Abstract
Background
Many studies suggest long femoral components should be used in revision THA. However, longer stems are more difficult to insert and reduce femoral bone stock for future revisions.
Questions/purposes
We investigated (1) how frequently a short (≤ 160-mm or primary-length) fully porous-coated stem could be utilized for Paprosky Type I to IIIA femoral defects, (2) how often the tip of the old stem or cement mantle was bypassed by the revision implant, (3) Harris hip scores, radiographic signs of osseointegration, and revision frequency, and (4) complications associated with these reconstructions.
Methods
Two surgeons performed 277 femoral revisions graded as Paprosky Types I to IIIA between 2004 and 2009. When femoral canal diameter was less than 18 mm, these surgeons generally used the shortest stem capable of achieving a minimum of 4 cm of scratch fit in the femoral isthmus. Patients were evaluated clinically using the Harris hip score and radiographically for component loosening and to determine whether the revision component bypassed the prior stem tip or cement mantle.
Results
A short stem was utilized in 144 of the 277 revisions (52%). In 113 (78%), the revision femoral component did not bypass the tip of the prior stem or cement mantle. The Harris hip score improved (p < 0.001) from 36 preoperatively to 76 at a mean of 4 years (range, 2–8 years). Twelve stems required repeat revision including six (4.9%) for failed ingrowth. Complications included four intraoperative fractures, three postoperative femoral fractures, one cortical perforation, and eight dislocations.
Conclusions
Primary-length extensively coated stems provided reliable fixation for ½ of our Paprosky Type I to IIIA femoral revisions. When considering the use of such a component, the revision surgeon should take into account a small risk of failed osseointegration and technical challenges associated with this technique.
Level of Evidence
Level IV, therapeutic study. See the Instructions to Authors for a complete description of levels of evidence.
Introduction
Rates of revision THA continue to rise [15]. The revision hip surgeon faces a multitude of decisions regarding preoperative planning, approach, implant type, and postoperative management. There remains a paucity of literature to assist the surgeon with the difficult choice of femoral implant type in revision THA.
THA revisions involving the femoral component are often complicated by proximal femoral bone loss. Fully porous-coated cementless stems provide a durable option for achieving stable distal fixation [10, 14, 16, 21, 23, 24, 30]. Historically, it has been suggested that revision stems should bypass femoral defects by at least two cortical diameters [4]. However, this practice is not well supported in the literature. Furthermore, the use of longer revision-type stems oftentimes requires navigation of the femoral bow [18, 27], which increases complexity, may increase the risk of intraoperative fracture [5], and reduces bone stock for future reconstructions [25].
Studies assessing radiographic osseointegration [6], stem failure rates [23], and torsional stability [19] demonstrate that a minimum of 4 cm of diaphyseal scratch fit is needed to provide adequate cementless fixation of the femoral component. In cases of mild to moderate proximal bone loss (Paprosky I, II, and IIIA femoral defects), this can often be achieved with the use of a primary-length fully coated monoblock femoral component that may not bypass the distal margin of the prior stem or cement mantle.
We therefore investigated (1) how frequently a short (≤ 160-mm or primary-length) fully porous-coated stem could be utilized for Paprosky Type I to IIIA femoral defects, (2) how often the tip of the old stem or cement mantle was bypassed by the revision implant, (3) Harris hip scores, radiographic signs of osseointegration, and revision frequency associated with these reconstructions, and (4) complications associated with the use of primary-length stems in revision THAs.
Patients and Methods
After obtaining institutional review board approval, we reviewed the medical records of 343 consecutive patients who underwent revision of the femoral component by one of the two senior authors (SMS, CJDV) between June 2004 and December 2009. The radiographs of these hips were graded using the Paprosky classification to identify all Paprosky Type I to IIIA femoral defects where a fully porous-coated stem could theoretically have been utilized [7] (Fig. 1). Sixty-six revisions were graded as Paprosky IIIB or IV, leaving 277 revisions that were reviewed. Our preference was to use primary-length, fully coated stems when initial intraoperative stability could be achieved with a minimum of 4 cm of scratch fit in the femoral isthmus. Common reasons for not using the primary-length stems included the following: in Type I defects, a proximally coated primary-length stem could occasionally be used (akin to a primary procedure), particularly in cases of failed hip resurfacings; in Type II defects, a slightly longer (7-inch) fully coated stem was sometimes needed to achieve adequate diaphyseal scratch fit for intraoperative stability; and in Type IIIA defects, a 7- or 8-inch fully coated monoblock stem was required for defects that spanned more distally, and modular titanium tapered stems were generally used if the diameter of the canal was larger than 18 mm or if marked proximal femoral remodeling precluded the use of a monoblock stem to optimize stability. A total of 144 femoral revisions in 139 patients were performed using primary-length fully coated monoblock stems. Of the 139 patients, 13 (9.0%) were deceased and nine (6.3%) were lost to followup before a minimum of 2 years, leaving 117 patients with 122 revisions. These 65 women and 52 men had a mean age at time of surgery of 63 years (range, 22–88 years) and were followed for a minimum of 2 years (mean, 4 years; range, 2–8 years).
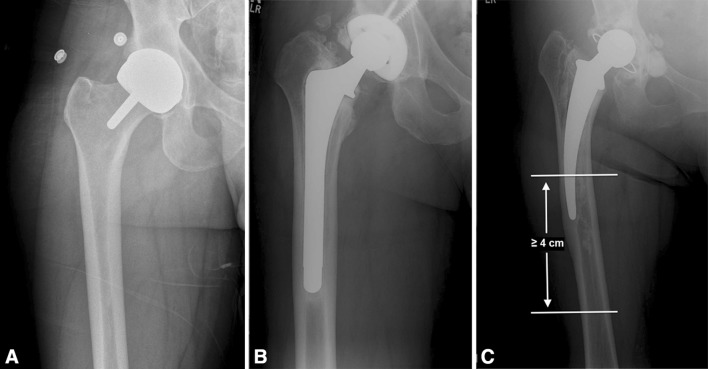
Fig. 1A–C.
Radiographs illustrate the Paprosky classification scheme. (A) In Type I femoral deficiency, there is minimal loss of metaphyseal cancellous bone and an intact diaphysis. (B) In Type II femoral deficiency, there is extensive loss of metaphyseal cancellous bone and an intact diaphysis. (C) In Type IIIA femoral deficiency, the metaphysis is severely damaged and nonsupportive, with at least 4 cm of intact diaphyseal bone available for distal fixation. The horizontal lines on the radiograph demarcate the amount of femoral isthmus available for distal fixation.
Preoperative femoral defects included two (1.6%) Paprosky Type I, 64 (52%) Type II, and 56 (46%) Type IIIA. The indication for revision THA was periprosthetic joint infection in 54 (44%) hips, aseptic loosening in 48 (39%), instability in seven (5.7%), periprosthetic femur fracture in six (4.9%), broken stem in two (1.6%), polyethylene wear with osteolysis in two (1.6%), metallosis in one (0.8%), failed resurfacing in one (0.8%), and component malposition (retroversion) in one (0.8%). Before revision surgery, templates were used to estimate the length and diameter of the stem required to achieve a minimum of 4 cm of scratch fit in the femoral isthmus. In all revisions, the femoral canal was underreamed by 0.5 mm relative to the diameter of the final implant. The distribution of stem diameters utilized is provided (Table 1). An extended or extra-extended offset neck was used in 17 (14%) hips and a low head center option neck was used in three (2.5%) hips. The specific stems used included the VerSys® 6-inch Beaded Full Coat (Zimmer Inc, Warsaw, IN, USA; n = 106), VerSys® Epoch® 2 Full Coat (Zimmer Inc; n = 5), Echelon Primary (Smith & Nephew Inc, Memphis, TN, USA; n = 10), and Solution System® (DePuy Orthopaedics Inc, Warsaw, IN, USA; n = 1). These devices were all FDA-approved for this use. All revision procedures were carried out via a posterior approach to the hip and an extended trochanteric osteotomy was utilized in 30 (25%) revisions. The general indications for extended osteotomy in these patients included the removal of a well-fixed cemented or cementless stem to access the bone-cement or bone-prosthesis interface or the presence of a subsided femoral component in which extraction using standard techniques would risk fracture of the greater trochanter. Concomitant acetabular component revision was performed in 97 (80%) revisions. The bearing surface was metal-on-polyethylene in 121 hips (99%) and metal-on-metal in one hip (0.8%).
Table 1.
Distribution of implanted stem diameters
| Stem diameter (mm) | Number of patients (n = 122) |
|---|---|
| 11 | 1 (0.8%) |
| 12 | 4 (3.3%) |
| 13 | 5 (4.1%) |
| 14 | 14 (11.5%) |
| 15 | 22 (18.0%) |
| 16 | 23 (18.9%) |
| 17 | 24 (19.7%) |
| 18 | 17 (13.9%) |
| 19 | 3 (2.5%) |
| 20 | 5 (4.1%) |
| 21 | 3 (2.5%) |
| 22 | 1 (0.8%) |
Each patient was evaluated preoperatively and postoperatively at 3 weeks, 6 weeks, 3 months, and annually thereafter for examination and radiographic followup. At each visit, standard evaluation measures included a Harris hip score [12] and plain radiographs (an AP view of the pelvis and AP and lateral views of the affected hip and femur). The 6-week postoperative plain films were compared to preoperative films to determine how often the revision stem bypassed the prior stem tip or cement. Serial radiographs were reviewed to evaluate osseointegration of the revision component using the criteria of Engh et al. [9]. Harris hip scores preoperatively and at final followup were compared using a paired t-test. Complications, including femoral fracture, dislocation, infection, and failed ingrowth of the femoral component, were noted and rerevision rate of the femoral component was assessed.
Results
Using our indication of employing primary-length revision stems when initial intraoperative stability could be achieved over 4 to 6 cm of diaphysis, we found we were able to use these short fully coated stems in a little more than ½ of Paprosky I to IIIA femoral revisions. Of 277 consecutive revisions over a 6.5-year period, a primary-length fully porous-coated stem was utilized in 144 (52%) instances. This included two of five (40%) Type I, 77 of 112 (69%) Type II, and 65 of 160 (41%) Type IIIA femoral defects.
Most of the primary-length fully coated revision stems did not bypass the tip of the prior stem or cement mantle (113 of 144 revisions, 78%). This included two of two (100%) Type I, 60 of 77 (78%) Type II, and 51 of 65 (78%) Type IIIA femoral defects. More than 4 cm of scratch fit was obtained in the remaining femoral isthmus in all revisions.
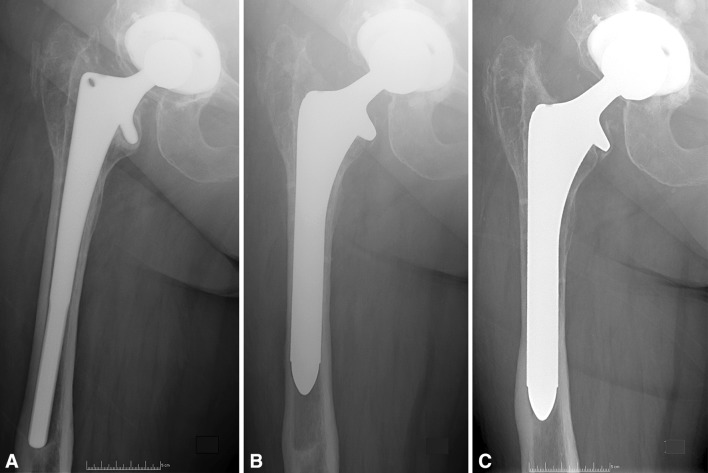
In the 122 hips with at least 2-year followup, the mean Harris hip score improved (p < 0.001) from a preoperative mean of 36 points (range, 0–93 points) to 76 points (range, 21–100) at the time of the most recent evaluation. Six of the 122 stems (4.9%) were determined to be loose on plain radiographs and underwent repeat femoral revision. The remaining stems were noted to be osseointegrated (Fig. 2). The loose stems occurred in four of 64 (6.3%) Type II femurs and two of 56 (3.6%) Type IIIA femurs. One of nine (11.1%) stems with a diameter of greater than 19 mm failed due to aseptic loosening compared to five of 113 (4.4%) with a diameter of 19 mm or less. An additional five stems (3.5%) were removed for deep infection and one well-fixed stem (0.7%) was revised for exposure during a complex acetabular revision.
Fig. 2A–C.
(A) A preoperative AP radiograph demonstrates a loose cementless stem with a Paprosky Type IIIA femoral defect. (B) A 4-month postoperative AP radiograph shows the 6-inch fully porous-coated stem used at revision. (C) At 4-year followup, an AP radiograph shows that the stem remains well fixed with distal spot welds evidencing bone ingrowth.
Additional complications included five (3.5%) intraoperative femoral shaft fractures (three Vancouver C fractures [3, 8] managed with a locking plate, one proximal femoral fracture treated with cerclage cables, and one anterior cortical perforation managed without further intervention); three (2.1%) postoperative fractures (all Vancouver B1; two treated with a locking plate and one managed nonoperatively); and eight (5.6%) dislocations (four close reduced without surgical intervention, three requiring conversion to a constrained liner, and one requiring revision for a loose stem). The five intraoperative fractures occurred in femurs in which the prior stem and cement mantle were not bypassed.
Discussion
Most femoral revisions in North America are performed with cementless stems. Goals of the procedure include obtainment of rigid immediate distal fixation to allow for osseointegration of the implant [9]. Many surgeons believe that revision femoral components must be long and bypass the prior stem [4]. We investigated the use of primary-length diaphyseal-engaging porous-coated stems in patients with mild to moderate femoral bone loss (Paprosky Types I–IIIA) in terms of (1) how frequently a short (≤ 160-mm or primary-length) fully porous-coated stem could be utilized for these femoral defects, (2) how often the tip of the old stem or cement mantle was bypassed by the revision implant, (3) Harris hip scores, radiographic signs of osseointegration, and revision frequency, and (4) complications.
Limitations of this study include its retrospective nature. A prospective randomized study would better answer whether the use of a shorter fully porous-coated stem would provide superior radiographic or clinical results or a lower risk of complications than would a longer-length or different stem design. That said, our retrospective series is large and we used consistent indications that should generalize well to most revision settings. Our length of followup was also relatively short; however, once osseointegrated, this type of stem has not been associated with loosening and thus we believe our results on osseointegration are likely to be durable [21, 23, 30]. Selection bias is a possible study limitation as some patients were deemed candidates for this approach while others were not. It is important to emphasize, however, that patient selection, even among those with Type I to IIIA femur defects, is vital to the effectiveness of this technique; in patients with considerable proximal remodeling of the femur or canal diameters larger than 18 mm, utilization of a monoblock fully coated stem is not recommended. Only in patients with 4 cm of isthmus available for distal fixation and canal diameters smaller than 19 mm is it reasonable to attempt this approach. Finally, while our results reported are good, the surgical technique may be experience-dependent as the authors had significant exposure to inserting stems of this design during their fellowship training and subsequent practice. While not a “limitation” of our study per se, we would like to point out that the selective use of short stems in the revision setting was based on the particular patterns of femoral bone loss identified on preoperative radiographs that we described in the Patients and Methods section. We continue to believe that acute intraoperative femoral perforations and severe femoral cortical defects identified preoperatively should be bypassed by using longer stems.
Our study found that a primary-length monoblock stem can be used in approximately ½ of femoral revisions associated with mild to moderate bone loss, and that this approach to reconstruction achieves a high rate of osseointegration so long as 4 cm of distal fixation is obtained. Krishnamurthy et al. [14] reported using 6-inch fully coated stems in 109 of 297 (36.7%) cementless femoral revisions for Type I to III femoral defects using an earlier classification system before the differentiation of Type IIIA and IIIB femoral defects. Our study strengthens the literature in support of this technique by showing that an even larger portion of revisions is amenable to primary-length stems when Type IIIB femoral defects are removed. Advantages of using a shorter stem include a simpler surgical technique [18, 27], the potential for a lower risk of complications [5], and preservation of femoral bone stock for future revisions if required [25]. Although the numbers of patients in each of our subgroups was small, we did see a trend toward a higher risk of failed ingrowth with stem diameters larger than 18 mm, and in these situations, we typically will use a tapered, titanium modular stem, as prior work has shown a canal diameter larger than 18 mm to be a risk factor for failure of osseointegration with monoblock fully coated stems [26].
Others have suggested that revision stems should bypass the tip of the prior stem or cement mantle by two cortical diameters [4]. In our series, the tip of the prior stem or cement mantle was not bypassed in the majority of revisions (78%), with a low rate of failed osseointegration similar to those of prior studies (Table 2). A key objective of femoral revision is to replace the initial stem with a stem that gains fixation “as proximal as possible and as distal as necessary” [2]. Because of proximal bone stock deficiency in the majority of revisions, axial and rotational stability is most reliably achieved in the diaphysis rather than the metaphysis [14, 28]; however, it does not appear that the revision implant must bypass the tip of the prior stem or cement mantle in most cases. This is an important and relatively novel point of emphasis of our work: primary-length fully coated stems may be utilized even when they stop short of prior defects.
Table 2.
Selected literature regarding extensively coated stem use in femoral revision THA
| Study | Number of hips | Followup (years)* | Surgical variables | Radiographic assessment | Stem failure rate |
|---|---|---|---|---|---|
| Weeden and Paprosky [30] | 170 | 14.2 (11–16) | Type I–IIIB defects | 82% ingrown 14% fibrous stable 4% unstable |
Overall: 4.1% mechanical failure Type II or IIIA: 5% failure Type IIIB: 21% failure 3.5% femoral revision for aseptic loosening |
| Krishnamurthy et al. [14] | 297 | 8.3 (5–13) | Type I–III defects (no differentiation between IIIA/IIIB) | 82% ingrown 15.6% fibrous stable 2.4% unstable |
2.4% mechanical failure (all Type III defects) 1.7% femoral revision for aseptic loosening |
| Della Valle and Paprosky [6] | 71 | 8 (minimum) | Type I–IV defects | Type I–IIIA: 96% ingrown Type IIIB or IV: 36% ingrown |
Failures not specified |
| Moreland and Moreno [21] | 137 | 9.3 (5–16) | Defects not specified | 83% ingrown 14% stable fibrous 3% unstable |
4% femoral revision for aseptic loosening |
| Moreland and Bernstein [20] | 175 | 5 (2–10) | Defects not specified | Overall: 82.8% ingrown Type I: 98% ingrown Type III: 76% ingrown |
2.9% mechanical failure 1.1% femoral revision for aseptic loosening |
| Lawrence et al. [16] | 83 | 9 (5–13) | “Mild” (not significantly damaged) “Moderate” (extensive damage above level of lesser trochanter without diaphyseal extension) “Severe” (bone stock damage extending into diaphysis) |
98.9% “stable” (bone or fibrous ingrown) 1.1% unstable |
11% mechanical failure 10% femoral rerevision |
| Szusczewicz and Engh [29] | 729 | 5.5 (0–19.2) | Femurs with minimum of 5 cm of distal fixation | Type I: 98% ingrown Type II: 85% ingrown Type IIIA: 75% ingrown |
1.4% femoral revision for aseptic loosening 98.1% survivorship at 5 years 96.5% survivorship at 10 years |
| Engh et al. [11] McAuley and Engh [18] |
777 (same series in both studies) | 2 (minimum) | Bone loss < 10 cm or > 10 cm below lesser trochanter | 2.3% unstable | 1.5% femoral revision for aseptic loosening 97.7% survivorship at 5 years Survivorship greater for: (1) defects < 10 cm below lesser trochanter (2) straight vs bowed stems (3) stem length < 210 mm |
| Peace et al. [24] | 1000 | 6.9 (0–26.8) | Defects not specified | 88% ingrown 7% fibrous stable 5% unstable |
1.4% femoral revision for aseptic loosening 97.0% survivorship at 5 years |
| Current study | 122 | 3.9 (2.0–7.7) | 6-inch stems in Type I–IIIA defects | 95.1% ingrown 4.9% loose |
4.9% mechanical failure rate 4.9% femoral revision for aseptic loosening |
* Values are expressed as mean, with range in parentheses.
The radiographic and clinical outcomes reported in this study are comparable to published data on the use of extensively coated monoblock stems in comparable femoral defects (Table 2). We observed osseointegration of 96% of stems, while average rates of osseointegration reported for prior series of Paprosky Type I to III femoral revisions have ranged from 82% to 96% [6, 14, 30]. While prerevision femoral bone stock has been shown to influence the potential for osseointegration of the stem [11, 18, 26], we did not observe a tiered difference in osseointegration rates among Type I, II, and IIIA defects, as was previously reported by Szusczewicz and Engh [29]. The reason for this discrepancy is unclear, but we believe our findings reinforce that short stems can be utilized effectively across this spectrum of femoral defects so long as consistent parameters are present (≥ 4 cm of diaphyseal scratch fits in canals ≤ 18 mm).
The rate of intraoperative femoral fractures observed in this study (3.5%) compares favorably with those reported for prior series of cementless revisions, which ranged as high as 20.9% [1, 13, 17]. Using fully porous-coated cylindrical stems, Weeden and Paprosky [30] reported an 8% risk of femoral fracture during stem insertion and a 5.9% risk of perforation or fracture during cement removal. That study included Type IIIB defects in addition to Type I to IIIA defects but did not differentiate rates of intraoperative fracture among the groups. Nonetheless, the high rate of femoral fracture during stem insertion reinforces the need for careful exposure and insertion of the stem and seems to support the use of shorter stems that avoid the femoral bow if and when adequate fixation can be achieved [5]. It is important to note that three of the four intraoperative fractures requiring intervention in our series were Vancouver C fractures (distal to the implanted stem) and thus likely were related to torquing of the distal femur (most commonly during trialing and final reduction of the hip). Particular care must be taken during this portion of the surgery as well, as a possible trade-off of “going short” is fewer fractures during stem insertion relative to longer stems but increased susceptibility to stresses at the end of the stem during hip reduction. Our dislocation rate in this study was also substantial, as we have reported in other studies [22, 31]. We believe that this is unrelated to use of a shorter stem but rather an inherent part of revision THA that is independent of stem length.
On the basis of our experience, we believe that many femoral revisions with mild to moderate bone loss (Type I–IIIA defects) can be performed effectively with the use of a primary-length diaphyseal-engaging fully porous-coated stem. We believe it is not necessary to bypass prior defects as long as 4 cm of scratch fit is obtained. By using a shorter stem, the femoral bow is avoided, yielding a more straightforward technique and preserving bone stock for future revisions. The revision surgeon should be aware that a possible trade-off of “going short” is increased susceptibility to torquing stresses at the end of the stem resulting in intraoperative fracture during component trialing and final hip reduction. Our findings should be verified in prospective, comparative trials.
Footnotes
The institution of the authors has received, during the study period, funding from Zimmer Inc (Warsaw, IN, USA). One of the authors certifies he (SMS) has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to 100,000 from Zimmer Inc (Warsaw, IN, USA), an amount of USD 10,000 to 100,000 from Smith & Nephew, Inc (Memphis, TN, USA), and an amount of USD 10,000 to 100,000 from Cadence Health (Winfield, IL, USA). One of the authors certifies he (CJDV) has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to 100,000 from Biomet Inc (Warsaw, IN, USA), an amount of USD 10,000 to 100,000 from Smith & Nephew, Inc (Memphis, TN, USA), an amount of USD 10,000 to 100,000 from Stryker Orthopaedics (Mahwah, NJ, USA), an amount of USD 10,000 to 100,000 from CD Diagnostics (Wynnewood, PA, USA), and an amount of USD less than 10,000 from ConvaTec (Skillman, NJ, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30:183–190. doi: 10.1016/S0030-5898(05)70073-0. [DOI] [PubMed] [Google Scholar]
- 2.Bohm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004;420:148–159. doi: 10.1097/00003086-200403000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Brady OH, Garbuz DS, Masri BA, Duncan CP. Classification of the hip. Orthop Clin North Am. 1999;30:235–247. doi: 10.1016/S0030-5898(05)70078-X. [DOI] [PubMed] [Google Scholar]
- 4.Burnett RS, Rosenberg AG, Barrack RL. Revision total hip arthroplasty: principles, planning, and decision making. In: Barrack RL, Rosenberg AG, editors. Master Techniques in Orthopaedic Surgery: The Hip. 2. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 297–319. [Google Scholar]
- 5.Davidson C, Pike J, Garbuz D, Duncan CP, Masri BA. Intraoperative periprosthetic fractures during total hip arthroplasty: evaluation and management. J Bone Joint Surg Am. 2008;90:2000–2012. doi: 10.2106/JBJS.H.00331. [DOI] [PubMed] [Google Scholar]
- 6.Della Valle CJ, Paprosky WG. Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J Bone Joint Surg Am. 2003;85(suppl 4):1–6. [DOI] [PubMed]
- 7.Della Valle CJ, Paprosky WG. The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res. 2004;420:55–62. [DOI] [PubMed]
- 8.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 9.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 10.Engh CA, Jr, Ellis TJ, Koralewicz LM, McAuley JP, Engh CA., Sr Extensively porous coated femoral revision for severe femoral bone loss: minimum 10-year follow-up. J Arthroplasty. 2002;17:955–960. doi: 10.1054/arth.2002.35794. [DOI] [PubMed] [Google Scholar]
- 11.Engh CA, Jr, Hopper RH, Jr, Engh CA., Sr Distal ingrowth components. Clin Orthop Relat Res. 2004;420:135–141. doi: 10.1097/00003086-200403000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end- result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 13.Issack PS, Guerin J, Butler A, Marwin SE, Bourne RB, Rorabeck CH, Barrack RL, Di Cesare PE. Intraoperative complications of revision hip arthroplasty using a porous-coated, distally slotted, fluted femoral stem. Clin Orthop Relat Res. 2004;425:173–176. doi: 10.1097/00003086-200408000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Krishnamurthy AB, MacDonald SJ, Paprosky WG. 5- to 13-year follow-up study on cementless femoral components in revision surgery. J Arthroplasty. 1997;12:839–847. doi: 10.1016/S0883-5403(97)90152-2. [DOI] [PubMed] [Google Scholar]
- 15.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 16.Lawrence JM, Engh CA, Macalino GE. Revision total hip arthroplasty: long-term results without cement. Orthop Clin North Am. 1993;24:635–644. [PubMed] [Google Scholar]
- 17.Malkani AL, Lewallen DG, Cabanela ME, Wallrichs SL. Femoral component revision using an uncemented, proximally coated, long-stem prosthesis. J Arthroplasty. 1996;11:411–418. doi: 10.1016/S0883-5403(96)80031-3. [DOI] [PubMed] [Google Scholar]
- 18.McAuley JP, Engh CA. Femoral fixation in the face of considerable bone loss—cylindrical and extensively coated femoral components. Clin Orthop Relat Res. 2004;429:215–221. doi: 10.1097/01.blo.0000150274.21573.f4. [DOI] [PubMed] [Google Scholar]
- 19.Meneghini RM, Hallab NJ, Berger RA, Jacobs JJ, Paprosky WG, Rosenberg AG. Stem diameter and rotational stability in revision total hip arthroplasty: a biomechanical analysis. J Orthop Surg Res. 2006;1:5. doi: 10.1186/1749-799X-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moreland JR, Bernstein ML. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin Orthop Relat Res. 1995;319:141–150. [PubMed] [Google Scholar]
- 21.Moreland JR, Moreno MA. Cementless femoral revision arthroplasty of the hip: minimum 5 years followup. Clin Orthop Relat Res. 2001;393:194–201. doi: 10.1097/00003086-200112000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Murray TG, Wetters NG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. The use of abduction bracing for the prevention of early postoperative dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2012;27(suppl 8):126–129. doi: 10.1016/j.arth.2012.03.030. [DOI] [PubMed] [Google Scholar]
- 23.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 24.Peace WJ, Ho H, Hopper RH, Jr, Engh CA., Jr The outcome of extensively porous coated stems for revision total hip arthroplasty. Semin Arthroplasty. 2011;22:112–116. doi: 10.1053/j.sart.2011.03.017. [DOI] [Google Scholar]
- 25.Pinaroli A, Lavoie F, Cartillier JC, Neyret P, Selmi TA. Conservative femoral stem revision: avoiding therapeutic escalation. J Arthroplasty. 2009;24:365–373. doi: 10.1016/j.arth.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Sporer SM, Paprosky WG. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;417:203–209. doi: 10.1097/01.blo.0000096803.78689.0c. [DOI] [PubMed] [Google Scholar]
- 27.Sporer SM, Paprosky WG. Cementless femoral revision: the role of monoblock versus modular stems. Curr Orthop. 2006;20:171–178. doi: 10.1016/j.cuor.2006.02.006. [DOI] [Google Scholar]
- 28.Sugiyama H, Whiteside LA, Engh CA. Torsional fixation of the femoral component in total hip replacement: the effect of surgical press-fit technique. Clin Orthop Relat Res. 1992;275:187–193. [PubMed] [Google Scholar]
- 29.Szuszczewicz ES, Engh CA., Sr Femoral bone stock loss in total hip arthroplasty. Semin Arthroplasty. 2002;13:293–317. [Google Scholar]
- 30.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17(suppl 1):134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 31.Wetters NG, Murray TG, Moric MS, Sporer SM, Paprosky WG, Della Valle CJ. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2013;471:410–416. doi: 10.1007/s11999-012-2561-7. [DOI] [PMC free article] [PubMed] [Google Scholar]