cam FAI clearly demonstrated that the circumference of the deformity clearly extended from the anterior to anterolateral quadrants. Interestingly, the significant sex difference in regard to location and size of the cam deformity was already noted with males tending to have larger deformities at the anterolateral quadrant compared with the anterior quadrant in females. Subsequent to the Ito and Notzli papers, Pfirrmann et al. [23] and Rakhra et al. [24] have demonstrated the increased sensitivity of the radial imaging for diagnosing cam FAI. The difference in alpha angle values at the 3:00 versus 1:30 radial positions (8.1° in the closed physes group and 7.1° in the open physes group) is similar to the published difference in values among adults (9.4° difference in adults [9]). This reinforces the importance of standardized alpha angle measurement regardless of age.
The presence of cam morphology in the closed physeal group only strongly supports its development during the period of physeal closure with increased activity level as a possible risk factor. More importantly, the femoral head-neck morphology influences the hip’s ROM with smaller alpha angles being associated with greater internal rotation in both the prephyseal and postphyseal closure groups as well as in those without a cam deformity. Finally, what represents a cam deformity at risk of developing symptoms as well as degenerative changes remains to be defined as well as methods to screen for it. Future studies are required to determine which clinical factors (patient activity level, BMI, sex, genetics) influence the development of the cam deformity, because there may be modifiable risk factors in its development.
Acknowledgments
We acknowledge the contributions of the Children’s Hospital of Eastern Ontario Bone Health Research Team, Steve Anderson, and Kyle Kemp, who have been integral to the completion of the study.
Footnotes
This research project was funded through only internal funding, from the Children’s Hospital of Eastern Ontario Bone Health Research Group (LMW) and the Department of Surgery Research Fund (RBW) as well as The Discovery Fund (PEB).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This research was performed at the Children’s Hospital of Eastern Ontario, Ottawa, Ontario, Canada.
References
- 1.Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. 1963;45:1–14. [PubMed] [Google Scholar]
- 2.Beaule PE, Zaragoza EJ, Motamedic K, Copelan N, Dorey J. Three-dimensional computed tomography of the hip in the assessment of femoro-acetabular impingement. J Orthop Res. 2005;23:1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 4.Dimeglio A. Growth in pediatric orthopaedics. J Pediatr Orthop. 2001;21:549–555. [PubMed] [Google Scholar]
- 5.Fraitzl CR, Kafer W, Nelitz M, Reichel H. Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean follow-up of 14.4 years after pinning in situ. J Bone Joint Surg Br. 2007;89:1592–1596. doi: 10.1302/0301-620X.89B12.19637. [DOI] [PubMed] [Google Scholar]
- 6.Ganz R, Parvizi J, Leunig M, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 7.Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR. Sublinical slipped capital femoral epiphysis. J Bone Joint Surg Am. 1997;79:1489–1497. doi: 10.2106/00004623-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint:a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49:436–441. doi: 10.1080/02841850801935567. [DOI] [PubMed] [Google Scholar]
- 9.Hack K, Diprimio G, Rakhra K, Beaule PE. Prevalence of CAM type femoroacetabular impingement in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 10.Hay JA. Development and testing of the Habitual Activity Estimation Scale. In: Armstrong N, ed. Children and Exercise XIX. Volume 2006. 2nd ed. Exeter, UK: Singer Press; 1997:125–129.
- 11.Hay JA, Cairney J. Development of the Habitual Activity Estimation Scale for clinical research: a systematic approach. Ped Exerc Sci. 2006;18:193–202. [Google Scholar]
- 12.Ito K, Minka-II MA, Leunig S, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 13.Kamegaya M, Saisu T, Nakamura J, Murakami R, Segawa Y, Wakou M. Drehmann sign and femoro-acetabular impingement in SCFE. J Pediatr Orthop. 2011;31:853–857. doi: 10.1097/BPO.0b013e31822ed320. [DOI] [PubMed] [Google Scholar]
- 14.Kapron AL, Anderson AE, Aoki SK, Phillips LG, Petron DJ, Toth R, Peters CL. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93:10–e111. doi: 10.2106/JBJS.K.00544. [DOI] [PubMed] [Google Scholar]
- 15.Kim YJ, Novais EN. Diagnosis and treatment of femoroacetabular impingement in Legg-Calve-Perthes disease. J Pediatr Orthop. 2011;31:S235–S240. doi: 10.1097/BPO.0b013e3182260252. [DOI] [PubMed] [Google Scholar]
- 16.Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616–622. doi: 10.1007/s11999-008-0646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leunig M, Beck M, Dora C, Ganz R. Femoroacetabular impingement: trigger for the development of coxarthrosis. Orthopade. 2006;35:77–84. doi: 10.1007/s00132-005-0896-4. [DOI] [PubMed] [Google Scholar]
- 18.Murray RO, Duncan C. Athletic activity in adolescence as an etiological factor in degenerative hip disease. J Bone Joint Surg Br. 1971;53:406–419. [PubMed] [Google Scholar]
- 19.Naal FD, Miozzari HH, Wyss TF, Notzli HP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011;39:544–550. doi: 10.1177/0363546510387263. [DOI] [PubMed] [Google Scholar]
- 20.Ng VY, Ellis TJ. Letter to the editor: the cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469:3506–3507. doi: 10.1007/s11999-011-2091-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ng VY, Ellis TJ. More than just a bump: cam-type femoroacetabular impingement and the evolution of the femoral neck. Hip Int. 2011;21:1–8. doi: 10.5301/HIP.2011.6288. [DOI] [PubMed] [Google Scholar]
- 22.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 23.Pfirrmann CW, Mengiardi B, Dora C, Kalverer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characterstic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 24.Rakhra K, Sheikh AM, Allen DJ, Beaule PE. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:660–665. doi: 10.1007/s11999-008-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reichenbach S, Juni P, Werlen S, Nuesch E, Pfirrmann CW, Trelle S, Odermatt A, Hofstetter W, Ganz R, Leunig M. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res (Hoboken). 2010;62:1319–1327. doi: 10.1002/acr.20198. [DOI] [PubMed] [Google Scholar]
- 26.Reichenbach S, Leunig M, Werlen S, Nuesch E, Pfirrmann CW, Bonel H, Odermatt A, Hofstetter W, Ganz R, Juni P. Association between cam-type deformities and magnetic resonance imaging-detected structural hip damage: a cross-sectional study in young men. Arthritis Rheum. 2011;63:4023–4030. doi: 10.1002/art.30589. [DOI] [PubMed] [Google Scholar]
- 27.Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, Mamisch TC. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469:3229–3240. doi: 10.1007/s11999-011-1945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: Cordell LD, Harris WH, Ramsey PL, MacEwen GD, editors. The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St Louis, MO, USA: CV Mosby; 1975. pp. 212–228. [Google Scholar]
- 29.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]
- 30.Wells GD, Wilkes DL, Schneiderman-Walker J, Elmi M, Tullis E, Lands LC, Ratjen F, Coates AL. Reliability and validity of the Habitual Activity Estimation Scale (HAES) in patients with cystic fibrosis. Pediatr Pulmonol. 2008;43:345–353. doi: 10.1002/ppul.20737. [DOI] [PubMed] [Google Scholar]
- 31.Wenger DE, Kendall KR, Miner M, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]