Abstract
Background
Treatment of periprosthetic femur fractures is challenging, and high failure and complication rates have been reported in many series. The optimal techniques and implants for the management of Vancouver B2 and B3 fractures remain in debate.
Questions/purposes
The purpose of this study was to evaluate the results of a relatively new class of femoral implants, uncemented fluted, tapered, modular stems, to treat periprosthetic femur fractures; we specifically evaluated (1) fracture union; (2) implant stability; (3) patient outcomes; and (4) complications.
Methods
We retrospectively identified 44 Vancouver B2 (25 patients) and B3 (19 patients) periprosthetic femur fractures treated consecutively with fluted, tapered stems at a single institution from 2000 to 2006. The mean patient age was 72 years (range, 34–92 years), and 24 were women. The minimum followup was 2 years (mean, 4.5 years; range, 2–8 years).
Results
Forty-three of 44 (98%) fractures healed radiographically and 43 of 44 (98%) femoral components were stable radiographically at latest followup. The mean postoperative Harris hip score was 83. There were seven additional reoperations (five for recurrent instability, two for deep infections).
Conclusions
Modular fluted, tapered stems provide a reliable treatment method for Vancouver B2 and B3 periprosthetic femoral fractures with a high rate of fracture union and implant osteointegration. The most common complication, instability, may be reduced by more consistent use of larger femoral head diameters.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
By 2030, the demand for primary THA in the United States is expected to grow by 174% to 572,000 annual procedures [10]. Total hip revisions are also projected to grow by 137% from 2005 to 2030 [10]. Periprosthetic femur fractures are among the top five reasons for THA revision in reports from large US databases and the Australian National Joint Replacement Registry [1, 5]. The prevalence of postoperative periprosthetic femur fracture has been estimated to be as high as 1.5% to 4% [4].
The challenges in treating such fractures include the complexity of the fracture itself, poor bone stock, and altered femoral anatomy from the prior arthroplasty [16]. These challenges have led to poor long-term implant survivorship (70% at 10 years) with a high frequency of postoperative complications and late complications leading to reoperation in a number of series [12, 13].
The goals of treating periprosthetic femur fractures include fracture healing and stable long-term implant fixation [7]. Recently, modular fluted, tapered stems have gained prominence in the revision setting. Such designs give surgeons the ability to achieve axial and rotational control of the implant in the diaphysis of the femur, distal to the proximal bone loss and comminution often present in periprosthetic fractures [3].
A few series have demonstrated the potential value of this technique, but most investigations to date are limited by small patient numbers and short followup [11, 14, 17, 18, 20–22]. The purpose of the current study was to determine the results of uncemented modular fluted, tapered stems for periprosthetic femoral fractures in regard to radiographic union and implant stability. Secondary objectives included determining patient outcome using the Harris hip score and surgical complications.
Patients and Methods
We performed a review of all uncemented modular fluted, tapered stems used for the treatment of Vancouver B2 or B3 periprosthetic femur fractures around THA at a single, tertiary care academic institution from 2000 to 2006. Patients were identified through a prospectively collected institutional database used to follow all patients who have undergone a total joint arthroplasty at our institution since 1969. Institutional review board approval was obtained before initiation of the study.
Postoperative periprosthetic femur fractures were classified according to the Vancouver system, which incorporates the site of the fracture, stability of implant, and quality of surrounding bone [6]. All patients included in this study had a loose stem and a Vancouver B2 (25 patients) or B3 (19 patients) fracture (Fig. 1A–B) for a total of 44 patients. The minimum followup was 2 years (mean, 4.5 years; range, 2–8 years), excluding five patients who died at less than 2 years after their surgical intervention. No patients were lost to clinical or radiographic followup.
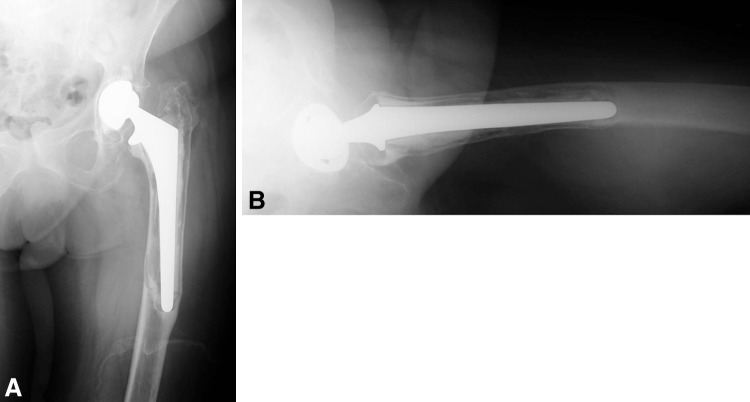
Fig. 1A–B.
(A) AP and (B) lateral radiographs are shown of an 88-year-old woman with a left Vancouver B3 periprosthetic femur fracture.
During this time period, a total of 129 revision THAs were performed for periprosthetic femur fractures. Fifty-four of these were graded as Vancouver B2 (defined as loose stem), and 62 were graded as Vancouver B3 fractures (defined as loose stem with substantial bone loss). Of these 116 patients, 52% (60 patients) were treated with fully coated stems, whereas 10% (12 patients) received long cemented stems. Of the 129 revision THAs for periprosthetic fractures, 44 (34%) were performed with modular fluted, tapered stems. The type of implant used was at the surgeon’s discretion, but this class of implant tended to be used selectively for more severe fractures during this time period.
This study cohort included 24 female patients (55%) and 20 male patients (45%). Thirty-seven patients (84%) experienced a periprosthetic fracture after a primary procedure, whereas seven patients (16%) sustained a periprosthetic fracture after a revision procedure. The mean age was 72 years (range, 34–92 years). The most common underlying diagnosis was osteoarthritis (75%) followed by rheumatoid arthritis (9.1%).
The mean operative time was 251 minutes (range, 113–426 minutes). The operative exposure was transtrochanteric in 23 patients, anterolateral in 12, and posterolateral in nine. The femoral implant used was a Link MP Reconstruction stem (Waldemar Link, Hamburg, Germany; 29 patients) or a Stryker Restoration Modular stem (Stryker, Mahwah, NJ, USA; 15 patients). Eight cortical strut allografts were used. The mean stem length was 230 mm (range, 180–330 mm) and the mean stem diameter was 18 mm (range, 14–22.5 mm). The femoral head diameter was 28 mm in 15 patients, 32 mm in 12, 36 mm in 14, and 40 mm in three. The existing acetabular component was retained in 14 hips; in 12 hips, the polyethylene liner of the existing acetabular component was exchanged but the metal shell was retained; and in 18 hips, the entire acetabular component was revised.
The Harris hip score and ambulatory status were used for clinical assessment by the operative surgeon [8].
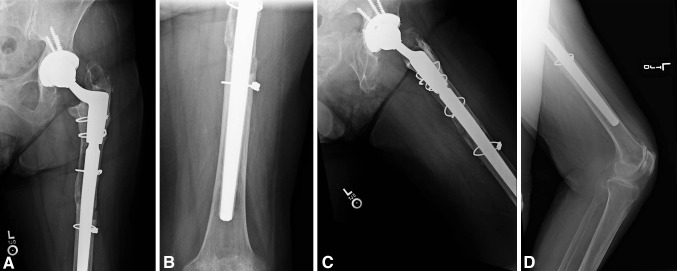
Radiographs from the preoperative, immediate postoperative, and each subsequent visit were analyzed. Postoperative radiographs were assessed for implant stability and fracture union. Subsidence was measured from fixed landmarks on the prosthesis (such as the modular junction) to fixed landmarks on the femur (such as cerclage cables). Implant loosening was defined as progressive implant subsidence or a continuous radiolucent line around the femoral component [16]. Fracture union was defined as bony bridging across the major visible fracture lines on serial radiographs (Fig. 2A–D).
Fig. 2A–D.
(A) Proximal AP, (B) distal AP, (C) proximal oblique, and (D) distal oblique radiographs are shown of the previous patient 6 years postoperatively revealing fracture union without subsidence or loosening.
Kaplan-Meier survivorship analyses were performed with revision of the femoral component for any reason as the end point [9].
Surgical Technique
Preoperative planning was completed with the use of templates to determine the approximate diameter and length of the proposed femoral implant. Regardless of operative approach to the hip (transtrochanteric, anterolateral, or posterior), the goal was to expose the proximal femur and failed implant with minimal disruption of the femoral bone blood supply and maximum preservation of soft tissue attachments to bone. The proximal femur was exposed either by splitting the muscle along the fracture lines or through the use of an osteotomy. If an osteotomy was used, a modified Wagner (extended trochanteric osteotomy) technique was preferred [4]. In this technique, the proximal femur was split in the coronal plane with the osteotomy entering the lateral femur, the tip of the greater trochanter, and then extending distally to the fracture. The medial cortex of the femur was split either through an existing fracture line or by completion of the osteotomy medially with an osteotome or saw. Effort was taken to preserve the entire muscle envelope. The abductors were split no greater than 5 cm proximal to the tip of the greater trochanter to prevent denervation. Distally, the femur was accessed by splitting the vastus lateralis along fracture lines to the level of the intact diaphysis.
Subsequently, the intact diaphysis was sequentially reamed with tapered stem reamers. Such reaming was performed until a medullary canal was milled to a strong supportive cone for the implant. A prophylactic cable or wire was then placed around the femur just distal to the fracture. Trial implants were placed and trial reduction was performed to ensure the implant would seat at a level that adequately restored leg length and hip stability. Next, a modular fluted, tapered stem was impacted into the intact diaphysis until it was rigidly stable to axial and torsional testing. The modular portions of the implants were used to reproduce optimal proximal implant length and anteversion. After reduction, the proximal fracture fragments were pulled around the upper portion of the femur with cerclage cables, wires, and/or sutures using the new implant as a scaffold around which the proximal femur was reconstituted. Anatomic reduction was not always obtained and the goal was preservation of blood supply to the fragments of the proximal femur. When available, autogenous bone graft reamings from the femur or acetabulum were packed along the accessible fracture lines.
The postoperative regimen included toe-touch weightbearing for 8 weeks followed by partial weightbearing for 1 month and then progressive weightbearing for an additional month. At 4 months postoperatively, patients were allowed to be weightbearing as tolerated without support.
Results
At most recent followup, 43 of 44 fractures (98%) had achieved radiographic union. In many patients, there was marked reconstitution of femoral bone stock related to fracture healing. One patient experienced aseptic femoral loosening and was revised to another modular fluted, tapered stem with a larger diameter. At last followup, she was doing well and free from revision. Of the remaining 43 stems, 42 had no measurable subsidence and were radiographically well fixed. One stem subsided 5 mm and then stabilized and appeared radiographically well fixed. Therefore, 43 of 44 patients had a well-fixed implant at last followup and 42 of 44 (96%) of patients had a well-fixed stem and healed fracture at last followup.
The mean postoperative Harris hip score was 83 (range, 55–99). All patients were ambulatory at most recent followup.
There were seven additional reoperations. Five patients (11%) had recurrent instability that was treated with reoperation. Of the five patients, three were converted to a constrained implant, one had revision of the acetabular component, and one had a larger diameter femoral head placed. All recurrent dislocations occurred in patients treated with a 28-mm or 32-mm femoral head diameter. Two patients had a deep infection, which in each case was treated with a two-stage procedure. In both, eventual reimplantation was completed successfully with another uncemented modular fluted, tapered stem. There were three other complications: one patient had a superficial infection treated with antibiotics, one had a deep venous thrombosis, and one patient had an intraoperative femur fracture that was recognized at the time of surgery and treated with a cerclage wire.
Discussion
The incidence of periprosthetic femoral fractures is increasing as a result of several factors. Foremost, excellent results with THA have led to expanded indications for the procedure, including more younger and elderly patients [13]. Furthermore, the average life expectancy has increased, leading to more elderly patients with THAs. This patient population has an increased risk of falls and poorer bone quality, which increase the risk for periprosthetic femoral fractures [13]. In this series, we found that uncemented modular fluted, tapered stems provided a high rate of implant stability and fracture union for treatment of this challenging diagnosis. In many patients, there was reconstitution of the proximal femoral bone without the need for bone grafting and cortical struts.
A limitation of the current study is the duration of followup. However, our followup was sufficiently long to demonstrate fracture healing, implant stability, and frequent reconstitution of proximal bone. Longer followup is essential to make certain that complications associated with modularity such as corrosion and implant fracture do not become an issue. This study included two similar implant designs from different manufacturers. With the numbers and followup period available, we did not observe differences between the results of each design; however, it is possible that differences in the implant designs, including different methods of attaching the modular stem to the proximal body, may lead to differing longer term results for the two implant designs.
Revision techniques for periprosthetic fractures include using cemented and uncemented stems, allograft-prosthetic composites, and/or a proximal femoral replacement [15]. Some series of cemented components have demonstrated a high rate of loosening, nonunion, and refracture [2, 19]. Springer et al. [19] found that of 18 patients who had revision surgery for periprosthetic fractures with an allograft-prosthetic composite or tumor prosthesis, seven failed because of aseptic loosening and one as a result of infection. More recently, modular fluted, tapered stems have been used to treat Vancouver B2 and B3 periprosthetic femoral fractures. Such components gain rotational and axial stability distal to the fracture site while preserving the proximal femoral bone. At a mean followup of 4.8 years, Park et al. reported a 92.6% union rate in 27 Vancouver B2 and B3 periprosthetic femoral fractures treated with a Link prosthesis (Table 1) [16]. Two patients subsided and two required revisions. Similarly, Mulay et al. noted a 91% union rate [15]. Berry previously reported on the preliminary results (mean followup, 1.5 years) of eight patients from our institution with Vancouver B3 femur fractures treated with long modular fluted, tapered uncemented stems. All patients had stable implants, healed fractures, and marked reconstitution of proximal femoral bone stock [4]. It should also be noted that there are some patulous canals in osteoporotic patients in whom a modular fluted, tapered stem will not allow for distal fixation. However, we did not experience such an issue in this series given that all patients who received this particular type of implant were chosen at the surgeon’s discretion.
Table 1.
Modular fluted, tapered stems in the literature
Dislocation was the most common complication (11% in this series) but may be reduced by more consistent use of larger femoral head diameters, which has become the practice since the time of this study. Of note, all dislocations occurred in patients with either 28-mm or 32-mm femoral heads. This rate is approximately half the rate (21%) reported by Mulay et al. but is greater than that reported by Park et al. (no dislocations out of 25 hips) [15, 16].
In summary, uncemented modular fluted, tapered stems provide reconstitution of the proximal femoral bone while being associated with a high rate of fracture union and implant stability. It is our current practice to routinely use uncemented modular fluted, tapered stems for Vancouver B2 and B3 periprosthetic femoral fractures that require distal fixation.
Acknowledgments
We thank Youlonda A. Loechler for her assistance in data collection from the total joint database.
Footnotes
The institution of one or more of the authors (MPA, DGL, DJB) has received funding from DePuy (Warsaw, IN, USA), Zimmer (Warsaw, IN, USA), Stryker (Mahwah, NJ, USA), and Biomet (Warsaw, IN, USA). One author certifies that he (DJB), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount in excess of USD 100,000 from DePuy Orthopaedics, Inc, a Johnson and Johnson Company (Warsaw, IN, USA). Another author certifies that he (DGL), or a member of his immediate family, has or may receive payments or benefits, during the study period, an amount in excess of USD 100,000 from Zimmer, Inc (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry. 2010 Annual Report. Adelaide, Australia: AOA; 2010.
- 2.Beals RK, Tower SS. Periprosthetic fractures of the femur. An analysis of 93 fractures. Clin Orthop Relat Res. 1996;327:238–246. doi: 10.1097/00003086-199606000-00029. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ. Total hip arthroplasty in patients with proximal femoral deformity. Clin Orthop Relat Res. 1999;369:262–272. doi: 10.1097/00003086-199912000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Berry DJ. Treatment of Vancouver B3 periprosthetic femur fractures with a fluted tapered stem. Clin Orthop Relat Res. 2003;417:224–231. doi: 10.1097/01.blo.0000096821.67494.f6. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 6.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 7.Garbuz DS, Masri BA, Duncan CP. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect. 1998;47:237–242. [PubMed] [Google Scholar]
- 8.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 9.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 10.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 11.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;18:94–97. doi: 10.1054/arth.2003.50083. [DOI] [PubMed] [Google Scholar]
- 12.Lindahl H, Garellick G, Regner H, Herberts P, Malchau H. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am. 2006;88:1215–1222. doi: 10.2106/JBJS.E.00457. [DOI] [PubMed] [Google Scholar]
- 13.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857–865. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 14.McInnis DP, Horne G, Devane PA. Femoral revision with a fluted, tapered, modular stem seventy patients followed for a mean of 3.9 years. J Arthroplasty. 2006;21:372–380. doi: 10.1016/j.arth.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 15.Mulay S, Hassan T, Birtwistle S, Power R. Management of types B2 and B3 femoral periprosthetic fractures by a tapered, fluted, and distally fixed stem. J Arthroplasty. 2005;20:751–756. doi: 10.1016/j.arth.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 16.Park MS, Lim YJ, Chung WC, Ham DH, Lee SH. Management of periprosthetic femur fractures treated with distal fixation using a modular femoral stem using an anterolateral approach. J Arthroplasty. 2009;24:1270–1276. doi: 10.1016/j.arth.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez JA, Fada R, Murphy SB, Rasquinha VJ, Ranawat CS. Two-year to five-year follow-up of femoral defects in femoral revision treated with the link MP modular stem. J Arthroplasty. 2009;24:751–758. doi: 10.1016/j.arth.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 18.Schuh A, Werber S, Holzwarth U, Zeiler G. Cementless modular hip revision arthroplasty using the MRP Titan Revision Stem: outcome of 79 hips after an average of 4 years’ follow-up. Arch Orthop Trauma Surg. 2004;124:306–309. doi: 10.1007/s00402-004-0656-7. [DOI] [PubMed] [Google Scholar]
- 19.Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am. 2003;85:2156–2162. doi: 10.2106/00004623-200311000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Tamvakopoulos GS, Servant CT, Clark G, Ivory JP. Medium-term follow-up series using a modular distal fixation prosthesis to address proximal femoral bone deficiency in revision total hip arthroplasty. A 5- to 9-year follow-up study. Hip Int. 2007;17:143–149. doi: 10.1177/112070000701700304. [DOI] [PubMed] [Google Scholar]
- 21.Weiss RJ, Beckman MO, Enocson A, Schmalholz A, Stark A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty. 2011;26:16–23. doi: 10.1016/j.arth.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Wirtz DC, Heller KD, Holzwarth U, Siebert C, Pitto RP, Zeiler G, Blencke BA, Forst R. A modular femoral implant for uncemented stem revision in THR. Int Orthop. 2000;24:134–138. doi: 10.1007/s002640000135. [DOI] [PMC free article] [PubMed] [Google Scholar]