Abstract
Purpose
Ocular trauma remains an important cause of visual morbidity worldwide. A previous population-based study in Scotland reported a 1-year cumulative incidence of 8.14 per 100 000 population. The purpose of this study was to identify any change in the incidence and pattern of serious ocular trauma in Scotland.
Methods
This study was a 1-year prospective observational study using the British Ophthalmological Surveillance Unit reporting scheme among Scottish ophthalmologists. Serious ocular trauma was defined as requiring hospital admission. Data were collected using two questionnaires for each patient 1 year apart.
Results
The response rate from ophthalmologists was 77.1%. There were 102 patients reported with complete data giving an incidence of 1.96 per 100 000 population, four times less than in 1992. In patients younger than 65 years, the age-adjusted incidence ratio (males/females) indicated a ninefold higher risk of trauma in males. In 25 patients (27.2%), the injured eye was blind (final visual acuities (FVA) <6/60), 24 being attributable to the eye injury. Standardised morbidity ratios suggested a threefold decrease in risk of poor visual outcome in 2009 compared with 1992.
Conclusions
The incidence of serious ocular trauma has fallen; this study has shown hospital admission for serious eye injury in Scotland has decreased fourfold in 17 years. Young adult males continue to be at highest risk, which needs to be specifically addressed in future health-prevention strategies. This study also observed a reduction in visual loss from serious ocular injuries, although the reasons for this require further exploration.
Keywords: ocular trauma, epidemiology, prevention, penetrating injury
Introduction
Ocular trauma is an important cause of avoidable visual morbidity worldwide, especially to children and young adults. Globally more than half a million blinding injuries occur every year and there are ∼1.6 million people blind from eye injuries, 2.3 million bilaterally visually impaired and 19 million with unilateral visual loss.1 Therefore, eye injuries are a significant burden to health care.
An earlier population-based study in Scotland2 reported a 1-year cumulative incidence of serious ocular trauma (necessitating admission to hospital) to be 8.14 per 100 000 population. At discharge, 13.2% of these patients had a visual acuity less than 6/12. The home was the most frequent place for blinding injury to occur (52%). Results from the United States showed a 4.4% decrease in hospital admission for ocular trauma between 1992 and 2001.3 The purpose of this current study was to identify any change in the incidence and pattern of serious ocular trauma, and to report on the subsequent visual outcome.
Materials and methods
This was a 1-year population-based, prospective study of ocular trauma. Cases were identified using active surveillance through the well-established British Ophthalmological Surveillance Unit (BOSU) reporting scheme.4 During the study period between 1 November 2008 and 31 October 2009, all consultant ophthalmologists in Scotland were sent a card once a month asking them to report whether or not they had seen any newly diagnosed cases of serious ocular trauma, defined as ‘an injury or wound to the eye or adnexae caused by external force or violence, which requires admission to hospital for observation or treatment'. Ethical approval was granted by the Newcastle and North Tyneside 1 Research Ethics Committee (Reference 08/H0906/70).
Following positive case notification to BOSU, reporting ophthalmologists were sent a detailed questionnaire to ascertain demographic data, cause of the injury, the presenting features and initial management of the injury. Data on outcome and secondary management were obtained from follow-up questionnaires sent out 12 months after the injury. Ophthalmologists who did not return questionnaires received reminder letters at 2 and 3 months after the initial questionnaire was sent.
National discharge data from the Scottish Morbidity Records (SMR01) covering the study period were obtained to ascertain completeness of reporting of events, using the International Classification of Diseases (ICD10)5 codes for ocular trauma shown in Table 1.
Table 1. The diagnostic codes that were used from International Classification of Diseases (ICD10)5 to search the Scottish Morbidity Records (SMR01) for the study period.
| S00.1—Contusion of eyelid and periocular area |
| S00.2—Other superficial injuries of eyelid and periocular area |
| S01.1—Open wound of eye and periocular area |
| S02.1—Fracture of base of skull includes orbital roof |
| S02.3—Fracture of orbital floor |
| S02.8—Fractures of other skull and facial bones |
| S04.1—Injury of oculomotor nerve |
| S04.2—Injury of trochlear nerve |
| S04.4—Injury of trigeminal nerve |
| S05—Injury of eye and orbit |
Statistical methods
Mid-2009 population estimates for Scotland were obtained from the General Register Office for Scotland (2010). Exact binomial 95% confidence intervals (CIs) were calculated for proportions. The Mantel–Haenszel methods for stratified data were used to estimate age-adjusted or age/gender-adjusted incidence ratios, for example, for comparison of ocular trauma incidence in males and females. Data were analysed by using Stata software, version 9 (StataCorp, College Station, TX, USA).
Results
Response rate
The response rate from consultants over the year for returning reporting cards was 77.1%. Of the cases reported, 89% of questionnaires were completed and returned for both admission and follow-up data.
Completeness of case ascertainment
The SMR01 data identified 274 patients who had been admitted to hospital during the study period with a principal diagnosis relating to ocular trauma (Table 1). These included patients with injuries such as orbital fractures, who may not have been admitted under the care of a consultant ophthalmologist, and as such not reported in the study.
Incidence of serious ocular trauma
Overall, a total of 102 individuals with completed questionnaires were reported as being admitted to hospital with ocular trauma during the 12-month study period, amounting to a 1-year cumulative incidence of 1.96 per 100 000 population in Scotland.
The age-specific incidence figures for males and for females are shown in Table 2. The highest incidence occurred in the age group 15–64 years. The incidence was substantially lower in females compared with males at all ages except for the 75–84 year age group. In persons younger than 65 years, the age-adjusted incidence ratio (males/females) was 9.08 indicating around nine times higher risk in males. A test of homogeneity yielded a P-value of 0.862, indicating uniformity of the incidence ratios across the age strata. In those 65 years and older, however, the higher risk in men was much less pronounced, the age-adjusted incidence ratio being 1.70, with a wide CI that included 1. The homogeneity test P-value was 0.612.
Table 2. One-year cumulative incidence of ocular trauma admitted to hospital in Scotland.
|
Resident cases admitted with ocular trauma (n) |
1-year cumulative incidence per 100 000 population (95% CI) |
||||||
|---|---|---|---|---|---|---|---|
| Age (years) | Males | Females | All | Males | Females | All | |
| 0–4 | 1 | 0 | 1 | 0.68 | 0.00 | 0.35 | |
| 5–14 | 7 | 1 | 8 | 2.44 | 0.36 | 1.42 | |
| Stratum summary | 0–14 | 8 | 1 | 9 | 1.84 (0.79–3.62) | 0.24 (0.01–1.34) | 1.06 (0.48–2.01) |
| 15–24 | 18 | 0 | 18 | 5.15 | 0.00 | 2.63 | |
| 25–34 | 23 | 2 | 25 | 7.10 | 0.62 | 3.88 | |
| 35–44 | 12 | 1 | 13 | 3.35 | 0.26 | 1.74 | |
| 45–54 | 8 | 4 | 12 | 2.19 | 1.02 | 1.59 | |
| 55–64 | 11 | 1 | 12 | 3.50 | 0.30 | 1.87 | |
| Stratum summary | 15–64 | 72 | 8 | 80 | 4.21 (3.29–5.30) | 0.45 (0.20–0.89) | 2.30 (1.83–2.87) |
| 65–74 | 5 | 2 | 7 | 2.30 | 0.79 | 1.49 | |
| 75–84 | 1 | 2 | 3 | 0.84 | 1.14 | 1.02 | |
| 85+ | 1 | 2 | 3 | 3.19 | 2.77 | 2.90 | |
| Stratum summary | 65–91 | 7 | 6 | 13 | 1.90 (0.76–3.92) | 1.20 (0.44–2.61) | 1.50 (0.80–2.56) |
| All age strata | 87 | 15 | 102 | 3.46 (2.77–4.27) | 0.56 (0.31–0.92) | 1.96 (1.60–2.38) | |
Final visual acuities
Final visual acuities (FVA) were based on visual acuities recorded 1 year after the ocular trauma. In six patients, the FVA was missing and could not be imputed with any certainty. These were excluded from analysis of FVA outcomes. Of the remaining 96 patients, 4 were excluded from this analysis because of no follow-up or follow-up of less than 12 months, and clinical indications that the last recorded visual acuity could well have changed materially by 1 year after the injury. This left 92 patients for analysis of FVA. Included in the 92 were 23 cases despite their follow-up being less than 12 months, because the recorded clinical data indicated that their last recorded visual acuity was highly unlikely to change materially, as a consequence of the injury, by 12 months of follow-up.
Thirty-six of the 92 (39.1%) patients had poor FVA (<6/12 including blindness). In 25 (27.2%) patients, the injured eye was blind (FVA <6/60), 24 being attributable to the eye injury. No perception of light in the injured eye was found in 17 (18.5%) patients, 16 being attributable to the eye injury. One patient was eligible for blind registration (not attributable to the eye injury), and three patients for partial sight registration (two being attributable to the eye injury). Only one patient had bilateral eye injuries (visual acuity not recorded).
Visual outcome attributable to the eye injury
Among the 92 valid cases, 4 patients who had poor or blinding visual outcome had a pre-existing condition that was recorded as the cause of the sight loss in the injured eye. These 4 patients were not counted as cases of blinding or poor visual outcome attributable to the eye injury. The number blind or visually impaired for this analysis is therefore slightly smaller to that used for the distribution of FVA.
Among cases of eye injury, the overall proportion of poor visual outcome due to the injury was 34.8% (95% CI: 25.15–45.42), and that of blinding outcome was 26.1% (95% CI: 17.48–36.29).
The observed proportion was lower in males compared with females (33% compared with 43%), the crude proportion ratio (M/F) being 0.78. With adjustment for age, the proportion ratio was closer to unity at 1.03 (95% CI: 0.48–2.20). Similar comparative results were found for proportion of blinding outcome due to the eye injury.
The 1-year cumulative incidence of blinding outcome (VA<6/60) attributable to the eye injury in ocular trauma was 0.46 (0.30–0.69, 95% CI) and for poor visual acuity outcome (VA<612) was 0.62 (0.42–0.87, 95% CI).
Overall, the incidence ratio (males/females) for blinding outcome was 5.32 (95% CI: 1.82–15.58) indicating about five times higher risk in males. Adjustment for age made no material difference, the age-adjusted incidence ratio being 5.56 (95% CI: 1.89–16.39). Two broad age strata could be defined (0–64 and ≥65) between which the incidence ratios seemed substantially different. The incidence of blinding outcome was about eight times higher in males within the 0–64 age stratum, but in those 65 and older, the higher risk in men was much less pronounced: the incidence ratio being 2.72, with a wide CI that included 1 (Table 3). Similar comparative results were found for poor visual outcome: 11 times higher risk in men within the 0–64 age stratum, and only a trivial difference within the older age group (Table 3).
Table 3. Incidence of blinding and poor visual outcomes attributable to the eye injury in males compared with that in females—Scotland 2009.
|
Incidence per 100 000 |
|||
|---|---|---|---|
| Males | Females | Incidence ratio: males/females (95% CI) | |
| Blinding outcome (<6/60) | |||
| Overall | 0.80 | 0.15 | 5.32 (1.82–15.58) |
| Age 0–64 years | 0.75 | 0.09 | 8.12 (1.87–35.31) |
| Age≥65 years | 1.09 | 0.40 | 2.72 (0.50–14.82) |
| Poor visual outcome (<6/12 including blindness) | |||
| Overall | 1.03 | 0.22 | 4.61 (1.90–11.21) |
| Age 0–64 years | 1.02 | 0.09 | 11.16 (2.62–47.47) |
| Age≥65 years | 1.09 | 0.80 | 1.36 (0.34–5.43) |
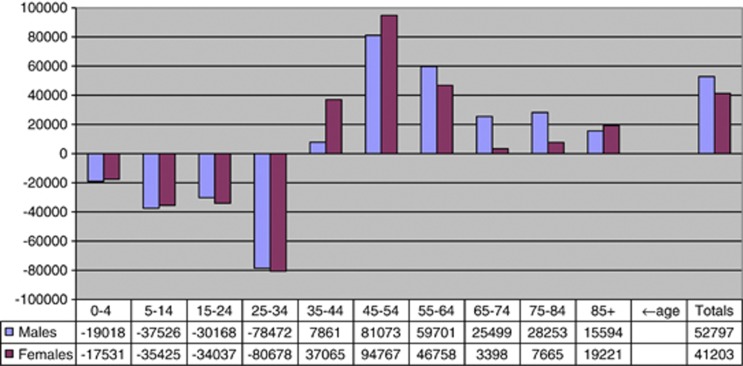
Demographic change relevant to incidence since 1992
The population of Scotland increased by 94 000 persons (52 797 males and 41 203 females) from mid-1991 to mid-2009. The changes in population numbers within age classes reflect the ‘aging trend' and are shown for males and for females in Figure 1. The proportion of females in the population showed a decline in 2009 in persons aged 75 years and older, with little or no change in the younger age groups.
Figure 1.
Changes in population numbers between 1992 and 2009 within age classes in Scotland, reflecting the ‘aging trend'.
Change in incidence of serious ocular trauma since 1992
The incidence of serious ocular trauma in Scotland was found to be around four times higher in 1992 compared with that in 2009. Only a small fraction of the reduction in risk could be attributed to demographic changes (changes in the population age and gender distribution), as indicated by the small differences between the crude and adjusted estimates of incidence ratios in Table 4a, that is, adjusting for the effects of age and gender resulted in only a small decrease in the incidence ratios.
Table 4a. Incidence of serious eye injuries in 2009 compared with that in 1992.
| 1-year cumulative incidence of ocular trauma per 100 000 | ||||
|---|---|---|---|---|
| |
1992 |
2009 |
Incidence ratio: 1992/2009 (95% CI) |
Homogeneity test P-value* |
| Males | ||||
| Crude estimates | 13.73 | 3.46 | 3.97 (3.13–5.02) | |
| Age-adjusted estimates | 3.77 (2.97–4.77) | 0.234 | ||
| Females | ||||
| Crude estimates | 2.54 | 0.56 | 4.54 (2.59–7.94) | |
| Age-adjusted estimates | 4.57 (2.55–8.17) | 0.295 | ||
| Males and females | ||||
| Crude estimates | 8.14 | 1.96 | 4.04 (3.25–5.02) | |
| Age- and sex-adjusted estimates | 3.88 (3.12–4.83) | 0.328 | ||
*Tests the hypothesis that there is homogeneity of incidence ratios across the strata of the adjustment variable(s).
Change in visual outcome due to the eye injury since 1992
As the 1992 published report did not include a breakdown of the number of patients with poor (or blinding) outcome by age or gender, it was not possible to compute incidence ratios (1992/2009) directly with adjustment for age or gender. However, the age- and gender-standardised morbidity ratios could be estimated. The observed number of patients with blinding outcome reported by the 1992 study was 21. The expected number (if the 2009 age- and gender-specific incidence figures applied) was 4.45. This gave a standardised morbidity ratio of 21/4.45=4.72 (95% CI: 3.08–7.24), indicating almost five times higher risk of blinding outcome in 1992 compared with 2009 (Table 4b).
Table 4b. Standardised morbidity ratios: comparing 1992 and 2009 in respect of the risk of blinding and poor visual outcome.
| Observed no. of cases in 1992 | Expecteda no. of cases in 1992 | SMR (95% CI) | |
|---|---|---|---|
| Blinding outcome (<6/60) | 21 | 4.55 | 4.72 (3.08–7.24) |
| Poor VA outcome (<6/12 including blindness) | 26 | 6.39 | 3.29 (2.14–5.04) |
Abbreviation: SMR, age- and sex-standardised morbidity ratio.
Expected number of cases if the 2009 age and gender specific incidence figures applied.
The observed number of patients with poor visual outcome reported by the 1992 study was 26. The expected number (if the 2009 age- and gender-specific incidence figures applied) was 6.39. This gave a standardised morbidity ratio of 26/6.39=3.29 (95% CI: 2.14–5.04), indicating about three times higher risk of poor visual outcome in 1992 compared with 2009 (Table 4b).
Discussion
The design of this study was deliberately similar to that of previous work done in Scotland2 so that the results could be directly comparable. The BOSU reporting card system also allowed access to every senior Scottish ophthalmologist to facilitate case ascertainment. The response rate of 77.1% that was achieved was similar to the Scottish response rate for other BOSU studies and better than that for most other regions in the United Kingdom.4
This national prospective study of ocular trauma requiring hospitalisation reports a 1-year cumulative incidence of 1.96 per 100 000 population in Scotland. The baseline 1992 study reported a higher incidence of 8.14 per 100 000 population2 and the worldwide incidence of ocular trauma requiring hospitalisation is estimated at 13 per 100 000 population.1
This study also reports a decrease in blinding outcome with a five times lower risk of blinding outcome compared with 1992, which may reflect a change in the type of injury observed or an improvement in the management of these patients.
Males remain at higher risk of ocular trauma than females, especially those under 65 years of age, with an age-adjusted incidence ratio of 9.08. A similar figure was found in 1992 when the risk ratio between males and females was 9.73 for the 15–64 age group (95% CI 6.49–14.14).2 There are few prospectively collected data in the literature but other contemporary prospective studies quote similar patterns in the incidence of ocular trauma, for example 4.9 per 100 000 in Southern Italy6 and 11.8 per 100 000 in Australia.7
Previously, the age distribution for the occurrence of serious ocular trauma was found to be bi-modal, with the maximum incidence in young adults and a second peak in the elderly.8, 9 However, this appears to be evolving with a single large peak observed for young adults, especially males. Both hospital- and population-based studies indicate a large preponderance of injuries affecting males10, 11, 12 and this study is no exception.
In developing countries, there is a trend towards increasing ocular trauma in childhood. Data are scarce but in India the Andhra Pradesh Eye Disease Study of 2522 people showed that the majority of blinding ocular trauma occurs in childhood. Prevention strategies have been aimed at mothers and children of lower socioeconomic status in urban India to address this problem.13
The findings reported here may reflect a true reduction of serious eye trauma in Scotland but there are other possible reasons for the substantial observed reduction compared with 1992 that need to be considered. Reporting of the incident cases might have been less complete compared with 1992 and criteria for admission, and therefore inclusion in this study, may have changed.
BOSU uses a systematic, prospective, case collection system, which has been shown to be a robust and pragmatic approach for identifying cases of interest in a routine clinical setting.4 Studies comparing passive and active surveillance systems consistently report that participants in an active scheme notify around twice as many cases per head of population.14, 15
However, under-reporting of cases is a methodological feature of routine surveillance that uses a single source to identify cases. Data verification through the SMR showed that 274 patients had been admitted in Scotland with various ocular and adnexal injuries, but some of these were not reported. The BOSU reporting scheme is dependent on voluntary reporting so a proportion of under-reporting will be due to random errors (eg, forgetting to report a case), which reduces the incidence estimate. Systematic under-reporting has been reported previously and will lead to bias and barriers to participation in the surveillance scheme.4 Furthermore, study-specific factors could be due to difficulties with the interpretation of the case definition,16 management of cases by doctors in specialties other than ophthalmology, or reluctance by participating ophthalmologists to report poor results.
Given the large discrepancy in admission figures found between the routine SMR01 data on admissions (274) and those identified through BOSU (102), it is likely that the study has underestimated the incidence of serious eye injury in 2009. It is, however, important to note that even if all of the 274 patients had been included in this study as valid cases, the study would still have found a considerable reduction in incidence of serious eye injury in 2009 compared with 1992. The degree of under-coverage, therefore, may explain some but not all of the reported reduction in incidence, and it may be reasonable to conclude that there has been a considerable reduction in incidence of serious eye injury in the population of Scotland since 1992.
The 2009 sample may have been biased towards more serious eye injuries, compared with the 1992 data, because of changes in the delivery of care. Among the eye injury cases, the study found higher proportion of patients with poor visual outcome in 2009 compared with 1992. This is consistent with the above-mentioned type of bias. Also consistent with the poorer coverage problem is the finding of a large reduction in population risk (incidence) of poor visual outcome in 2009 compared with 1992.
This study suggests that there is overall less ocular trauma being admitted to hospitals in Scotland and less risk of a poor visual outcome. These results could be used to plan future acute eye care services, potential centralisation of ocular trauma management and how to target campaigns to prevent trauma.
In summary, we report a reduction in the incidence of serious ocular trauma, and a reduction in vision loss from such injuries. But as with other serious trauma, young adult males continue to be at highest risk, posing a challenge for creating alternative approaches to prevention strategies.
Acknowledgments
We are very grateful to the WH Ross Foundation (Scotland) for funding the study and Tracy Sparey for administering the project. We also thank the Scottish Ophthalmological Club and the whole Scottish ophthalmic community for their hard work and enthusiasm especially A Agrawal, D Assheton, HR Atta, A Azura-Blanco, PS Baines, CW Barras, G Bedford, H Bennett, N Boyle, P Cauchi, C Cobb, G Cormack, A Cox, HC Devlin, J Ellis, L Esakowitz, A Ferguson, AI Fern, B Fleck, A Gaskell, ND George, J Gillen, D Grierson, M Gupta, H Hammer, IT Hanna, S Hewick, W Ho, F Imrie, P Kearns, J Kerr, L Kuffova, T Leslie, N Lois, CJ MacEwen, JA MacRae, S Madill, D Mansfield, DM Montgomery, J Murdoch, H Murgatroyd, RI Murray, SB Murray, A Pyott, A Reddy, C Scott, A Singh, JA Scott, J Singh, C Styles, S Sutherland, K Thompson, RP Savides, MG Stoddart, DRA Wardrop, C Weir, J Welch, K Wong, WW Wykes, D Yorston, YY Zhang.
The authors declare no conflict of interest.
Footnotes
This study was presented at the Royal College of Ophthalmologists Annual Congress in 2012 as a rapid fire presentation and at the Scottish Ophthalmological Club Centenary Meeting in 2011 as an invited lecture.
References
- Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5 (3:143–169. doi: 10.1076/opep.5.3.143.8364. [DOI] [PubMed] [Google Scholar]
- Desai P, MacEwen CJ, Baines P, Minassian DC. Incidence of cases of ocular trauma admitted to hospital and incidence of blinding outcome. Br J Ophthalmol. 1996;80 (7:585. doi: 10.1136/bjo.80.7.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGwin G, Hall TA, Xie A, Owsley C. Trends in eye injury in the United States, 1992–2001. Invest Ophth Vis Sci. 2006;47:521–527. doi: 10.1167/iovs.05-0909. [DOI] [PubMed] [Google Scholar]
- Foot B, Stanford M, Rahi J, Thompson J. The British Ophthalmological Surveillance Unit: an evaluation of the first 3 years. Eye. 2003;17:9–15. doi: 10.1038/sj.eye.6700233. [DOI] [PubMed] [Google Scholar]
- World Health Organisation . ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines. World Health Organisation: Geneva; 1992. [Google Scholar]
- Cillino S, Casuccio A, Di Pace F, Pillitteri F, Cillino G. A five-year retrospective study of the epidemiological characteristics and visual outcomes of patients hospitalized for ocular trauma in a Mediterranean area. BMC Ophthalmol. 2008;8:6. doi: 10.1186/1471-2415-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ARE, O'Hagan SB, Gole GA. Epidemiology of open- and closed-globe trauma presenting to Cairns Base Hospital, Queensland. Clin Exp Ophthalmol. 2006;34:252–259. doi: 10.1111/j.1442-9071.2006.01200.x. [DOI] [PubMed] [Google Scholar]
- Glynn RJ, Seddon JM, Berlin BM. The incidence of eye injuries in New England. Arch Ophthalmol. 1988;106 (6:785–789. doi: 10.1001/archopht.1988.01060130855039. [DOI] [PubMed] [Google Scholar]
- Desai P, MacEwen CJ, Baines P, Minaissian DC. Epidemiology and implications of ocular trauma admitted to hospital in Scotland. J Epidemiol Community Health. 1996;50 (4:436–441. doi: 10.1136/jech.50.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schein OD, Hibberd PL, Shingleton BJ, Kunzweiler T, Frambach DA, Seddon JM, et al. The spectrum and burden of ocular injury. Ophthalmology. 1988;95 (3:300–305. doi: 10.1016/s0161-6420(88)33183-0. [DOI] [PubMed] [Google Scholar]
- Katz J, Teilsch JM. Lifetime prevalence of ocular injuries from the Baltimore Eye Survey. Arch Ophthalmol. 1993;111 (11:1564–1568. doi: 10.1001/archopht.1993.01090110130038. [DOI] [PubMed] [Google Scholar]
- MacEwen CJ. Eye injuries: a prospective survey of 5671 cases. Br J Ophthalmol. 1989;73 (11:888–894. doi: 10.1136/bjo.73.11.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dandona L, Dandona R, Srinivas M, John RK, McCarty CA, Rao GN. Ocular trauma in an urban population in southern India: The Andhra Pradesh Eye Disease Study. Clin Exp Ophthalmol. 2000;28:350–356. doi: 10.1046/j.1442-9071.2000.00334.x. [DOI] [PubMed] [Google Scholar]
- Thacker SB, Redmond S, Berkelman RL. A controlled trial of disease surveillance strategies. Am J Prev Med. 1986;2:345–350. [PubMed] [Google Scholar]
- Vogt RL, LaRue D, Klaucke DN, Jillison DA. Comparison of an active and passive surveillance system of primary care providers for hepatitis, measles, rubella and salmonellosis in Vermont. Am J Public Health. 1983;73:795–797. doi: 10.2105/ajph.73.7.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foot BG, Stanford MR. Questioning questionnaires. Eye. 2001;15:693–694. doi: 10.1038/eye.2001.232. [DOI] [PubMed] [Google Scholar]