Abstract
Background
Surgeons have several implant choices when managing Vancouver B2 and B3 periprosthetic fractures about the hip. Few long-term studies have reported outcomes for tapered fluted titanium stems.
Questions/purposes
We determined (1) survival, with femoral revision as the end point, of distal taper stems in the treatment of Vancouver B2 and B3 periprosthetic fractures at our institution, (2) radiographic outcomes, and (3) quality of life and hip function after revision.
Methods
Of the 200 patients with Vancouver B2 or B3 periprosthetic fractures treated with femoral revision between February 2000 and February 2010, 55 (38 B2, 17 B3) were treated with modular tapered titanium stems. Of the surviving 47 patients, one was lost to followup, leaving 46 (30 B2, 16 B3) available for review at a mean of 54 months (range, 24–143 months). Initial indications for using these implants were treatment of periprosthetic fractures where less than 4 cm of diaphyseal fit was available, but this evolved during the study period to all fractures unless no diaphysis remained, in which case complex revision techniques were used. Radiographs were assessed to establish fracture healing, stem subsidence, and bone stock restoration. Quality of life and hip function were assessed using WOMAC, Oxford, SF-12, UCLA activity level, and satisfaction scores.
Results
Two femoral stems were revised: one subsided and was revised at 12 months; the other had deep infection and underwent two-stage revision at 49 months. Radiographic review showed one nonunion, with maintenance or improvement of bone stock in 89% of patients. Subsidence occurred in 24%. Mean Oxford score was 76 of 100, WOMAC function and pain scores were 75 and 82 of 100, satisfaction score was 91 of 100, and SF-12 mental and physical scores were 53 and 40 of 100.
Conclusions
We report encouraging short-term results in terms of survival of distal taper stems in the treatment of B2 and B3 periprosthetic fractures. Although subsidence was frequent, most migrated less than 3 mm without correlation to poor pain and functional scores.
Level of Evidence
Level IV, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
The number of THA procedures continues to increase worldwide. The combination of broadening indications, greater functional expectations, and an aging population is likely to lead to increased prevalence of periprosthetic fractures [7]. Registry data indicate that periprosthetic fractures cause between 9.3% and 14.7% of THA revisions [2, 17, 19].
Fractures can be reliably classified according to the Vancouver classification [9] and this can assist in the decision-making process. Based on this classification, the treating surgeon has several options based on fracture location, implant stability, and bone stock and strength available to support a new implant. Vancouver Type B fractures are nonapophyseal (not the lesser or greater trochanter alone) but affect the femur around or just beside the stem. If the stem is solidly fixed, it is subcategorized as a B1. Fracture reduction and fixation are indicated. If the stem is loose with good remaining bone stock, it is subcategorized as B2. Fracture reduction and fixation, coupled with longer-stem revision, is usually preferred. Finally, if in addition to a loose stem there is inadequate bone to support a straightforward revision (such as severe comminution, osteolysis, or severe osteopenia), this is subclassified as B3. More complex reconstruction is usually used.
Revision THA with distally tapered fluted titanium cementless stems was originally described by Wagner in the 1980s [29, 30]. Axial stability of the implant is achieved by driving the tapered region of the stem into the femoral diaphysis that has been prepared using conical reamers. Longitudinal spines provide rotational stability. The original designs were monoblock in design except for head-neck modularity. The subsequent addition of stem modularity to a number of systems added to the versatility of the implant and to its broad application in revision hip arthroplasty and periprosthetic fracture management. This method of reconstruction has been successfully utilized in femoral revision after aseptic loosening [11, 12, 15, 21, 23–25, 28, 32]. Short-term survival of greater than 87% and good functional scores have been described for femoral revision with these stems in the presence of severe bone deficiency [26, 28]. In light of this, modular tapered stems also have become an attractive option in the treatment of Vancouver B2 and B3 fractures.
In this study, we determined (1) the survival, with femoral revision as the end point, of distal taper stems in the treatment of Vancouver B2 and B3 periprosthetic fractures at our institution, (2) the radiographic outcome in patients with these fractures treated with this stem, and (3) the quality of life and hip function after revisions performed for this indication with this implant.
Patients and Methods
Between February 2000 and February 2010, we performed 200 femoral revisions for periprosthetic fractures in patients with Vancouver Type B2 and B3 fractures. This included 34 proximal femoral replacements performed for severe bone loss and a nonsupportive diaphysis. We identified 55 patients treated with one of two tapered modular fluted titanium stems. The ZMR® (Zimmer, Inc, Warsaw, IN, USA) has a 3.5° distal taper while the Revitan® (Zimmer, Inc) has a 2° distal taper (Fig. 1). No patient treated with a tapered stem was excluded. Of the 55, 38 had a B2 fracture and 17 had a B3 fracture. Eight patients died at a mean of 23 months after surgery (range, 6 days to 42 months). None of the femoral stems were revised in this group. Of the surviving 47 patients, one who had moved overseas was lost to followup, leaving 46 patients with 30 B2 and 16 B3 fractures for review. All previous radiographs were obtained and hospital notes reviewed for surgical data and complications. Minimum followup for surviving patients was 24 months (mean, 54 months; range, 24–143 months). Average age was 72 years (range, 44–93 years) at surgery and 76 years (range, 47–96 years) at followup.
Fig. 1A–C.

Photographs show the ZMR® and Revitan® stems: (A) ZMR® stem with a 3.5° taper and (B, C) two sizes of the Revitan® stem and modular bodies with a 2° stem taper.
The general indications for use of tapered stems evolved during the study period. In the earlier period, they were reserved for Type B3 fractures with less than 4 cm of diaphyseal fit and therefore insufficient for a cylindrical fully porous cobalt-chromium stem, our commonly used revision stem at the time. After concerns about stress shielding with cylindrical stems and positive results with tapered stems, they became our stem of choice for all B2 and B3 fractures. The Revitan® stem with a 2° taper was used in smaller patients with B2 fractures as it required less bone resection than the ZMR® system.
Surgery was performed through a posterior extensile approach, using the transfemoral modification to facilitate removal of the loose stem and cement. All cases underwent preoperative templating. Stem length was planned to obtain 4 to 8 cm of distal fit with an estimate of diameter required. A prophylactic wire or cable was routinely used at the level of intact diaphyseal bone. Preparation of the femur was conducted with hand reamers to the pretemplated depth with increasing diameter until axial and coronal/sagittal stability of the reamer were established. Trial stems were used to check stability and trial bodies suitable restoration of length and offset. We initially used onlay allograft to support the proximal implant whenever bone was weakened or contained defects were present but currently only use this when proximal bone is absent, usually the medial calcar. The fracture occurred after primary arthroplasty (including one hemiarthroplasty) in 47 patients and after revision THA in eight. Thirty were cemented stems and 25 cementless stems. The existing stem was removed using the fracture as an extended osteotomy. Cortical onlay allografts were used in 14 of the B3 fractures to support the proximal implant. Fracture fragments were reduced around the proximal stem and secured with Luque wires in 15 patients, cerclage cables in 38, and heavy suture in two. In four patients, a claw plate with cables was used to secure the greater trochanter. Patients were managed with partial weightbearing for 6 weeks if stem fixation was judged to be secure and toe-touch weightbearing for 6 weeks followed by partial weightbearing (50%) for 6 weeks if there was any doubt.
Radiographs that included the full length of the femoral component in AP and lateral plain views were obtained along with the original films of the fracture and postoperative views. Subsidence was measured as movement relative to anatomic landmarks and checked against wires or cables. The known size of the femoral head was used to confirm scale. Subsidence was classified into three groups: up to 3 mm, 3 to 10 mm, and greater than 10 mm. Measurements on plain radiographs have a reported error of up of 1 to 5 mm but acceptable intra- and interobserver error of greater than 0.8 [5, 14]. Changes in femoral bone stock were classified according to the system of Böhm and Bischel [6]: A (increasing defects), B (constant defects), or C (osseous restoration). Osseous restoration is calculated by comparing immediate postoperative radiographs to the latest followup images. A comparison of cortical thickness to bone diameter establishes a ratio, and if increasing, is defined as osseous restoration. Femoral union was defined as bone bridging across the fracture site on three of four cortices [18, 22]. Complete sets of radiographs were available for 38 patients, including 24 B2 fractures and 14 B3 fractures. This included three of the deceased patients who survived longer than 24 months. The five other deceased patients did not have sufficient followup. Twelve other patients were missing films for comparison or lived in geographically remote locations and did not wish to or were unable to attend for new imaging.
To assess patient quality of life and hip function, the 47 surviving patients were invited by mail to complete a standardized self-administered questionnaire incorporating the Oxford Hip Score [8], the WOMAC Osteoarthritis Index [3], the SF-12 [31], the Hip and Knee Arthroplasty Satisfaction questionnaire [13], and the UCLA activity score [1]. When patients did not return questionnaires, they were contacted by telephone, asked to complete the assessment themselves, and then contacted again to report their answers. Of the surviving 47 patients, the two with failed tapered fluted stems were excluded from self-assessed evaluation. One patient was lost to followup. Four patients did not wish to participate. Four patients did not return the questionnaire despite repeated efforts to retrieve the information. Ten patients were unable to answer due to inability to comprehend the questionnaire, medical comorbidity, or a language barrier. We included three self-assessment scores from deceased patients with minimum 2-year followup. A total of 28 complete assessments (16 for B2 and 12 for B3) were available for evaluation.
Comparisons of quality of life and hip function between cohorts were assessed with two-sample t-tests using SAS® Version 9.3 (SAS Institute Inc, Cary, NC, USA).
Results
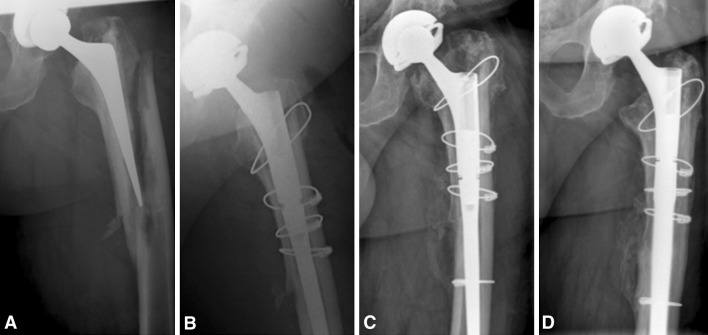
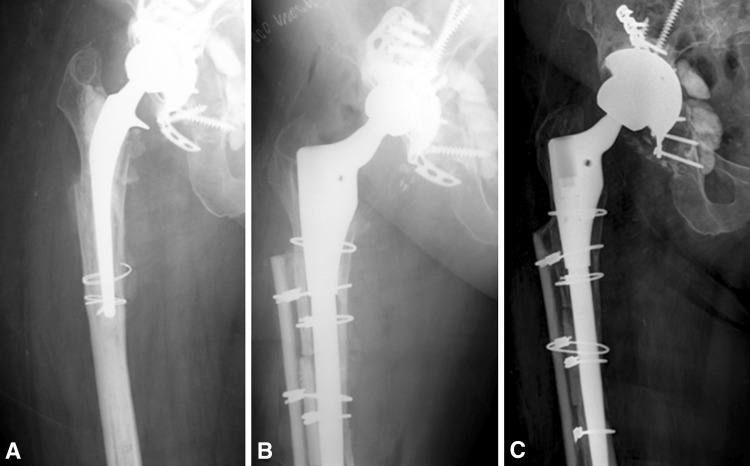
Two stem revisions were required (4%). One stem required revision for loosening. It was a Type B2 fracture in which the stem subsided more than 10 mm. Revision at 12 months to a stem that was 6 mm larger in diameter led to an excellent outcome (Fig. 2). The fracture was found to be united at revision. A second stem required revision at 49 months for the two-stage management of a late-onset bacteremic periprosthetic infection due to Streptococcus oralis. The initially inserted tapered fluted titanium stem was solidly fixed. One asymptomatic fracture nonunion was identified. However, the femur was in continuity. This occurred in a 63-year-old woman with a B3 fracture around a primary cemented stem. At 8-year followup, her allograft strut had bonded proximally and distally (Fig. 3).
Fig. 2A–D.
Images illustrate revision of a Type B2 fracture using a 14-mm-diameter tapered fluted modular titanium stem. (A) A preoperative radiograph shows a fracture around a loose cemented stem. (B) An initial postoperative view shows position of the tapered stem. (C) The undersized stem has clearly subsided. (D) The patient was revised to a 20-mm stem and had excellent results at 12 months. A constrained liner had been used because of severe abductor deficiency and high risk of dislocation.
Fig. 3A–C.
Images illustrate revision of a Type B3 fracture with an allograft strut in a 63-year-old woman. (A) An AP radiograph of the femur demonstrates a fracture around a cemented stem with an extensive cement mantle. After removal of the cement, there was severe bone loss. (B) An immediate postoperative view shows the tapered stem with allograft to restore lateral bone stock. (C) Eight years later, the fracture has not united, but the onlay allograft has united to the femur. There is obvious bone loss (Type A) around the proximal implant. Her cup acetabular cage construct was revised for loosening and pelvic discontinuity by plating the posterior column and using an enhanced fixation surface cup.
Subsidence was noted in nine of 38 patients (24%). This was less than 3 mm in five patients, 3 to 10 mm in two, and greater than 10 mm in two, including the stem that failed (Fig. 2). Subsidence occurred in six B2 fractures (25%) and three B3 fractures (21%). Bone stock was classified as Type A (diminished) in 11% (Fig. 3), Type B (unchanged) in 63%, and Type C (increased) in 26% (Fig. 4). Eleven of 14 allografts were imaged and eight were radiographically incorporated (Fig. 4).
Fig. 4A–C.
Images illustrate revision of a Type B3 fracture in an 83-year-old woman. (A) An AP radiograph of the femur demonstrates a fracture with osteolysis of the proximal femur. (B) An initial postoperative view shows allograft postioned medially with thinning of the cortical bone. (C) Followup at 34 months shows recovery of proximal bone and incorporation of the allograft strut. Despite the subsidence of the stem, the patient was asymptomatic.
Self-assessed pain and function scores were generally good (Table 1). There was no significant difference in outcome scores when comparing the B2 and B3 fractures. With the low numbers available, subsidence was not associated with a difference in WOMAC pain (p = 0.745) or functional scores (p = 0.962). As patients presented immediately after a fracture, preoperative pain and functional scores could not be obtained.
Table 1.
Quality-of-life and hip function scores for Vancouver B2 and B3 fractures
| Scoring system | B2 fractures (n = 16) | B3 fractures (n = 12) | p value |
|---|---|---|---|
| Mean patient age (years) | 73 | 71 | 0.501 |
| Mean WOMAC global score (points)* | 76 | 77 | 0.822 |
| Mean WOMAC function score (points)* | 75 | 75 | 0.989 |
| Mean WOMAC stiffness score (points)* | 70 | 76 | 0.496 |
| Mean WOMAC pain score (points)* | 80 | 85 | 0.499 |
| Mean Oxford Hip Score (points)* | 74 | 77 | 0.637 |
| Mean satisfaction score overall (points)† | 96 | 94 | 0.781 |
| Mean satisfaction score pain (points)† | 98 | 92 | 0.341 |
| Mean satisfaction score function (points)† | 90 | 90 | 0.856 |
| Mean satisfaction score recreation (points)† | 86 | 80 | 0.542 |
| Mean UCLA activity score (points)‡ | 4 | 5 | 0.404 |
| Mean SF-12 physical summary score (points) | 41 | 38 | 0.802 |
| Mean SF-12 mental summary score (points) | 53 | 54 | 0.803 |
* WOMAC and Oxford Hip Scores are normalized to a range of 0 to 100 points, with 0 being worst and 100 being best; †satisfaction scores range from 0 to 100 points; ‡a UCLA activity score of 4 correlates to regular participation in mild activities and a UCLA score of 5 to sometimes participates in moderate activities.
Eight reoperations were required in the 54 patients not lost to followup, in addition to the two requiring stem exchange. Three patients had dislocations, including one of those who was deceased. One patient with a 36-mm head underwent closed reduction after a single dislocation in the early postoperative period. It did not recur. The other two, both with 40-mm heads, required revision of the acetabular component and head. None of the stems had subsided and all were noted to be well fixed at the time of rerevision. Two patients sustained supracondylar femur fractures (Vancouver Type C) after falls 12 and 14 months after revision. In both patients, the fractures were well distal to the implants and were treated with reduction and internal fixation. One patient with an acetabular reconstruction cage construct for pelvic dissociation required revision of the acetabular component after cage failure (Fig. 3). The stem was stable. One aseptic superficial hematoma was washed out, and one patient had late removal of a claw plate because of soft tissue irritation.
Discussion
Surgeons have several implant choices when managing Vancouver B2 and B3 periprosthetic fractures about the hip. We reviewed our results to determine (1) the survival of distal tapered fluted modular titanium stems in the treatment of Vancouver B2 and B3 periprosthetic fractures, using femoral revision as the end point, (2) the radiographic outcome, and (3) the quality of life and hip function after revision.
We note several limitations of the study. The study is retrospective and has no control group. The use of standardized outcome measures does allow us to compare this cohort with similar groups undergoing revision for different reasons or with different implants. Additionally, our stem selection evolved during the study period. Initially, we reserved tapered stems for Type B3 fractures but currently use them for the majority of B2 and B3 fractures that require revision. This should however mean that we have captured those patients with more severe bone loss and only one B3 fracture was lost. Unfortunately, several patients were medically unwell and unable to complete questionnaires. While this was not necessarily due to their hips, the results are biased toward those patients doing well. In this series, we had complete data (radiographic and quality-of-life assessment) on only 51% of patients treated. Thus, the results must be regarded as the best-case scenario as patients with incomplete followup are more likely to have inferior scores. We did obtain self-assessed quality-of-life data for 12 of 16 potentially assessable B3 fractures, a group we would expect to have more subsidence and poorer functional outcomes. Finally, reports of bone remodeling must be interpreted with caution. Plain radiographs can only detect reduction in bone stock when at least 30% of mineral density has been lost [10, 33].
We observed excellent short-term survival of tapered fluted titanium stems used in the management of B2 and selected B3 periprosthetic femoral fractures. This represents one of the largest reported series for tapered fluted titanium stems used for this indication. At a mean followup of 54 months, two (4%) femoral components had been revised. Only one femoral component failed for mechanical reasons. In this case, the stem (Fig. 2) was unable to resist axial load. This emphasizes the critical surgical step of reaming an adequate taper into the distal femur to receive an appropriately sized stem. Few studies have assessed survival of distally tapered stems used specifically in the management of periprosthetic fractures (Table 2). Mulay et al. [16] reviewed 10 B2 and 14 B3 fractures managed with a modular fluted tapered stem (Link® MP™ Hip Stem; Waldemar, Hamburg, Germany). The only revision was in a patient with deep infection treated with excision arthroplasty. Park et al. [22] observed similar performance with the same stem at mean followup of 58 months. Two stems in their series failed, one due to deep infection and one due to subsidence and loosening. Neumann et al. [18] recently reported survival of a modular tapered titanium stem used to treat 35 B2 and 20 B3 fractures (Modular Plus System®; Smith & Nephew, London, UK). Two stems failed due to uncontrolled subsidence. Of note, this system has a curved stem that requires a different approach when preparing the distal femur. A small series of eight B3 fractures was reported by Berry [4], with no failures at a short minimum followup of 12 months. Other management options have been assessed. Springer et al. [27] reported outcomes from the Mayo Clinic registry for 118 femoral revisions after periprosthetic fracture. Fully coated cylindrical stems had superior survival compared to partially coated prostheses and cemented stems. Kaplan-Meier analysis demonstrated 90% survival at 5 years, falling to 79% at 10 years. O’Shea et al. [20] assessed 22 B2 and B3 fractures managed with extensively coated stems. Two stems failed: one used in a B2 fracture subsided and did not stabilize and one used in a B3 fracture became infected. We have previously used these stems but have found the rate of subsidence unacceptable when less than 4 cm of bone is available distally.
Table 2.
Outcomes for Vancouver B2 and B3 periprosthetic fractures treated with tapered fluted stems reported in the literature
| Study | Number of patients | Followup (months)* | Number of B2/B3 fractures | Number of stems revised for any reason | Number of stems with deep infection | Union rate | Number of stems revised for loosening | Number of intraoperative fractures | Subsidence (mm) | Clinical outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Berry [4] (2003) | 8 (1 died) | 18 (12–24) | 0/8 | 0 | 0 | 100% healed by 12 months | 0 | 0 | 0 | 5 patients with no pain, 2 with mild pain 3 walking independently, 2 with cane, 2 with walker |
| Mulay et al. [16] (2005) | 24 (2 died) | NR | 10/14 | 0 | 1 | 91% healed by 12 months | 0 | 1 (anterior cortex femur) | 5 (2–10) in 17 patients | HHS (points)*: 69 (34–97) |
| Park et al. [22] (2009) | 27 | 58 (36–122) | 16/11 | 0 | 1 | 93% | 0 | 2 | > 5 in 1 stem > 10 in 1 stem |
HHS (points)*: 85 (64–94) |
| Neumann et al. [18] (2012) | 55 (2 died) | 67 (60–144) | 35/20 | 2 | 1 | 100% healed by 6 months | 2 | 0 | > 5 in 2 stems | HHS (points)*: 72 (45–97) |
| Current study | 55 (8 died) | 54 (24–143) | 38/17 | 2 | 1 | 98% healed by 24 months | 1 | 0 | < 3 in 5 stems 3–10 in 2 stems > 10 mm in 2 stems |
Oxford Hip Score (points)*: 76 WOMAC global score (points)*: 76 Satisfaction score (points)*: 95 |
* Values are expressed as mean, with range in parentheses; NR = not reported; HHS = Harris hip score.
Subsidence was observed in 24% of patients although the majority were less than 3 mm. Overall, only 9% subsided more than 3 mm and only one patient was symptomatic and required revision. We did not see any subsidence occurring beyond 12 months. Two stems subsided more than 10 mm, one of which failed. It must be noted that 31% of the cohort had incomplete radiographic followup; thus, the true rate is unknown. Similar rates of subsidence have been reported after revision for aseptic loosening [12, 21, 25]. Mulay et al. [16] reported mean subsidence of 5 mm (range, 2–10 mm) occurring in 17 of 24 patients. Several authors have reported favorable bone remodeling and osseous integration after revision with tapered titanium stems for aseptic loosening [15, 24, 25]. These results have been similar to our experience, with the majority of patients demonstrating stable bone or restoration of bone stock with increasing cortical volume and healing of defects [6, 25]. While plain radiographs are not the most accurate means of determining bone remodeling, we have not observed the marked proximal stress shielding seen with cylindrical cobalt-chromium stems [24, 26].
Pain and functional scores were acceptable for those assessed, especially as there were no differences in outcomes between B2 or B3 fractures. Richards et al. [24] performed a cross-sectional cohort study comparing 103 tapered fluted modular titanitum stems to 114 cylindrical nonmodular cobalt-chromium stems. The surgical indication was aseptic loosening in 78%, periprosthetic fracture in 10% and second-stage reconstruction after infection in 12%. Despite a larger number of patients with severe bone loss, both pain and functional scores were significantly higher for the tapered stems than for the cylindrical stems (Table 3). Van Houwelingen et al. [28] found similarly favorable scores when reviewing the longer-term followup of patients revised with tapered fluted modular titanitum stems with severe (Paprosky Type IIIB and IV) bone loss (Table 3) [26]. The same questionnaire was used in our study. Scores reported by our group of patients were closely aligned to scores reported in both studies.
Table 3.
Comparison of reported quality-of-life and hip function scores for TFMT stems in femoral revision
| Scoring system | Richards et al. [24] | Van Houwelingen et al. [28] | Current study | |
|---|---|---|---|---|
| TFMT stems | CNCC stems | |||
| Mean WOMAC global score (points)* | 77 | 76 | ||
| Mean WOMAC function score (points)* | 75 | 75 | ||
| Mean WOMAC stiffness score (points)* | 76 | 68 | 76 | 73 |
| Mean WOMAC pain score (points)* | 84 | 78 | 85 | 82 |
| Mean Oxford Hip Score (points)* | 77 | 69 | 77 | 76 |
| Mean satisfaction score overall (points)† | 97 | 90 | 94 | 95 |
| Mean satisfaction score pain (points)† | 92 | 95 | ||
| Mean satisfaction score function (points)† | 90 | 90 | ||
| Mean satisfaction score recreation (points)† | 80 | 83 | ||
| Mean UCLA activity score (points)‡ | 5.1 | 4.6 | 4.9 | 4.6 |
| Mean SF-12 physical summary score (points) | 39 | 38 | 38 | 40 |
| Mean SF-12 mental summary score (points) | 53 | 51 | 54 | 53 |
Note the comparison with CNCC stems from Richards et al. [24], which showed significant differences in patient quality-of-life scores when comparing the two stem types; * WOMAC and Oxford Hip Scores are normalized to a range of 0 to 100 points, with 0 being worst and 100 being best; †satisfaction scores range from 0 to 100; ‡ a UCLA activity score of 4 correlates to regular participation in mild activities and a UCLA score of 5 to sometimes participates in moderate activities; TFMT = tapered fluted modular titanium; CNCC = cylindrical nonmodular cobalt-chromium.
We believe the continued use of tapered fluted titanium stems in the treatment of Vancouver B2 and B3 fractures is justified, and further followup is needed to ensure that patients with asymptomatic subsidence do not become symptomatic.
Acknowledgments
We thank Eric Sayre PhD for his assistance with the statistical analysis and Daphné Savoy BA for her assistance in the preparation of the manuscript.
Footnotes
The institution of the authors has received, during the study period, funding from Zimmer, Inc (Warsaw, IN, USA), DePuy Synthes Canada Ltd (Markham, ON, Canada), Johnson & Johnson (Canada) Inc (Markham, ON, Canada), Stryker Canada (Hamilton, ON, Canada), and Bayer Inc (Toronto, ON, Canada). One or more of the authors certify that they have received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000, from Zimmer, Inc (JTM, DSG, BAM, CPD), and an amount of USD 10,000 to USD 100,000, from DePuy Synthes Canada Ltd (JTM, CPD).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 2.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2010. Adelaide, Australia: AOA; 2010.
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 4.Berry DJ. Treatment of Vancouver B3 periprosthetic femur fractures with a fluted tapered stem. Clin Orthop Relat Res. 2003;417:224–231. doi: 10.1097/01.blo.0000096821.67494.f6. [DOI] [PubMed] [Google Scholar]
- 5.Biedermann R, Krismer M, Stöckl B, Mayrhofer P, Ornstein E, Franzén H. Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement. Einzel-Bild-Röntgen-Analyse-femoral component analysis. J Bone Joint Surg Br. 1999;81:266–272. doi: 10.1302/0301-620X.81B2.8842. [DOI] [PubMed] [Google Scholar]
- 6.Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;83:1023–1031. doi: 10.1302/0301-620X.83B7.11413. [DOI] [PubMed] [Google Scholar]
- 7.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 8.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63–69. doi: 10.1302/0301-620X.80B1.7859. [DOI] [PubMed] [Google Scholar]
- 9.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 10.Engh CA, Jr, McAuley JP, Sychterz CJ, Sacco ME, Engh CA., Sr The accuracy and reproducibility of radiographic assessment of stress-shielding: a postmortem analysis. J Bone Joint Surg Am. 2000;82:1414–1420. doi: 10.2106/00004623-200010000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Garbuz DS, Toms A, Masri BA, Duncan CP. Improved outcome in femoral revision arthroplasty with tapered fluted modular titanium stems. Clin Orthop Relat Res. 2006;453:199–202. doi: 10.1097/01.blo.0000238875.86519.cf. [DOI] [PubMed] [Google Scholar]
- 12.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;18:94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 13.Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis. 2011;2011:591253. doi: 10.1155/2011/591253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malchau H, Kärrholm J, Wang YX, Herberts P. Accuracy of migration analysis in hip arthroplasty: digitized and conventional radiography, compared to radiostereometry in 51 patients. Acta Orthop Scand. 1995;66:418–424. doi: 10.3109/17453679508995578. [DOI] [PubMed] [Google Scholar]
- 15.McInnis DP, Horne G, Devane PA. Femoral revision with a fluted, tapered, modular stem seventy patients followed for a mean of 3.9 years. J Arthroplasty. 2006;21:372–380. doi: 10.1016/j.arth.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 16.Mulay S, Hassan T, Birtwistle S, Power R. Management of types B2 and B3 femoral periprosthetic fractures by a tapered, fluted, and distally fixed stem. J Arthroplasty. 2005;20:751–756. doi: 10.1016/j.arth.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 17.National Joint Registry for England and Wales. Available at: http://www.njrcentre.org.uk/njrcentre/ Reports,PublicationsandMinutes/Annualreports/tabid/86/Default.aspx. Accessed November 12, 2011.
- 18.Neumann D, Thaler C, Dorn U. Management of Vancouver B2 and B3 femoral periprosthetic fractures using a modular cementless stem without allografting. Int Orthop. 2012;36:1045–1050. doi: 10.1007/s00264-011-1371-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.New Zealand Joint Registry. Eleven Year Report. Christchurch, New Zealand: NZOA; 2010.
- 20.O’Shea K, Quinlan JF, Kutty S, Mulcahy D, Brady OH. The use of uncemented extensively porous-coated femoral components in the management of Vancouver B2 and B3 periprosthetic femoral fractures. J Bone Joint Surg Br. 2005;87:1617–1621. doi: 10.1302/0301-620X.87B12.16338. [DOI] [PubMed] [Google Scholar]
- 21.Ovesen O, Emmeluth C, Hofbauer C, Overgaard S. Revision total hip arthroplasty using a modular tapered stem with distal fixation: good short-term results in 125 revisions. J Arthroplasty. 2010;25:348–354. doi: 10.1016/j.arth.2008.11.106. [DOI] [PubMed] [Google Scholar]
- 22.Park MS, Lim YJ, Chung WC, Ham DH, Lee SH. Management of periprosthetic femur fractures treated with distal fixation using a modular femoral stem using an anterolateral approach. J Arthroplasty. 2009;24:1270–1276. doi: 10.1016/j.arth.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 23.Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty. 2007;22:993–999. doi: 10.1016/j.arth.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 24.Richards CJ, Duncan CP, Masri BA, Garbuz DS. Femoral revision hip arthroplasty: a comparison of two stem designs. Clin Orthop Relat Res. 2010;468:491–496. doi: 10.1007/s11999-009-1145-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez JA, Deshmukh AJ, Klauser WU, Rasquinha VJ, Lubinus P, Ranawat CS. Patterns of osseointegration and remodeling in femoral revision with bone loss using modular, tapered, fluted, titanium stems. J Arthroplasty. 2011;26:1409–1417. doi: 10.1016/j.arth.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 26.Sporer SM, Paprosky WG. Femoral fixation in the face of considerable bone loss: the use of modular stems. Clin Orthop Relat Res. 2004;429:227–231. doi: 10.1097/01.blo.0000150120.80409.0d. [DOI] [PubMed] [Google Scholar]
- 27.Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am. 2003;85:2156–2162. doi: 10.2106/00004623-200311000-00015. [DOI] [PubMed] [Google Scholar]
- 28.Van Houwelingen AP, Duncan CP, Masri BA, Greidanus NV, Garbuz DS. High survival of modular tapered stems for proximal femoral bone defects at 5 to 10 years followup. Clin Orthop Relat Res. 2013;471:454–462. doi: 10.1007/s11999-012-2552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wagner H. Revision prosthesis for the hip joint in severe bone loss. Orthopade. 1987;16:295–300. [PubMed] [Google Scholar]
- 30.Wagner H. A revision prosthesis for the hip joint. Orthopade. 1989;18:438–453. [PubMed] [Google Scholar]
- 31.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Weiss RJ, Beckman MO, Enocson A, Schmalholz A, Stark A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty. 2011;26:16–23. doi: 10.1016/j.arth.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 33.Wright JM, Pellicci PM, Salvati EA, Ghelman B, Roberts MM, Koh JL. Bone density adjacent to press-fit acetabular components: a prospective analysis with quantitative computed tomography. J Bone Joint Surg Am. 2001;83:529–536. doi: 10.1302/0301-620X.83B8.12390. [DOI] [PubMed] [Google Scholar]