Abstract
Objective
Nurse practitioners (NPs) provide frontline care in women’s health, including contraception, an essential preventive service. Their importance for contraceptive care will grow, with healthcare reforms focused on affordable primary care. This study assessed practice and training needs to prepare NPs to offer high-efficacy contraceptives - IUDs and implants.
Method
A US nationally representative sample of nurse practitioners in primary care and women’s health was surveyed in 2009 (response rate 69%, n=586) to assess clinician knowledge and practices, guided by the CDC US Medical Eligibility Criteria for Contraceptive Use.
Results
Two-thirds of women’s health NPs (66%) were trained in IUD insertions, compared to 12% of primary care NPs. Contraceptive counseling that routinely included IUDs was low overall (43%). Nurse practitioners used overly restrictive patient eligibility criteria, inconsistent with CDC guidelines. Insertion training (aOR=2.4, 95%CI: 1.10 5.33) and knowledge of patient eligibility (aOR=2.9, 95%CI: 1.91 4.32) were associated with IUD provision. Contraceptive implant provision was low: 42% of NPs in women’s health and 10% in primary care . Half of NPs desired training in these methods.
Conclusion
Nurse practitioners have an increasingly important position in addressing high unintended pregnancy in the U.S., but require specific training in long-acting reversible contraceptives.
Keywords: Nurse practitioners, contraceptive care, IUD, contraceptive implant, long-acting reversible contraception
Introduction
Nurse Practitioners (NP) are important providers of women’s preventive care, especially in publicly-funded clinics serving populations at highest risk of unintended pregnancy.(Landry et al., 2008) Unintended pregnancy has persisted as a public health challenge in the United States, with significant economic and health-related costs.(Finer and Zolna, 2011; Sonfield et al., 2011) The role of nurse practitioners in contraceptive care stands to expand, with the inclusion of contraceptives and counseling as essential preventive care to be covered by insurance plans under the Affordable Care Act.(Institute of Medicine, 2011) Up-front costs have been a barrier for women to access contraceptives with the highest efficacy, the IUD and contraceptive implant, or long-acting reversible contraceptives (LARC).(Harper et al., 2012) Use of these methods has been greater in states where women have coverage for contraceptives, such as insurance mandates and Medicaid family planning expansion programs.(Thompson et al., 2011) Now that contraceptive coverage is expanding across the country, more women will be able to access these methods. The Centers for Disease Control and Prevention (CDC) points to the importance of increasing access to LARC methods to reach the Healthy People 2020 objective of reduced unintended pregnancy.(Centers for Disease Control and Prevention, 2013b; US Department of Health and Human Services, 2012)
While almost all contraceptive providers currently offer women oral contraceptives and condoms,(Landry et al., 2008) these methods have high discontinuation and typical-use failure rates, especially among underserved populations, where failure of oral contraceptives can be as high as 16 pregnancies per 100 person-years.(Kost et al., 2008; Raine et al., 2011; Vaughan et al., 2008) LARC methods have extremely low typical use failure rates (< 1%), similar to perfect use failure rates from clinical trials, because the methods require no user action for effectiveness.(Trussell, 2011) Many contraceptive providers have inadequate education on LARC methods.(Dehlendorf et al., 2010; Harper et al., 2008; Harper et al., 2012) LARC method use is low in the U.S., compared to some European countries, (U.S. 5%, France 23%, Finland 26%, Norway 27%) where health systems are focused on preventive and primary care.(Mosher and Jones, 2010; United Nations Department of Economic and Social Affairs Population Division, 2011) We are not aware of prior research that has examined the nursing profession to assess contraceptive care practices of NPs trained in women’s health and in primary care, particularly for the high-efficacy methods. In primary care, patients are seen for a wide range of medical issues, and there are competing demands on provider time. However, primary care NPs, as well as specialists in women’s health, will be called upon for women’s preventive health needs in our national context of improved contraceptive coverage and access.(Cleland et al., 2011; Pace and Cohen, 2011)
This study uses nationally representative survey data to identify counseling and provision practices for LARC methods among nurse practitioners serving women of reproductive age. Nationally representative data can help to reveal the prevalence of evidence-based contraceptive care among nurse practitioners and whether LARC is routinely provided in clinical practice. Study results can be used to help inform training and programmatic efforts to prepare our primary healthcare workforce to address the epidemic of unintended pregnancy. Our hypothesis is that LARC-specific, evidence-based education is required for nurse practitioners to integrate these high-efficacy methods into standard contraceptive care in the US.
Methods
We conducted a national probability survey of nurse practitioners (NPs) specializing in women’s health and primary care in 2009. The study was approved by the University of California, San Francisco Committee on Human Research. Our aim was for a sample size of at least 500 eligible respondents to achieve population estimates with ± 5% precision. For a detailed description of methodology, see Henderson et al. 2010.(Henderson et al., 2010) We used the Verispan national database of nurse practitioners, a comprehensive database updated monthly. Stratified probability samples of 600 primary care NPs and 600 women’s health NPs were drawn, using a random number generator. Duplicate names were dropped and 1,179 unique surveys were mailed. Primary care NPs were defined as NPs who worked in family medicine, primary care and adult medicine. Women’s health NPs were working in obstetrics and gynecology, women’s health, and reproductive medicine/family planning. To be eligible, NPs had to spend most of their time in direct patient care and provide family planning or HIV/STI services. There were 586 eligible respondents, and 221 ineligible NPs (or 27.4% of the total). Among the 372 non-responders, we assumed that the proportion ineligible was similar (27.4%; n=102), and removed all ineligibles (n=323) from the response rate denominator of 1,179.(The American Association for the Public Opinion Research, 2009) The response rate was 69%.
We sent selected NPs a letter explaining the study, followed by a survey, cover letter, return envelope and $20 cash by U.S. Priority Mail. A reminder postcard was sent one week later, and another survey to non-respondents in three weeks. Research staff made a maximum of four reminder calls.
The survey instrument was developed through formative qualitative interviews with clinicians, and items validated in previous research.(Harper et al., 2008; Harper et al., 2010b; Henderson et al., 2011) Survey items covered clinician characteristics, professional training, practice factors, patient population, and contraceptive care. Measures on LARC methods included clinician insertion skills, perceptions of safety, and beliefs of patient interest. Survey items included clinician knowledge of patient eligibility and method indications. Clinicians were also asked whether they would like training in IUDs or contraceptive implants.
Outcome Measures: Counseling and Provision of IUDs
Nurse practitioners were asked about the frequency of counseling female contraceptive patients on IUDs, using a 4-point likert scale (always, usually, sometimes, never). We created a dichotomous variable for routine counseling (usually/always v. sometimes/never). For contraceptive provision, the survey asked which methods were currently offered, and included the levonorgestrel-releasing IUD (Mirena®), the copper IUD (ParaGard®). We combined the two IUDs into a dichotomous outcome variable of IUD provision (yes/no).
The main predictor variable was professional training (primary care or women’s health). We also assessed practicum training in IUD insertion (yes/no). We evaluated clinician knowledge of method indications for the copper IUD and the levonorgestrel-releasing system, based on the CDC U.S. Medical Eligibility Criteria for Contraceptive Use.(Centers for Disease Control and Prevention, 2010) We created scale variables measuring knowledge and attitudes, based on previous research.(Harper et al., 2008; Harper et al., 2012) The knowledge variable had a reliability coefficient of 0.95. For knowledge, clinicians were asked whether they considered women with the following medical conditions to be eligible for the copper IUD: fibroids without distortion of uterine cavity, diabetes, obesity, smoker, history of hypertension. We used the same list of eligible conditions for the levonorgestrel-releasing system, as well as menorrhagia, dysmenorrhea, and iron deficiency anemia. NPs who responded that they would consider a woman for IUD use with these conditions were considered to have more evidence-based views of eligible women. We also created a 6-item scale variable to measure risk perceptions on how often clinician concerns about certain medical issues would prevent him/her from recommending IUDs: Uterine perforation at insertion, expulsion, sexually transmitted infections (STIs), pelvic inflammatory disease (PID), infertility, bleeding pattern changes. Responses (never, sometimes, usually, always) were reverse-coded for scale construction of low risk perception. The scale reliability coefficient on perception of risk was 0.84.
Statistical Analysis
We presented frequencies by specialty, and estimated odds ratios through bivariate and multivariable analyses, with 95% confidence intervals. We applied stratification design specifications in analyses to account for disproportionate sampling of NPs by specialty. The design-based Pearson Chi-square test for overall categorical differences and the Wald test for mean differences were calculated. We conducted multivariable logistic regression analysis to estimate the variation in each outcome variable, routine counseling and provision of IUDs, with clinician factors, evidence-based knowledge, and attitudes. We controlled for practice setting factors, including location and provider type (hospital-based, private office, community or family planning clinic). Significance was reported at p ≤ 0.05. Stata 11.1 (Stata Corp., College Station, TX) was used for analyses.
Results
A total of 586 eligible nurse practitioners responded, including 224 in primary care and 360 in women’s health (Table 1). Most of the NPs (86%) were trained in family planning, including almost all working in women’s health (97%). All of the NPs surveyed saw female patients in need of contraception, but women’s health NPs saw on average more than three times as many contraceptive patients per week as primary care NPs (p≤0.001).
Table 1.
US Nurse Practitioner Characteristics and Contraception Practices
| Women’s Health NPs |
Primary Care NPs |
Total | |
|---|---|---|---|
| (n=363) | (n=223) | N=586 | |
| Clinician Characteristics | |||
| Age, mean years (sd)** | 51 (9.8) | 49 (9.8) | 50 (9.9) |
| Gender, n (%) | |||
| Male | 3 (0.8) | 12 (5) | 15 (4) |
| Female | 360 (99) | 211 (95) | 571 (96) |
| Race/ethnicity, n (%) | |||
| White | 313 (87) | 198 (89) | 511 (88) |
| African-American | 20 (6) | 14 (6) | 34 (6) |
| Hispanic/Latino | 10 (3) | 6 (3) | 16 (3) |
| Asian/Pacific Islander | 9 (3) | 2 (1) | 11 (1) |
| Multi-racial/other | 6 (2) | 3 (1) | 9 (1) |
| Practice Setting & Patient Population | |||
| Practice setting, n (%)** | |||
| Private office | 154 (42) | 124 (56) | 278 (52) |
| Community clinic | 131 (36) | 50 (23) | 181 (27) |
| Hospital-based practice | 78 (21) | 46 (21) | 124 (21) |
| Urban v. rural, n (%)** | 284 (79) | 150 (68) | 434 (71) |
| Region, n (%)*** | |||
| West | 112 (30) | 32 (14) | 144 (19) |
| Midwest | 66 (18) | 40 (18) | 106 (18) |
| Northeast | 62 (17) | 50 (22) | 112 (21) |
| South | 123 (34) | 101 (45) | 224 (42) |
| Contraceptive patients per week, mean (sd)*** | 30 (30) | 9 (13) | 22 (27) |
| Training | |||
| Trained in family planning, n (%)*** | 353 (97) | 181 (82) | 583 (86) |
| Inserted IUC in clinical practicum, n (%)*** | 237 (66) | 27 (13) | 264 (29) |
| Comfortable inserting IUD, n (%)*** | 232 (73) | 25 (12) | 257 (30) |
| Comfortable inserting single-rod implant, n (%)*** | 90 (26) | 12 (6) | 102 (12) |
| Contraceptive Counseling | |||
| Time to counsel patients on contraceptives, n (%)** | 302 (84) | 159 (74) | 461 (77) |
| Patients receptive to learning about IUD, n (%)*** | 338 (95) | 180 (86) | 518 (89) |
| Routinely discuss IUD with patients, n (%)*** | 260 (72) | 64 (30) | 324 (43) |
| Contraceptives Provided to Patients | |||
| Oral contraceptive pills, n (%)*** | 351 (97) | 182 (84) | 533 (88) |
| Vaginal ring, n(%)*** | 321 (88) | 132 (61) | 453 (69) |
| Transdermal patch, n(%)*** | 290 (80) | 120 (55) | 410 (63) |
| Injectable, n (%)*** | 337 (93) | 155 (71) | 492 (78) |
| Emergency contraceptive pills, n (%)*** | 310 (85) | 111 (51) | 421 (61) |
| IUDs, n (%)*** | 311 (86) | 67 (31) | 378 (48) |
| Implant, n (%)*** | 154 (42) | 21 (10) | 175 (20) |
p ≤ 0.05
p ≤ 0.010
p ≤ 0.001
IUD insertion skills were limited among primary care NPs; only 12% reported they were comfortable inserting IUDs, although 92% believed IUDs to be a safe. However, 72% of NPs in women’s health were comfortable inserting IUDs, with 98% believing the method to be safe. Compared to women’s health NPs, those in primary care were unlikely to have received clinical IUD insertion practicum training (66% v. 12%). Training and skills in the contraceptive implant were also low, with 26% of women’s health NPs competent in insertions and only 6% of primary care nurses.
Over three-quarters of NPs thought they had sufficient time to counsel their patients on contraceptive options, and most (89%) reported that their patients would be receptive to learning about IUDs. Most NPs (73%) believed IUDs were under-used in their patient population, with no difference by specialty. However, only 30% of primary care NPs and 72% in women’s health reported routinely including IUDs in discussions with contraceptive patients. About 60% of NPs considered cost of LARC methods an important obstacle to provision.
While oral contraceptives were provided by 97% of women’s health NPs and 83% of primary care NPs, IUDs were offered far more frequently by women’s health NPs than primary care NPs (86% v. 31%). The contraceptive implant was offered by only 42% of women’s health NPs and 10% of primary care NPs .
Fifty percent of women’s health NPs desired training in the contraceptive implant, as did 30% of primary care NPs. Twenty percent of women’s health NPs and 35% in primary care desired IUD training. Overall, half of NPs desired training in LARC methods with no significant difference by specialty.
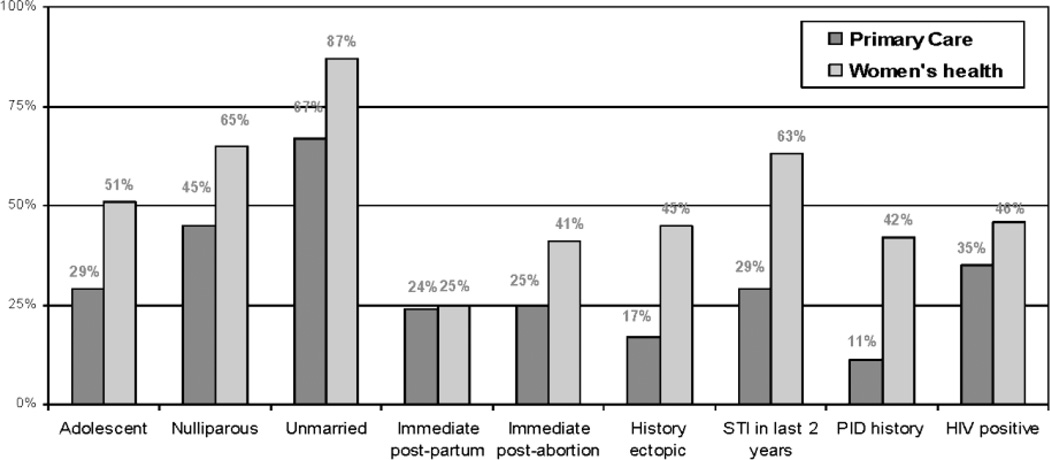
Many NPs were not aware of the wide range of women eligible for IUD use, according to the CDC Medical Eligibility Criteria for Contraception, including teenagers and nulliparous women. Only 29% of NPs in primary care and 51% in women’s health thought teenagers were eligible. In general, primary care NPs had lower knowledge about patient eligibility for IUDs than did women’s health NPs (see Figure 1).
Figure 1.
Percentage of advance practice nurses who would consider Intrauterine contraception for the following patients
Table 2 shows IUD knowledge and risk perceptions among NPs, by specialty. NPs working in women’s health had more accurate knowledge of method contraindications, but few NPs in primary care knew that IUDs are appropriate for women with common conditions, including diabetes, obesity, or smoking. Few NPs in primary care were aware of the non-contraceptive benefits of levonorgestrel-releasing IUDs, including improvement in menorrhagia and dysmenorrhea. Primary care NPs’ lower knowledge of method contraindications was accompanied by higher perceptions of risks associated with IUDs, particularly concerns about STIs, PID and infertility.
Table 2.
Knowledge and Attitudes on Intrauterine Contraception among Nurse Practitioners in the United States
| Women’s health NPs |
Primary care NPs |
Total | |
|---|---|---|---|
| % | % | % | |
| Nurse practitioner knowledge of appropriate IUC use | |||
| Would consider LNG-IUS for patients withү: | |||
| Diabetes*** | 81 | 39 | 52 |
| Obesity*** | 85 | 42 | 56 |
| Smoker*** | 84 | 36 | 51 |
| History of Hypertension*** | 84 | 38 | 53 |
| Fibroids without distortion uterine cavity*** | 74 | 31 | 44 |
| Would consider copper IUD for patient withү: | |||
| Diabetes*** | 82 | 40 | 54 |
| Obesity*** | 86 | 43 | 57 |
| Smoker*** | 92 | 47 | 61 |
| History of hypertension*** | 91 | 48 | 62 |
| Fibroids without distortion uterine cavity*** | 53 | 25 | 34 |
| Nurses practitioner attitudes (perception of risk) | |||
| Concerns about the following issues would prevent IUD recommendation: | |||
| Sexually transmitted infections** | 35 | 49 | 44 |
| Pelvic inflammatory disease*** | 38 | 55 | 50 |
| Infertility*** | 15 | 27 | 23 |
| Expulsion*** | 4 | 14 | 11 |
| Uterine perforation at insertion*** | 5 | 19 | 15 |
| Changes in bleeding pattern*** | 11 | 26 | 21 |
All conditions approved for method use by CDC Medical Eligibility Criteria for Contraception
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001
LNG, levonorgestrel-releasing intrauterine system
Results from multivariable logistic regression (Table 3) showed that primary care NPs were significantly less likely to routinely counsel contraceptive patients on IUDs compared to women’s health NPs (aOR=.41, 95%CI: 0.23 0.72). However, NPs with a high level of knowledge were almost twice as likely to routinely counsel patients (OR=1.9, 95%CI: 1.35 2.80). Results in Table 4 show that primary care NPs had significantly lower odds of IUD provision (OR=0.19, 95%CI: 0.10 0.38). Practicum training for insertions was associated with greater provision later in practice (OR=2.4, 95%CI: 1.10 5.33). Attitudes and knowledge were also associated with IUD provision: NPs with low perception of IUD risks had increased odds of provision (OR=1.5, 95%CI 1.00 2.19), as did those with a high level of IUD knowledge (OR=2.9, 95%CI: 1.91 4.32).
Table 3.
Routine Counseling on Intrauterine Contraceptives to Female Contraceptive Patients: Multivariable Logistic Regression Results of US Nurse Practitioners
| Routinely counsel patients on IUDs | Unadjusted Odds Ratio |
[95% CI] | Adjusted Odds Ratio |
[95% CI] |
|---|---|---|---|---|
| Clinician characteristics | ||||
| Specialty | ||||
| Women’s Health NP (reference) | -- | -- | -- | -- |
| Primary Care NP | 0.17 | [0.11 0.24] | 0.41 | [0.23 0.72] |
| Trained in IUD insertions in practicum | 3.89 | [2.59 5.85] | 1.60 | [0.84 3.04] |
| Age (years) | 1.01 | [0.99 1.03] | 1.00 | [0.98 1.03] |
| White (non-Hispanic) | 1.39 | [0.76 2.52] | 1.02 | [0.43 2.44] |
| Evidence-based attitudes/knowledge | ||||
| Low perception of IUD risks | 1.89 | [1.40 2.57] | 1.44 | [0.97 2.13] |
| High level IUD knowledge | 3.20 | [2.38 4.30] | 1.94 | [1.35 2.80] |
| Practice setting | ||||
| Provider type | ||||
| Hospital-based practice (reference) | -- | -- | -- | -- |
| Private office | 1.24 | [0.75 2.05] | 1.61 | [0.85 3.04] |
| Community clinic | 1.37 | [0.79 2.38] | 1.11 | [0.54 2.27] |
| Urban location | 1.91 | [1.22 2.98] | 1.74 | [0.99 3.04] |
| Region | ||||
| West (reference) | -- | -- | -- | -- |
| Midwest | 0.45 | [0.24 0.84] | 0.65 | [0.30 1.42] |
| Northeast | 0.62 | [0.33 1.15] | 1.00 | [0.46 2.18] |
| South | 0.38 | [0.22 0.65] | 0.63 | [0.33 1.17] |
| Patient population | ||||
| Female contraceptive patients (#/wk) | 1.04 | [1.02 1.05] | 1.00 | [0.99 1.01] |
| Number of observations | 517 |
Table 4.
Provision of Intrauterine Contraceptives to Female Contraceptive Patients: Multivariable Logistic Regression Results of US Nurse Practitioners
| Provide IUD to patients | Unadjusted Odds Ratio |
[95% CI] | Adjusted Odds Ratio |
[95% CI] |
|---|---|---|---|---|
| Clinician characteristics | ||||
| Specialty | ||||
| Women’s Health NP (reference) | -- | -- | -- | -- |
| Primary care NP | 0.07 | [0.05 0.11] | 0.19 | [0.10 0.38] |
| Trained in IUD insertions in practicum | 6.37 | [3.98 10.1] | 2.42 | [1.10 5.33] |
| Age (years) | 1.01 | [0.99 1.03] | 1.02 | [0.99 1.05] |
| White (non-Hispanic) | 1.55 | [0.86 2.78] | 3.11 | [1.00 9.62] |
| Evidence-based attitudes/knowledge | ||||
| Low perception of IUD risks | 1.97 | [1.50 2.57] | 1.48 | [1.00 2.19] |
| High level IUD knowledge | 4.88 | [3.50 6.80] | 2.87 | [1.91 4.32] |
| Practice setting | ||||
| Provider type | ||||
| Hospital-based practice (reference) | -- | -- | -- | -- |
| Private office | 1.95 | [1.19 3.20] | 4.54 | [1.96 10.51] |
| Community clinic | 2.50 | [1.44 4.33] | 3.36 | [1.27 8.90] |
| Urban location | 1.38 | [0.89 2.14] | 1.28 | [0.52 1.32] |
| Region | ||||
| West (reference) | -- | -- | -- | -- |
| Midwest | 0.57 | [0.29 1.11] | 0.68 | [0.37 1.26] |
| Northeast | 0.37 | [0.19 0.70] | 0.32 | [0.16 0.63] |
| South | 0.32 | [0.18 0.57] | 0.30 | [0.16 0.57] |
| Patient population | ||||
| Female contraceptive patients (#/wk) | 1.02 | [1.01 1.03] | 1.01 | [1.00 1.02] |
| Number of observations | 518 |
Discussion
Nurse practitioners serve millions of contraceptive patients, and are trained to have skills in counseling and clinical care. The clinic visit is especially important for patient education and counseling on LARC methods. Few U.S. women are familiar with LARC methods, especially younger women at high risk of unintended pregnancy.(Kaye et al., 2009; Whitaker et al., 2008) National survey data have shown that young women consider their healthcare providers their most trusted source of contraceptive information.(Kaye et al., 2009) Young women are also more likely to choose a new method, including the IUD, if their provider has discussed it with them.(Fleming et al., 2010; Harper et al., 2010a) While LARC method used has increased recently in the U.S., most of the increase is among parous women.(Finer et al., 2012; Kavanaugh et al., 2011) Although young women relying on user-dependent methods have elevated failure and pregnancy rates,(Raine et al., 2011) these results showed that NPs often do not view adolescent and nulliparous women as IUD candidates, due to overly restrictive views of eligibility.(Centers for Disease Control and Prevention, 2010; Deans and Grimes, 2009) Integrating long-acting contraception into NPs’ counseling and clinical practice can help to prevent pregnancy and also rapid subsequent pregnancy among adolescent mothers and young women.(Waggoner et al., 2012)
Results showed that women with common conditions seen in the primary care setting, including history of hypertension, obesity, and diabetes, are often viewed as ineligible for IUD use. Offering high-efficacy methods to a wide range of women, including those with medical problems, is particularly important as these women are more likely to have complicated pregnancies. Furthermore, estrogen-containing methods, such as the combined oral contraceptive pill, are associated with a small increased risk for women with risk factors for cardiovascular disease, such as hypertension, obesity and diabetes(Burkman R et al., 2011). The NPs surveyed offered oral contraceptives almost universally, but were far less likely to offer the IUD or implant, high-efficacy methods without estrogen. It is important for clinicians to offer these methods to increase safe and effective pregnancy prevention for women with medical conditions.
While primary care NPs have general family planning training, these data showed that training to competency in IUDs or implants was rare, but widely desired by NPs working in primary care as well as in women’s health. Almost all NPs considered IUDs to be safe, but less than half reported routinely counseling women. Results on attitudes showed while general attitudes about safety were high, NPs in primary care also held relatively high risk perceptions of the IUD in specific areas, for example, PID and infertility. However, risk perceptions were lower among NPs with higher knowledge, and the lower risk perceptions were also associated with higher provision. Qualitative data have also shown this inverse relationship, and that risk perceptions tend to decrease with greater familiarity and experience.(Morse et al., 2012) Core training during advanced practice nursing programs is needed. Curriculums should be revised to include these methods in core training. Continuing education for practicing NPs is critical as well, particularly as contraceptive technologies advance and new methods, such as the single-rod implant, become available. Resources should be given for hands-on training in continuing education. The training must include didactics on method indications and appropriate patient eligibility criteria, in order for NPs to be able to offer evidence-based counseling to patients. The CDC US Medical Eligibility Criteria for Contraceptive Use,(Centers for Disease Control and Prevention, 2010) as well as the newly released US Selected Practice Recommendations for Contraceptive Use(Centers for Disease Control and Prevention, 2013a), are important sources for evidence-based training. In this study evidence-based views of IUDs accompanied greater counseling and provision of the method.
According to diffusion of innovation theory, significant investment is needed early on for new clinical practices to be disseminated, or change falters.(Berwick, 2003) These results show that among primary care NPs significant investments will be needed for evidence-based information on LARC methods to become part of standard contraceptive care. However, for NPs in women’s health, supplementary educational efforts should be able to achieve more widespread access to LARC methods.
Strengths of this study include nationally representative data assessing provision of the most effective contraceptive methods, and a relatively high response rate for national surveys of clinicians.(Lawrence and Curlin, 2009; U.S. Department of Health and Human Services and Health Resources and Services Administration (2010)) All analyses show association, rather than causation. A limitation is that we asked the NPs themselves about their practices, and responses may have social desirability bias. However, bias would likely mean training needs would only be more pronounced; data on provision may be more objective. When the survey was planned, the implant was available in few practices, so survey questions were more heavily concentrated on the IUD. It is possible that LARC competence among NPs has increased since data collection. As a nationally representative survey, these results can stand as an important baseline upon which we can compare any improvements in LARC competency over time, among primary care and women’s health NPs. Similar findings, of limited implant training and low counseling of young women on IUDs, was also found in a 2011 survey of publicly funded family planning clinics in the U.S. (Kavanaugh et al., 2013)
Conclusions
A shift in the current paradigm towards a greater emphasis on prevention and evidence-based care may hold promise to achieve Healthy People 2020 goals.(Levi and Dau, 2011; Taylor and James, 2011) NPs provide important care to underserved patient populations, and can make a difference in our nation’s health.(Grumbach et al., 2003; Kuehn, 2010) NPs offer care to vulnerable women of reproductive age in primary care settings, such as Federally Qualified Health Centers, as well as in community family planning clinics. To address the persistent problem of unintended pregnancy, it is essential to train nurse practitioners who deliver contraceptive care to offer the most effective methods, alongside more familiar methods.
Highlights.
Contraceptives are now included as women’s essential preventive care.
With emphasis on affordable primary care, NPs are prominent in contraceptive care.
Counseling on IUDs and implants is not yet a part of standard contraceptive care.
Evidence-based training was rare, but desired, for primary care nurse practitioners.
Education based on CDC US Medical Eligibility Criteria for Contraception is needed.
Acknowledgements
This project was funded by NIH/NICHD R01 HD046027 and the William and Flora Hewlett Foundation. Its contents are solely the responsibility of the authors.
We would like to acknowledge Ms. Lily Loew and Ms. Cait Quinlivan for their adept research assistance.
Conflict of Interest Statement
Dr. Raine-Bennett and Dr. Cynthia Harper have received grant support for research on emergency contraception from Teva Pharmaceuticals Inc, administered through the University of California, San Francisco. Ms. Debbie Postlethwaite is using research funds provided by Bayer HealthCare Pharmaceutical Inc. for a study, administered through the Kaiser Foundation Research Institute. Dr. J. Joseph Speidel serves as a consultant to Medicines360, WomanCare Global and Bayer Healthcare Pharmaceutical Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data were presented at the North American Forum on Family Planning, Washington, DC, October 2011.
Contributor Information
Cynthia C. Harper, Email: harperc@obgyn.ucsf.edu.
Laura Stratton, Email: strattonl@obgyn.ucsf.edu.
Tina R. Raine, Email: Tina.R.Raine-Bennett@kp.org.
Kirsten Thompson, Email: thompsonkm@obgyn.ucsf.edu.
Jillian T. Henderson, Email: Jillian.T.Henderson@kpchr.org.
Maya Blum, Email: blumm@obgyn.ucsf.edu.
Debbie Postlethwaite, Email: Debbie.A.Postlethwaite@kp.org.
J Joseph Speidel, Email: speidelj@obgyn.ucsf.edu.
References
- Berwick DM. Disseminating innovations in health care. JAMA. 2003;289:1969–1975. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- Burkman R, Bell C, Serfaty D. The evolution of combined oral contraception: improving the risk-to-benefit ratio. Contraception. 2011;84:19–34. doi: 10.1016/j.contraception.2010.11.004. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. United States medical eligibility criteria for contraceptive use, 2010. MMWR. 2010;59:1–6. [Google Scholar]
- Centers for Disease Control and Prevention. U.S. Selected Practice Recommendations for Contraceptive Use, 2013. 2013a;62:1–46. [Google Scholar]
- Centers for Disease Control and Prevention. Unintended Pregnancy Prevention. 2013b http://www.cdc.gov/reproductivehealth/UnintendedPregnancy/.
- Cleland K, Peipert JF, Westhoff C, Spear S, Trussell J. Family planning as a cost-saving preventive health service. N Engl J Med. 2011;364:e37. doi: 10.1056/NEJMp1104373. [DOI] [PubMed] [Google Scholar]
- Deans E, Grimes D. Intrauterine devices for adolescents: a systematic review. Contraception. 2009;79:418–423. doi: 10.1016/j.contraception.2008.12.009. [DOI] [PubMed] [Google Scholar]
- Dehlendorf C, Levy K, Ruskin R, Steinauer J. Health care providers' knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81:292–298. doi: 10.1016/j.contraception.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. 2012;98:893–897. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–485. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming K, Sokoloff A, Raine T. Attitudes and beliefs about the IUD among teenagers and young women. Contraception. 2010;82:178–182. doi: 10.1016/j.contraception.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grumbach K, Hart LG, Mertz E, Coffman J, Palazzo L. Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med. 2003;1:97–104. doi: 10.1370/afm.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper CC, Blum M, De Bocanegra HT, Darney PD, Speidel JJ, Policar M, Drey EA. Challenges in translating evidence to practice: The provision of intrauterine contraception. Obstet Gynecol. 2008;111:1359–1369. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- Harper CC, Brown BA, Foster-Rosales A, Raine TR. Hormonal contraceptive method choice among young, low-income women: How important is the provider? Patient Educ Couns. 2010a;81:349–354. doi: 10.1016/j.pec.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper CC, Henderson JT, Raine TR, Goodman S, Darney PD, Thompson K, Dehlendorf C, Speidel JJ. Evidence-based IUD practice: family physicians and obstretrician-gynecologists. Fam Med. 2012;44:637–645. [PMC free article] [PubMed] [Google Scholar]
- Harper CC, Henderson JT, Schalet A, Becker D, Stratton L, Raine TR. Abstinence and teenagers: Prevention counseling practices of health care providers serving high-risk patients in the United States. Perspect Sex Reprod Health. 2010b;42:125–132. doi: 10.1363/4212510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson JT, Raine T, Schalet A, Blum M, Harper CC. "I Wouldn't Be this Firm if I Didn't Care": Preventive clinical counseling for reproductive health. Patient Educ Couns. 2011;82:254–259. doi: 10.1016/j.pec.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson JT, Sawaya GF, Blum M, Stratton L, Harper CC. Pelvic Examinations and Access to Oral Hormonal Contraception. Obstet Gynecol. 2010;116:1257–1264. doi: 10.1097/AOG.0b013e3181fb540f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Clinical preventive services for women: Closing the gaps. Washington, DC: The National Academies Press; 2011. [Google Scholar]
- Kavanaugh ML, Jerman J, Ethier K, Moskosky S. Meeting the contraceptive needs of teens and young adults: Youth-friendly and Long-acting reversible contraceptive services in U. S. family planning facilities. 2013;52:284–292. doi: 10.1016/j.jadohealth.2012.10.276. [DOI] [PubMed] [Google Scholar]
- Kavanaugh ML, Jerman J, Hubacher D, Kost K, Finer LB. Characteristics of women in the United States who use long-acting reversible contracetpive methods. 2011;117:1349–1357. doi: 10.1097/AOG.0b013e31821c47c9. [DOI] [PubMed] [Google Scholar]
- Kaye K, Suellentrop K, Soup C. The fog zone: How misperceptions, magical thinking and ambivalence put young adults at risk of unplanned pregnancy. Washington, DC: 2009. [Google Scholar]
- Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehn BM. IOM: Boost nurses' role in health care. JAMA. 2010;304:2345–2346. doi: 10.1001/jama.304.21.2345. [DOI] [PubMed] [Google Scholar]
- Landry D, Wei J, Frost J. Public and private providers' involvement in improving their patients' contraceptive use. Contraception. 2008;78:42–51. doi: 10.1016/j.contraception.2008.03.009. [DOI] [PubMed] [Google Scholar]
- Lawrence RE, Curlin FA. Physicians' beliefs about conscience in medicine: a national survey. Acad Med. 2009;84:1276–1282. doi: 10.1097/ACM.0b013e3181b18dc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levi A, Dau KQ. Meeting the national health goal to reduce unintended pregnancy. JOGNN. 2011;40:775–781. doi: 10.1111/j.1552-6909.2011.01292.x. [DOI] [PubMed] [Google Scholar]
- Morse J, Freedman L, Speidel JJ, Thompson KMJ, Stratton L, Harper CC. Post-abortion contraception: Qualitative interviews on counseling and provision of long-acting reversible contraceptive methods. 2012;44:100–106. doi: 10.1363/4410012. [DOI] [PubMed] [Google Scholar]
- Mosher WD, Jones J. Use of contraception by in the United States: 1982–2008. National Center for Health Statistics. Vital Health Stat. 2010;23 [PubMed] [Google Scholar]
- Pace LE, Cohen L. Contraception in primary care - embracing the Institute of Medicine Challenge. N Engl J Med. 2011;365:2438–2439. doi: 10.1056/NEJMc1109240. [DOI] [PubMed] [Google Scholar]
- Raine TR, Foster-Rosales A, Upadhyay UD, Boyer CB, Brown BA, Sokoloff A, Harper CC. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol. 2011;117:363–371. doi: 10.1097/AOG.0b013e31820563d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonfield A, Kost K, Gold RB, Finer LB. The public costs of births resulting from unintended pregnancies: national and state-level estimates. Perspect Sex Reprod Health. 2011;43:94–102. doi: 10.1363/4309411. [DOI] [PubMed] [Google Scholar]
- Taylor D, James A. An evidence-based guideline for unintended pregnancy prevention. JOGNN. 2011;40:782–793. doi: 10.1111/j.1552-6909.2011.01296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The American Association for the Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. Deerfield: American Association for Public Opinions Research; 2009. [Google Scholar]
- Thompson KMJ, Speidel JJ, Saporta V, Waxman NJ, Harper CC. Contraceptive policies affect post-abortion provision of long-acting reversible contraception. Contraception. 2011;83:41–47. doi: 10.1016/j.contraception.2010.06.008. [DOI] [PubMed] [Google Scholar]
- Trussell J. Contraceptive efficacy. In: Hatcher R, Trussell J, Nelson A, Cates W, Kowal D, Policar M, editors. Contraceptive Technology. 20th ed. New York: Ardent Media; 2011. pp. 779–863. [Google Scholar]
- U.S. Department of Health and Human Services, Health Resources and Services Administration. The Registered Nurse Population: Findings from the 2008 National Sample Survey of Registered Nurses. 2010. [Google Scholar]
- United Nations Department of Economic and Social Affairs Population Division. World Contraceptive Use 2011. 2011 http://www.un.org/esa/population/publications/contraceptive2011/wallchart_front.pdf.
- Us Department of Health and Human Services. Healthy People 2020. 2012 http://www.healthypeople.gov/2020/topicsobjectives2020.
- Vaughan B, Trussell J, Kost K, Singh S, Jones R. Discontinuation and resumption of contraceptive use: results from the 2002 National Survey of Family Growth. Contraception. 2008;78:271–283. doi: 10.1016/j.contraception.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waggoner MR, Gaines Lanzi R, Klerman LV. Pregnancy intentions, long-acting contraceptive use, and rapid subsequent pregnancies among adolescent and adult first-time mothers. J Child Adolesc Psychiatr Nurs. 2012;25:96–104. doi: 10.1111/j.1744-6171.2012.00326.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker A, Johnson L, Harwood B, Chiappetta L, Creinin M, Gold M. Adolescent and young adult women's knowledge of and attitudes toward the intrauterine device. Contraception. 2008;78:211–217. doi: 10.1016/j.contraception.2008.04.119. [DOI] [PubMed] [Google Scholar]