Abstract
Although pharmacological treatment constitutes the main therapeutic approach for depression, non-pharmacological treatments (self-care or psychotherapeutic approach) are usually regarded as more essential therapeutic approaches in clinical practice. However, there have been few clinical practice guidelines concerning self-care or psychotherapy in the management of depression. This study introduces the 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression in Korea.' For the first time, a guideline was developed for non-pharmacological treatments for Korean adults with mild-to-moderate depression. The guideline development process consisted of establishing several key questions related to non-pharmacologic treatments of depression, searching the literature for studies which answer these questions, assessing the evidence level of each selected study, drawing up draft recommendation, and peer review. The Scottish Intercollegiate Guidelines Network grading system was used to evaluate the quality of evidence. As a result of this process, the guideline recommends exercise therapy, bibliotherapy, cognitive behavior therapy, short-term psychodynamic supportive psychotherapy, and interpersonal psychotherapy as the non-pharmacological treatments for adult patients with mild-to-moderate depression in Korea. Hence, it is necessary to develop specific methodologies for several non-pharmacological treatment for Korean adults with depression.
Keywords: Depression, Non-Pharmacological Treatment, Self-Care, Psychotherapy, Guideline, Korea
INTRODUCTION
Depression is a highly prevalent psychiatric disorder that tends to be recurrent and chronic (1). World Health Organization (WHO) has predicted that depression will be the second leading cause of early death or disability by 2020 (2). In Korea, depression is a prominent social issue, as suicidal rates have rapidly increased after the year 2000 (3). Nevertheless, clinical treatment for depression had not been standardized and is usually dependent on the clinical experiences or decisions of individual psychiatrists. Since the late 1990s, several mental health groups in Korea have developed evidence-based clinical practice guidelines in order to provide an organized systemic review of therapeutic recommendations for depression (4, 5).
The Korean Guideline Development Team for Depression considered the minimal infrastructure needed to develop an evidence-based clinical practice guideline for depression in Korea. The group was encouraged by the improving research environment in which the communication network provided up-to-date knowledge of depression treatment (6). By 2005, the Ministry of Health and Welfare, Republic of Korea Government took note of depression as a serious public health issue and considered a clinical practice guideline for depression to be essential to improve and organize its treatment or management. Eventually, the Ministry founded the Clinical Research Center for Depression as a project to develop the infrastructure of public mental health and medical management for depression (7). The Clinical Research Center for Depression aimed to identify the natural history of disease through clinical studies in Korean adults with depression and made a Korean version of an evidence-based treatment guideline for depression. By 2006, the necessity for a non-pharmacological treatment guideline for depression was confirmed through 'Investigation of the Current Status and Requirement of Non-Pharmacological Treatment for Depression in Korea' by the Third Detailed Task Force of the Clinical Research Center for Depression. In this investigation, 236 consecutive outpatients with depression in Korea were recruited in 12 university-affiliated hospitals. The depressed patients filled out a self-report questionnaire about current clinical status and non-pharmacological treatment for depression. Specifically, the questionnaire composed of 19 questions concerning desired type of depression treatment by patients, desired length and cost of psychiatric interviews by patients, means of obtaining information about depression, and other matters relating to psychiatric care. When asked about the goal of treatment for depression, 75.5% of patients answered that the goal to be improvements in physical and affective symptoms, but 24.5% desired a higher level of treatment goal including reformulation of personality or resolution of inner conflicts. When asked about sources of information regarding depression, 60% of patients referred to individual clinical psychiatrists while 18.9% cited mass media. These findings indicated that non-pharmacological approaches for depression were necessary and also that clinical psychiatrists required a clinical practice guideline for depression (8).
Although the basic therapeutic approach for depression is pharmacological treatment, clinical psychiatrists considered that non-pharmacological approaches were more essential. However, non-pharmacological treatment guidelines had not been developed in Korea at that time. Hence, the Development Group of the Standardized Treatment Guideline for Depression of the Clinical Research Center for Depression, assigned by the Ministry of Health and Welfare, hoped that the present guideline would promote non-pharmacological approaches to provide alternative or adjuvant therapeutic mode of depression. Since relatively more severe depression essentially requires pharmacological treatment, pharmacological guidelines focus on patients with moderate or severe depression (7). However, according to severity classification of major depressive disorder of the DSM-IV (9), relatively less severe depression can be managed through non-pharmacological approaches. Thus, the 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression in Korea' has been indicated to the Korean adults with mild or moderate depression. We described below a summary of the guideline, which has been developed according to a strict and systematic process using an evidence-based approach.
MATERIALS AND METHODS
Development group
The Development Group for the Standardized Treatment Guideline for Depression was formed as a multidisciplinary team consisting psychiatrists, administrative researchers, clinical psychologists, systematic review experts, and specialists in preventive medicine. Throughout the process of developing the clinical practice guideline, members of the group carried out ongoing comparative assessment and evaluation of all results while performing the investigations and procedures required in order to base the findings on scientific methodology (8).
Range of the guideline
The Development Group investigated pre-existing domestic and international treatment guidelines, as well as trends in the management of depression among Korean psychiatrists. Subsequently, the Development Group analyzed the results of previous investigations (10-50) and developed a non-pharmacological treatment guideline for depression. The Development Group also assessed the domestic status of depression treatments in Korea. The 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression in Korea' was indicated at Korean adult patients with an initial diagnosis of mild or moderate depression by DSM-IV (9).
Key questions
Common self-care methods for depression include bibliotherapy, computer-based treatment, dietary supplements (St. John's wort, S-adenosylmethionine, selenium, vitamin B, C, D, folic acid, Ginkgo biloba, glutamine, tyrosine, natural progesterone, oriental medicine, caffeine, alcohol, omega-3 fatty acids, and others), acupuncture therapy, light therapy, anion therapy, massage therapy, exercise therapy, relaxation therapy, music therapy, hypnotherapy, yoga, meditation, and aromatherapy (51). Among these, the literature evidence was the most convincing for St. John's wort, exercise therapy, bibliotherapy, and light therapy during the winter. In the context of domestic situation in Korea, exercise therapy and bibliotherapy were considered to be worthy of recommendation as first stage of treatments for mild or moderate depression. St. John's wort was not included in this guideline, since it is classified as not a Over-the-Counter (OTC) drug but a prescription medication in Korea. Light therapy was also excluded, because it is not widely clinically-available in Korea. In addition to self-care methods, this guideline addressed psychotherapy methods. For any form of psychotherapy, it is important to consider whether a given method has independent and well-established therapeutic features that justify the title of 'psychotherapy' because an unverified psychotherapy is nothing but a placebo treatment. According to Wampold et al. (52), psychotherapy should have the following key elements to be distinguished from general clinical management or a placebo treatment. First, the therapy is mediated by a trained specialist. Second, the therapist can carry out treatments tailored to the needs of each patient. Third, there should be a unique and clear psychotherapeutic principle that distinguishes it from other forms of psychotherapy. From this viewpoint, only a few kinds of psychotherapy are comparable to pharmacological treatments or placebo controls. These are cognitive-behavioral therapy (CBT), short-term psychodynamic supportive psychotherapy (SPSP), interpersonal psychotherapy (IPT), problem-solving treatment, and marital therapy. Among these, the guideline evaluated three psychotherapies, namely CBT, SPSP, and IPT because these three methods have been supported by theoretical and clinical evidence. In addition, therapeutic and theoretical evidences suggest that these three psychotherapies could be applied to different groups of depressed patients (53). On one hand, both CBT and IPT follow structured procedures with limited numbers of therapy sessions. However, CBT deals with the association between negative emotions and thoughts, while IPT deals with the association between negative emotions and corresponding life-events (mostly, interpersonal). On the other hand, psychodynamic psychotherapy deals with transference relationships, and its treatment principles are based on earlier theories of psychotherapy. Psychodynamic approaches have been claimed by a number of psychotherapists to be effective, but the classical psychoanalytic treatment is not suitable in the management of depression because the treatment is ultimately aimed at self-understanding and personality change. Especially, SPSP is defined as 16-session psychotherapy which focus on the affective, behavioral, and cognitive aspects of interpersonal or intrapersonal relationships (54). As a short term psychodynamic psychotherapy, SPSP recognizes the therapeutic utility of the transference relationship but does not interpret this relationship to the patient. Thus, among a number of self-care or psychotherapeutic methods, the Development Group regarded exercise therapy and bibliotherapy as self-care procedures available for mild or moderate depression, and also considered CBT, SPSP and IPT as available psychotherapeutic methods (8). Hence, our key questions referred to exercise therapy, bibliotherapy, CBT, SPSP, and IPT.
These key questions were designed to elicit accurate and correct answer, usually by employing the "PICO" method. The basic elements of a key question were P, I, C, and O, where P represents patients or the corresponding problems (patient population), I represents an intervention such as diagnostic evaluation, prognostic factors, and treatments (interventions), C represents an alternative intervention with which the former is to be compared (comparison), and O represents clinical outcome (outcome) (55).
Scope and process of literature search
Within the scope expressed in the Core Standard Ideal (COSI), the following literature sources were searched: PubMed, EMBASE, Cochrane CENTRAL, Korea Med, KMbase, RICH, and the National Assembly Library. Since systematic reviews and meta-analyses did not include Korean publications, the administrative researchers were obliged to search the literature manually and extract the contents of the relevant journals to access and evaluate original publications.
Literature search was carried out in several steps, including the development of the search strategy itself. First, the researcher who was responsible for selection of key questions converted the questions into the PICO format (55) and forwarded them to the literature search team. The team extracted preliminary search words and sent them back to the researcher in charge. Second, the team searched the database using the selected search words, listed the initial basic search results and abstracts, and sent this data back to the researcher in charge. Then, the researcher read and judged each abstract and created a list of suitable studies, given the key question being asked. The literature search team obtained the original publications in the list. Third, the researcher in charge received the original publications from the search team, read them carefully, and selected the publications to be used in the systematic review. Finally, the search team searched for published findings of randomized controlled trials (RCTs) conducted after the publication of the most recently selected systematic reviews.
Literature quality and evidence levels
For evaluation of each study, the Development Group used the Scottish Intercollegiate Guidelines Network (SIGN) grading system (56). Meta-analyses and RCT were allocated as top level evidence; un-randomized clinical research and observational research as mid level evidence; and, expert opinion and case reports were allocated as low level evidence. The SIGN systematic review evaluation method was generally used to judge the following criteria: first, if the research questions were carefully chosen and well-focused; second, if there was a methodological description; third, if the literature search was comprehensive enough to discover all the appropriate findings; and fourth, if all the research findings were homogeneous enough to be combined together. Publications in languages other than Korean or English were excluded from the scope of this search. The Development Group had been trained by an expert of evidence-based medicine in evaluating the appropriate literature with experts in methodology, and such efforts were continued to unify the evaluation criteria used by all researchers.
Evidence levels used are summarized in Table 1 (57). These were prepared by systematically summarizing relative research findings to allow readers to compare the results in a single view. In general, the tables included research type and quality, research type, arbitration, confidence intervals, and results.
Table 1.
Evidence levels for the 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression in Korea' (57)
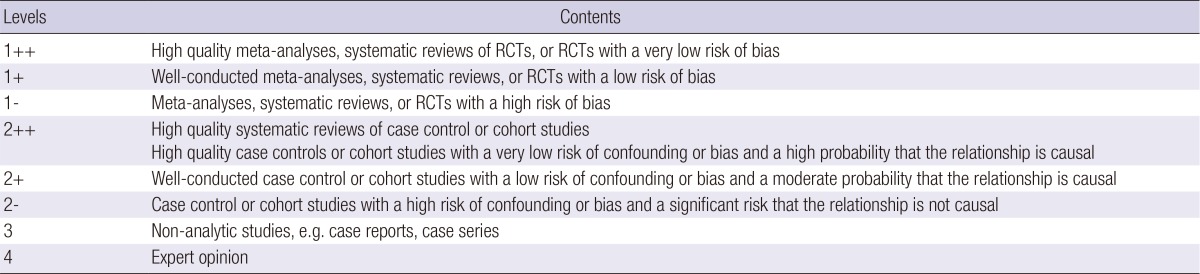
RCTs, Randomized Controlled Trials.
Recommendation grades
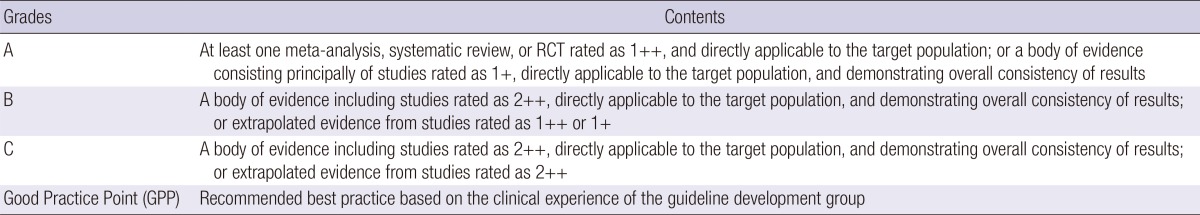
The Development Group classified grades of recommendation into 4 levels, A, B, C, and Good Practice Point (GPP), as indicated in Table 2. GPP is a recommendation grade with an evidence level of 3 or 4 (57). The development of recommendations consisted of synthesizing and analyzing all the data gathered for each key question. However, if findings were diverse or controversial on a certain issue, the evidence was not consistent, most of the claims underlying the evidence were inadequate or poor, or if the evidence had a high evidence level but were of a lower clinical applicability, careful consideration were given to the recommendation grade. As a consequence, expert opinion sometimes influenced recommendation grades, and official agreement amongst all the researchers were used in place of evaluations from a single researcher.
Table 2.
Recommendation grades for the 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression in Korea' (57)
External expert review and academy certification
The Development Group requested external experts to review the draft of the guideline for its feasibility and availability, and the review result was considered for during the revision process after a subsequent internal discussion. The 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression in Korea' was certified at the Annual Meeting of the Korean Neuropsychiatric Association in April, 2010.
RESULTS
Key question 1. Is exercise therapy more efficacious than placebo or antidepressant for adult patients with mild or moderate depression?
Evidence
The evidence for efficacy of exercise therapy is presented in Table 3. Exercise therapy is more efficacious than no treatment for adult patients with mild-to-moderate depression, and its efficacy is similar to that of antidepressant treatment or cognitive behavioral therapy alone (Evidence Level: 1++).
Table 3.
Evidence of the efficacy of exercise therapy for depression
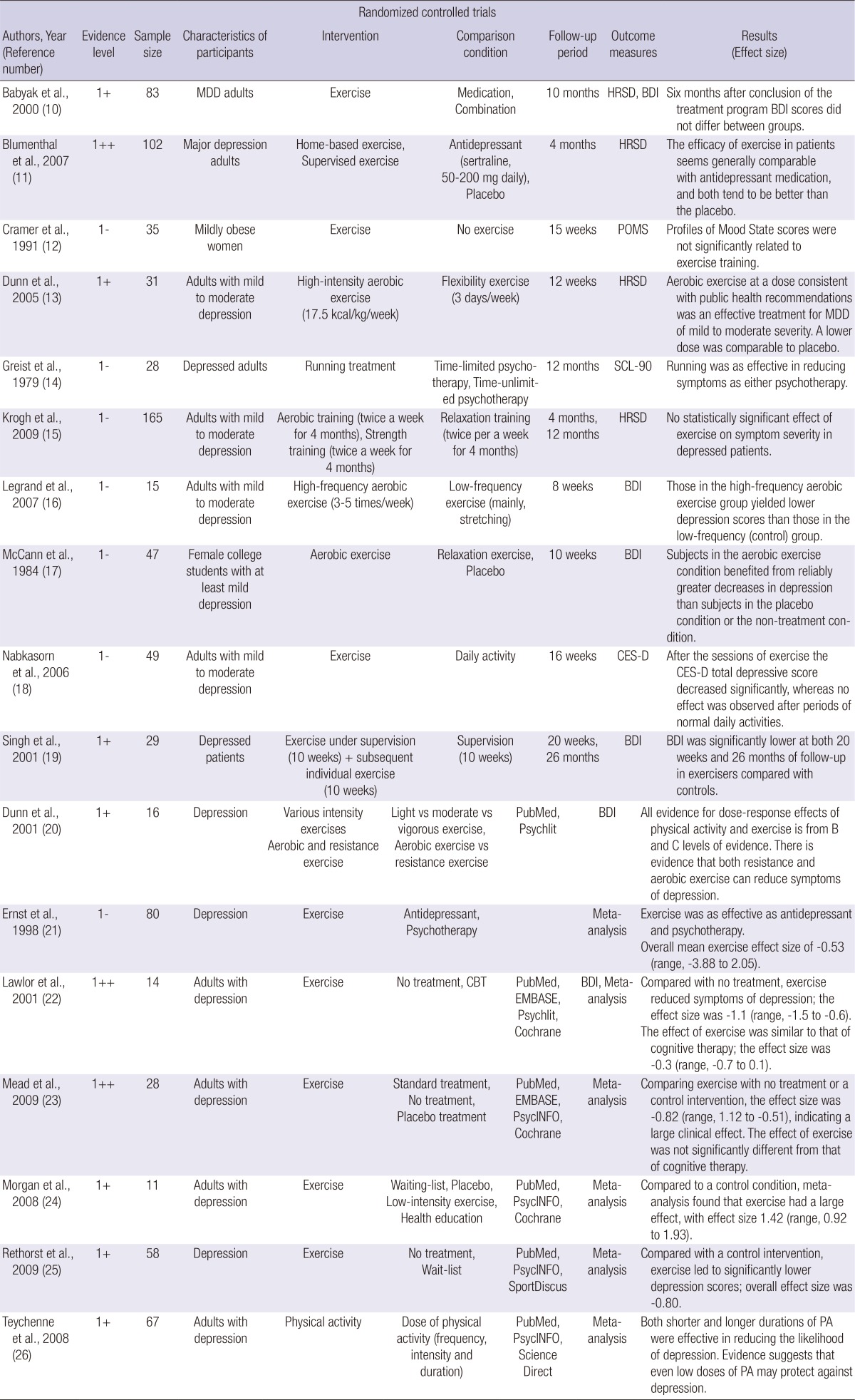
BDI, Beck Depression Inventory; CBT, cognitive behavioral therapy; CES-D, Center for Epidemiological Studies Depression Scale; HRSD, Hamilton Rating Scale for Depression; POMS, Profiles of Mood State; SCL-90, Symptom Checklist-90.
Recommendations
Exercise therapy is recommended for adult patients with mild or moderate depression (Recommendation Grade: A). Structured exercise therapy may be considered a non-pharmacological treatment in adult patients with mild or moderate depression (Recommendation Grade: B).
Key question 2. Is bibliotherapy more efficacious than placebo or antidepressant for adult patients with mild or moderate depression?
Evidence
The evidence for efficacy of bibliotherapy is presented in Table 4. Bibliotherapy decreased the severity of depressive symptoms significantly, and the efficacy was reported to last for up to 6 months (Evidence Level: 1+).
Table 4.
Evidence of the efficacy of bibliotherapy for depression
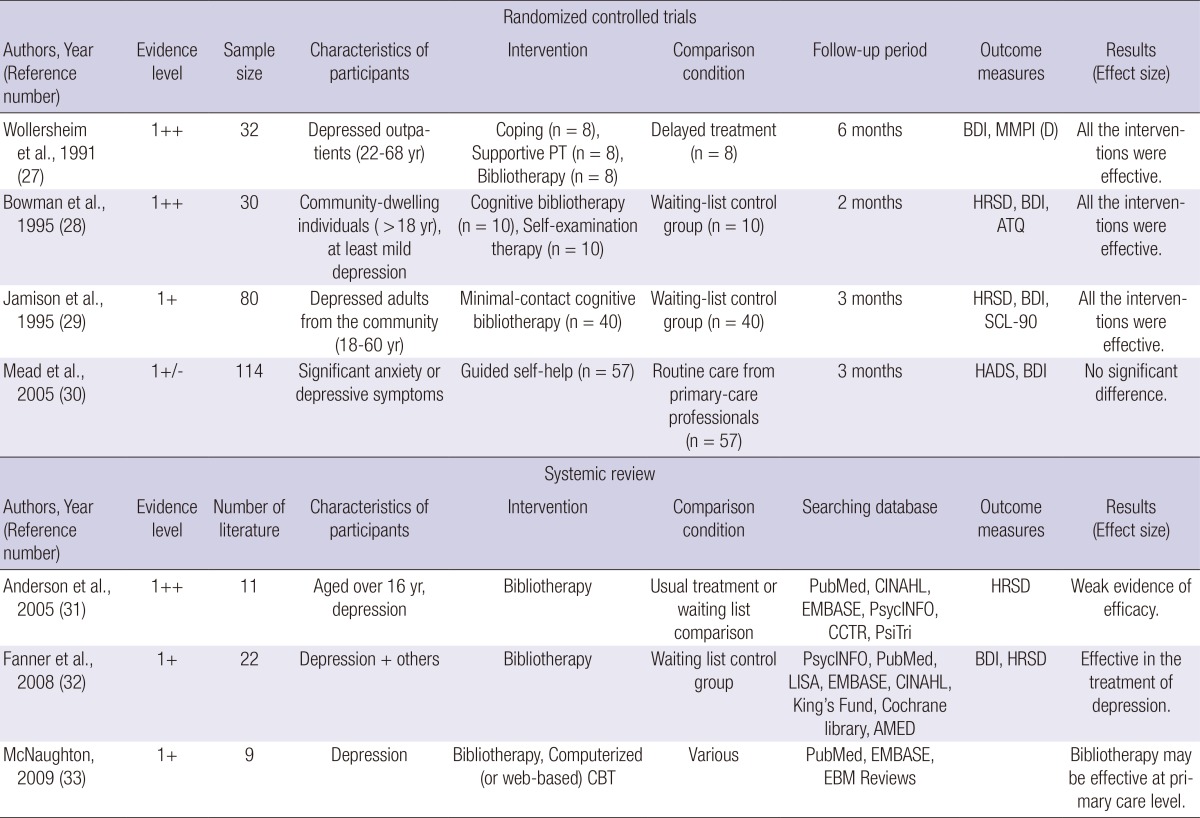
ATQ, Automatic Thought Questionnaire; BDI, Beck Depression Inventory; CBT, cognitive behavioral therapy; HADS, Hospital Anxiety & Depression Scale; HRSD, Hamilton Rating Scale for Depression; MMPI (D), Minnesota Multiphasic Personality Inventory - Depression Scale; SCL-90, Symptom Checklist-90.
Recommendations
Bibliotherapy may be considered a non-pharmacological treatment for adult patients with mild-to-moderate depression (Recommendation Grade: B).
Key question 3. Is cognitive-behavioral therapy (CBT) more efficacious than placebo and antidepressant treatment for adult patients with mild or moderate depression?
Evidence
The evidence for efficacy of CBT is presented in Table 5. CBT was considered to be more efficacious than placebo for adult patients with mild or moderate depression and to be as efficacious as antidepressant treatment alone (Evidence Level: 1+).
Table 5.
Evidence of the efficacy of cognitive behavioral therapy for depression
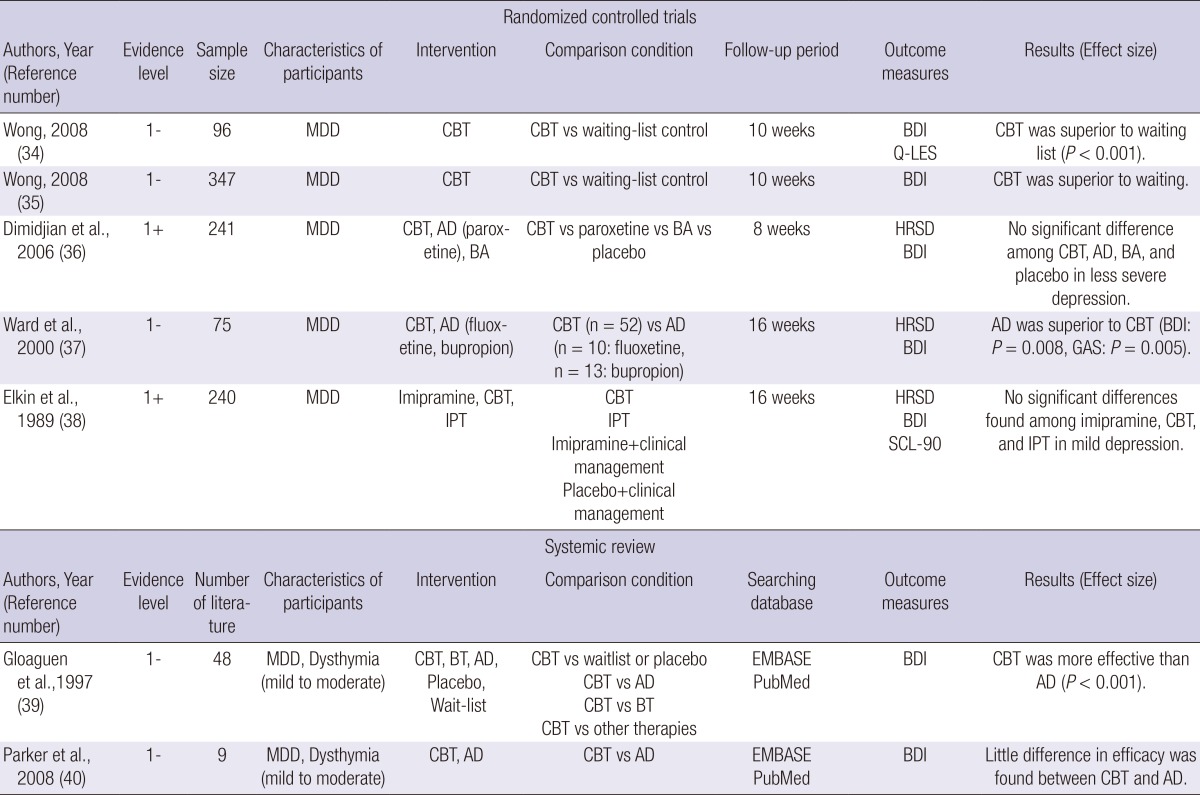
AD, Antidepressant; BA, Behavioral Activation; BDI, Beck Depression Inventory; BT, Behavioral Therapy; CBT, Cognitive Behavioral Therapy; HRSD, Hamilton Rating Scale for Depression; IPT, Interpersonal Psychotherapy; Q-LES, Quality of Life Enjoyment and Satisfaction; MDD, major depressive disorder; SCL-90, Symptom Checklist-90.
Recommendations
CBT may be considered a non-pharmacological treatment for adult patients with mild-to-moderate depression (Recommendation Grade: B).
Key question 4. Is CBT more efficacious than other psychotherapies for adult patients with mild or moderate depression?
Evidence
The evidence for efficacy of CBT is shown in Table 5. The efficacy of CBT appears similar to that of other interpersonal psychotherapies or other kinds of psychotherapy (Evidence level: 1+).
Recommendations
CBT may be considered a non-pharmacological treatment in adult patients with mild-to-moderate depression (Recommendation Grade: B).
Key question 5. Is short-term psychodynamic supportive psychotherapy (SPSP) more efficacious for adult patients with mild or moderate depression than placebo or antidepressant?
Evidence
The evidence for efficacy of SPSP is shown in Table 6. SPSP is expected to have a similar efficacy to pharmacological treatment alone for mild or moderate depression. In particular, combination SPSP-pharmacological therapy may be considered not only for improving depressive symptoms but also for improving social function and reducing the rate of discontinuation of treatment (Evidence Level: 1+).
Table 6.
Evidence of the efficacy of short-term psychodynamic supportive psychotherapy for depression
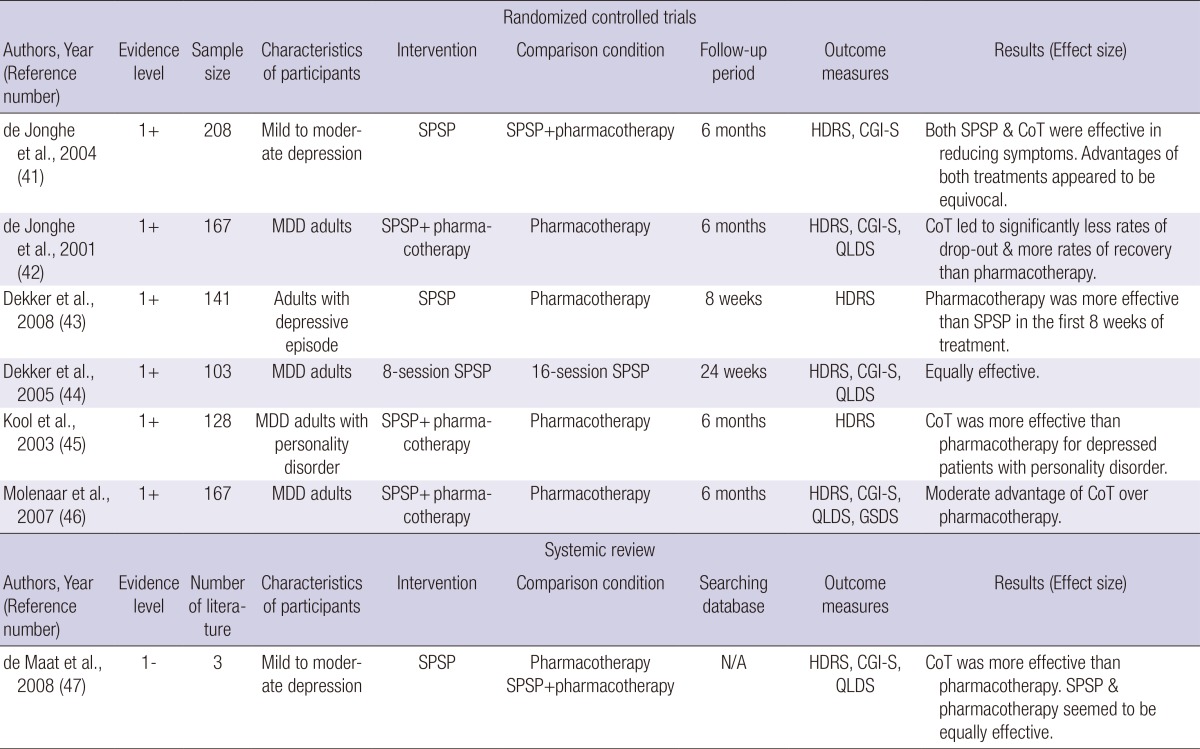
CGI-S, Clinical Global Impression of Severity; CoT, Combined therapy; HDRS, Hamilton Depression Rating Scale; GSDS, Groningen Social Disability Schedule; SPSP, Short-term Psychodynamic Supportive Psychotherapy; QLDS, Quality of Life Depression Scale.
Recommendations
SPSP may be considered a non-pharmacological treatment in adult patients with mild-to-moderate depression (Recommendation Grade: B).
Key question 6. Is interpersonal psychotherapy (IPT) more efficacious for adult patients with mild or moderate depression than placebo or antidepressant?
Evidence
The evidence for efficacy of IPT is shown in Table 7. IPT appeared to be more efficacious than placebo and at least as efficacious as pharmacological treatment alone for adult patients with mild or moderate depression (Evidence Level: 1+).
Table 7.
Evidence of the efficacy of interpersonal psychotherapy for depression
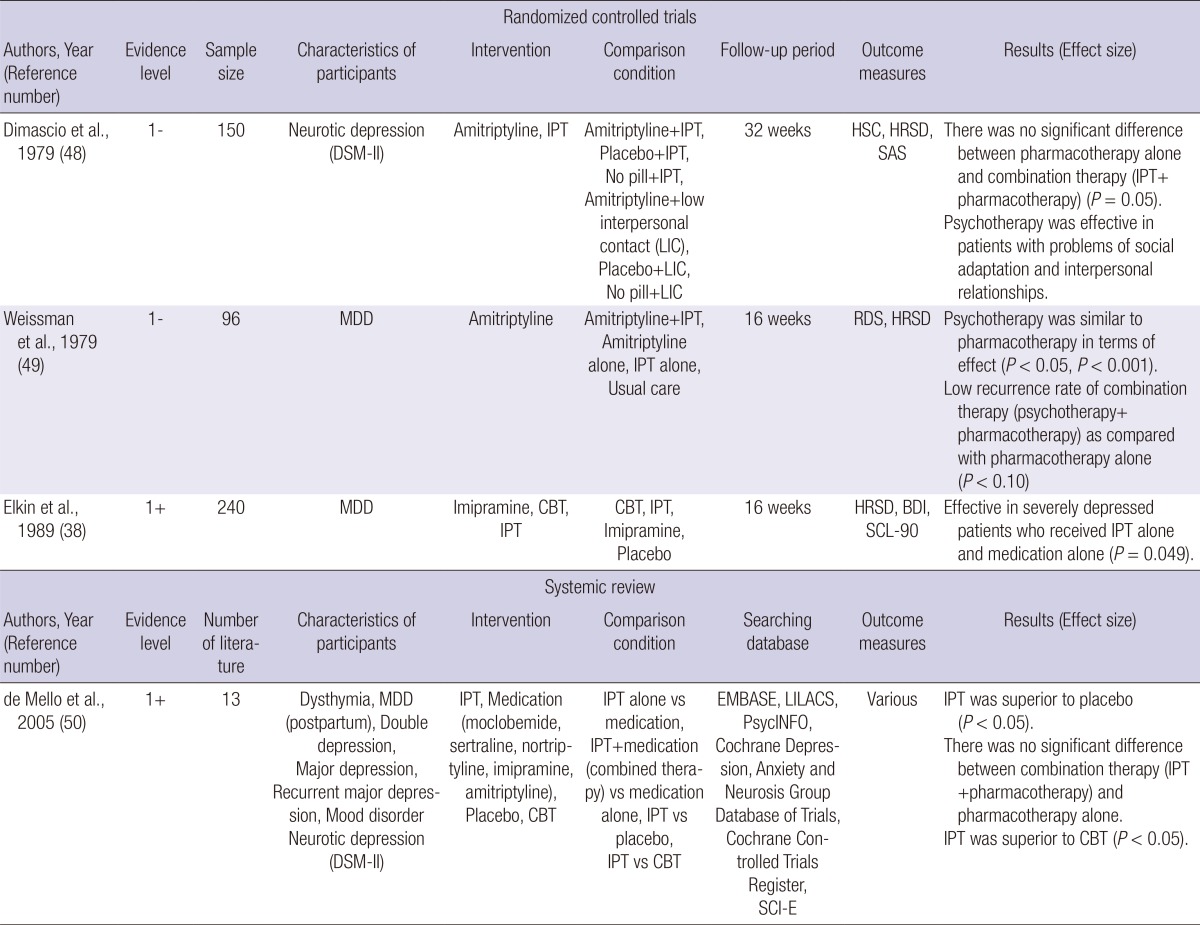
BDI, Beck Depression Inventory; HDRS, Hamilton Depression Rating Scale; IPT, interpersonal psychotherapy; RDS, Raskin Depression Scale; SAS, Self-rating Anxiety Scale; SCL-90, Symptom Checklist-90.
Recommendations
IPT may be considered a non-pharmacological treatment in adult patients with mild or moderate depression (Recommendation Grade: B).
Key question 7. Is combination IPT-pharmacological treatment more efficacious for adult patients with mild or moderate depression than single treatment (IPT or pharmacological treatment alone)?
Evidence
The evidence for efficacy of IPT is given in Table 7. In adult patients with mild or moderate depression, the efficacy of combination of IPT and pharmacological treatment is not significantly greater than that of pharmacological treatment alone, but the combination treatment been suggested to be more efficacious than pharmacological treatment alone for severe depression (Evidence Level: 1+).
Recommendations
The combination of IPT and pharmacological treatment does not seem to be more efficacious than pharmacological treatment alone for mild or moderate depression, but the combination treatment may be considered for severe depression (Recommendation Grade: B).
DISCUSSION
The present guideline was developed to improve the quality of treatment and reduce the differences in clinical practice, inappropriate treatment and treatment cost in the management of Korean adults with mild-to-moderate depression. In addition, evidence-based findings on medical cost, outcomes, and patient preferences have been incorporated in the guideline to support the medical decision-making process. Presently, evidence-based treatment guidelines have been developed in the USA, UK, Canada, New Zealand, and Singapore (3, 4). There are two main reasons why these standardized guidelines have been developed. First, no one individual can keep up with the rate of development of medical knowledge given the increasing number of studies published. Second, expert recommendations often contradict each other, and advice regarding clinical treatment can vary significantly depending on the source of a given knowledge. In Korea, very little high-quality RCTs on the management of depression and the absence of an internet-based domestic literature database have hindered access to what little evidence-based knowledge is available for the treatment of depression.
There are a considerable number of treatments whose efficacy has been verified in favorable clinical trials, and the two most representative of these treatments are pharmacological therapy (mainly, antidepressant) and CBT. However, patients with depression prefer self-care and alternative therapies before seeking either of these two treatments (58), and this is particularly true in Korea (8, 53). In the initial phase of depression, a patient may find self-care desirable, when considering problems of cost, geographical hindrance, time, or the stigma associated with seeking professional psychiatric care. Thus, depression self-care treatments should be considered for the advantages of cost, prevention of adverse effects of pharmacologic therapy, and continuation of psychiatric treatment. Moreover, studies have been frequently reported specific patient groups which responded to these three psychotherapeutic methods (34-50). CBT has been reported to be most efficacious for depressed patients who suffer from anxiety symptoms but has preserved cognitive function. SPSP provides a 'support' aimed at satisfying the developmental needs which until the time of therapy had remained unfulfilled (59). SPSP can be described as being on the supportive side of the traditional 'supportive-expressive' line dividing the two main schools of psychoanalytic psychotherapies. IPT is considered efficacious for patients who are socially well adapted, with short-term psychodynamic psychotherapy reserved for patients with accompanying personality disorders (41, 60). Consequently, this guideline evaluated and reviewed the evidence regarding these three psychotherapies to allow tailored treatment of individual patients in their respective conditions.
A web-based survey for implementation of clinical practice guidelines for depression demonstrated that over half (55.7%) of 386 Korean psychiatrists had clinical experiences with the guide in practice. The obstacles to implement the guidelines for depression were regarded as lack of knowledge, difficulties in accessing the guidelines, lack of support for mental health services, and general attitudes toward guideline necessity. Moreover, adding a summary booklet, providing teaching sessions, and improving guidance delivery systems had been suggested as effective methods for increasing the depression treatment guideline usage (61). These findings can anticipate the limitations and usage increasing tools of the 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression.' The most significant limitation of the guideline was the poverty of evidence from lack of clinical studies within Korea. This was of utmost importance to secure such evidence from studies within Korea, because non-pharmacological treatment is greatly affected by social and cultural norms and practices (62). Moreover, there is no specific bibliotherapy tailored for depression. Likewise, no standardized protocol for SPSP exists, although a specific protocol for IPT has recently been translated and introduced in Korea. Hence, it is important to develop or prepare a Korean-written specific book for bibliotherapy and a Korean version of specific protocol for SPSP. Despite these several limitations, the 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression' has the virtue of the first evidenced-based guideline of non-pharmacological treatments for Korean adults with mild or moderate depression.
CONCLUSIONS
The 'Evidence-Based, Non-Pharmacological Treatment Guideline for Depression in Korea' was developed through a comprehensive systemic review. It proposes that exercise therapy, bibliotherapy, CBT, SPSP, and IPT should be considered as valid non-pharmacological treatments for Korean adult patients with mild or moderate depression. Further development of a Korean-written specific book for bibliotherapy and a Korean version of specific protocol for SPSP is urgently needed in Korea.
Footnotes
This research was supported by a grant from the Korea Health 21 R&D, Ministry of Health and Welfare, Republic of Korea (A102065).
The authors have no conflicts of interest to disclose.
References
- 1.Oh DH, Kim SA, Lee HY, Seo JY, Choi BY, Nam JH. Prevalence and correlates of depressive symptoms in Korean adults: results of a 2009 Korean community health survey. J Korean Med Sci. 2013;28:128–135. doi: 10.3346/jkms.2013.28.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global burden of disease and risk factors. Washington, D.C.: World Bankm; 2006. [PubMed] [Google Scholar]
- 3.Jeon HJ. Epidemiologic studies on depression and suicide. J Korean Med Assoc. 2012;55:322–328. [Google Scholar]
- 4.Lim SW, Lee MS. Korean clinical practice guideline for the treatment of depressive disorders: the present state and future direction of development. Korean J Biol Psychiatry. 2006;13:11–18. [Google Scholar]
- 5.Kang RH, Kim SY, Lee MS. Korean clinical practice guideline for the treatment of depressive disorders (II) Korean J Biol Psychiatry. 2006;13:219–225. [Google Scholar]
- 6.Kim TS, Jeong SH, Kim JB, Lee MS, Kim JM, Yim HW, Jun TY. The clinical research center for depression study: baseline characteristics of a Korean long-term hospital-based observational collaborative prospective cohort study. Psychiatry Investig. 2011;8:1–8. doi: 10.4306/pi.2011.8.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park SC, Sung SH, Han KM, Won ES, Lee HY, Paik JW, Jeon HJ, Lee MS, Shim SH, Ko YH, et al. Evidence-based Korean pharmacological treatment guideline for depression, revised edition (I): initial choice of antidepressant treatment. J Korean Neuropsychiatr Assoc. 2013;52:253–262. [Google Scholar]
- 8.Oh HS, Lee HW, Park YC. The current status and requirements for non-pharmacological treatment of depression in Korea. Korean J Biol Psychiatry. 2007;14:21–27. [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: American Psychiatric Association; 1994. [Google Scholar]
- 10.Babyak M, Blumenthal JA, Herman S, Khatri P, Doraiswamy M, Moore K, Craighead WE, Baldewicz TT, Krishnan KR. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62:633–638. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, Herman S, Craighead WE, Brosse AL, Waugh R, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69:587–596. doi: 10.1097/PSY.0b013e318148c19a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cramer SR, Nieman DC, Lee JW. The effects of moderate exercise training on psychological well-being and mood state in women. J Psychosom Res. 1991;35:437–449. doi: 10.1016/0022-3999(91)90039-q. [DOI] [PubMed] [Google Scholar]
- 13.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Greist JH, Klein MH, Eischens RR, Faris J, Gurman AS, Morgan WP. Running as treatment for depression. Compr Psychiatry. 1979;20:41–54. doi: 10.1016/0010-440x(79)90058-0. [DOI] [PubMed] [Google Scholar]
- 15.Krogh J, Saltin B, Gluud C, Nordentoft M. The DEMO trial: a randomized, parallel-group, observer-blinded clinical trial of strength versus aerobic versus relaxation training for patients with mild to moderate depression. J Clin Psychiatry. 2009;70:790–800. doi: 10.4088/jcp.08m04241. [DOI] [PubMed] [Google Scholar]
- 16.Legrand F, Heuze JP. Antidepressant effects associated with different exercise conditions in participants with depression: a pilot study. J Sport Exerc Psychol. 2007;29:348–364. doi: 10.1123/jsep.29.3.348. [DOI] [PubMed] [Google Scholar]
- 17.McCann IL, Holmes DS. Influence of aerobic exercise on depression. J Pers Soc Psychol. 1984;46:1142–1147. doi: 10.1037//0022-3514.46.5.1142. [DOI] [PubMed] [Google Scholar]
- 18.Nabkasorn C, Miyai N, Sootmongkol A, Junprasert S, Yamamoto H, Arita M, Miyashita K. Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. Eur J Public Health. 2006;16:179–184. doi: 10.1093/eurpub/cki159. [DOI] [PubMed] [Google Scholar]
- 19.Singh NA, Clements KM, Singh MA. The efficacy of exercise as a long-term antidepressant in elderly subjects: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2001;56:M497–M504. doi: 10.1093/gerona/56.8.m497. [DOI] [PubMed] [Google Scholar]
- 20.Dunn AL, Trivedi MH, O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33:S587–S597. doi: 10.1097/00005768-200106001-00027. [DOI] [PubMed] [Google Scholar]
- 21.Ernst E, Rand JI, Stevinson C. Complementary therapies for depression: an overview. Arch Gen Psychiatry. 1998;55:1026–1032. doi: 10.1001/archpsyc.55.11.1026. [DOI] [PubMed] [Google Scholar]
- 22.Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomised controlled trials. BMJ. 2001;322:763–767. doi: 10.1136/bmj.322.7289.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mead GE, Morley W, Campbell P, Greig CA, McMurdo M, Lawlor DA. Exercise for depression. Cochrane Database Syst Rev. 2009;3:CD004366. doi: 10.1002/14651858.CD004366.pub4. [DOI] [PubMed] [Google Scholar]
- 24.Morgan AJ, Jorm AF. Self-help interventions for depressive disorders and depressive symptoms: a systematic review. Ann Gen Psychiatry. 2008;7:13. doi: 10.1186/1744-859X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rethorst CD, Wipfli BM, Landers DM. The antidepressive effects of exercise: a meta-analysis of randomized trials. Sports Med. 2009;39:491–511. doi: 10.2165/00007256-200939060-00004. [DOI] [PubMed] [Google Scholar]
- 26.Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med. 2008;46:397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Wollersheim JP, Wilson GL. Group treatment of unipolar depression: a comparison of coping, supportive, bibliotherapy, and delayed treatment groups. Prof Psychol Res Pr. 1991;22:496–502. [Google Scholar]
- 28.Bowman D, Scogin F, Lyrene B. The efficacy of self-examination therapy and cognitive bibliotherapy in the treatment of mild-to-moderate depression. Psychother Res. 1995;5:131–140. [Google Scholar]
- 29.Jamison C, Scogin F. The outcome of cognitive bibliotherapy with depressed adults. J Consult Clin Psychol. 1995;63:644–650. doi: 10.1037//0022-006x.63.4.644. [DOI] [PubMed] [Google Scholar]
- 30.Mead N, MacDonald W, Bower P, Lovell K, Richards D, Roberts C, Bucknall A. The clinical effectiveness of guided self-help versus waiting-list control in the management of anxiety and depression: a randomized controlled trial. Psychol Med. 2005;35:1633–1643. doi: 10.1017/S003329170500560X. [DOI] [PubMed] [Google Scholar]
- 31.Anderson L, Lewis G, Araya R, Elgie R, Harrison G, Proudfoot J, Schmidt U, Sharp D, Weightman A, Williams C. Self-help books for depression: how can practitioners and patients make the right choice? Br J Gen Pract. 2005;55:387–392. [PMC free article] [PubMed] [Google Scholar]
- 32.Fanner D, Urquhart C. Bibliotherapy for mental health service users Part 1: a systematic review. Health Info Libr J. 2008;25:237–252. doi: 10.1111/j.1471-1842.2008.00821.x. [DOI] [PubMed] [Google Scholar]
- 33.McNaughton JL. Brief interventions for depression in primary care: a systematic review. Can Fam Physician. 2009;55:789–796. [PMC free article] [PubMed] [Google Scholar]
- 34.Wong DF. Cognitive behavioral treatment groups for people with chronic depression in Hong Kong: a randomized wait-list control design. Depress Anxiety. 2008;25:142–148. doi: 10.1002/da.20286. [DOI] [PubMed] [Google Scholar]
- 35.Wong DF. Cognitive and health-related outcomes of group cognitive behavioural treatment for people with depressive symptoms in Hong Kong: randomized wait-list control study. Aust N Z J Psychiatry. 2008;42:702–711. doi: 10.1080/00048670802203418. [DOI] [PubMed] [Google Scholar]
- 36.Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Gallop R, McGlinchey JB, Markley DK, Gollan JK, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- 37.Ward E, King M, Lloyd M, Bower P, Sibbald B, Farrelly S, Gabbay M, Tarrier N, Addington-Hall J. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy, and usual general practitioner care for patients with depression: I: clinical effectiveness. BMJ. 2000;321:1383–1388. doi: 10.1136/bmj.321.7273.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, Glass DR, Pilkonis PA, Leber WR, Docherty JP, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry. 1989;46:971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- 39.Gloaguen V, Cottraux J, Cucherat M, Blackburn IM. A meta-analysis of the effects of cognitive therapy in depressed patients. J Affect Disord. 1998;49:59–72. doi: 10.1016/s0165-0327(97)00199-7. [DOI] [PubMed] [Google Scholar]
- 40.Parker GB, Crawford J, Hadzi-Pavlovic D. Quantified superiority of cognitive behaviour therapy to antidepressant drugs: a challenge to an earlier meta-analysis. Acta Psychiatr Scand. 2008;118:91–97. doi: 10.1111/j.1600-0447.2008.01196.x. [DOI] [PubMed] [Google Scholar]
- 41.De Jonghe F, Hendricksen M, van Aalst G, Kool S, Peen V, Van R, van den Eijnden E, Dekker J. Psychotherapy alone and combined with pharmacotherapy in the treatment of depression. Br J Psychiatry. 2004;185:37–45. doi: 10.1192/bjp.185.1.37. [DOI] [PubMed] [Google Scholar]
- 42.De Jonghe F, Kool S, van Aalst G, Dekker J, Peen J. Combining psychotherapy and antidepressants in the treatment of depression. J Affect Disord. 2001;64:217–229. doi: 10.1016/s0165-0327(00)00259-7. [DOI] [PubMed] [Google Scholar]
- 43.Dekker JJ, Koelen JA, Van HL, Schoevers RA, Peen J, Hendriksen M, Kool S, Van Aalst G, De Jonghe F. Speed of action: the relative efficacy of short psychodynamic supportive psychotherapy and pharmacotherapy in the first 8 weeks of a treatment algorithm for depression. J Affect Disord. 2008;109:183–188. doi: 10.1016/j.jad.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 44.Dekker J, Molenaar PJ, Kool S, Van Aalst G, Peen J, de Jonghe F. Dose-effect relations in time-limited combined psycho-pharmacological treatment for depression. Psychol Med. 2005;35:47–58. doi: 10.1017/s0033291704002685. [DOI] [PubMed] [Google Scholar]
- 45.Kool S, Dekker J, Duijsens IJ, de Jonghe F, Puite B. Changes in personality pathology after pharmacotherapy and combined therapy for depressed patients. J Pers Disord. 2003;17:60–72. doi: 10.1521/pedi.17.1.60.24058. [DOI] [PubMed] [Google Scholar]
- 46.Molenaar PJ, Dekker J, Van R, Hendriksen M, Vink A, Schoevers RA. Does adding psychotherapy to pharmacotherapy improve social functioning in the treatment of outpatient depression? Depress Anxiety. 2007;24:553–562. doi: 10.1002/da.20254. [DOI] [PubMed] [Google Scholar]
- 47.De Maat S, Dekker J, Schoevers R, van Aalst G, Gijsbers-van Wijk C, Hendriksen M, Kool S, Peen J, Van R, de Jonghe F. Short psychodynamic supportive psychotherapy, antidepressants, and their combination in the treatment of major depression: a mega-analysis based on three randomized clinical trials. Depress Anxiety. 2008;25:565–574. doi: 10.1002/da.20305. [DOI] [PubMed] [Google Scholar]
- 48.DiMascio A, Weissman MM, Prusoff BA, Neu C, Zwilling M, Klerman GL. Differential symptom reduction by drugs and psychotherapy in acute depression. Arch Gen Psychiatry. 1979;36:1450–1456. doi: 10.1001/archpsyc.1979.01780130068008. [DOI] [PubMed] [Google Scholar]
- 49.Weissman MM, Prusoff BA, Dimascio A, Neu C, Goklaney M, Klerman GL. The efficacy of drugs and psychotherapy in the treatment of acute depressive episodes. Am J Psychiatry. 1979;136:555–558. [PubMed] [Google Scholar]
- 50.De Mello MF, de Jesus Mari J, Bacaltchuk J, Verdeli H, Neugebauer R. A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. Eur Arch Psychiatry Clin Neurosci. 2005;255:75–82. doi: 10.1007/s00406-004-0542-x. [DOI] [PubMed] [Google Scholar]
- 51.Lee SH, Park YC. Self care in depression. Korean J Biol Psychiatry. 2007;14:5–13. [Google Scholar]
- 52.Wampold BE, Mondin GW, Moody M, Stich F, Benson K, Ahn H. A meta-analysis of outcome studies comparing bona fide psychotherapies: empirically, "all must have prizes". Psychol Bull. 1997;122:203–215. [Google Scholar]
- 53.Roh S, Park YC. Characteristics of depression in Korea and non-pharmacological treatment. Korean J Biol Psychiatry. 2006;13:226–233. [Google Scholar]
- 54.Van HL, Dekker J, Koelen J, Kool S, van Aalst G, Hendriksen M, Peen J, Schoevers R. Patient preference compared with random allocation in short-term psychodynamic supportive psychotherapy with indicated addition of pharmacotherapy for depression. Psychother Res. 2009;19:205–212. doi: 10.1080/10503300802702097. [DOI] [PubMed] [Google Scholar]
- 55.Huang X, Lin J, Demner-Fushman D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Annu Symp Proc. 2006;2006:359–363. [PMC free article] [PubMed] [Google Scholar]
- 56.Petrie JC, Grimshaw JM, Bryson A. The Scottish Intercollegiate Guidelines Network Initiative: getting validated guidelines into local practice. Health Bull (Edinb) 1995;53:345–348. [PubMed] [Google Scholar]
- 57.Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A, Schünemann HJ GRADE Working Group. Going from evidence to recommendations. BMJ. 2008;336:1049–1051. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jorm AF, Christensen H, Griffiths KM, Rodgers B. Effectiveness of complementary and self-help treatments for depression. Med J Aust. 2002;176:S84–S96. doi: 10.5694/j.1326-5377.2002.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 59.De Jonghe F, Rijnierse P, Janssen R. Psychoanalytic supportive psychotherapy. J Am Psychoanal Assoc. 1994;42:421–446. doi: 10.1177/000306519404200205. [DOI] [PubMed] [Google Scholar]
- 60.Cutler JL, Goldyne A, Markowitz JC, Devlin MJ, Glick RA. Comparing cognitive behavior therapy, interpersonal psychotherapy, and psychodynamic psychotherapy. Am J Psychiatry. 2004;161:1567–1573. doi: 10.1176/appi.ajp.161.9.1567. [DOI] [PubMed] [Google Scholar]
- 61.Yang J, Han C, Yoon HK, Pae CU, Kim MJ, Park SY, Ahn J. Experiences and barriers to implementation of clinical practice guideline for depression in Korea. BMC psychiatry. 2013;13:150. doi: 10.1186/1471-244X-13-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Park YC, Kim KI. The psychiatric practices relevant to the Korean culture. Ment Health Res. 1998;17:4–17. [Google Scholar]


