Abstract
Background
Periprosthetic fractures can occur both intraoperatively and postoperatively with implantation of cementless tapered stems.
Questions/purposes
In a large cohort of patients receiving cementless, proximally hydroxyapatite-coated femoral implants, we answered the following questions: What was the incidence of intraoperative and postoperative fractures associated with the implant? What were the fracture patterns as classified by the Vancouver classification system? Did the Vancouver classification represent the fracture patterns found? How were the fractures treated and what were the treatment outcomes; that is, how many fractures healed and did the stems osseointegrate?
Methods
We evaluated 1039 hips (932 patients) from three prospective studies. The hips were divided into three groups: no fractures, intraoperative fractures, and postoperative fractures. Demographic differences among the groups were noted. Postoperative fractures were classified using the Vancouver classification system. We judged stem stability using Engh’s criteria and fracture union was determined by the treating surgeon and confirmed by the authors.
Results
We identified 58 periprosthetic fractures in the 1039 hips (5.6%): 38 intraoperative (3.7%) and 20 postoperative (1.9%). Eleven of the postoperative fractures were classifiable by the original Vancouver classification system and nine were of the newly described “clamshell” variety, not classifiable by this system. No intraoperative fractures extended below the lesser trochanter. Twenty-five of these fractures were treated with a single cable or cerclage wire. The remaining received no specific treatment. Of the 20 postoperative fractures, five were treated nonoperatively. All stems osseointegrated.
Conclusions
Both intraoperative and postoperative fractures can be managed with success when the stem is stabilized or found to be osseointegrated. An adjustment to the Vancouver classification is suggested to include the clamshell fracture, which has not been previously described.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
The reported frequency of fracture around cementless proximally fixed stems is between 0.4% and 11%, and for the most part, those data derive from small studies (100–436 patients) [4, 10–13, 15]. The much larger national registries focus on primarily cemented femoral implants, reporting fracture frequencies of 0.4% to 2.5% [2, 8]. Intraoperative fractures with cementless implants have been reported only rarely, and some of these data are much older. Two reports show the fracture risk to be 4% and 15%, the latter being a 1987 publication [1, 7].
In a large number of patients receiving similar cementless, proximally hydroxyapatite (HA)-coated femoral implants, we posed the following questions: (1) What was the incidence of intraoperative and postoperative fractures associated with the implant? (2) What were the fracture patterns as classified by the Vancouver classification system? (3) Did the Vancouver classification represent the fracture patterns found? (4) How were the fractures treated and what were the treatment outcomes; that is, how many fractures healed and did the stems osseointegrate?
Patients and Methods
All data were retrospectively gathered from three prospective studies (involving Omnifit®, ABC/Trident®, and Trident® X3®; Stryker Orthopaedics, Mahwah, NJ, USA) in which a double-wedged, tapered, TiAl6V4 implant, whose upper 1/3 was coated with HA, was used. The pooled data were used to identify the incidence and classification of intraoperative and postoperative periprosthetic fracture in a large cohort of cementless proximally fixed femoral stems. Patients were included in each study provided they met the study specific inclusion criteria. All studies required patients to be skeletally mature, had obesity restrictions, excluded patients with active or suspected infections around the joint, and included patients who were willing and able to comply with the postoperative schedule and who agreed to participate in the study by signing a study-specific, institutional review board-approved informed consent form. The older Omnifit® HA study allowed diagnoses of rheumatoid arthritis and revision arthroplasty while the other studies were restricted to primary noninflammatory degenerative joint disease diagnoses (Table 1). All three studies shared similarities: an intraoperative complication form; and preoperative and postoperative Harris hip score clinical data forms collected at 6 weeks, 6 months, 1 year, and annually through 5 years and at protocol-specified times beyond 5 years. The studies differed in length of followup and acetabular component usage, and the most recent study (X3®) utilized a femoral implant with identical metallurgy and geometry as the other two studies but differed in that beneath the HA coating was a roughened layer of arc-deposited Ti. All stems were grit blasted before the application of the HA and/or the arc deposit.
Table 1.
Study demographics
| Variable | Omnifit® HA | ABC/Trident® | Trident® X3® |
|---|---|---|---|
| Number of men/women | 113/113 | 309/176 | 105/116 |
| Number of patients/hips | 226/262 | 485/537 | 221/240 |
| Followup (years)* | 15.3 (0–22.6) | 7.8 (0.1–12.4) | 4 (0–7) |
| Age at surgery (years)† | 51.6 ± 10.8 | 53.4 ± 10.4 | 62.0 ± 8.8 |
| Diagnosis (%) | |||
| Osteoarthritis | 68 | 81 | 90 |
| Traumatic arthritis | 4 | 3 | 1 |
| Avascular necrosis | 12 | 13 | 8 |
| Revision | 7 | NA | NA |
| Rheumatoid arthritis | 4 | NA | NA |
| Congenitally dysplastic hip | 4 | 0 | 0 |
| Other‡ | 1 | 3 | 1 |
| Number of fractures | 18 (6.9%) | 19 (3.5%) | 1 (0.4%) |
* Values are expressed as mean, with range in parentheses; †values are expressed as mean ± SD; ‡other diagnoses include less than 2% each of slipped capital femoral epiphysis, femoral fracture, failed fracture fixation, and diastrophic variant; NA = not applicable.
Each of the three studies underwent yearly monitoring by the study sponsor (Stryker Orthopaedics). During those audits, complication and clinical forms were validated relative to patient hospital and outpatient records. Any discrepancies were reconciled through the operating physician.
In this combined study, we evaluated 1039 hips in 932 patients. The hips were divided into three groups: no fractures (n = 982; mean followup, 8.3 years; range, 0–22.3 years); intraoperative fractures (n = 38; mean followup, 11.4 years; range, 0–20.8 years); and postoperative fractures (n = 20; mean followup, 8.7 years; range, 0–21.0 years) (Table 2). Some important differences existed among the three groups: the no fracture group had more patients with osteoarthritis; the intraoperative fracture group had fewer men and a lower mean BMI; and the postoperative fracture group had a higher mean age.
Table 2.
Demographics and fracture distribution group
| Variable | No fracture group | Intraoperative fracture group | Postoperative fracture group | p value |
|---|---|---|---|---|
| Mean age (years) | 55 | 51 | 58 | 0.025 |
| Sex (% male) | 58 | 34 | 58 | 0.017 |
| Diagnosis (%) | < 0.001 | |||
| Osteoarthritis | 80 | 68 | 53 | |
| Traumatic arthritis | 3 | 3 | 5 | |
| Avascular necrosis | 11 | 21 | 16 | |
| Revision | 1 | 3 | 16 | |
| Rheumatoid arthritis | 1 | 0 | 10 | |
| Congenitally dysplastic hip | 1 | 5 | 0 | |
| Other* | 3 | 0 | 0 | |
| Mean BMI | 28 | 26 | 28 | 0.014 |
| Number of patients | ||||
| Omnifit® study | 235 | 18 | 9 | |
| ABC/Trident® study | 509 | 19 | 10 | |
| Trident® X3® study | 238 | 1 | 1 | |
| Total | 982 | 38 | 20 | |
* Other included 1% or less each of diastrophic variant, femoral fracture, failed fracture fixation, and slipped capital femoral epiphysis.
All data regarding intraoperative fractures were obtained from the intraoperative data forms. No specific indications for surgery were established prospectively. The operating surgeons determined whether to cerclage cable/wire the crack or treat it without fixation. All patients who were noted to have intraoperative fractures were evaluated radiographically and the implant’s stability was assessed using the criteria developed by Engh et al. [6]. Our preferred approach to intraoperative cracks or fractures is to remove the implant, place one cerclage cable above the lesser trochanter, and reinsert the implant. Any patient who sustained a postoperative fracture as determined by the complication form entry was also evaluated radiographically, and the unrevised stem’s stability was determined by the criteria of Engh et al. [6]. The treatment of postoperative fractures was more complex. Osseointegrated stems (stable stems) associated with minimally displaced fractures were sometimes treated with no operative measures such as protected weightbearing for 6 weeks. Markedly displaced fractures, even with osseointegrated stems, were frequently operated on using multiple cables or wires with and without adjunctive plate fixation. Finally, fractures associated with unstable stems were always treated operatively with stem removal, fracture reconstruction, and new stem insertion. Postoperatively, all patients were instructed to limit weightbearing by using crutches or a walker for 6 weeks.
Operating surgeon’s notes were used to determine healing of fractures, which was confirmed by the authors. Any demographic differences among the three fracture groups were noted. All postoperative fractures were classified using the original Vancouver classification system [5] and a recently modified version [14] (Table 3).
Table 3.
Comparison of the original Vancouver classification system of periprosthetic fractures and our modified version*
| Vancouver classification | Description | Our modified Vancouver classification | Description |
|---|---|---|---|
| ATG | Fracture in greater trochanteric region | TG | Same as original |
| ATL | Fracture in lesser trochanteric region | TL | Same as original |
| Pseudo ATL/new B†2 | Fracture of the lesser trochanter, includes a segment of the proximal medial femoral cortex, is associated with destabilization of the stem. and requires early reintervention | A1 | Fracture of medial cortex that includes the residual neck, calcar, and lesser trochanter and is displaced medially, with a well-fixed stem |
| A2 | Fracture of medial cortex that includes the residual neck, calcar, and lesser trochanter and is displaced medially, with a loose stem | ||
| B1 | Fracture around stem or just below it, with a well-fixed stem | B1 | Same as original |
| B2 | Fracture around stem or just below it, with a loose stem but good proximal bone stock | B2 | Same as original |
| B3 | Fracture around stem or just below it, with poor-quality or severely comminuted proximal bone | B3 | Same as original |
| C | Fracture well below prosthesis | C | Same as original |
Categorical variables were summarized as count and percentage, and the chi-square test was used to test the distribution difference among the three groups. Continuous numeric variables were summarized as mean and SD, and the Kruskal-Wallis test was used to compare population location parameters among the three groups. All statistical tests were two-sided with a significance level of 0.05. We used SAS/STAT® Version 9.1.3 software (SAS Institute Inc, Cary, NC, USA) for all data analyses.
Results
Fifty-eight fractures were identified among the 1039 hips, for an overall incidence of 5.6%. Of those, 38 (3.7%) were intraoperative fractures and 20 (1.9%) occurred postoperatively (mean, 3.3 years; range, 0.2–11.1 years). There were differences in the incidence of intraoperative fractures among the three studies, the oldest (Omnifit®) having the highest incidence (6.9%) (Table 1). All intraoperative fractures were small, and none extended below the lesser trochanter. All occurred either during broaching of the canal or during stem insertion.
Nine of the 20 postoperative fractures (45%) were not classifiable under the original Vancouver classification system [5] but with recent modifications [14] would have been called pseudo ATL or new B2 (Table 4). Our postoperative fractures also included nine B1 and two C fractures. The age at fracture was not different among the three fracture types we identified. Eleven of 20 postoperative fractures (55%) occurred within the first year postoperatively. The pseudo ATL/new B2 fractures occurred early, with six of nine occurring within the first 2 months after surgery compared to three of nine B1 fractures. Also, the pseudo ATL/new B2 fractures occurred more frequently in women and in patients with poorer bone.
Table 4.
Demographics of pseudo ATL and B1 fractures
| Variable | Pseudo ATL | B1 |
|---|---|---|
| Number of fractures | 9 | 9 |
| Number of men/women | 3/6 | 6/3 |
| Dorr bone type (number of fractures) | A = 2, B = 3, C = 4 | A = 5, B = 4, C = 0 |
| Stems removed (number of fractures) | 5 (all loose) | 3 (none loose) |
Twenty-five of the 38 intraoperative fractures (66%) were treated with a single cable or cerclage wire. The remaining (13 of 38, 34%) received no specific treatment. One stem subsided 5 mm but has remained stable for 16 years and at latest radiographic review was judged to have been osseointegrated. None of the remaining 37 stems have subsided or loosened or been revised. Of the 20 postoperative fractures, five were treated nonoperatively, three in the pseudo ATL/new B2 group, one in the B1 group, and one in the C group (Table 5). None of these five femoral fractures managed nonoperatively underwent subsequent surgery, and all were radiographically osseointegrated at latest followup. Of the 15 postoperative femoral fractures treated surgically, seven stems initially were retained and eight were revised. Two of the removed stems were secure but removed to address the fracture. One stem, initially retained, was eventually removed to manage a nonunion.
Table 5.
Postoperative fracture distribution by Vancouver classification and fracture treatment
| Original Vancouver classification | Number of fractures | Our modified Vancouver classification | Number of fractures | Age at fracture (years)* | ORIF (number of fractures) | Nonoperative (number of fractures) | Loose stems (number of fractures) | Stems removed (number of fractures) |
|---|---|---|---|---|---|---|---|---|
| ATG | 0 | TG | 0 | NA | ||||
| ATL | 0 | TL | 0 | NA | ||||
| Pseudo ATL/new B†2 | 9 | A1 | 3 | 61 (39–75) | 6 | 3 | 6 | 6 |
| A2 | 6 | |||||||
| B1 | 9 | B1 | 9 | 57.7 (49–79) | 8 | 1 | 0 | 3 |
| B2 | 0 | B2 | 0 | NA | ||||
| B3 | 0 | B3 | 0 | NA | ||||
| C | 2 | C | 2 | 66.5 (59–74) | 1 | 1 | 0 | 0 |
* Values are expressed as mean, with range in parentheses; †modification added by Van Houwelingen and Duncan [14]; ORIF = open reduction and internal fixation; NA = not applicable.
Discussion
Periprosthetic fractures around the femoral components of THAs are a recognized complication of that procedure. We evaluated a large series of patients, all having a cementless femoral implant of identical metallurgy and geometry with an HA coating over the proximal 1/3 of the stems, by answering the following questions: (1) What was the incidence of both intraoperative and postoperative fractures associated with the implant? (2) What were the fracture patterns as classified by the Vancouver classification system? (3) Did the Vancouver classification represent the fracture patterns found? (4) How were the fractures treated and what were the treatment outcomes; that is, how many fractures healed and did the stems osseointegrate?
There are several limitations to our work. (1) The review was retrospective and involved gathering data from three studies with different followup intervals and different acetabular components. However, they all had used a femoral component of similar geometry, metallurgy, and HA coating. (2) We were also dependent on complication forms, filled out by participating surgeons, to identify patients sustaining periprosthetic fractures. All three studies were monitored by the sponsoring organization. Thorough audits were conducted annually to validate the complications and followup data by comparing those reports with data contained within the patient’s hospital and outpatient records. (3) Fracture classification was done by the authors using both complication forms supplied by the operating surgeon and postfracture radiographs. We did not control for intraoperative observer errors. We did match fracture patterns with published Vancouver classification. (4) Another limitation was the adequacy of the periprosthetic fracture classification system used. Even with recent modifications [14], it did not fully describe the fracture pattern seen in 45% of our postoperative fractures. (5) A final limitation was the differing intraoperative fracture rates in the three studies we used for our data. The decreasing rates with time reflect improved instrumentation, particularly the broach-implant relationship. Also, some surgeons participated in all three studies and this improvement is part of their learning curve in using both instruments and implants.
Our incidence of intraoperative fractures was 3.7%. This is a marked improvement over an early report by Fitzgerald et al. [7], who noted a 15% incidence when using a stem of identical geometry but made of cobalt-chromium with a beading ingrowth surface on its proximal 1/3. A similar-sized series reported by Berend et al. [1] had an incidence of 4% with a proximally wedged-shaped, tapered, and porous-coated implant. They also reported no failures associated with these fractures. All of these fractures were treated with intraoperative cerclage wires or cables compared to 2/3 of our fractures.
Our postoperative fracture incidence of 1.9% also compares favorably with published series of fractures around cementless femoral implants reporting rates of less than 1% to more than 10% [4, 10–13, 15]. We found three patterns of postoperative fractures: pseudo ATL/new B2 (n = 9), B1 (n = 9), and C (n = 2). Of the nine pseudo ATL/new B2 fractures, three with well-fixed stems were treated without surgery and six with loose stems required stem removal and fracture fixation, with all healing. Although no literature is available for comparison, similar intraoperative fractures were described by Berend et al. [1]. All were managed by removal of the implant, and the fractures were reduced and secured with single or multiple cerclage wires or cables followed by reinsertion of the implant. One stem subsided 17 mm and restabilized. No stem was revised or was radiographically loose. Eight of the nine B1 fractures were treated with open reduction and internal fixation, two requiring stem removal to secure the fracture. One B1 fracture went on to nonunion, requiring subsequent surgery with stem removal. One B1 fracture was managed without surgery and healed unremarkably. No other stems have been revised. The series of Corten et al. [3] included 36 B1 fractures. A lateral plate was used in 33 hips; in the three in which the medial comminution could not be reduced anatomically, an additional plate or strut was placed anteriorly. One patient had hardware failure at 3 weeks and was reoperated on; a second took 30 months to radiographically heal, with no additional surgery being needed. Our one nonunion, treated with strut grafts, appeared to have an unreduced medial cortex, as did the one hardware failure in the series of Corten et al. [3]. One of the two C fractures was treated closed, with subsequent healing and no stem exchange. The other required open reduction and internal fixation and also healed without stem revision. A study by Corten et al. [3] of 106 periprosthetic fractures include 11 Vancouver C fractures, five treated with the plate/cable plus anterior strut. All fractures healed, one requiring stem removal because of a persistent infection.
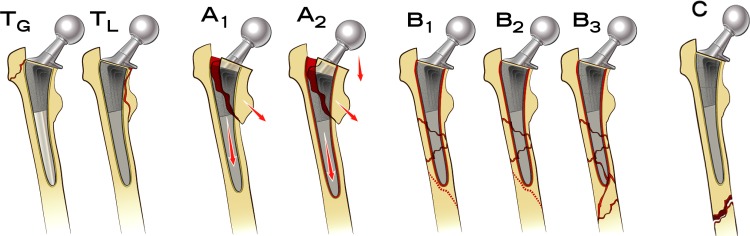
The proximal fractures we identified in nine of 20 hips we have labeled “clamshell” fractures (Fig. 1), which involve the lesser trochanters and proximal medial femoral cortex. This type of fracture was first described by Mallory et al. [9] in 1989 as an intraoperative fracture. There was then no mention of it occurring postoperatively. A followup report by Berend et al. [1] likewise only mentioned it as an intraoperative complication. More recently (2011), Van Houwelingen and Duncan [14] labeled it a pseudo ATL or New B2 fracture so as to not confuse it with an ATL fracture as described in the original Vancouver classification system. They do state that risk factors associated with this fracture pattern include using tapered, proximally coated, cementless stems in primary THAs. No literature describing this type of fracture is available for comparison of incidence, treatment, or outcome. Our experience differs from that described by Van Houwelingen and Duncan [14]. They suggest all these fractures require surgery, whereas three of ours were successfully managed nonoperatively. This has also been the experience of one of the authors (WNC) involving patients not in these studies, where the fracture has been noted early postoperatively, frequently with stem subsidence but with no surgery needed and the stem restabilizing, not requiring subsequent surgery. To categorize these clamshell fractures as new B2 does not allow for those fractures where the stem is stable. The pseudo ATL-label also does not differentiate between secure and nonsecure stems. Our suggestion is to change the classification system to accurately reflect these fractures as follows: (1) change the current ATL and ATG to TL and TG (the “T” designating the trochanter); (2) add a new A category to encompass this clamshell fracture, with A1 designating this fracture with a stable stem and A2 designating this fracture with an unstable stem; and (3) keep the B and C categories unchanged from the original Vancouver classification system (Table 3; Fig. 2). Thus, using our modification of the Vancouver classification, we found three A1, six A2, nine B1, and two C fractures (Table 5).
Fig. 1.

A radiograph shows the clamshell (pseudo ATL or new B2) fracture.
Fig. 2.
A proposed modification of the Vancouver classification is shown, now including the clamshell fracture. For definitions of the fracture types, see Table 3.
Periprosthetic fractures remain a serious complication of THA. Our data suggest these proximally fixed, tapered, HA-coated stem achieves excellent fixation in that we reported no B2 or B3 fractures. We did employ stem removal in our B1 fractures to assist in fracture management or to address a nonunion. A new early postoperative fracture described (A1/A2 by our modified Vancouver classification) is possibly related to an unrecognized intraoperative fracture and, we believe, directly related to the geometry of the tapered stem used. These fractures frequently came to stem removal and further surgery to manage the fractures.
Acknowledgments
The authors thank Molly M. Moore for assistance with manuscript preparation and Christopher M. Brown BFA, MS for providing illustrations.
Footnotes
Two of the authors certify that they (WNC, JAD) have received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Stryker Orthopaedics (Mahwah, NJ, USA). One author (MN) is an employee of Stryker Orthopaedics.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Indiana University Medical Center (Indianapolis, IN, USA), Sewickley Valley Hospital (Sewickley, PA, USA), and Stryker Orthopaedics (Mahwah, NJ, USA).
References
- 1.Berend KR, Lombardi AV, Jr, Mallory TH, Chonko DJ, Dodds KL, Adams JB. Cerclage wires or cables for the management of intraoperative fracture associated with a cementless, tapered femoral prosthesis: results at 2 to 16 years. J Arthroplasty. 2004;19(suppl 2):17–21. doi: 10.1016/j.arth.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Cook RE, Jenkins PJ, Walmsley PJ, Patton JT, Tobinson CM. Risk factors for periprosthetic fractures of the hip a survivorship analysis. Clin Orthop Relat Res. 2008;466:1652–1656. doi: 10.1007/s11999-008-0289-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corten K, Vanrykel F, Bellemans J, Reynders Frederix P, Simon JP, Broos PL. An algorithm for the surgical treatment of periprosthetic fractures of the femur around a well-fixed femoral component. J Bone Joint Surg Br. 2009;91:1424–1430. doi: 10.1302/0301-620X.91B11.22292. [DOI] [PubMed] [Google Scholar]
- 4.D’Angelo F, Murena L, Vulcano E, Zatti G, Cherubino P. Seven to twelve year results with Versys ET cementless stem: a retrospective study of 225 cases. Hip Int. 2010;20:81–86. doi: 10.1177/112070001002000112. [DOI] [PubMed] [Google Scholar]
- 5.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 6.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 7.Fitzgerald RH, Jr, Brindley GW, Kavanagh BF. The uncemented total hip arthroplasty. Clin Orthop Relat Res. 1988;235:61–66. [PubMed] [Google Scholar]
- 8.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857–865. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Mallory TH, Kraus TJ, Vaughn BK. Intraoperative femoral fractures associated with cementless total hip arthroplasty. Orthopedics. 1989;12:231–239. doi: 10.3928/0147-7447-19890201-06. [DOI] [PubMed] [Google Scholar]
- 10.McNally SA, Shepperd JA, Mann CV, Walczak JP. The results at nine to twelve years of the use of a hydroxyapatite-coated femoral stem. J Bone Joint Surg Br. 2000;82:378–382. doi: 10.1302/0301-620X.82B3.10114. [DOI] [PubMed] [Google Scholar]
- 11.Radl R, Aigner C, Hungerford M, Pascher A, Windhager R. Proximal femoral bone loss and increased rate of fracture with a proximally hydroxyapatite-coated femoral component. J Bone Joint Surg Br. 2000;82:1151–1155. doi: 10.1302/0301-620X.82B8.11030. [DOI] [PubMed] [Google Scholar]
- 12.Schroder D, Bornstein L, Bostrom MP, Nestor BJ, Padgett DE, Westrich GH. Ceramic-on-ceramic total hip arthroplasty: incidence of instability and noise. Clin Orthop Relat Res. 2011;469:437–442. doi: 10.1007/s11999-010-1574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Streit MR, Merle C, Clarius M, Aldinger PR. Late peri-prosthetic femoral fracture as a major mode of failure in uncemented primary hip replacement. J Bone Joint Surg Br. 2011;93:178–183. doi: 10.1302/0301-620X.93B2.24329. [DOI] [PubMed] [Google Scholar]
- 14.Van Houwelingen AP, Duncan CP. The pseudo A (LT) periprosthetic fracture: it’s really a B2. Orthopedics. 2011;34:e479–e481. doi: 10.3928/01477447-20110714-27. [DOI] [PubMed] [Google Scholar]
- 15.Vidalain JP. Twenty-year results of the cementless Corail stem. Int Orthop. 2011;35:189–194. doi: 10.1007/s00264-010-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]