Abstract
Background
Total hip arthroplasty (THA) is a beneficial and cost-effective procedure for patients with osteoarthritis. Recent initiatives to improve hospital quality of care include assessing unplanned hospital readmission rates. Patients presenting for THA have different indications and medical comorbidities that may impact rates of readmission.
Questions/purposes
This study measured (1) the unplanned hospital readmission rate in primary THA, revision THA, and antibiotic-spacer staged revision THA to treat infection. Additionally, we determined (2) the medical and surgical causes of readmission; and (3) the risk factors associated with unplanned readmission.
Methods
A total of 1415 patients (988 primary THA, 344 revision THA, 82 antibiotic-spacer staged revision THA to treat infection) from a single institution were included. All hospital readmissions within 90 days of discharge were reviewed. Patient demographics and medical comorbidities were included in a Cox proportional hazards model to assess risk of readmission.
Results
The overall unplanned readmission rate was 4% at 30 days and 7% at 90 days. At 90 days, primary THA (5%) had a lower unplanned readmission rate than revision THA (10%, p < 0.001) and antibiotic-spacer staged revision THA (18%, p < 0.001). Medical diagnoses were responsible for almost one-fourth of unplanned readmissions, whereas over half of surgical readmissions were the result of dislocation, surgical site infection, and postoperative hematoma. Type of procedure, hospital stay greater than 5 days, cardiac valvular disease, diabetes with end-organ complications, and substance abuse were each associated with increased risk of unplanned readmission.
Conclusions
Higher rates of unplanned hospital readmissions in revision THA rather than primary THA suggest that healthcare quality measures that incorporate readmission rates as a proxy for quality of care should distinguish between primary and revision procedures. Failure to do so may negatively impact tertiary referral hospitals that often care for patients requiring complex revision procedures.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
THA is an effective treatment for degenerative joint disease [18, 19] and has been shown to be both clinically effective and cost-effective [13, 22]. Rates of hip replacement are expected to increase dramatically as the population ages and the prevalence of hip osteoarthritis increases [9]. Even so, complications associated with THA can result in inferior outcomes and increased costs [4]. Recently, there has been increased focus on improving the value of healthcare services and reducing the costs of care [2, 10, 14, 24].
Readmission to the hospital after an index procedure is expensive and is considered a key undesirable outcome by the World Health Organization [25]. In 2004, almost 20% of Medicare beneficiaries were rehospitalized within 30 days of discharge from a prior hospitalization at an estimated cost of 17.4 billion USD [8]. Beginning in 2013, Medicare will reduce payments for unplanned readmissions for underperforming hospitals with higher rates of readmission compared with the national average through their value-based purchasing program. Although this assessment will begin only for patients with specific diagnoses [15], it is clear that there is increased emphasis on the transparent evaluation of healthcare value by measuring specific quality metrics [23]. Thus, to address the unsustainable growth in healthcare costs in the long term, it is prudent to identify and potentially mitigate preventable causes of hospital readmissions.
Perioperative complications in total joint arthroplasty have been well described [12, 16, 17]. However, studies that have examined short-term complications after discharge tend to focus on specific common diagnoses that are found in administrative claims data [11, 26]. The purpose of this study was to compare the unplanned 90-day hospital readmission rates at one institution for patients undergoing primary and revision THA using patient-level data and to characterize the causes and risk factors associated with unplanned readmissions.
Patients and Methods
Patient Selection
Consecutive patients who underwent THA at a single institution between 2005 and 2011 were identified using an administrative claims database with International Classification of Diseases, 9th Revision (ICD-9) and Current Procedural Terminology codes for primary THA (81.51; 27130), revision THA (00.70–00.73, 81.53; 27134, 27137, 27138), and antibiotic spacer implantation/removal (84.56, 84.57; 27091). Patients were grouped by type of procedure: (1) primary THA; (2) revision THA; and (3) infected THA with staged implant removal, placement of cement-eluding antibiotic spacer, and finally revision THA. Patients were excluded if they did not meet minimum followup of 90 days. Patient medical comorbidities were identified using the Elixhauser definitions, which define groups of medical diagnoses using ICD-9 codes [6]. Additionally, patient severity of illness was assessed using the All Payer Refined Diagnosis Related Group Severity of Illness scale [7] but was not included in the multivariate analysis because it was unavailable before 2007.
Hospital Readmission
All hospital readmissions within 90 days of discharge that were identified from the administrative record were further evaluated by reviewing patients’ medical records. Planned hospital admissions were defined as when it was predetermined before the initial procedure that the patient would return for a second hospitalization; all other hospitalizations were classified as unplanned. Causes of readmission were grouped as surgical or medical. Patients were censored after one hospital readmission to ensure that patients with multiple hospital readmissions did not excessively weight the results.
Patient Characteristics
A total of 1415 patients met inclusion criteria for the study; 415 patients were excluded for insufficient followup (Table 1). There were 989 patients who underwent a primary THA, 344 who underwent a revision THA, and 82 who underwent a revision THA after staged antibiotic spacer to treat an infected THA. The average age was 58.8 ± 15.0 years for primary THA, 59.6 ± 14.5 years for revision THA, and 59.6 ± 14.5 years for infected THA. There were more women in the primary THA group than in the other two groups. Severity of illness scores were higher in the primary THA group than the revision THA group (p = 0.014) or the infected revision THA group (p = 0.017), but the infected THA group had more medical comorbidities than revision THA (p = 0.01) and primary THA (p < 0.001). Patients in the infected THA group had a longer length of hospital stay than primary THA (p < 0.001) or revision THA (p < 0.001). Medi-Cal (California’s Medicaid program) patients made up a higher percentage of the infected THA group (18.3%) than the primary (12.8%) or revision (7.9%) THA groups (p = 0.001). Medicare patients contributed more to the revision THA group (44.8%) than primary THA (33.5%) or infected THA (32.9%), whereas private payer patients made up approximately half of all groups (47.4%, 53.7%, and 48.8%, respectively).
Table 1.
Patient demographics
| Demographic | Primary THA | Revision THA | Antibiotic spacer | p value |
|---|---|---|---|---|
| Total | 989 | 344 | 82 | – |
| Age (years) | 58.8 ± 15.0 | 61.8 ± 13.6 | 59.2 ± −11.0 | 0.001* |
| Female | 581 (58.7%) | 191 (55.5%) | 35 (42.7%) | 0.015* |
| Length of stay (days) | 4.05 ± 2.3 | 5.41 ± 5.8 | 13 ± 17.4 | < 0.001* |
| Discharge to inpatient rehabilitation | 108 (10.9%) | 53 (15.4%) | 12 (14.6%) | 0.072 |
| Discharge to skilled nursing | 134 (13.5%) | 59 (17.2%) | 16 (19.5%) | 0.123 |
| APR SOI | 2.24 ± 1.1 | 2.07 ± 1.2 | 1.95 ± 1.3 | 0.009* |
| Total comorbidities | 2.07 ± 1.9 | 2.38 ± 2.1 | 3.11 ± 2.6 | < 0.001* |
Values are numbers with percentage in parentheses or mean ± SD; * statistical significance at p < 0.05; APR SOI = All Payer Refined Diagnosis Related Group Severity of Illness scale.
Statistical Analyses
Comparisons were made using a t-test for continuous variables and a chi-square test for categorical variables. Readmission rates were measured using a time-to-readmission analysis, and failure curves were compared using a log-rank test. Risk factors for unplanned readmission were assessed using a Cox proportional hazards model, which included patient demographic, surgical, and medical comorbidity information. Variables were included in the risk model if they showed a univariate association with readmission with a p value < 0.2. The final risk model removed variables stepwise if the p value was > 0.1. All other comparisons were considered statistically significant if the p value was < 0.05.
Results
Readmission Rate
The rate of unplanned readmissions was 4.3% (n = 61 of 1415) at 30 days and 6.6% (n = 93 of 1415) at 90 days. The all-cause 90-day readmission rate was 8.8% (n = 124 of 1415). Ten patients in the primary THA group (1.0%) had a planned readmission for a contralateral primary THA. There were 25 patients in the infected THA group (30.5%) who had planned readmissions for antibiotic spacer removal and revision THA. Patients were readmitted from the emergency department (43.0%), directly from the clinic (36.6%), and transferred from other hospitals (20.4%). Unplanned hospital readmissions included a surgical intervention in 59.1% of cases. Patients with private insurance had fewer unplanned readmissions than Medi-Cal patients (5.3% versus 9.7%, p = 0.027) but had a similar rate of readmission as Medicare patients (6.6%, p = 0.313).
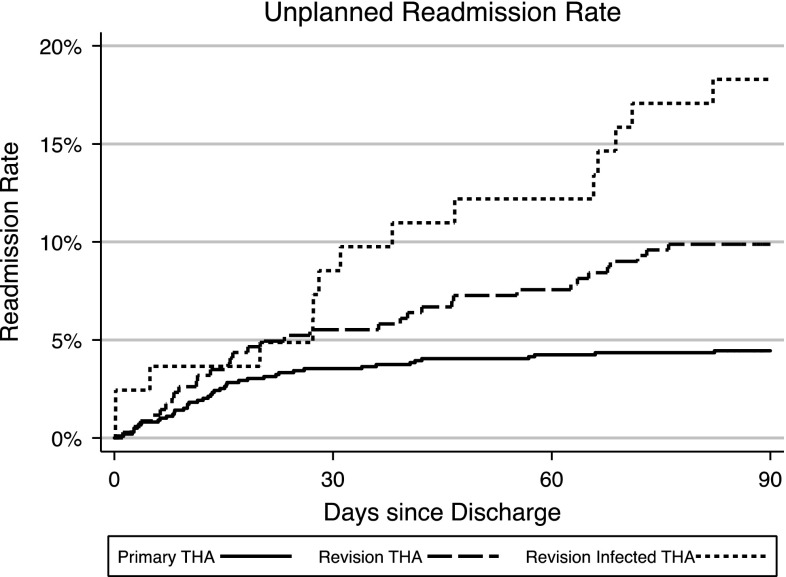
The 30-day unplanned readmission rates for primary, revision, and infected THA were 3.5%, 5.5%, and 8.5%, respectively. The infected THA group had significantly more readmissions than the primary THA group (p = 0.027). At 90 days, the infected THA group (18.3%) had significantly higher readmission rates than revision THA (9.9%, p = 0.034) and primary THA (4.5%, p < 0.001); revision THA was also higher than primary THA (p < 0.001) (Fig. 1). There were no differences in age or sex between readmitted and not readmitted patients, but readmitted patients were more likely to have had an index hospital stay more than 5 days (p\0.001), have been discharged to a skilled nursing facility (p = 0.001), and have more medical comorbidities (p < 0.001) (Table 2).
Fig. 1.
Ninety-day unplanned readmission rates for THA were significantly higher for the revision THA and infected THA groups compared with primary THA.
Table 2.
Demographics of readmitted and not readmitted patients
| Demographics | Readmitted | Not Readmitted | Odds ratio | SE (95% CI) | p value |
|---|---|---|---|---|---|
| Demographics | |||||
| Number | 93 | 1323 | – | – | – |
| Age (years) | 58.3 ± 15.8 | 59.6 ± 14.4 | 0.99 | 0.0 (1.0–1.0) | 0.388 |
| Female | 57 (61.3%) | 750 (56.7%) | 1.21 | 0.3 (0.8–1.9) | 0.387 |
| Surgical characteristics | |||||
| THA group | |||||
| Primary THA | 44 (4.4%) | 945 (95.6%) | Reference | Reference | Reference |
| Revision THA | 34 (9.9%) | 310 (90.1%) | 2.36 | 0.6 (1.5–3.8) | <0.001* |
| Antibiotic spacer | 15 (18.3%) | 67 (81.7%) | 4.81 | 1.6 (2.5–9.1) | <0.001* |
| Length of stay over 5 days | 46 (49.5%) | 235 (17.8%) | 4.53 | 1.0 (2.9–7.0) | <0.001* |
| Discharged to rehabilitation | 17 (18.3%) | 156 (11.8%) | 1.67 | 0.5 (1.0–2.9) | 0.067 |
| Discharged to skilled nursing facility | 20 (21.5%) | 189 (14.3%) | 1.64 | 0.4 (1.0–2.8) | 0.060 |
| Patient medical comorbidities | |||||
| APR severity of illness (1–4) | 2.0 ± 1.3 | 2.2 ± 1.1 | 0.89 | 0.1 (0.7–1.1) | 0.210 |
| Osteoporosis | 5 (5.4%) | 38 (2.9%) | 1.92 | 0.9 (0.7–5.0) | 0.182 |
| Tobacco use | 33 (35.5%) | 407 (30.8%) | 1.24 | 0.3 (0.8–1.9) | 0.345 |
| Morbid obesity | 9 (9.7%) | 70 (5.3%) | 1.92 | 0.7 (0.9–4.0) | 0.080 |
| Total comorbidities | 3.0 ± 2.3 | 2.2 ± 2.0 | 1.20 | 0.1 (1.1–1.3) | <0.001* |
Values are number with percentage in parentheses or mean ± SD; * statistical significance at p < 0.05; CI = confidence interval; APR = All Payer Refined Diagnosis Related Group.
Causes of Readmission
Surgical complications were responsible for 74.7% (n = 68 of 90) of readmissions, whereas medical causes accounted for 25.3% (n = 23 of 90) (Table 3). The majority of surgical causes were the result of dislocation (32.4%, n = 22 of 68), surgical site infection (SSI) (23.5%, n = 16 of 68), and postoperative hematoma (10.3%, n = seven of 68). However, there were differences between groups for the main causes of readmission. Dislocation occurred more often in revision THA (4.4%) than primary THA (0.7%, p < 0.001). SSI occurred in 0.3% of patients undergoing primary THA compared with 1.7% of patients with revision THA (p = 0.005) and 9.8% of patients with infected TKA (p < 0.001). Similarly, hematoma occurred in 0.3% of primary THA cases compared with 0.6% in revision THA (p = 0.169) and 2.4% in infected THA (p = 0.05).
Table 3.
Causes of readmission
| Cause | 0–90 days | 0–30 days | 31–60 days | 61–90 days |
|---|---|---|---|---|
| Medical | 23 (25.3%) | 16 (27.1%) | 5 (29.4%) | 2 (13.3%) |
| Pneumonia | 2 (8.7%) | 2 (12.5%) | – | – |
| Abdominal pain | 1 (4.3%) | 1 (6.2%) | – | – |
| Acute renal failure | 1 (4.3%) | 1 (6.2%) | – | – |
| Anemia | 1 (4.3%) | 1 (6.2%) | – | – |
| Breast cancer | 1 (4.3%) | 1 (6.2%) | – | – |
| Constipation | 1 (4.3%) | 1 (6.2%) | – | – |
| Chronic obstructive pulmonary disease | 1 (4.3%) | 1 (6.2%) | – | – |
| Medication compliance | 1 (4.3%) | 1 (6.2%) | – | – |
| Lower extremity edema | 1 (4.3%) | 1 (6.2%) | – | – |
| Nausea/vomiting | 1 (4.3%) | 1 (6.2%) | – | – |
| Neutropenic fever | 1 (4.3%) | 1 (6.2%) | – | – |
| Pulmonary edema | 1 (4.3%) | 1 (6.2%) | – | – |
| Pyelonephritis | 1 (4.3%) | 1 (6.2%) | – | – |
| Rheumatoid arthritis flare | 1 (4.3%) | 1 (6.2%) | – | – |
| Sick sinus syndrome | 1 (4.3%) | 1 (6.2%) | – | – |
| Cardiac tamponade | 1 (4.3%) | – | 1 (20.0%) | – |
| Cough | 1 (4.3%) | – | 1 (20.0%) | – |
| Pancreatitis | 1 (4.3%) | – | 1 (20.0%) | – |
| Polycystic kidney disease | 1 (4.3%) | – | 1 (20.0%) | – |
| Small bowel obstruction | 1 (4.3%) | – | 1 (20.0%) | – |
| Diabetes | 1 (4.3%) | – | – | 1 (50.0%) |
| Placement/social | 1 (4.3%) | – | – | 1 (50.0%) |
| Surgical | 68 (74.7%) | 43 (72.9%) | 12 (70.6%) | 13 (86.7%) |
| Dislocation | 22 (32.4%) | 13 (30.2%) | 5 (41.7%) | 4 (30.8%) |
| Surgical site infection | 16 (23.5%) | 9 (20.9%) | 4 (33.3%) | 3 (23.1%) |
| Hematoma | 7 (10.3%) | 3 (7.0%) | 1 (8.3%) | 3 (23.1%) |
| Noninfected draining wound | 6 (8.8%) | 5 (11.6%) | 1 (8.3%) | – |
| Acetabular cup loosening | 4 (5.9%) | 1 (2.3%) | 1 (8.3%) | 2 (15.4%) |
| Periprosthetic fracture | 3 (4.4%) | 3 (7.0%) | – | – |
| Cellulitis | 2 (2.9%) | 2 (4.7%) | – | – |
| Dehiscence | 2 (2.9%) | 2 (4.7%) | – | – |
| Pain management | 2 (2.9%) | 2 (4.7%) | – | – |
| Deep vein thrombosis | 1 (1.5%) | 1 (2.3%) | – | – |
| Osteolysis | 1 (1.5%) | 1 (2.3%) | – | – |
| Pulmonary embolism | 1 (1.5%) | 1 (2.3%) | – | – |
| Tendonitis | 1 (1.5%) | – | – | 1 (7.7%) |
Risk Factors
Revision THA was independently associated with increased risk of unplanned readmission (p = 0.007), whereas staged antibiotic spacer revision THA showed a trend for increased risk (p = 0.062). Additionally, patients with a hospital stay longer than 5 days are more likely to have a hospital readmission (p < 0.001) (Table 4). Patient comorbidities that were independently associated with increased risk of readmission were cardiac valvular disease, diabetes with end-organ complications, and substance abuse.
Table 4.
Independent risk factors for readmission
| Risk factor | Hazard ratio | SE (95% CI) | p value |
|---|---|---|---|
| Revision THA (versus primary) | 1.84 | 0.4 (1.2–2.9) | 0.007 |
| Antibiotic spacer THA (versus primary) | 1.85 | 0.6 (1.0–3.5) | 0.062 |
| Hospital stay over 5 days | 3.26 | 0.7 (2.1–5.1) | <0.001 |
| Diabetes with complications | 11.55 | 6.8 (3.6–36.8) | <0.001 |
| Cardiac valve disease | 2.52 | 0.9 (1.3–5.1) | 0.009 |
| Substance abuse | 2.05 | 0.9 (0.9–4.8) | 0.094 |
CI = confidence interval.
Discussion
Unplanned hospital readmissions are an unfortunate event for patients and increase the overall cost of treatment. In light of recent pressure to reduce hospital readmissions among common diagnoses and procedures, this study evaluated the unplanned hospital readmission rate after primary and revision THAs. In this observational cohort study of patients undergoing THA, we found that primary THAs had lower readmission rates than revision or staged antibiotic cement spacer THAs. One-fourth of unplanned readmissions were for medical causes, whereas the majority were the result of surgical complications. Additionally, almost half of readmissions were attributable to dislocation, SSI, or postoperative hematoma, which in many cases are considered preventable causes of readmission. The type of procedure, an index hospital length of stay over 5 days, and certain patient medical comorbidities (cardiac valvular disease, diabetes, and substance abuse) were found to have independent risk of unplanned hospital readmission.
This retrospective study has some limitations. We only captured patients whose readmissions took place at our hospital and thus may have underestimated the rate of readmissions insofar as some patients likely were readmitted elsewhere. Additionally, as a referral center that treats a large number of complex patients, our overall readmission rates may not generalize well to other referral centers or to community practices, depending on the profile of patients and procedures. However, this limitation should be at least partially mitigated by the way we grouped patients by procedure type. Additionally, we only evaluated the earliest procedure for each patient, so complicated patients with multiple procedures or multiple readmissions have not unfairly weighted these results. Finally, although most information was identified from primary record review, medical comorbidity diagnoses were obtained from administrative data, which assumes accuracy in coding. However, it has been shown that comorbidity data in administrative claims are accurate and if anything are underreported [1]. Thus, it is unlikely that these results show a falsely elevated risk of readmission associated with comorbidities.
Our results for 90-day unplanned readmission rates of 4.5% and 9.9% for primary and revision THA, respectively, are consistent with previous findings using cross-sectional patient samples. de Vries et al. [4] reported a 5.1% unplanned readmission rate for primary THA using a national database in the Netherlands, whereas Mahomed et al. [11] reported rates of 4.6% for primary THA and 10.0% for revision THA in a Medicare population in the United States. All-cause readmission rates at 90 days were reported by Zhan et al. [26] at 8.9% and 15.7% for primary and revision THA, respectively, using national- and state-level claims databases. Studies that use administrative claims databases rely on identifying complications before analysis; causes of readmission such as medical complications may be missed. Although claims databases offer increased power as a result of large sample size, one of the major advantages to our study design is the ability to confirm every hospital readmission with medical record verification. The literature has established a role for using administrative claims data for such analyses, but our study suggests that it is important to cross-reference these results with the clinical record to best target quality-of-care improvement initiatives based on such results.
Informed analysis of readmission rates in the context of an adverse outcome assessment requires separating planned and unplanned readmissions. We found that one-fourth of all readmissions were planned. Evaluating hospital performance with calculations based solely on administrative claims data may indiscriminately label all readmissions as complications, which would result in inaccurate quality data and could possibly lead to undeserved financial penalties. Planned readmissions were mostly for staged procedures for treatment of patients referred with an infection using protocols that are the standard of care associated with resection of implants with implantation of an antibiotic cement spacer and subsequent revision THA in a second stage [5]. However, this group of patients with planned two-stage procedures also had the highest rate of unplanned readmissions after the second stage of their procedure. Revision THA has been shown to have higher readmission rates than primary THA [3], and our results show that staged antibiotic spacer revision for infected THA has a greater risk for unplanned readmission than other patients undergoing revision THA. However, in the multivariate risk model, revision and antibiotic spacer THA showed similar risk, suggesting that factors such as patient comorbidities may be responsible for different readmission rates between these two groups of patients undergoing revision THA. Thus, assessments that distinguish patients based on procedure should stratify these groups separately when evaluating outcomes and quality data for THA.
Unplanned hospital readmissions resulting from medical causes occurred in 25% of cases, which is comparable to what has been reported after other orthopaedic procedures. In studies that also used detailed medical record review, medical complications contributed to 18% of unplanned readmissions after spine fusion for adult spinal deformity and 25% of readmissions after TKA [20, 21]. Jencks et al. [8] also found multiple different causes of hospital readmission after major hip or knee surgery, but as a result of the use of administrative claims data, the authors did not delineate all causes of readmission. Although the specific medical causes of readmission in this study were quite varied, this finding emphasizes the importance of preprocedure medical evaluation to identify and optimize comorbid medical conditions. Importantly, diabetes, cardiac valvular disease, and substance abuse each independently raise the risk of unplanned readmission and should be specifically addressed during preoperative counseling in an effort to optimize these conditions before elective surgery. Dislocation, infection, and hematoma accounted for the majority of surgical complications. These serious complications after total joint arthroplasty occur in the early postoperative course and may be related to other factors such as provider procedure volume and process standardization, which have been shown to affect quality of care [16]. However, these results highlight the potential impact of surgical process optimization with emphasis on targeted reductions in dislocation, infection, and postoperative hematoma complications.
Unplanned hospital readmissions add to the cost associated with elective surgical procedures such as THA. Accurate assessment and benchmarking of readmission rates for THA must differentiate among primary, revision, and staged antibiotic spacer arthroplasty procedures, because complications and readmissions after revision THAs may be inherently more common than after primary procedures. Additionally, it is important to distinguish planned readmissions from unplanned readmissions, because failure to do so would inappropriately inflate the readmission rate for revision THA cases for infection that require a two-stage treatment plan. Dislocation, SSI, and hematoma were responsible for almost half of the unplanned readmissions among patients undergoing THA in our hospital. These conditions may serve as targets for cost-effective process improvements to reduce expensive hospital readmissions. Finally, the independent risk factors identified here can help to improve risk stratification both for planning treatment options for patients and for more accurately assessing quality and value after primary and revision THA.
Acknowledgments
We thank Vanessa Chan MPH, for her help in preparing the manuscript.
Footnotes
One of the authors (TPV) certifies that he has received or may receive payments or benefits, during the study period, an amount in excess of USD 10,000 from DePuy Orthopaedics, Inc (Warsaw, IN, USA). KJB received funding from Orthopaedic Research and Education Foundation which ended in 2009. Although the study period (2005-2011) included the years of his research funding. This study was completed after his OREF funding was completed. The institution of one or more of the authors (KJB) has received, during the study period, funding from the OREF (Rosemont, IL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that institution where the work was performed approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bozic KJ, Bashyal RK, Anthony SG, Chiu V, Shulman B, Rubash HE. Is administratively coded comorbidity and complication data in total joint arthroplasty valid? Clin Orthop Relat Res. 2013;471:201–205. doi: 10.1007/s11999-012-2352-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010;92:2643–2652. doi: 10.2106/JBJS.I.01477. [DOI] [PubMed] [Google Scholar]
- 3.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, Li Y. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011;305:1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Vries LM, Sturkenboom MC, Verhaar JA, Kingma JH, Stricker BH. Complications after hip arthroplasty and the association with hospital procedure volume. Acta Orthop. 2011;82:545–552. doi: 10.3109/17453674.2011.618907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duncan CP, Masri BA. The role of antibiotic-loaded cement in the treatment of an infection after a hip replacement. Instr Course Lect. 1995;44:305–313. [PubMed] [Google Scholar]
- 6.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Iezzoni LI. Examining the validity of severity measures in today’s health policy context. J Gen Intern Med. 1995;10:406–408. doi: 10.1007/BF02599844. [DOI] [PubMed] [Google Scholar]
- 8.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 10.Larsen K, Hansen TB, Thomsen PB, Christiansen T, Soballe K. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91:761–772. doi: 10.2106/JBJS.G.01472. [DOI] [PubMed] [Google Scholar]
- 11.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85:27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty. Anesthesiology. 2002;96:1140–1146. doi: 10.1097/00000542-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Mariconda M, Galasso O, Costa GG, Recano P, Cerbasi S. Quality of life and functionality after total hip arthroplasty: a long-term follow-up study. BMC Musculoskelet Disord. 2011;12:222. doi: 10.1186/1471-2474-12-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marshall DA, Wasylak T, Khong H, Parker RD, Faris PD, Frank C. Measuring the value of total hip and knee arthroplasty: considering costs over the continuum of care. Clin Orthop Relat Res. 2012;470:1065–1072. doi: 10.1007/s11999-011-2026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Medicare Payment Advisory Commission (MedPAC). Medicare Payment Policy. Washington, DC, USA: Medicare Payment Advisory Commission (MedPAC); 2012.
- 16.Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]
- 17.Pulido L, Parvizi J, Macgibeny M, Sharkey PF, Purtill JJ, Rothman RH, Hozack WJ. In hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23:139–145. doi: 10.1016/j.arth.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Quintana JM, Arostegui I, Escobar A, Azkarate J, Goenaga JI, Lafuente I. Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Arch Intern Med. 2008;168:1576–1584. doi: 10.1001/archinte.168.14.1576. [DOI] [PubMed] [Google Scholar]
- 19.Rasanen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynanen OP, Roine RP. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop. 2007;78:108–115. doi: 10.1080/17453670610013501. [DOI] [PubMed] [Google Scholar]
- 20.Schairer WW, Carrer A, Deviren V, Hu SS, Takemoto S, Mummaneni P, Chou D, Ames C, Burch S, Tay B, Sawyer A, Berven SH. Hospital readmission after spine fusion for adult spinal deformity. Spine. 2013 May 21 [Epub ahead of print]. [DOI] [PubMed]
- 21.Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res. 2013 May 4 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 22.Sepucha KR, Stacey D, Clay CF, Chang Y, Cosenza C, Dervin G, Dorrwachter J, Feibelmann S, Katz JN, Kearing SA, Malchau H, Taljaard M, Tomek I, Tugwell P, Levin CA. Decision quality instrument for treatment of hip and knee osteoarthritis: a psychometric evaluation. BMC Musculoskelet Disord. 2011;12:149. doi: 10.1186/1471-2474-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Department of Health and Human Services. Medicare Hospital Compare Quality of Care. Available at: http://www.hospitalcompare.hhs.gov. Accessed March 15, 2013.
- 24.Volpp KG, Loewenstein G, Asch DA. Assessing value in health care programs. JAMA. 2012;307:2153–2154. doi: 10.1001/jama.2012.3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Do Current Discharge Arrangements From Inpatient Hospital Care for the Elderly Reduce Readmission Rates, the Length of Inpatient Stay or Mortality, or Improve Health Status? Copenhagen, Denmark: WHO Regional Office for Europe; 2005. [Google Scholar]
- 26.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89:526–533. doi: 10.2106/JBJS.F.00952. [DOI] [PubMed] [Google Scholar]