Abstract
Background
Tibialis anterior tendon transfer surgery forms a part of Ponseti management for children with congenital talipes equinovarus who, after initial correction, present with residual dynamic supination. Although retrospective studies support good outcomes, prospective longitudinal studies in this population are lacking.
Questions/purposes
We assessed strength, plantar loading, ROM, foot alignment, function, satisfaction, and quality of life in patients with clubfoot that recurred after Ponseti casting who met indications for tibialis anterior tendon transfer surgery, and compared them with a group of patients with clubfoot treated with casting but whose deformity did not recur (therefore who were not indicated for tibialis anterior tendon transfer surgery).
Methods
Twenty children with idiopathic congenital talipes equinovarus indicated for tibialis anterior tendon transfer surgery were recruited. Assessment at baseline (before surgery), and 3, 6, and 12 months (after surgery) included strength (hand-held dynamometry), plantar loading (capacitance transducer matrix platform), ROM (Dimeglio scale), foot alignment (Foot Posture Index©), function and satisfaction (disease-specific instrument for clubfoot), and quality of life (Infant Toddler Quality of Life Questionnaire™). Outcomes were compared with those of 12 age-matched children with congenital talipes equinovarus not indicated for tibialis anterior tendon transfer surgery. Followup was 100% in the control group and 95% (19 of 20) in the tibialis anterior transfer group.
Results
At baseline, the tibialis anterior tendon transfer group had a significantly worse eversion-to-inversion strength ratio, plantar loading, ROM, foot alignment, and function and satisfaction. At 3 months after surgery, eversion-to-inversion strength, plantar loading, and function and satisfaction were no longer different between groups. Improvements were maintained at 12 months after surgery (eversion-to-inversion strength mean difference, 8% body weight; 95% CI, −26% to 11%; p = 0.412; plantar loading, p > 0.251; function and satisfaction, p = 0.076). ROM remained less and foot alignment more supinated in the tibialis anterior tendon transfer group between baseline and followup (p < 0.001, p < 0.001).
Conclusions
Tibialis anterior tendon transfer surgery was an effective procedure, which at 12-month followup restored the balance of eversion-to-inversion strength and resulted in plantar loading and function and satisfaction outcomes similar to those of age-matched children with congenital talipes equinovarus who after Ponseti casting were not indicated for tibialis anterior tendon transfer.
Level of Evidence
Level III, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Tibialis anterior tendon transfer is part of the Ponseti management for congenital talipes equinovarus, which, when indicated, seeks to decrease the likelihood of future recurrence of the deformity [8, 11, 12, 14, 16]. The decision to recommend surgery is made by observation of dynamic supination during gait and a manually tested imbalance between inversion and eversion strength [12].
Although long-term retrospective data have shown good outcomes after tibialis anterior tendon transfer surgery, the majority of trials include patients who have undergone various treatments, including serial plaster casting, and soft tissue and bony surgical procedures [6, 10, 13, 23]. Furthermore, it is unknown whether improvements after tibialis anterior tendon transfer surgery result in outcomes comparable to those of children with congenital talipes equinovarus who do not require this surgery.
We therefore assessed strength, plantar loading, ROM, foot alignment, function, satisfaction, and quality of life in patients with clubfoot that recurred after Ponseti casting who met indications for tibialis anterior tendon transfer surgery, and compared them with those of a group of patients with clubfoot treated with casting and but whose deformity did not recur (therefore who were not indicated for tibialis anterior tendon transfer surgery). We also compared the abovementioned end points before and after surgery in the tendon transfer group.
Patients and Methods
After institutional ethics board approval, a prospective case-control cohort study of children with idiopathic congenital talipes equinovarus before and after tibialis anterior tendon transfer was performed. Sample size was estimated with a power of 80% (α = 0.05). Based on clinical experience, the sample size was calculated to detect a difference between groups at 12 months’ followup of 50% (SD, 35%) in restoration of eversion-to-inversion muscle strength imbalance. With a total dropout and noncompliance rate of 10%, a minimum sample size of 12 participants in each group was estimated.
Patients and Surgical Indications
Indications for tibialis anterior transfer surgery, for the purposes of this study, were observation of a supinated foot during the swing phase of gait with initial weightbearing on the lateral border of the foot. The control group comprised age-matched patients who did not present with dynamic supination (and therefore were deemed not to require tibialis anterior tendon transfer). Patients with comorbidities, complex or atypical congenital talipes equinovarus, and prior foot surgery (other than Achilles tenotomy) were excluded.
Between August 2009 and October 2010, 21 patients (26 feet) met the study inclusion criteria and underwent tibialis anterior transfer surgery. All were invited to participate; of those, 20 patients (24 feet; 95%) agreed, were enrolled, and underwent the surgery.
An age-matched control group consisted of 12 patients (18 feet) with idiopathic congenital talipes equinovarus who were treated previously by Ponseti casting and showed acceptable compliance of the bracing regime. These patients did not meet indications for tibialis anterior tendon transfer surgery but were invited and agreed to participate in the study.
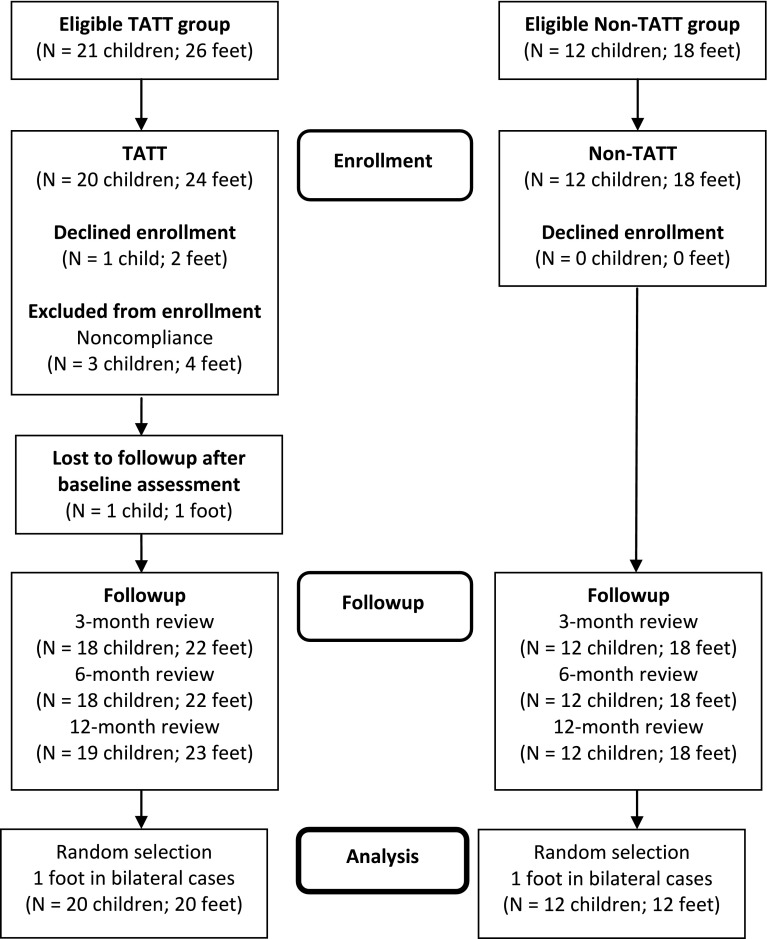
The average age of the patients at baseline was 50.5 months (tibialis anterior tendon transfer group, 53 ± 10 months; nontibialis anterior tendon transfer group, 48 ± 12 months) (Table 1). In both groups, more right feet were included and there were more boys than girls. One child in the tibialis anterior tendon transfer group was lost to followup after baseline assessment. All children in the nontibialis anterior tendon transfer group attended every followup. In the tibialis anterior tendon transfer group, 18 of 20 attended the 3- and 6-month followups and 19 of 20 attended the 12-month followup (Fig. 1). Owing to technical complications, not all patients could do the plantar loading assessment.
Table 1.
Patient characteristics
| Group | Number of patients | Age at initial presentation (months)* | Males/females (number of patients) | Presurgery casting (number of patients) | Number of bilateral cases | Foot (right/left) |
|---|---|---|---|---|---|---|
| TATT | 20 | 53 ± 10 | 16/4 | 14 | 6 | 11/9 |
| Non-TATT | 12 | 48 ± 12 | 11/1 | NA | 6 | 9/3 |
* Values are expressed as mean ± SD; TATT = tibialis anterior tendon transfer; NA = not applicable.
Fig. 1.
A flowchart for the study is shown.
Serial Casting
Of the 20 patients who underwent tibialis anterior tendon transfer surgery, 14 underwent repeat Ponseti serial plaster casting for secondary structural deformity before surgery. A combination of long and short leg casts were changed weekly until abduction and dorsiflexion were 30° or greater or a plateau in range was reached. Casts were removed 1 to 2 weeks before surgery and baseline assessment was conducted immediately before surgery.
Tibialis Anterior Tendon Transfer Procedure
All surgical procedures were performed by two surgeons (MB, PG) at the same hospital using a technique similar to that described by Thompson et al. [23]. In all but one foot, the tibialis anterior tendon was wholly transferred to the lateral cuneiform, attached via a whipstitch suture passed through a drill hole and sutured over a sponge and button in the sole of the foot. In the remaining foot, the tendon was wholly transferred to the intermediate cuneiform. Five feet required a posterior lengthening procedure for equinus deformity (indicated when there was less than 10° hindfoot dorsiflexion), which included soft tissue lengthening (five patients, five feet) and additional posterior ankle capsulotomy, subtalar capsulotomy, and division of the calcaneofibular ligament (three patients, three feet). Postoperatively, all but one foot were placed in a short leg cast in maximum dorsiflexion. The patients were nonweightbearing for 3 weeks and then weightbearing as tolerated for an additional 3 weeks. The final child wore a long leg cast (maximum abduction and dorsiflexion, knee 90°) for 6 weeks with the same weightbearing protocol. Casts were removed 6 weeks after surgery.
Bracing
One child was prescribed a night knee-ankle-foot orthosis after removal of the postsurgical cast as an additional precaution to prevent future relapse, and another child in the nontibialis anterior tendon transfer group wore a knee-ankle-foot orthosis at night previously prescribed after relapse.
Outcome Measures
Isometric foot muscle strength was assessed using a hand-held dynamometer (CIT Technics, Groningen, The Netherlands) using the reliable method described by Rose et al. [21]. Ankle inversion, eversion, dorsiflexion, and plantar flexion strength were measured using the “make” test, whereby the assessor holds the dynamometer stationary while the child exerts maximal force against it. Three trials were taken, normalized to body weight, and then averaged to produce a final strength score (expressed as percentage of body weight [% BW]).
Plantar loading was assessed using a capacitance transducer matrix platform (EMED-AT®; Novel GmbH, Munich, Germany). Data were collected using the midgait protocol where patients took a minimum of five barefoot steps at a self-selected pace before striking the platform [1]. Trials were excluded if there was obvious targeting of the pressure platform or if the pace was not representative of their normal gait. Three successful trials were recorded from each foot, averaged, and divided into medial and lateral regions (50%) for analysis.
Passive ROM was assessed in a standardized way using the classification of clubfoot (Dimeglio scale) [4], and foot alignment was assessed in standing using the Foot Posture Index© (Anthony Redmond, University of Leeds, Leeds, West Yorkshire, UK) [19, 20].
All patients were assessed at baseline (before surgery) and 3, 6, and 12 months after surgery by a physiotherapist (KG) with 9 years of experience.
Function and satisfaction were assessed using the disease-specific instrument for clubfoot questionnaire [3, 22], and quality of life was assessed using the Infant Toddler Quality of Life Questionnaire™ (www.healthact.com/itqol.php) [18].
Statistical Analysis
Descriptive statistics were calculated to characterize the study sample in SPSS® v 21 (SPSS Inc, Chicago, IL, USA). In bilateral cases, one side was randomly selected for inclusion (computer number generation) to satisfy the independence requirement for statistical analysis [15]. Therefore, the tibialis anterior tendon transfer and nontibialis anterior tendon transfer groups included 20 patients (20 feet) and 12 patients (12 feet), respectively. Independent t-tests were performed to compare groups and paired t-tests were performed to identify changes in the tibialis anterior tendon transfer group. For data not normally distributed (Kolmogorov-Smirnov test), corresponding Mann-Whitney U and Wilcoxon signed-rank tests were used. Factors associated with surgical outcome were normally distributed and analyzed using Pearson product-moment correlation coefficient. A p value less than 0.05 was considered significant.
Results
Strength
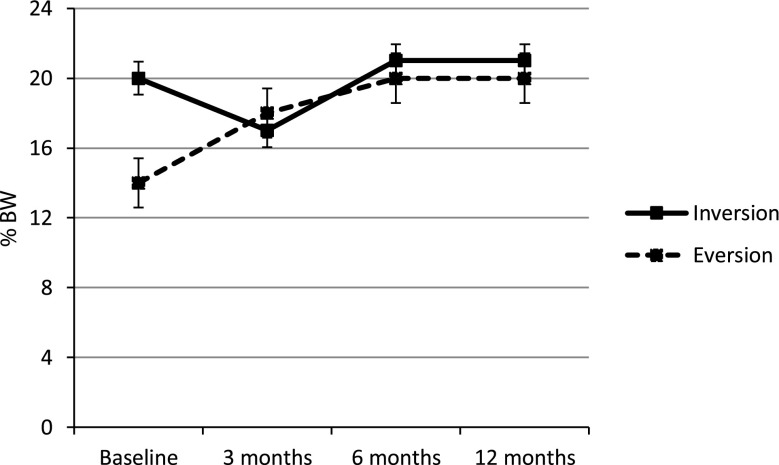
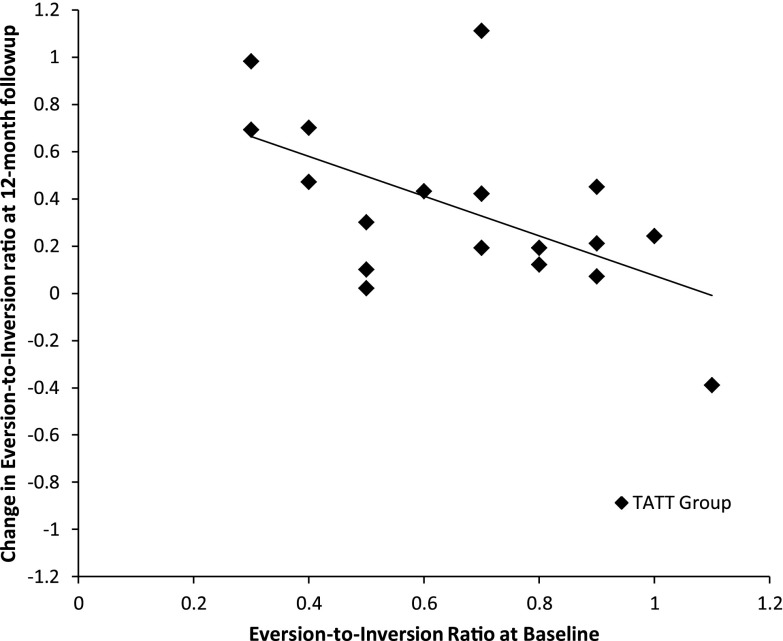
Before surgery, eversion strength was weaker in the tibialis anterior tendon transfer group compared with the control group (mean difference, −11% BW; 95% CI, −16% to −7%; p < 0.001), whereas inversion strength was not significantly different between groups (Table 2). Additionally, there was an imbalance of eversion-to-inversion strength in the tibialis anterior tendon transfer group compared with the nontibialis anterior tendon transfer group (mean difference, −44% BW; 95% CI, −58% to −29%; p < 0.001). Three months after surgery, a decline in inversion strength (mean difference, 3% ± 0% BW) and an improvement in eversion strength were observed (mean difference, 4% ± −2% BW), such that imbalance of eversion-to-inversion strength no longer was different between groups (Fig. 2). Between 3 and 6 months after surgery, recovery of inversion strength was observed (mean difference, 1% ± 0% BW), while additional gains in eversion strength also were seen (mean difference, 2% ± 0% BW) and the ratio of eversion-to-inversion strength remained similar between groups. Improvements were maintained at 12 months after surgery. Children with greater imbalance of eversion-to-inversion strength at baseline showed greater improvement 12 months after surgery (r = −0.634; p = 0.004) (Fig. 3).
Table 2.
Outcome measures
| Outcome measure | Baseline | 3 months | 6 months | 12 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-TATT group (n = 12) | TATT group (n = 20) | p value | Non-TATT group (n = 12) | TATT group (n = 18) | p value | Non-TATT group (n = 12) | TATT group (n = 18) | p value | Non-TATT group (n = 12) | TATT group (n = 18) | p value | |
| Foot alignment | ||||||||||||
| Dimeglio score (points) | 2.5 (2)a | 4.5 (3)a | 0.001b,* | 2 (2)a | 4.2 (1.6) | 0.009b,* | 2 (1)a | 4.6 (2) | 0.001b,* | 3 (1)a | 5 (2)a | <0.001b,* |
| Foot Posture Index© | 4.0 (3.4) | 0.2 (3.5) | 0.005 | 4.7 (2.6) | 2.1 (2.3) | 0.009* | 4.2 (2.9) | 1.6 (2.6) | 0.003* | 4.8 (2.9) | 1.2 (2.3) | <0.001* |
| Strength (% BW) | ||||||||||||
| Inversion | 23 (6) | 20 (4) | 0.288 | 20 (4) | 17 (4) | 0.023* | 21 (4) | 21 (5) | 0.859 | 24 (6) | 21 (5) | 0.159 |
| Eversion | 25 (6) | 14 (6) | <0.001* | 23 (6) | 18 (4) | 0.008* | 22 (5) | 20 (4) | 0.472 | 24 (5)a | 20 (6)a | 0.017b,* |
| Dorsiflexion | 30 (7) | 27 (8) | 0.271 | 25 (8)a | 25 (6) | 0.687b | 25 (7) | 26 (5) | 0.866 | 26 (6) | 23 (8) | 0.392 |
| Plantar flexion | 65 (13) | 59 (13) | 0.238 | 59 (12) | 57 (14) | 0.746 | 61 (11) | 66 (16) | 0.324 | 65 (11) | 65 (14) | 0.800 |
| Eversion/inversion ratio | 1.1 (0.13) | 0.66 (0.22) | <0.001* | 1.13 (0.24) | 1.08 (0.23) | 0.553 | 1.05 (0.16) | 1.00 (0.19) | 0.407 | 1.09 (0.20) | 1.02 (0.27) | 0.412 |
| Function | ||||||||||||
| Disease-specific instrument (points) | 14 (3) | 18 (5) | 0.008* | 14 (4) | 17 (4) | 0.099 | 13 (2) | 15 (4) | 0.055 | 12 (2) | 14 (3) | 0.076 |
Values are expressed as mean, with SD in parentheses, unless stated otherwise; aMedian (IQR); bMann-Whitney U test; *p < 0.05.
Fig. 2.
A graph shows the eversion and inversion strength of the tibialis anterior tendon transfer group at baseline and during 12 months after tibialis anterior tendon transfer. There was an initial decline of inversion strength at 3 months after surgery and subsequent recovery and maintenance at 6 and 12 months after surgery.
Fig. 3.
A graph shows the correlation of change in eversion-to-inversion ratio during 12 months to baseline eversion-to-inversion ratio in the tibialis anterior tendon transfer group. Worse imbalance of inversion-to-eversion ratio at baseline correlated with greater improvement in balance after tibialis anterior tendon transfer surgery (r = −0.63; p = 0.004). TATT = tibialis anterior tendon transfer.
Dorsiflexion and plantar flexion strength were similar at baseline and remained so at 3, 6, and 12 months after surgery.
In the five patients (five feet) who underwent additional posterior lengthening procedures, plantar flexion strength was maintained between baseline and 12 months followup (mean difference, +9% BW).
Plantar Loading
At baseline, the tibialis anterior tendon transfer group had lower peak pressure and maximum mean pressure beneath the medial side of the foot (p < 0.043) and the total contact area was less compared with that of the nontibialis anterior tendon transfer group (mean difference, −8 cm2; 95% CI, −16 to −1; p = 0.033). There were no differences between groups at 3, 6, and 12 months after surgery (Table 3).
Table 3.
Plantar pressure
| Variable | Baseline | 3 months | 6 months | 12 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-TATT group (n = 12) | TATT group (n = 20) | p value | Non-TATT group (n = 10) | TATT group (n = 17) | p value | Non-TATT group (n = 12) | TATT group (n = 17) | p value | Non-TATT group (n = 12) | TATT group (n = 18) | p value | |
| Contact area (cm2) | 66 (11) | 58 (10) | 0.033* | 65 (12) | 62 (9) | 0.376 | 69 (11) | 65 (10) | 0.286 | 73 (10) | 69 (10) | 0.251 |
| Peak pressure (kPa) | ||||||||||||
| Total | 200 (55) | 157 (54) | 0.036* | 188 (59) | 156 (49) | 0.145 | 188 (60) | 196 (75) | 0.763 | 221 (115) | 226 (67) | 0.887 |
| Medial | 185 (55) | 129 (33) | 0.006* | 164 (55) | 134 (35) | 0.098 | 179 (53) | 164 (72) | 0.546 | 175 (56) | 189 (67) | 0.626 |
| Lateral | 165 (56) | 151 (52) | 0.468 | 154 (62) | 127 (73)a | 1 | 154 (50) | 181 (62) | 0.215 | 152 (90) | 204 (60) | 0.570 |
| Maximum mean pressure (kPa) | ||||||||||||
| Total | 69 (13) | 63 (21) | 0.374 | 73 (26) | 61 (17) | 0.138 | 67 (18) | 73 (23) | 0.497 | 68 (13) | 74 (21) | 0.524 |
| Medial | 63 (14) | 51 (14) | 0.025* | 59 (24) | 50 (10) | 0.184 | 64 (19) | 61 (25) | 0.642 | 63 (11) | 59 (21) | 0.475 |
| Lateral | 55 (13) | 60 (21) | 0.423 | 59 (24) | 48 (31)a | 0.880 | 50 (9) | 65 (18) | 0.012* | 57 (14) | 67 (17) | 0.122 |
TATT = tibialis anterior tendon transfer; values are expressed as mean (standard deviation) unless stated; a median (interquartile range); *p < 0.05.
ROM
At baseline, Dimeglio scores [4] were higher in the tibialis anterior tendon transfer group (median difference, 2; 95% CI, 1–3; p = 0.001) and remained so at 3 (median difference, 1; 95% CI, 0–3; p = 0.009), 6 (median difference, 2; 95% CI, 1–3; p = 0.001), and 12 (median difference, 2; 95% CI, 1–3; p < 0.001) months after surgery (Table 2). At baseline, the degree of abduction and dorsiflexion were less in the tibialis anterior tendon transfer group (p = 0.05, p < 0.001) and remained so at 3 (p = 0.02, p = 0.007), 6 (p = 0.01, p = 0.003), and 12 (p = 0.002, p = 0.02) months after surgery. In the five patients (five feet) who underwent additional posterior lengthening procedures, an improvement in maximum dorsiflexion was seen between baseline and 3 months (mean difference, 15° ± 2°). A decline was observed between 3 and 6 months (mean difference, −3° ± 1°) and between 6 and 12 months (mean difference, −3° ± 3°) after surgery. The 15 patients (15 feet) who did not undergo posterior lengthening showed a similar degree of dorsiflexion between baseline (15° ± 7°) and 12 months after surgery (17° ± 6°) (p = 0.137).
Foot Alignment
At baseline, the Foot Posture Index© identified a more supinated foot posture in the tibialis anterior tendon transfer group (mean difference, −3.9; 95% CI, −6.4 to −1.3; p = 0.005) than in the nontibialis anterior tendon transfer group. This difference remained at 3 (mean difference, −2.6; 95% CI, −4.5 to −0.7; p = 0.009), 6 (mean difference, −3.2; 95% CI, −5.3 to −1.2; p = 0.003), and 12 (mean difference, −3.7; 95% CI, −5.6 to −1.8; p < 0.001) months after surgery (Table 2).
Function and Satisfaction
At baseline, the tibialis anterior tendon transfer group scored higher (worse) on the disease-specific instrument for clubfoot than the nontibialis anterior tendon transfer group (mean difference, 5; 95% CI, 1–8; p = 0.008). Scores no longer were significantly different between groups at 3, 6, and 12 months after surgery (Table 2).
Quality of Life
The Infant Toddler Quality of Life Questionnaire™ [18] was not different between groups for any domain at baseline (p > 0.311). Overall health was perceived as higher in the tibialis anterior tendon transfer group than in the nontibialis anterior tendon transfer group at 3 months after surgery (median difference, 15; 95% CI, 0–15; p = 0.01) but was comparable at 6 (p = 0.30) and 12 (p = 0.90) months after surgery. The physical abilities of the tibialis anterior tendon transfer group were perceived to be less at 6 months after surgery (median difference, 0; 95% CI, −3 to 0; p = 0.025) but had recovered by 12 months after surgery (p = 0.765). All other domains were not significantly different after surgery.
Adverse Events
Two patients experienced relapse after tibialis anterior tendon transfer during the followup period. Both had undergone Ponseti serial casting for structural deformity before surgery and neither had posterior lengthening as part of their tibialis anterior tendon transfer procedure. The first patient had relapses of equinus deformity at 6 and 12 months after surgery. This was the only patient who had a decline in eversion-to-inversion balance after tibialis anterior tendon transfer. The second patient had a relapse of equinus and adduction deformity at 6 months after tibialis anterior tendon transfer. All relapses were treated with additional Ponseti serial casting followed by night bracing with a knee-ankle-foot orthosis. There were no relapses in the nontibialis anterior tendon transfer group during the 12-month followup period. There were no other adverse events.
Discussion
Tibialis anterior tendon transfer has been documented as a treatment option for congenital talipes equinovarus since the 1940s [7] and forms part of the Ponseti management [17]. The current evidence base for tibialis anterior tendon transfer includes a cadaveric biomechanical study [9], retrospective chart reviews [14, 23], a cross-sectional trial [6], or cohorts who had previous surgery [12]. However, prospective evidence of efficacy is lacking. In the context of a prospective, comparative study, we assessed strength, plantar loading, ROM, foot alignment, function, satisfaction, and quality of life in patients with clubfoot that recurred after Ponseti casting who met indications for tibialis anterior tendon transfer surgery. We compared these patients with a group of patients with clubfoot treated with casting but whose deformity did not recur (therefore who were not indicated for tibialis anterior tendon transfer surgery). We also compared the abovementioned end points before and after surgery for the tendon transfer group.
There are some limitations to this study. First, our trial is limited by small patient numbers; larger trials will improve precision of the findings. Second, the 12-month followup might not have captured all recurrences; longer followup will be important. Third, although all patients reported compliance with the Ponseti technique, this cannot be objectively confirmed. Fourth, although blinding of the assessor was not possible (owing to postoperative scars), blinding in future trials will reduce potential bias. Finally, 14 of the 20 patients required Ponseti serial casting before surgery. These patients may have had reduced strength and altered gait when casts were removed. To minimize these effects, but without compromising gains in ROM, casts were removed at least 1 week before baseline assessment.
Consistent with our findings, improvements of eversion strength after tibialis anterior tendon transfer surgery have been reported, however this has not been documented after Ponseti treatment [6, 12, 23]. In a retrospective review of 55 patients (71 congenital talipes equinovarus feet), Kuo et al. [12] noted an improvement of eversion strength of 1.5 grades according to the Jones classification at an average of 8.8 years after tibialis anterior tendon transfer surgery. Thompson et al. [23] reviewed muscle balance after tibialis anterior tendon transfer surgery using an independent assessment that graded postoperative muscle balance as good (full restoration), fair (partial restoration), or poor (no improvement). At 4.3 years after tibialis anterior tendon transfer surgery, they found 87% had good results, 13% had fair results, and 0% had poor results. To our knowledge, our study is the first to quantify muscle strength balance using a hand-held dynamometer in patients with congenital talipes equinovarus. Hand-held dynamometry has superior reliability and accuracy compared with manual muscle testing [5], has proven validity in other pediatric populations [2], and can be used in children as young as 2 years [21]. We found that the significant imbalance of eversion-to-inversion strength at baseline in the tibialis anterior tendon transfer group was no longer present at 3 months after surgery. However, the improvement appears to be partially attributable to a transient weakness of inversion after surgery. At 6 months after surgery, recovery of inversion strength was observed and muscular balance was achieved through ongoing improvement in eversion strength.
To our knowledge, our study is the first to compare plantar pressure outcomes between children with congenital talipes equinovarus who did and did not undergo tibialis anterior tendon transfer surgery. Tulchin et al. [24] reported plantar pressures in 30 children (37 feet) with congenital talipes equinovarus before and after tibialis anterior tendon transfer compared with healthy age-matched controls. After surgery, they found normalization of contact area and contact time in the hindfoot and a medial shift in peak pressure from the lateral forefoot to the first metatarsal. Our study showed similar significant differences between tibialis anterior tendon transfer and nontibialis anterior tendon transfer groups at baseline. Improvements in medial peak pressure, maximum mean pressure, and contact area observed 3 months after surgery were sustained at the 6- and 12-month followups.
Dimeglio scores were significantly different at baseline between the two groups and did not improve significantly after surgery. Previous studies have noted improvements in passive ROM after tibialis anterior tendon transfer; however, many patients in these trials had undergone additional major surgical procedures, including joint releases and osteotomies [12, 13]. It is unknown whether the preexisting loss in ROM in the tibialis anterior tendon transfer group is a result of the muscular imbalance or if it represents a more severe form of congenital talipes equinovarus.
The Foot Posture Index© is a screening tool for measuring standing static foot alignment [20]. It has not been used previously in the congenital talipes equinovarus population. The Foot Posture Index© identified a significant difference between groups at baseline and therefore may be a useful tool in screening children for tibialis anterior tendon transfer surgery. However, the ongoing significant differences after surgery did not reflect the improvements seen in plantar pressure and strength, suggesting that the Foot Posture Index© is not sensitive enough to detect change after this surgery or that an underlying deformity may persist in this population.
To our knowledge, ours is the first study to explore the use of the disease-specific instrument for clubfoot as a reassessment tool in children before and after tibialis anterior tendon transfer. We found that children awaiting tibialis anterior tendon transfer had worse function and satisfaction than children not undergoing tibialis anterior tendon transfer surgery. Dietz et al. [3] reported that children who previously underwent joint-sparing surgery had better disease-specific instrument outcomes than children who underwent joint invasive surgery. Total disease-specific instrument scores of the tibialis anterior tendon transfer group at 12-month followup were similar to those of the joint-sparing surgery group reported by Dietz et al. (p = 0.379).
Quality of life in children in the tibialis anterior tendon transfer and nontibialis anterior tendon transfer groups were not significantly better compared with previously published norm data of children of the same age (p > 0.074) [18]. However, the Infant Toddler Quality of Life Questionnaire™ does not interrogate for advanced gross motor skills, such as high-intensity exercise, and may have resulted in a ceiling effect and thus no difference between the groups. Measures which include high-functioning activities may provide a more accurate assessment of function in this population.
Two participants in the tibialis anterior tendon transfer group experienced relapse during the followup period. Although we did not think either patient required additional posterior lengthening procedures, it is possible that relapse may have been related to an underlying equinus deformity. Undiagnosed neuromuscular disorders have been cited as a cause for relapse after tibialis anterior tendon transfer but were not identified in either of these patients [14].
We report a 12-month prospective clinical trial evaluating the outcomes of 20 children with congenital talipes equinovarus undergoing tibialis anterior tendon transfer compared with 12 age-matched children with congenital talipes equinovarus who were treated with Ponseti casting and who did not meet indications for tibialis anterior transfer. Patients who underwent tibialis anterior tendon transfer surgery showed dynamic imbalance and reduced function before surgery compared with patients who did not require tibialis anterior tendon transfer. At 12 months, these outcomes were not significantly different between groups. Persistent differences in foot alignment and passive range of movement, and documentation of two recurrences, suggest that an underlying deformity may be present in this population. Larger prospective trials using reliable and valid outcome measures are required to accurately document mid- and long-term outcomes of this population.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was performed at The Children’s Hospital at Westmead, Westmead, Australia.
References
- 1.Burns J, Crosbie J, Hunt A, Ouvrier R. The effect of pes cavus on foot pain and plantar pressure. Clin Biomech (Bristol, Avon). 2005;20:877–882. doi: 10.1016/j.clinbiomech.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Burns J, Ouvrier R, Estilow T, Shy R, Laura M, Pallant JF, Lek M, Muntoni F, Reilly MM, Pareyson D, Acsadi G, Shy ME, Finkel RS. Validation of the Charcot-Marie-Tooth disease pediatric scale as an outcome measure of disability. Ann Neurol. 2012;71:642–652. doi: 10.1002/ana.23572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dietz FR, Tyler MC, Leary KS, Damiano PC. Evaluation of a disease-specific instrument for idiopathic clubfoot outcome. Clin Orthop Relat Res. 2009;467:1256–1262. doi: 10.1007/s11999-008-0700-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dimeglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop. 1995;4:129–136. doi: 10.1097/01202412-199504020-00002. [DOI] [PubMed] [Google Scholar]
- 5.Escolar DM, Henricson EK, Mayhew J, Florence J, Leshner R, Patel KM, Clemens PR. Clinical evaluator reliability for quantitative and manual muscle testing measures of strength in children. Muscle Nerve. 2001;24:787–793. doi: 10.1002/mus.1070. [DOI] [PubMed] [Google Scholar]
- 6.Farsetti P, Caterini R, Mancini F, Potenza V, Ippolito E. Anterior tibial tendon transfer in relapsing congenital clubfoot: long-term follow-up study of two series treated with a different protocol. J Pediatr Orthop. 2006;26:83–90. doi: 10.1097/01.bpo.0000188999.21427.fb. [DOI] [PubMed] [Google Scholar]
- 7.Garceau GJ. Anterior tibial tendon transposition in recurrent congenital club-foot. J Bone Joint Surg Am. 1940;22:932–936. [PubMed] [Google Scholar]
- 8.Garceau GJ, Palmer RM. Transfer of the anterior tibial tendon for recurrent club foot: a long-term follow-up. J Bone Joint Surg Am. 1967;49:207–231. [PubMed] [Google Scholar]
- 9.Hui JH, Goh JC, Lee EH. Biomechanical study of tibialis anterior tendon transfer. Clin Orthop Relat Res. 1998;349:249–255. doi: 10.1097/00003086-199804000-00031. [DOI] [PubMed] [Google Scholar]
- 10.Ippolito E, Farsetti P, Caterini R, Tudisco C. Long-term comparative results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg Am. 2003;85:1286–1294. doi: 10.2106/00004623-200307000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Ippolito E, Ricciardi-Pollini PT, Tudisco C, Ronconi P. The treatment of relapsing clubfoot by tibialis anterior transfer underneath the extensor retinaculum. Ital J Orthop Traumatol. 1985;11:171–177. [PubMed] [Google Scholar]
- 12.Kuo KN, Hennigan SP, Hastings ME. Anterior tibial tendon transfer in residual dynamic clubfoot deformity. J Pediatr Orthop. 2001;21:35–41. doi: 10.1097/01241398-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Lampasi M, Bettuzzi C, Palmonari M, Donzelli O. Transfer of the tendon of tibialis anterior in relapsed congenital clubfoot: long-term results in 38 feet. J Bone Joint Surg Br. 2010;92:277–283. doi: 10.1302/0301-620X.92B2.22504. [DOI] [PubMed] [Google Scholar]
- 14.Masrouha KZ, Morcuende JA. Relapse after tibialis anterior tendon transfer in idiopathic clubfoot treated by the Ponseti method. J Pediatr Orthop. 2012;32:81–84. doi: 10.1097/BPO.0b013e31823db19d. [DOI] [PubMed] [Google Scholar]
- 15.Menz HB. Analysis of paired data in physical therapy research: time to stop double-dipping? J Orthop Sports Phys Ther. 2005;35:477–478. doi: 10.2519/jospt.2005.0108. [DOI] [PubMed] [Google Scholar]
- 16.Ponseti I, Morcuende JA, Mosca V, Pirani S, Dietz F, Herzenberg JE, Weinstein S, Penny N, Steenbeek M. Clubfoot: Ponseti Management. Ed 2. In: Staheli L, ed. Seattle, WA: Global-HELP Organization; 2005.
- 17.Ponseti IV, Smoley EN. Congenital club foot: the results of treatment. J Bone Joint Surg Am. 1963;45:261–344. [Google Scholar]
- 18.Raat H, Landgraf JM, Oostenbrink R, Moll HA, Essink-Bot ML. Reliability and validity of the Infant and Toddler Quality of Life Questionnaire (ITQOL) in a general population and respiratory disease sample. Qual Life Res. 2007;16:445–460. doi: 10.1007/s11136-006-9134-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Redmond A. The Foot Posture Index (FPI-6). Available at: http://www.leeds.ac.uk/medicine/FASTER/fpi.htm. Accessed September 10, 2010.
- 20.Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin Biomech (Bristol, Avon). 2006;21:89–98. [DOI] [PubMed]
- 21.Rose KJ, Burns J, Ryan MM, Ouvrier RA, North KN. Reliability of quantifying foot and ankle muscle strength in very young children. Muscle Nerve. 2008;37:626–631. doi: 10.1002/mus.20961. [DOI] [PubMed] [Google Scholar]
- 22.Roye B, Vitale MG, Gelijns AC, Roye DP., Jr Patient-based outcomes after clubfoot surgery. J Pediatr Orthop. 2001;21:42–49. doi: 10.1097/01241398-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Thompson GH, Hoyen HA, Barthel T. Tibialis anterior tendon transfer after clubfoot surgery. Clin Orthop Relat Res. 2009;467:1306–1313. doi: 10.1007/s11999-009-0757-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tulchin K, Jeans KA, Karol LA, Crawford L. Plantar pressures and ankle kinematics following anterior tibialis tendon transfers in children with clubfoot. J Foot Ankle Res. 2012;5(suppl 1):O32. doi: 10.1186/1757-1146-5-S1-O32. [DOI] [PubMed] [Google Scholar]