Abstract
Background
Many surgical interventions are used to treat osteonecrosis of the femoral head. The instance and distribution of these various procedures may give some insight into the practicing community’s understanding of the efficacy of these treatments. We therefore sought to determine trends in the types and numbers of procedures performed for atraumatic osteonecrosis from 1992 through 2008 in the United States.
Questions/purposes
(1) How has the overall incidence of surgical treatment for atraumatic osteonecrosis changed over this time period; and (2) how has the percentage of THA performed for osteonecrosis (compared with joint-preserving procedures) changed over this time period?
Methods
The Nationwide Inpatient Sample database was used to collect information for all patients who had an International Classification of Diseases, 9th Revision diagnosis of hip osteonecrosis between 1992 and 2008. Procedures were collated according to frequency, and trends were analyzed for joint-preserving and joint-replacing procedures.
Results
The total number of procedures performed over this time period for osteonecrosis of the hip increased from 3570 procedures to 6400 procedures per year. In 1992, 75% (n = 2678) of the procedures performed to treat osteonecrosis of the hip were THA, which increased to 88% (n = 5632) in 2008. The percentage of joint-preserving procedures consequently decreased from 25% to 12% over this period.
Conclusions
Previously, THA was believed to have poor survivorship and clinical results for the treatment of osteonecrosis of the hip, but reports since 1993 have suggested improved survivorship of these reconstructions. Our study suggests that surgeons have incorporated this into their practice patterns, in that an increasing percentage of patients with this diagnosis are treated with THA. Additionally, the total number of procedures performed for osteonecrosis has increased, which may reflect an improved awareness of this disease and more aggressive approaches to diagnosis and treatment.
Level of Evidence
Level III, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Atraumatic osteonecrosis is a disease process that was originally described in 1925 as ischemic necrosis of the hip and since that time has had various names, including atraumatic necrosis, avascular necrosis, and idiopathic necrosis [26]. Although it can affect any joint, it most commonly occurs in the hip. Despite a poorly understood pathophysiology, it is known that patients in their third decade of life are at highest risk and that there is an annual prevalence of 10,000 to 20,000 new cases per year in the United States [47]. Left untreated, the natural history of the disease will progress to end-stage degenerative joint disease in greater than 80% of symptomatic cases and nearly two-thirds of asymptomatic ones [46, 47, 51].
Treatment options have continued to evolve for osteonecrosis and include potential nonoperative pharmacotherapies (such as anticoagulants, bisphosphonates, shockwave therapy, or hyperbaric oxygen) [5, 6, 16, 17, 23, 24, 43, 52, 68]; joint-preserving surgeries (core decompression and various vascularized and nonvascularized bone grafting procedures) [18, 35, 36]; and joint-replacing surgeries, including THA. Although numerous treatment algorithms have been proposed to provide guidance to the treating physician [18, 19, 45, 58, 64], controversy remains surrounding the most appropriate surgery and at what stage of the disease process these procedures should be performed [9, 10, 34, 50, 59, 60].
In 2005, in an effort to better understand how the orthopaedic community treated this disease, the American Association of Hip and Knee Surgeons (AAHKS) conducted a study of their membership to determine the frequency of different procedures for the treatment of osteonecrosis of the femoral head [44]. The most frequently reported precollapse procedure was core decompression and the most frequently reported postcollapse procedure was THA. Because the reported incidence of THA has overall been increasing and projected to further increase in the coming decades [40], the goal of the present study was to determine trends in the types and numbers of procedures performed for secondary, nontraumatic osteonecrosis of the femoral head from 1992 through 2008 in the United States based on data from the National Inpatient Sample (NIS). Because osteonecrosis is a disease that may be difficult to treat, and has many different treatment options, the authors wanted to assess how treatment trends have changed since 1992 given advances in surgical implants, surgical techniques for osteonecrosis as well as to assess the practicing physician’s understanding of the efficacy of these treatments.
We therefore asked the following questions: (1) How has the overall incidence of surgical treatment changed over this time period; and (2) how has the percentage of THAs performed for osteonecrosis (compared with joint-preserving procedures) changed over this time period?
Patients and Methods
The NIS is a database maintained by the Agency for Healthcare Research and Quality and contains a longitudinal representative 20% sample of hospitals in the United States, tracking nearly 8 million hospitalizations per year [3]. All discharge records and information are cataloged each year and are subsequently stratified according to region, location, teaching status, and number of beds. For example, the NIS now contains data from 1051 hospitals located in 45 states. This represents a 20% stratified sample of all US hospitals from which sampling weights can be used to statistically estimate valid national totals. Review of this publicly available data set is exempt from review by our institutional review board.
All patients who had an International Classification of Diseases, 9th Revision diagnosis of osteonecrosis of the hip (733.42) between 1992 and 2008 were evaluated. The following procedure codes were extracted from the database for use in the analysis: core decompression (27299, s2325), nonvascular bone grafting (27170), free vascularized fibular graft (20955), angular or rotational osteotomy (27161), limited femoral head resurfacing (27125), THA (27130), conversion to THA (27090, 20680), and revision THA (27134, 27137, 27138).
The various procedure codes were then collated according to yearly frequency between 1992 and 2008, and trends were analyzed for joint-preserving and joint-replacing procedures. Core decompression, nonvascular bone grafting, free vascularized fibular graft, angular or rotational osteotomy, and limited femoral head resurfacing were considered joint-preserving procedures. Only THA was considered a joint-replacing procedure.
To answer the first question regarding the change in the overall incidence of surgical treatment of osteonecrosis, the total number of discharge records that was coded as an admission for osteonecrosis of the hip and had an associated procedure code listed here was collected. These records were then collated by year to evaluate the generalized trend in the total number of surgical cases performed to treat osteonecrosis between 1992 and 2008.
To answer the second question, regarding the percentage of joint-preserving procedures performed for osteonecrosis relative to the total number of osteonecrosis procedures performed, the same records were stratified based on whether the procedure was joint-preserving or joint-replacing, as detailed previously. Furthermore, the various types of joint-preserving procedures that were performed were analyzed to determine if there was a change in preferences for treating early stages of the disease.
Data analysis was carried out using JMP 8.2 statistical software (SAS Institute, Cary, NC, USA). To account for the stratified sampling used in the NIS database, weighted analysis was performed. Fisher’s exact test was used to compare proportional differences between various groups. Probability values of < 0.05 were considered significant for all analyses.
Results
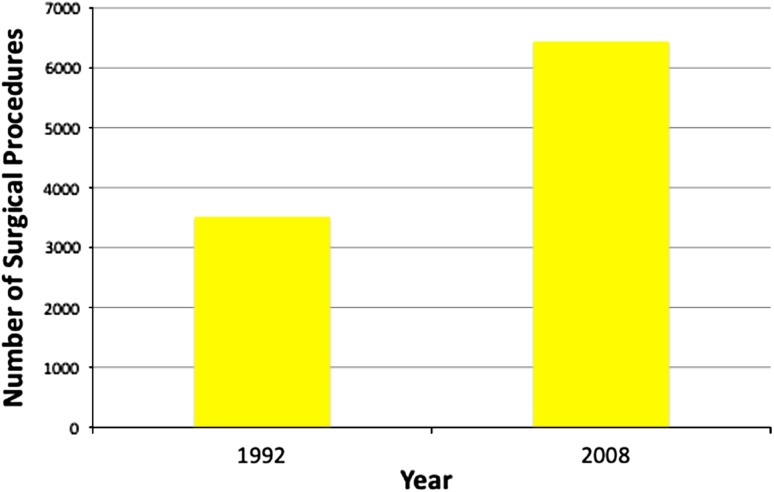
The total number of procedures performed over this time period for osteonecrosis of the femoral head increased from 3570 procedures to 6400 procedures per year (Fig. 1), nearly doubling over a 16-year time period (p < 0.001).
Fig. 1.
This figure represents the total number of surgical procedures performed for osteonecrosis of the femoral head.
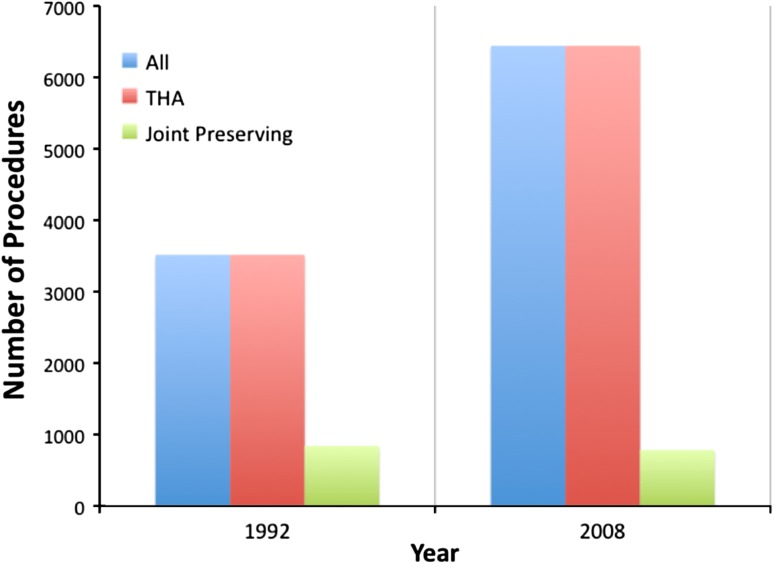
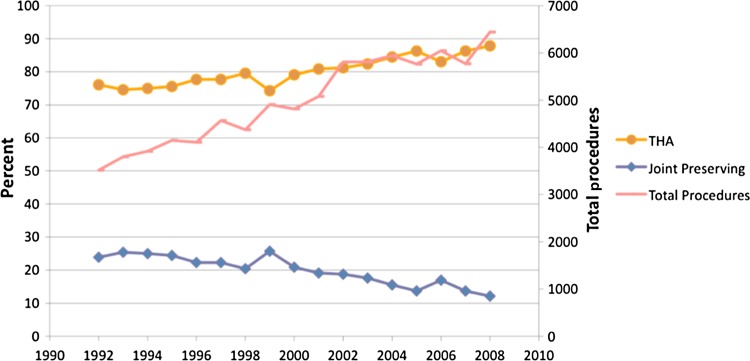
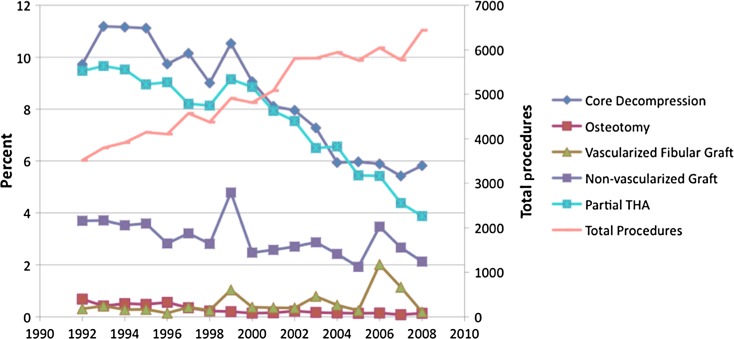
In 1992, 76% (n = 2678) of the procedures performed to treat osteonecrosis of the hip were THA. This increased to 88% (n = 5632 in 2008 (p < 0.001; Figs. 2, 3). The percentage of joint-preserving procedures consequently decreased from 25% to 12% over this same time period (p < 0.001; Fig. 3). The percentage of joint-preserving procedures as a fraction of total procedures decreased overall over the study period (Fig. 4).
Fig. 2.
This figure represents the total number of procedures performed for osteonecrosis of the femoral head stratified by THA or joint-preserving procedures.
Fig. 3.
Relative amounts of joint-preserving procedures are compared with THA. The primary Y axis (“Percent”; left axis) refers to each type of procedure; the secondary Y axis (“Total Procedures”; right axis) refers to the nominal number of total procedures performed during that year.
Fig. 4.
Relative amounts of joint-preserving procedures performed for osteonecrosis of the femoral head are here stratified by procedure. The primary Y axis (“Percent”; left axis) refers to each type of procedure (core decompression, osteotomy, vascularized fibular graft, nonvascularized graft, partial THA); the secondary Y axis (“Total Procedures”; right axis) refers to the nominal number of total procedures (joint- and nonjoint-preserving) performed during that year.
Discussion
Osteonecrosis is a potentially devastating disease with multiple treatment options and controversy both about the timing and the type of surgical intervention. Although some interventions have fallen from favor (at least in the United States) such as partial joint arthroplasty [2, 7, 8, 13, 63] and osteotomy [31, 53, 57, 66], other joint-preserving interventions remain in use, and THA also is an option. In an effort to better understand and characterize the evolution and distribution of the types of procedures performed in the United States between the years 1992 and 2008 for osteonecrosis of the hip, the NIS was used to assess the change in overall surgical treatment incidence as well as the breakdown of specific procedures performed during that time period. Such an analysis is important because many physicians will see only small numbers of patients with osteonecrosis and may not have extensive experience treating the disease. Consequently, the authors aimed to assess the prevalence of treatment options in an effort to better understand the practicing community’s understanding and preference in treating osteonecrosis.
There are several limitations to this study. Early precollapse disease is much less morbid than end-stage postcollapse disease, and it is not possible to distinguish the stage of the disease at the time of presentation based on the NIS database. Consequently, it is impossible to interpret if total joint arthroplasties are being performed on early- or late-stage lesions. If this were the case, it is possible that early precollapse lesions may have been treated with joint-replacing procedures rather than a more appropriate joint-preserving procedure. Similarly, there may be a number of patients who may not have been coded as osteonecrosis, but rather osteoarthritis if the patient may have had end-stage degenerative joint disease subsequent to osteonecrosis. This would increase the percentage and incidence of THA if higher numbers of these patients were included in the analysis. It is interesting to note that in 1999 there was an acute decrease in procedures reported in the NIS. Although the NIS is a longitudinal database, it is constantly expanded. This may reflect a change in the number of hospitals or a change in types of practices that were represented at various hospitals in the NIS. Another limitation is that age was not compared between treatment types in this analysis. Because younger patients may place higher demands on their implants, it may be of interest to see if there was a difference in age between treatment types. Future studies could assess this to determine whether age plays a factor in the treatment algorithm. Despite these limitations, we believe the results of this study effectively demonstrate the trends of the practice community in their treatment of this difficult disease, which in turn may be a reflection of the understanding of treatment options and their efficacy.
Previously, THA had poor reported survivorship and clinical results for the treatment of osteonecrosis of the hip. However, reports since 1993 have suggested improved outcomes in patients with osteonecrosis with survivorship reportedly improving from as low as 38% before 1993 [1, 12, 27, 48, 60, 62] to most studies reporting survivorship greater than 80% since 1993 [4, 9, 11, 14, 15, 20–22, 25, 28–30, 32, 33, 37–39, 41, 42, 49, 54–56, 61, 65, 67, 69–72]. The trends reported in this study may suggest that providers have taken heed of this and are using THA more frequently. Additionally, although the percentage of joint-preserving procedures has decreased, the total number of procedures (such as core decompression and bone grafting procedures) has increased. This suggests that despite a lower percentage, the number of patients who receive a joint-preserving procedure and may not require an arthroplasty has increased.
We found an increased percentage of cases performed for osteonecrosis were joint-replacing procedures. An earlier study [39] surveyed surgeons in the AAHKS to ascertain their preferred surgical procedures based on the Steinberg classification system [64]. That study, which had a response rate of 53% (403 of 760), found that core decompression was the preferred treatment option for symptomatic precollapse lesions (Steinberg Stages IB and IIB), and THA was the preferred treatment option for postcollapse lesions (Steinberg Stages IIIB, IVB, V, and VI). Although the present study, which was based on NIS values, was able to assess trends in treatment options, it could not provide insight into each surgeon’s decision-making based on the stage of the disease. However, one may conclude that the most prevalent procedure, overall, for the treatment of osteonecrosis of the femoral head between 1992 and 2008 was THA and that the most prevalent joint-sparing procedure was core decompression. It is possible that this reported effect may have been the result of the complexity of the alternative joint-sparing procedures (grafting or osteotomy procedures) coupled with improved outcomes of primary THA in patients who have osteonecrosis.
Regardless of the type of surgery, either joint-preserving or joint-replacing, the trends reported in this study indicate an overall increase in the number of procedures performed for osteonecrosis of the femoral head. This may reflect an improved awareness of this disease, more aggressive approaches to diagnosis and treatment (including more frequent use of THA), improved access to health care, technological improvements, or improved treatment for early, precollapse lesions. This study provided insight into the preferred treatment options of the orthopaedic community, which is important to know, especially for conditions such as osteonecrosis that have numerous classification algorithms as well as a variety of treatment options, some of which may be technically challenging. Future studies are necessary to assess the current prevalence of the disease among the general population to better characterize these findings. It is important to recognize that this study was purely descriptive. As such, we do not recommend that all patients who have osteonecrosis be treated with THA; individualized approaches to treatment, based on age, stage of disease, and surgeon experience, are most appropriate as are continuing research into new biological and mechanical joint-preserving technologies that may provide additional conservative treatment options to the patient who has osteonecrosis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Acurio MT, Friedman RJ. Hip arthroplasty in patients with sickle-cell haemoglobinopathy. J Bone Joint Surg Br. 1992;74:367–371. doi: 10.1302/0301-620X.74B3.1587879. [DOI] [PubMed] [Google Scholar]
- 2.Adili A, Trousdale RT. Femoral head resurfacing for the treatment of osteonecrosis in the young patient. Clin Orthop Relat Res. 2003;417:93–101. doi: 10.1097/01.blo.0000096815.78689.3e. [DOI] [PubMed] [Google Scholar]
- 3.Agency for Healthcare Research and Quality. Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2010. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/NISIntroduction2010.pdf. Accessed January 1, 2013.
- 4.Al-Mousawi F, Malki A, Al-Aradi A, Al-Bagali M, Al-Sadadi A, Booz MM. Total hip replacement in sickle cell disease. Int Orthop. 2002;26:157–161. doi: 10.1007/s00264-002-0337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alves EM, Angrisani AT, Santiago MB. The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: a systematic review. Clin Rheumatol. 2009;28:1247–1251. doi: 10.1007/s10067-009-1231-y. [DOI] [PubMed] [Google Scholar]
- 6.Bassett CA, Schink-Ascani M, Lewis SM. Effects of pulsed electromagnetic fields on Steinberg ratings of femoral head osteonecrosis. Clin Orthop Relat Res. 1989;246:172–185. [PubMed] [Google Scholar]
- 7.Beaule PE, Amstutz HC, Le Duff M, Dorey F. Surface arthroplasty for osteonecrosis of the hip: hemiresurfacing versus metal-on-metal hybrid resurfacing. J Arthroplasty. 2004;19(Suppl 3):54–58. doi: 10.1016/j.arth.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Beaule PE, Schmalzried TP, Campbell P, Dorey F, Amstutz HC. Duration of symptoms and outcome of hemiresurfacing for hip osteonecrosis. Clin Orthop Relat Res. 2001;385:104–117. doi: 10.1097/00003086-200104000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Berend KR, Gunneson E, Urbaniak JR, Vail TP. Hip arthroplasty after failed free vascularized fibular grafting for osteonecrosis in young patients. J Arthroplasty. 2003;18:411–419. doi: 10.1016/S0883-5403(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 10.Chen CH, Chang JK, Huang KY, Hung SH, Lin GT, Lin SY. Core decompression for osteonecrosis of the femoral head at pre-collapse stage. Kaohsiung J Med Sci. 2000;16:76–82. [PubMed] [Google Scholar]
- 11.Chen YW, Chang JK, Huang KY, Lin GT, Lin SY, Huang CY. Hip arthroplasty for osteonecrosis in patients with systemic lupus erythematosus. Kaohsiung J Med Sci. 1999;15:697–703. [PubMed] [Google Scholar]
- 12.Clarke HJ, Jinnah RH, Brooker AF, Michaelson JD. Total replacement of the hip for avascular necrosis in sickle cell disease. J Bone Joint Surg Br. 1989;71:465–470. doi: 10.1302/0301-620X.71B3.2722941. [DOI] [PubMed] [Google Scholar]
- 13.Cuckler JM, Moore KD, Estrada L. Outcome of hemiresurfacing in osteonecrosis of the femoral head. Clin Orthop Relat Res. 2004;429:146–150. doi: 10.1097/01.blo.0000150121.88033.50. [DOI] [PubMed] [Google Scholar]
- 14.D’Antonio JA, Capello WN, Manley MT, Feinberg J. Hydroxyapatite coated implants. Total hip arthroplasty in the young patient and patients with avascular necrosis. Clin Orthop Relat Res. 1997;344:124–138. doi: 10.1097/00003086-199711000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Delank KS, Drees P, Eckardt A, Heine J. [Results of the uncemented total hip arthroplasty in avascular necrosis of the femoral head] [in German] Z Orthop Ihre Grenzgeb. 2001;139:525–530. doi: 10.1055/s-2001-19235. [DOI] [PubMed] [Google Scholar]
- 16.Disch AC, Matziolis G, Perka C. The management of necrosis-associated and idiopathic bone-marrow oedema of the proximal femur by intravenous iloprost. J Bone Joint Surg Br. 2005;87:560–564. doi: 10.1302/0301-620X.87B4.15658. [DOI] [PubMed] [Google Scholar]
- 17.Eftekhar NS, Schink-Ascani MM, Mitchell SN, Bassett CA. Osteonecrosis of the femoral head treated by pulsed electromagnetic fields (PEMFs): a preliminary report. Hip. 1983:306–330. [PubMed]
- 18.Ficat C. [Value of the functional investigation of the bone: intramedullary pressure measurement, trans-osseus phlebography and needle biopsy] [in French] Acta Orthop Belg. 1999;65(Suppl 1):35–44. [PubMed] [Google Scholar]
- 19.Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 20.Fyda TM, Callaghan JJ, Olejniczak J, Johnston RC. Minimum ten-year follow-up of cemented total hip replacement in patients with osteonecrosis of the femoral head. Iowa Orthop J. 2002;22:8–19. [PMC free article] [PubMed] [Google Scholar]
- 21.Fye MA, Huo MH, Zatorski LE, Keggi KJ. Total hip arthroplasty performed without cement in patients with femoral head osteonecrosis who are less than 50 years old. J Arthroplasty. 1998;13:876–881. doi: 10.1016/S0883-5403(98)90193-0. [DOI] [PubMed] [Google Scholar]
- 22.Garino JP, Steinberg ME. Total hip arthroplasty in patients with avascular necrosis of the femoral head: a 2- to 10-year follow-up. Clin Orthop Relat Res. 1997;334:108–115. doi: 10.1097/00003086-199701000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Glueck CJ, Freiberg RA, Fontaine RN, Sieve-Smith L, Wang P. Anticoagulant therapy for osteonecrosis associated with heritable hypofibrinolysis and thrombophilia. Expert Opin Investig Drugs. 2001;10:1309–1316. doi: 10.1517/13543784.10.7.1309. [DOI] [PubMed] [Google Scholar]
- 24.Glueck CJ, Freiberg RA, Fontaine RN, Tracy T, Wang P. Hypofibrinolysis, thrombophilia, osteonecrosis. Clin Orthop Relat Res. 2001;386:19–33. doi: 10.1097/00003086-200105000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Gonzalez MH, Ortinau ET, Buonanno W, Prieto J. Cementless total hip arthroplasty in patients with advanced avascular necrosis. J South Orthop Assoc. 1997;6:162–168. [PubMed] [Google Scholar]
- 26.Haenisch H. [Arthritis of the hip] [in German] Zentralblatt. 1925;52:1. [Google Scholar]
- 27.Hanker GJ, Amstutz HC. Osteonecrosis of the hip in the sickle-cell diseases. Treatment and complications. J Bone Joint Surg Am. 1988;70:499–506. [PubMed] [Google Scholar]
- 28.Hartley WT, McAuley JP, Culpepper WJ, Engh CA, Jr, Engh CA., Sr Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. J Bone Joint Surg Am. 2000;82:1408–1413. doi: 10.2106/00004623-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Hickman JM, Lachiewicz PF. Results and complications of total hip arthroplasties in patients with sickle-cell hemoglobinopathies. Role of cementless components. J Arthroplasty. 1997;12:420–425. doi: 10.1016/S0883-5403(97)90198-4. [DOI] [PubMed] [Google Scholar]
- 30.Hungerford MW, Mont MA, Scott R, Fiore C, Hungerford DS, Krackow KA. Surface replacement hemiarthroplasty for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 1998;80:1656–1664. doi: 10.2106/00004623-199811000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Ikemura S, Yamamoto T, Jingushi S, Nakashima Y, Mawatari T, Iwamoto Y. Use of a screw and plate system for a transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. J Orthop Sci. 2007;12:260–264. doi: 10.1007/s00776-007-1123-4. [DOI] [PubMed] [Google Scholar]
- 32.James D, Young A, Kulinskaya E, Knight E, Thompson W, Ollier W, Dixey J, Early Rheumatoid Arthritis Study Group UK. Orthopaedic intervention in early rheumatoid arthritis. Occurrence and predictive factors in an inception cohort of 1064 patients followed for 5 years. Rheumatology (Oxford). 2004;43:369–376. [DOI] [PubMed]
- 33.Kantor SG, Huo MH, Huk OL, Salvati EA. Cemented total hip arthroplasty in patients with osteonecrosis. A 6-year minimum follow-up study of second-generation cement techniques. J Arthroplasty. 1996;11:267–271. doi: 10.1016/S0883-5403(96)80076-3. [DOI] [PubMed] [Google Scholar]
- 34.Kerboul M, Thomine J, Postel M, Merle d’Aubigne R. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56:291–296. [PubMed] [Google Scholar]
- 35.Kim SY, Kim DH, Park IH, Park BC, Kim PT, Ihn JC. Multiple drilling compared with standard core decompression for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Br. 2004;86(Suppl):1. [Google Scholar]
- 36.Kim TH, Hong JM, Oh B, Cho YS, Lee JY, Kim HL, Shin ES, Lee JE, Park EK, Kim SY. Genetic association study of polymorphisms in the catalase gene with the risk of osteonecrosis of the femoral head in the Korean population. Osteoarthritis Cartilage. 2008;16:1060–1066. doi: 10.1016/j.joca.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Kim YH, Oh JH, Oh SH. Cementless total hip arthroplasty in patients with osteonecrosis of the femoral head. Clin Orthop Relat Res. 1995;320:73–84. [PubMed] [Google Scholar]
- 38.Kim YH, Oh SH, Kim JS, Koo KH. Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:675–681. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 39.Krackow KA, Mont MA, Maar DC. Limited femoral endoprosthesis for avascular necrosis of the femoral head. Orthop Rev. 1993;22:457–463. [PubMed] [Google Scholar]
- 40.Kurtz S, Mowat F, Ong K, Chang N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 41.Lieberman JR, Fuchs MD, Haas SB, Garvin KL, Goldstock L, Gupta R, Pellicci PM, Salvati EA. Hip arthroplasty in patients with chronic renal failure. J Arthroplasty. 1995;10:191–195. doi: 10.1016/S0883-5403(05)80126-3. [DOI] [PubMed] [Google Scholar]
- 42.Lins RE, Barnes BC, Callaghan JJ, Mair SD, McCollum DE. Evaluation of uncemented total hip arthroplasty in patients with avascular necrosis of the femoral head. Clin Orthop Relat Res. 1993;297:168–173. [PubMed] [Google Scholar]
- 43.Ludwig J, Lauber S, Lauber HJ, Dreisilker U, Raedel R, Hotzinger H. High-energy shock wave treatment of femoral head necrosis in adults. Clin Orthop Relat Res. 2001;387:119–126. doi: 10.1097/00003086-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 44.McGrory BJ, York SC, Iorio R, Macaulay W, Pelker RR, Parsley BS, Teeny SM. Current practices of AAHKS members in the treatment of adult osteonecrosis of the femoral head. J Bone Joint Surg Am. 2007;89:1194–1204. doi: 10.2106/JBJS.F.00302. [DOI] [PubMed] [Google Scholar]
- 45.Miller KD, Masur H, Jones EC, Joe GO, Rick ME, Kelly GG, Mican JM, Liu S, Gerber LH, Blackwelder WC, Falloon J, Davey RT, Polis MA, Walker RE, Lane HC, Kovacs JA. High prevalence of osteonecrosis of the femoral head in HIV-infected adults. Ann Intern Med. 2002;137:17–25. doi: 10.7326/0003-4819-137-1-200207020-00008. [DOI] [PubMed] [Google Scholar]
- 46.Min BW, Song KS, Cho CH, Lee SM, Lee KJ. Untreated asymptomatic hips in patients with osteonecrosis of the femoral head. Clin Orthop Relat Res. 2008;466:1087–1092. doi: 10.1007/s11999-008-0191-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459–474. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 48.Moran MC, Huo MH, Garvin KL, Pellicci PM, Salvati EA. Total hip arthroplasty in sickle cell hemoglobinopathy. Clin Orthop Relat Res. 1993;294:140–148. [PubMed] [Google Scholar]
- 49.Murzic WJ, McCollum DE. Hip arthroplasty for osteonecrosis after renal transplantation. Clin Orthop Relat Res. 1994;299:212–219. [PubMed] [Google Scholar]
- 50.Musso ES, Mitchell SN, Schink-Ascani M, Bassett CA. Results of conservative management of osteonecrosis of the femoral head. A retrospective review. Clin Orthop Relat Res. 1986;207:209–215. [PubMed] [Google Scholar]
- 51.Nam KW, Kim YL, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Fate of untreated asymptomatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 2008;90:477–484. doi: 10.2106/JBJS.F.01582. [DOI] [PubMed] [Google Scholar]
- 52.Neumayr LD, Aguilar C, Earles AN, Jergesen HE, Haberkern CM, Kammen BF, Nancarrow PA, Padua E, Milet M, Stulberg BN, Williams RA, Orringer EP, Graber N, Robertson SM, Vichinsky EP. Physical therapy alone compared with core decompression and physical therapy for femoral head osteonecrosis in sickle cell disease. Results of a multicenter study at a mean of three years after treatment. J Bone Joint Surg Am. 2006;88:2573–2582. doi: 10.2106/JBJS.E.01454. [DOI] [PubMed] [Google Scholar]
- 53.Onodera S, Majima T, Abe Y, Ito H, Matsuno T, Minami A. Transtrochanteric rotational osteotomy for osteonecrosis of the femoral head: relation between radiographic features and secondary collapse. J Orthop Sci. 2005;10:367–373. doi: 10.1007/s00776-005-0906-8. [DOI] [PubMed] [Google Scholar]
- 54.Ortiguera CJ, Pulliam IT, Cabanela ME. Total hip arthroplasty for osteonecrosis: matched-pair analysis of 188 hips with long-term follow-up. J Arthroplasty. 1999;14:21–28. doi: 10.1016/S0883-5403(99)90197-3. [DOI] [PubMed] [Google Scholar]
- 55.Phillips FM, Pottenger LA, Finn HA, Vandermolen J. Cementless total hip arthroplasty in patients with steroid-induced avascular necrosis of the hip. A 62-month follow-up study. Clin Orthop Relat Res. 1994;303:147–154. [PubMed] [Google Scholar]
- 56.Piston RW, Engh CA, De Carvalho PI, Suthers K. Osteonecrosis of the femoral head treated with total hip arthroplasty without cement. J Bone Joint Surg Am. 1994;76:202–214. doi: 10.2106/00004623-199402000-00006. [DOI] [PubMed] [Google Scholar]
- 57.Rijnen WH, Gardeniers JW, Westrek BL, Buma P, Schreurs BW. Sugioka’s osteotomy for femoral-head necrosis in young Caucasians. Int Orthop. 2005;29:140–144. doi: 10.1007/s00264-005-0639-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roudiere L, Viard JP. Osteonecrosis of the hip, lipodystrophy and antiretroviral treatment. AIDS. 2000;14:2056. doi: 10.1097/00002030-200009080-00026. [DOI] [PubMed] [Google Scholar]
- 59.Saito S, Ohzono K, Ono K. Joint-preserving operations for idiopathic avascular necrosis of the femoral head. Results of core decompression, grafting and osteotomy. J Bone Joint Surg Br. 1988;70:78–84. doi: 10.1302/0301-620X.70B1.3276703. [DOI] [PubMed] [Google Scholar]
- 60.Saito S, Saito M, Nishina T, Ohzono K, Ono K. Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop Relat Res. 1989;244:198–207. [PubMed] [Google Scholar]
- 61.Schneider W, Knahr K. Total hip replacement in younger patients: survival rate after avascular necrosis of the femoral head. Acta Orthop Scand. 2004;75:142–146. doi: 10.1080/00016470412331294385. [DOI] [PubMed] [Google Scholar]
- 62.Scott RD, Urse JS, Schmidt R, Bierbaum BE. Use of TARA hemiarthroplasty in advanced osteonecrosis. J Arthroplasty. 1987;2:225–232. doi: 10.1016/S0883-5403(87)80042-6. [DOI] [PubMed] [Google Scholar]
- 63.Siguier T, Siguier M, Judet T, Charnley G, Brumpt B. Partial resurfacing arthroplasty of the femoral head in avascular necrosis. Methods, indications, and results. Clin Orthop Relat Res. 2001;386:85–92. doi: 10.1097/00003086-200105000-00011. [DOI] [PubMed] [Google Scholar]
- 64.Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77:34–41. [PubMed] [Google Scholar]
- 65.Stulberg BN, Singer R, Goldner J, Stulberg J. Uncemented total hip arthroplasty in osteonecrosis: a 2- to 10-year evaluation. Clin Orthop Relat Res. 1997;334:116–123. doi: 10.1097/00003086-199701000-00015. [DOI] [PubMed] [Google Scholar]
- 66.Sugioka Y, Yamamoto T. Transtrochanteric posterior rotational osteotomy for osteonecrosis. Clin Orthop Relat Res. 2008;466:1104–1109. doi: 10.1007/s11999-008-0192-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Taylor AH, Shannon M, Whitehouse SL, Lee MB, Learmonth ID. Harris Galante cementless acetabular replacement in avascular necrosis. J Bone Joint Surg Br. 2001;83:177–182. doi: 10.1302/0301-620X.83B2.11419. [DOI] [PubMed] [Google Scholar]
- 68.Wang BL, Sun W, Shi ZC, Zhang NF, Yue DB, Guo WS, Shi SH, Li ZR. Treatment of nontraumatic osteonecrosis of the femoral head using bone impaction grafting through a femoral neck window. Int Orthop. 2010;34:635–639. doi: 10.1007/s00264-009-0822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wei SY, Klimkiewicz JJ, Lai M, Garino JP, Steinberg ME. Revision total hip arthroplasty in patients with avascular necrosis. Orthopedics. 1999;22:747–757. doi: 10.3928/0147-7447-19990801-06. [DOI] [PubMed] [Google Scholar]
- 70.Xenakis TA, Beris AE, Malizos KK, Koukoubis T, Gelalis J, Soucacos PN. Total hip arthroplasty for avascular necrosis and degenerative osteoarthritis of the hip. Clin Orthop Relat Res. 1997;341:62–68. doi: 10.1097/00003086-199708000-00011. [DOI] [PubMed] [Google Scholar]
- 71.Xenakis TA, Gelalis J, Koukoubis TA, Zaharis KC, Soucacos PN. Cementless hip arthroplasty in the treatment of patients with femoral head necrosis. Clin Orthop Relat Res. 2001;386:93–99. doi: 10.1097/00003086-200105000-00012. [DOI] [PubMed] [Google Scholar]
- 72.Zangger P, Gladman DD, Urowitz MB, Bogoch ER. Outcome of total hip replacement for avascular necrosis in systemic lupus erythematosus. J Rheumatol. 2000;27:919–923. [PubMed] [Google Scholar]