Abstract
Benign metastasizing leiomyoma (BML) is composed of well-differentiated smooth muscle cells and dense connective tissue. BML affects middle-aged women who have had previous hysterectomies due to a histologically benign-appearing uterine leiomyoma. We report here on a case of BML from the uterine leiomyoma in a 39-year-old woman that involved the soft tissues, skeletal muscles, lungs and breasts. She underwent a hysterectomy for the uterine leiomyoma, double oophorectomy for hormonal ablation and lung wedge resection to confirm the diagnosis. The microscopic findings of the breast and lung tumor were similar to those of the benign uterine leiomyoma. Therefore, we consider that these lesions were breast and pulmonary metastases of the uterine leiomyoma. We report here on a rare case of benign metastasizing uterine leiomyoma that involved the soft tissue, skeletal muscles, lungs and breasts, and we include a review of the relevant literature.
Keywords: Benign metastasizing leiomyoma, Uterine leiomyoma
INTRODUCTION
Benign metastasizing leiomyoma (BML) was first identified by Steiner in 1939, and as he believed it to be a primary lung neoplasm, BML was first referred to as fibroleiomyomatous hamartoma. About 100 cases have been reported in the literature through 20031). The term refers to a type of lesion that is characterized by well-circumscribed, singular or often multiple nodules of proliferating smooth muscle cells in the lungs of women who have a history of hysterectomy. Such lesions have commonly been reported in young premenopausal women whose resected uteri have displayed leiomyomatous alterations without any indication of malignancy. Most women are diagnosed after an incidental abnormal chest radiograph. Because both the benign uterine tumors and the pulmonary tumors have been found to depend on the estrogen/progesterone status, this tumors' growth is mainly hormone dependent2). Hormone-level changes that occur during pregnancy and menopause may have an affect on the general course of the disease. We report here on a rare case of multiple BML in a woman with a history of uterine myomectomy that involved her soft tissue, skeletal muscle, lungs and breasts.
CASE REPORT
A 39-year-old woman was referred to our hospital. At the age of 19, she was treated for miliary pulmonary tuberculosis because multiple pulmonary nodules were found on her chest radiograph, although she had no symptoms. At the age of 31, she was diagnosed uterine leiomyoma, but she was not treated; four years later, she underwent myomectomy. At the age of 39, she visited a local clinic due to bilateral, multiple small nodular lesions that were seen on a chest radiograph and both breasts had palpable breast masses. She had undergone excisional biopsy of the breast before being referred to our hospital.
The patient was asymptomatic on admission to our clinic, but bilateral, multiple small nodular lesions were still noted on the chest radiograph (Figure 1). There was no abnormality on the physical examination, and her breathing sounds were clear. A complete blood count, blood chemistry, c-reactive protein, arterial blood gas analysis and pulmonary function test were all within the normal ranges. The serum levels of tumor markers including alpha-fetoprotein (AFP), squamous cell carcinoma (SCC) antigen and carcinoembryonic antigen (CEA), CA19-9, CA-125 and CA15-3 were within the normal ranges.
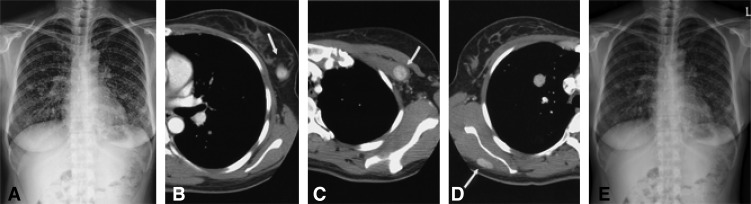
Figure 1.
Radiologic findings of benign metastasizing leiomyoma in a 39-year-old woman. The chest radiograph (A) shows multiple, variable-sized nodules in both lungs, suggesting hematogenous metastasis. Chest CT scans with intravenous contrast enhancement demonstrate multiple, well-enhancing masses in the left breast (B, arrow), the left pectoralis minor muscle (C, arrow), and the right infraspinatus muscle (D, arrow). The follow-up chest radiography (E) showed the decreased size of the multiple nodular lesions.
The chest radiograph showed multiple, variable-sized nodules in both lungs, suggesting hematogenous metastasis (Figure 1A). Chest CT scans with intravenous contrast enhancement demonstrated multiple well-enhancing masses in both breasts (Figure 1B), the left pectoralis minor muscle (Figure 1C), and the right infraspinatus muscle (Figure 1D). A CT scan obtained with a lung window setting showed multiple variable-sized nodules in both lungs, which suggested hematogenous metastasis (not shown).
We initially planned to treat her with progesterone under the clinical impression of BML or lymphangioleiomyomatosis (LAM). However, the follow-up chest radiologic findings showed progressive disease, and so we performed a hysterectomy, bilateral oophorectomy and wedge resection of the lung for the purpose of both treatment and diagnosis.
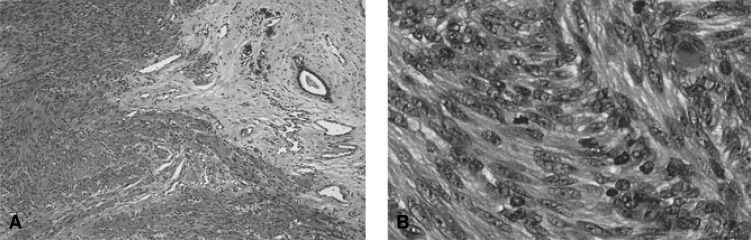
The pathologic findings of the lung, breast (Figure 2A), and retroperitoneal tissue showed nodular proliferations of spindle cells. The tumor showed occasional mitotic activity (4-7/50HPF) (Figure 2B), but no nuclear atypia, hemorrhage or necrosis. Immunohistochemial staining of the lung mass showed a positive reaction for smooth muscle actin and a negative reaction for thyroid transcription factor-1 (TTF-1), a 10% positive cell area with a weak intensity for estrogen receptor, a 95% positive cell area with a strong intensity for progesterone receptor and a low mitotic index (less than 5%) for Ki-67.
Figure 2.
Breast (A, H&E stain ×200) showed nodular proliferation of smooth muscle cells. The tumor shows occasional mitotic activity (4-7/HPF) (B, H&E stain ×400), but no nuclear atypia, hemorrhage or necrosis.
After surgical hormonal ablation, she was prescribed tamoxifen. Follow-up chest radiography (Figure 1E) showed the decreased size of the multiple nodular lesions. This response has been sustained until the present.
DISCUSSION
In 1939, Steiner first proposed the contradictory term of benign metastasizing fibroleiomyoma. This mainly occurs in the uterus, but it can occur in other locations such as skin, lung, trachea, bladder, esophagus, liver and adrenal gland. Leiomyoma is a benign tumor of well-differentiated smooth muscle tissue and vascular collagenous tissue, and it mainly occurs in the uterus. BML has been described as originating from a uterine smooth muscle tumor of unknown malignant potential, but because of the limits of histopathologic testing, this tumor cannot easily be classified as having a malignant potential3).
This disease is common in middle-aged women. Bachmann and Wolff reported that BML occurs in 36- to 64- (average 44-) years-old women and it shows variable clinical courses from chronic inactive lesions to acute respiration distress syndrome (ARDS) followed by death4).
The chromosomal abnormalities associated with BML have been difficult to characterize. Approximately 25% of the uterine leiomyomas may have a balance translocation, the most common of which are t(12;14)(q13-15;q23-24), del(70q21.2q31.2), trisomy 12 and rearrangements of 6p5). Tietze et al. have reported a case of BML in which tumors from both the uterus and lung were characterized as being monoclonal smooth muscle proliferations with identical X-chromosome inactivation and a balanced karyotype; this is very consistent with a clonal metastasizing process6).
Pulmonary tumors in BML can be treated with bronchoscopic resection, conservative pulmonary surgery and hormonal manipulation. Surgical hormonal management can be accomplished with performing bilateral oophorectomy. The medical hormonal management includes the use of luteinizing hormone-releasing hormone analogue, tamoxifen, progesterone, and aromatase inhibitors.
Because of the limited number of therapeutic options, the use of new drugs or new therapeutic modalities should be considered. The recent interest in the c-kit expression in low-grade leiomyosarcoma and gastrointestinal stromal tumor has led investigators to explore using the novel tyrosine kinase inhibitor, STI571 (Gleevec, Novartis Pharmaceuticals, Basel, Switzerland). STI571 has been reported to suppress the expression of c-kit, abl and platelet-derived growth factors. The histologic similarities between low-grade leiomyosarcoma and BML led us to test for c-kit (CD117) because we thought that the presence of c-kit expression in BML may be of academic interest. However, the c-kit was negative in this case.
The treatment modalities for BML are administering progesterone, medical castration using luteinizing hormone-releasing hormone analogue, bilateral oophorectomy, radiation therapy to the ovary and chemotherapy. It is thought that progesterone down-regulates the estrogen receptor so that estrogen is less active. Because our patient's radiographic findings did not show regression despite progesterone therapy, she underwent a hysterectomy with oophorectomy for achieving surgical hormonal ablation.
When possible, a combination of medical and surgical treatment has to be considered to arrive at an effective therapeutic plan. We report here on a rare case of BML with multiple metastasis in the soft tissue, skeletal muscle, lungs and breasts.
References
- 1.Pitts S, Oberstein EM, Glassberg MK. Benign metastasizing leiomyoma and lymphangioleiomyomatosis: sex-specific diseases? Clin Chest Med. 2004;25:343–360. doi: 10.1016/j.ccm.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 2.Takemura G, Takatsu Y, Kaitani K, Ono M, Ando F, Tanada S, Niwa H, Tankawa H, Fujiwara T, Yamabe H. Metastasizing uterine leiomyoma: a case with cardiac and pulmonary metastasis. Pathol Res Pract. 1996;192:622–629. doi: 10.1016/S0344-0338(96)80116-6. [DOI] [PubMed] [Google Scholar]
- 3.Andrade LA, Torresan RZ, Sales JF, Jr, Vicentini R, DeSouza GA. Intravenous leiomyomatosis of the uterus: a report of three cases. Pathol Oncol Res. 1998;4:44–47. doi: 10.1007/BF02904695. [DOI] [PubMed] [Google Scholar]
- 4.Bachman D, Wolff M. Pulmonary metastases from benign appearing smooth muscle tumors of the uterus. AJR Am J Roentgenol. 1976;127:441–446. doi: 10.2214/ajr.127.3.441. [DOI] [PubMed] [Google Scholar]
- 5.Esteban JM, Allen WM, Schaerf RH. Benign metastasizing leiomyoma of the uterus: histologic and immunohistochemical characterization of primary and metastatic lesions. Arch Pathol Lab Med. 1999;123:960–962. doi: 10.5858/1999-123-0960-BMLOTU. [DOI] [PubMed] [Google Scholar]
- 6.Evans AJ, Wiltshaw E, Kochanowski SJ, Macfarlane A, Sears RT. Metastasizing leiomyoma of the uterus and hormonal manipulations. Br J Obstet Gynaecol. 1986;93:646–648. doi: 10.1111/j.1471-0528.1986.tb08043.x. [DOI] [PubMed] [Google Scholar]