Significance
Media coverage of collective traumas may trigger psychological distress in individuals outside the directly affected community. We examined whether repeated media exposure to the Boston Marathon bombings was associated with acute stress and compared the impact of direct exposure (being at/near the bombings) vs. media exposure (bombing-related television, radio, print, online, and social media coverage) on acute stress. We conducted an Internet-based survey 2–4 wk postbombings with a nationally representative sample and representative subsamples from Boston and New York (4,675 adults). Repeated bombing-related media exposure was associated with higher acute stress than was direct exposure. Media coverage following collective traumas can diffuse acute stress widely. This unique study compares the impact of direct vs. indirect media-based community trauma exposure on acute stress responses.
Abstract
We compared the impact of media vs. direct exposure on acute stress response to collective trauma. We conducted an Internet-based survey following the Boston Marathon bombings between April 29 and May 13, 2013, with representative samples of residents from Boston (n = 846), New York City (n = 941), and the remainder of the United States (n = 2,888). Acute stress symptom scores were comparable in Boston and New York [regression coefficient (b) = 0.43; SE = 1.42; 95% confidence interval (CI), −2.36, 3.23], but lower nationwide when compared with Boston (b = −2.21; SE = 1.07; 95% CI, −4.31, −0.12). Adjusting for prebombing mental health (collected prospectively), demographics, and prior collective stress exposure, six or more daily hours of bombing-related media exposure in the week after the bombings was associated with higher acute stress than direct exposure to the bombings (continuous acute stress symptom total: media exposure b = 15.61 vs. direct exposure b = 5.69). Controlling for prospectively collected prebombing television-watching habits did not change the findings. In adjusted models, direct exposure to the 9/11 terrorist attacks and the Sandy Hook School shootings were both significantly associated with bombing-related acute stress; Superstorm Sandy exposure wasn't. Prior exposure to similar and/or violent events may render some individuals vulnerable to the negative effects of collective traumas. Repeatedly engaging with trauma-related media content for several hours daily shortly after collective trauma may prolong acute stress experiences and promote substantial stress-related symptomatology. Mass media may become a conduit that spreads negative consequences of community trauma beyond directly affected communities.
The bombings at the 2013 Boston Marathon were the first major terror attacks on US soil since September 11, 2001 (9/11). As reporters’ and spectators’ cameras filmed the mayhem over the subsequent week, graphic images were shown repeatedly in both traditional and social media worldwide. Like the 9/11 attacks, the US population was the terrorists’ intended psychological target.
Widespread media coverage extends the boundaries of local disasters, transmitting their impact far beyond the directly exposed population and turning them into collective traumas with potentially detrimental health effects (1, 2). For example, television exposure to the Oklahoma City bombing (3), the 1990 Gulf War (4), and 9/11 (5–8) have all been associated with widespread diffusion of trauma-related symptoms soon after collective trauma. Early post-9/11 media exposure has even been prospectively associated with increases in 9/11-related posttraumatic stress (PTS) symptoms over 3 y following the attacks (9).
Nonetheless, a prevailing assumption underlying professional response to collective trauma is that directly exposed individuals are, by definition, at greatest risk for stress-related disorders. This belief persists despite mounting evidence that both live and video observation of threatening content can lead to fear conditioning (10), a central component of traumatic stress responses. More recent work further challenges this key assumption by demonstrating that experimental exposure to a traumatic film can activate fear circuitry in the brain and produce flashbacks—two key processes associated with the development of posttraumatic stress disorder (PTSD) (11). In light of these findings, we suggest that repeatedly engaging with trauma-related stories via the media may prolong the acute experience by constantly reminding people of trauma-related information and encouraging ruminative thinking. Repeatedly watching disturbing images may also affect threat appraisals and may contribute to stress-related symptoms (12). Because rumination keeps the mind focused on a past negative event (13), media exposure may perpetuate activation of fear circuitry in the brain, especially in the early aftermath of the event when memory consolidation is most pronounced; this could contribute to the abnormal consolidation of fear conditioning that is associated with development of acute and PTS responses (14). Unlike direct exposure to a collective trauma, which can end when the acute phase of the event is over, media exposure keeps the acute stressor active and alive in one’s mind. In so doing, repeated media exposure may contribute to the development of trauma-related disorders by prolonging or exacerbating acute trauma-related symptoms.
We compared the impact of direct and media exposure to the Boston Marathon bombings (BMB) in a large representative national sample of US residents, including an oversample from the Boston metropolitan area. We were particularly concerned with acute stress responses, which appear within weeks of a disaster and have potential longer-term health consequences (15). Because cumulative exposure to adverse events appears to systematically increase risk for 12-mo incidence and lifetime psychiatric disorder (16, 17), we also sought to investigate the role of direct and indirect exposure to several recent collective traumas in the United States that triggered widespread media attention: the 9/11 attacks, Superstorm Sandy, and the Sandy Hook Elementary School shootings. Prior research suggests both the type and frequency of prior traumas must be assessed to understand the impact of direct and indirect exposure to collective events on acute stress (18). To ensure a sample of individuals who were likely to have been directly exposed to these three recent collective events, we included an oversample from the New York City area.
Between April 29 and May 13, 2013 (2–4 wk after the Boston Marathon), we conducted an Internet-based survey with representative samples of residents from metropolitan Boston (n = 846), New York City (n = 941), and the rest of the United States (n = 2,888). Respondents were drawn from the GfK KnowledgePanel, a probability-based Web-enabled panel recruited via traditional survey methods to complete Web-based surveys in exchange for compensation or free Internet (as an incentive for participation). We assessed BMB-related acute stress; direct exposure to the BMB; hours of BMB-related media exposure (via traditional and social media); and prior exposure to the 9/11 attacks, Superstorm Sandy, and Sandy Hook Elementary School shootings. Pre-BMB media use and physician-diagnosed mental health had previously been collected on the majority of the panel before the bombings.
Results
Exposure to the Boston Marathon Bombings and Aftermath.
A total of 9.6% of respondents (weighted n = 449) reported being directly exposed to the BMB themselves or through a close relationship: 1.15% (weighted n = 53) were at or near the site, 8.74% (weighted n = 407) reported someone close to them was at the site, 0.48% (weighted n = 23) knew someone who was injured, and 0.35% (weighted n = 16) knew someone who died. A total of 8.98% (weighted n = 420) reported being directly exposed (themselves or through a close relationship) to the Boston-area lockdown that occurred shortly after the bombings: 2.52% (weighted n = 118) were in the area of the lockdown and 7.55% (weighted n = 351) reported someone close to them was in the area.
Exposure to Prior Collective Trauma.
Direct exposure (self or close other) to at least one prior collective trauma was reported by 26.27% (weighted n = 1,228): 17.92% (weighted n = 838) for 9/11; 18.67% (weighted n = 873) for Superstorm Sandy; and 2.66% (weighted n = 124) for Sandy Hook. Indirect exposure (e.g., live media) was reported by 74.53% (weighted n = 3,484) for 9/11; 60.73% (weighted n = 2,839) for Superstorm Sandy; and 50.77% (weighted n = 2,373) for Sandy Hook.
Prevalence of Acute Stress Symptoms.
When coded “high” vs. “low” by Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition (DSM-IV) criteria, 4.46% (weighted n = 209) of the sample met criteria for high acute stress (19). High acute stress was equally likely in New York [odds ratio (OR) = 1.50; 95% confidence interval (CI), 0.77, 2.94] and the national sample (OR = 0.99; 95% CI, 0.56, 1.77) as it was in Boston. The mean total Stanford Acute Stress Reaction Questionnaire (SASRQ) score was 43.41 (SE = 0.40; 95% CI, 42.62, 44.21). Continuous acute stress symptom scores were also comparable in Boston and New York [regression coefficient (b) = 0.43; SE = 1.42; 95% CI, −2.36, 3.23], but lower in the national sample compared with Boston (b = −2.21; SE = 1.07; 95% CI, −4.31, −0.12).
Correlates of BMB-Related Acute Stress.
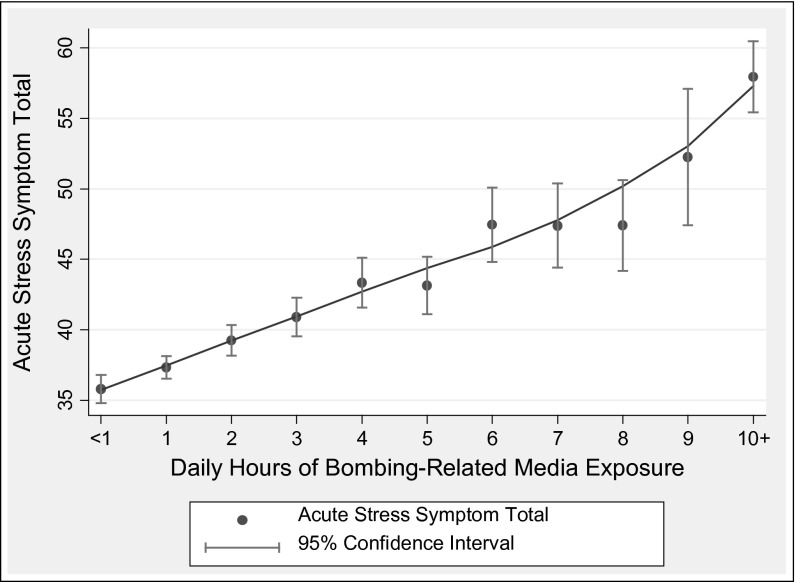
Table 1 presents analyses examining correlates of continuous acute stress symptom scores. Prior mental health problems and high media exposure were associated with acute stress (model 1), even after controlling for direct exposure to the BMB (model 2), prior collective trauma exposure (model 3), and demographic covariates (model 4). Prior direct exposure to the 9/11 attacks and the Sandy Hook School shootings were significantly associated with BMB-related acute stress; neither Superstorm Sandy nor lockdown exposure were associated with acute stress scores. Fig. 1 presents acute stress symptom totals by hours of daily BMB-related media exposure, demonstrating that acute stress steadily increases with additional hours of BMB-related media exposure.
Table 1.
Predictors of continuous acute stress symptom scores (n = 4,652)
| Variables | Model 1 b (95% CI) | Model 2 b (95% CI) | Model 3 b (95% CI) | Model 4 b (95% CI) |
| Prior mental health | 4.25(2.61, 5.89)*** | 4.29(2.64, 5.92)*** | 4.21(2.58, 5.85)*** | 3.52 (1.88, 5.16)*** |
| Media exposure (hours per day)† | ||||
| 1.5–2.9 | 2.20(0.52, 3.89)* | 1.97(0.30, 6.64)* | 1.57(−0.14, 3.28) | 2.61 (0.99, 4.23)** |
| 3–5.9 | 6.26(4.50, 8.02)*** | 6.10(4.36, 7.85)*** | 5.56(3.80, 7.32)*** | 6.38 (4.64, 8.13)*** |
| 6 or more | 17.50(15.03, 19.97)*** | 16.84(14.31, 19.35)*** | 15.73(13.22, 18.24)*** | 15.85 (13.42, 18.28)*** |
| Boston Marathon bombing exposure | ||||
| Direct exposure | 4.54(1.43, 7.65)** | 3.86(0.72, 7.01)* | 6.17 (3.09, 9.25)*** | |
| Prior collective stress exposures | ||||
| Direct exposure to 9/11 | 3.94(1.53, 6.35)** | 4.89 (2.45, 7.33)*** | ||
| Direct exposure to Sandy Hook | 10.02(2.13, 17.90)* | 8.36 (0.76, 15.96)* | ||
| Indirect exposure to Sandy Hook | 0.72(−0.80, 2.24) | 0.35 (−1.12, 1.83) | ||
| Demographics | ||||
| Geographic comparison | ||||
| National sample‡ | 1.29 (−0.51, 3.08) | |||
| Female sex | 2.16 (0.68, 3.65)** | |||
| Education§ | ||||
| High school | −5.33 (−9.35, −1.30)** | |||
| Some college | −5.06 (−11.05, −3.06)*** | |||
| Bachelor’s degree or higher | −6.98 (−11.04, −2.91)** | |||
| Ethnicity¶ | ||||
| Mixed race, non-Hispanic | 9.31 (5.06, 13.56)*** | |||
| Hispanic | 1.47 (−0.76, 3.71) | |||
| Income | −1.13 (−1.52, −0.74)*** | |||
| Model statistics | F(4, 4,647) = 59.37*** | F(4, 4,646) = 50.00*** | F(8, 4,652) = 35.04*** | F(16, 4635) = 24.67*** |
| R2 = 0.12 | R2 = 0.12 | R2 = 0.14 | R2 = 0.18 |
P < 0.05; **P < 0.01; ***P < 0.001.
From 0 to 1.49 h of media exposure comprise the reference group.
Boston and New York subsamples were not significantly different and comprise the reference group.
Less than a high school education comprises the reference group.
Caucasians and African Americans were not significantly different and comprise the reference group.
Fig. 1.
Acute stress symptom total by the number of hours per day of Boston Marathon bombing media exposure in the week following the Boston Marathon bombings.
Table 2 presents analyses examining correlates of high vs. low acute stress. Prior mental health ailments and six or more hours of daily BMB media exposure were significantly associated with high acute stress (model 1), even when controlling for direct BMB exposure (model 2). Direct exposures to 9/11 and to the Sandy Hook shootings were also associated with high acute stress (model 3), and these findings remained significant after controlling for demographic covariates (model 4). High acute stress was not associated with Superstorm Sandy exposure or exposure to the lockdown. In both sets of analyses, six or more hours of daily media exposure was associated with higher acute stress symptomatology than was direct BMB exposure.
Table 2.
Predictors of DSM-IV criteria B, C, and D high acute stress (n = 4,652)
| Variable | Model 1, OR (95% CI) | Model 2, OR (95% CI) | Model 3, OR (95% CI) | Model 4, OR (95% CI) |
| Prior mental health | 1.91(1.43, 2.54)*** | 1.91(1.43, 2.5)*** | 1.93(1.45, 2.57)*** | 1.77(1.29, 2.43)*** |
| Media exposure (hours per day)† | ||||
| 1.5–2.9 | 1.0(0.33, 3.01) | 0.99(0.33, 2.99) | 0.93(0.30, 2.84) | 1.18(0.41, 3.40) |
| 3–5.9 | 2.69(0.98, 7.35) | 2.67(0.98, 7.30) | 2.49(0.89, 6.97) | 2.86(1.07, 7.66)* |
| 6 or more | 11.02(4.23, 28.70)*** | 10.75(4.08, 28.37)*** | 9.45(3.54, 25.25)*** | 9.56(3.74, 24.43)*** |
| Boston Marathon bombing exposure | ||||
| Direct exposure | 1.17(0.66, 2.08) | 1.04(0.58, 1.88) | 1.47(0.80, 2.70) | |
| Prior collective stress exposures | ||||
| Direct exposure to 9/11 | 1.97(1.19, 3.25)** | 2.38(1.39, 4.09)** | ||
| Direct exposure to Sandy Hook | 2.47(1.19, 5.15)* | 2.11(0.95, 4.72) | ||
| Demographics | ||||
| Female sex | 1.36(0.86, 2.14) | |||
| Education‡ | ||||
| High school | 0.45(0.23, 0.87)* | |||
| Some college | 0.23(0.11, 0.48)*** | |||
| Bachelor’s degree or higher | 0.15(0.07, 0.33)*** | |||
| Ethnicity§ | ||||
| Mixed race, non-Hispanic | 2.80(1.29, 6.08)** | |||
| Model statistics | χ2(4) = 104.31*** | χ2(5) = 108.32*** | χ2(7) = 133.49*** | χ2(12) = 204.56*** |
| pseudo R2 = 0.13 | pseudo R2 = 0.13 | pseudo R2 = 0.15 | pseudo R2 = 0.19 |
P < 0.05; **P < 0.01;***P < 0.001.
0–1.49 h of media exposure comprises the reference group.
Less than high school education comprises the reference group.
White, Hispanic, and black respondents were not significantly different and comprise the reference group.
Because participants directly exposed to the BMB reported more subsequent BMB-related media exposure (b = 7.05; 95% CI, 6.24, 7.87; P < 0.001), we examined whether our findings were driven by directly exposed individuals who were also exposed to a great deal of BMB-related media content. The interaction between direct BMB exposure and BMB-related media exposure was not associated with continuous BMB-related acute stress symptoms (b = −0.01; 95% CI, −0.70, 0.68; P = 0.98)—that is, acute stress symptoms increased incrementally as BMB media exposure increased both for respondents who were directly (b = 1.50; 95% CI, 0.89, 2.11; P < 0.001) and not directly (b = 1.38; 95% CI, 1.14, 1.61; P < 0.001) exposed to the bombings. Although pre-BMB mental health was not associated with exposure to BMB media coverage (r = 0.03; P = 0.08), we tested whether the interaction between BMB media exposure and pre-BMB mental health was associated with acute stress—it was not significant (b = −0.51; 95% CI, −2.42, 1.40; P = 0.60).
We also had data on pre-BMB daily television-watching habits that were assessed prior to the bombings on the vast majority of respondents (n = 4,383). Pre-BMB daily television watching was moderately associated with post-BMB media exposure (r = 0.20; P < 0.001) and modestly associated with pre-BMB mental health (r = 0.04; P < 0.01) and acute stress (r = 0.08; P < 0.001). When pre-BMB television watching was included as a covariate in the analyses reported above, post-BMB media exposure findings remained robust with nearly identical effects to those reported in the tables. Thus, the association between post-BMB media exposure and acute stress cannot be explained through respondents’ television-watching habits alone. We also tested whether the interactions between pre-BMB television-watching habits and pre-BMB mental health or direct BMB exposure were associated with continuous BMB-related acute stress scores. The interactions were not significant (pre-BMB mental health b = −0.11; 95% CI, −2.63, 2.41; P = 0.93; direct exposure b = 3.10; 95% CI, −0.73, 6.94; P = 0.11).
Finally, analyses were conducted using a continuous count (0–3) of cumulative direct exposure to 9/11, Sandy Hook, and Superstorm Sandy rather than three dichotomous direct exposure variables. Cumulative exposure was significantly associated with continuous acute stress (b = 3.25; 95% CI, 1.97, 4.54; P < 0.001) and high acute stress (OR = 1.70; 95% CI, 1.36, 2.15; P < 0.001). Media exposure variables remained significantly associated with acute stress, with results comparable to those presented in the tables.
Discussion
Community-based traumas (e.g., mass shootings, natural disasters) receive extensive media coverage that spreads rapidly across the multiple media outlets woven into our daily lives. Understanding how widespread media coverage of these events may play a role in our well-being is an important public health issue. This study compares the mental health correlates of direct personal exposure vs. widespread media exposure to a community-based trauma—the Boston Marathon bombings. We demonstrate that trauma-related media exposure is associated with acute psychological response in the aftermath of the bombings. The fact that a group of respondents from our national sample reported high acute stress raises the concern that prolonged media exposure could have far-reaching implications for population well-being. Indeed, respondents who engaged with media coverage for six or more hours daily in the week following the BMB were nine times more likely to report high acute stress than respondents reporting minimal media exposure. Moreover, pre-BMB mental health and habitual pre-BMB television watching did not explain these findings, further supporting our view that media exposure following highly stressful events may contribute to significant trauma-related distress. Given that acute stress reactions may precede long-term mental (e.g., posttraumatic stress symptoms) (20) and physical (e.g., cardiac) (9, 15) health ailments, our findings have significant implications. These potential health risks may be further intensified by the nature of some collective events that continue beyond an initial trauma (e.g., the lockdown after the BMB bombings, the Washington, DC, sniper shootings), because individuals remain vigilant and may regularly scan media sources for information about ongoing threats. Though it is important to stay informed, watching coverage of a traumatic event repeatedly may exacerbate psychological distress and impede the normal recovery process, leading to increased health problems that can extend to people living well beyond the borders of communities directly affected by the trauma.
Nonetheless, we note that the response captured in this study reflects tremendous population resilience; levels of acute stress reported in our sample were generally quite low, probably due to the rapid and effective response mounted by law enforcement and emergency response teams, health professionals, and the public (21). In fact, surprisingly, although direct BMB exposure was associated with continuous acute stress symptom scores (as expected), it was not associated with high acute stress (using DSM-IV criteria B-E), whereas six or more hours of daily media exposure in the week following the BMB was associated with a ninefold increased likelihood of reporting high acute stress (Table 2). We suspect these findings may be due to both environmental and personal factors. Perhaps the well-prepared emergency response teams at the site of the BMB were able to provide sufficient support for directly exposed individuals that their acute stress symptoms were kept at a minimum. An American Red Cross public campaign encouraging Bostonians to limit their exposure to media may also have helped to limit the spread of acute stress. At the same time, given the robust nature of our findings, there are likely to be unique characteristics (other than mental health and habitual television watching) that led individuals to expose themselves to extensive BMB-related media. Understanding how personal characteristics (e.g., risk-taking, world views) might affect the choices people make regarding media exposure could help identify those most vulnerable to its negative impact and guide targeted public health interventions seeking to prevent trauma-related disorders.
Acute stress responses were also associated with prior direct exposure to two of the three recent community traumas (9/11 and Sandy Hook School shootings)—both of which involved deliberately perpetrated violence against the community. Although Superstorm Sandy caused substantial death and destruction, direct exposure to it did not appear to arouse the same sensitivity to BMB-related media exposure as did exposure to prior violent events. These findings are consistent with previous evidence that exposure to similar and/or violent events may render some individuals more vulnerable to the negative effects of subsequent collective trauma (17).
Given the potential health implications of our findings, it is also important to explore how ongoing media exposure to collective stress may affect stress responses over time. Repeated exposure to trauma-related content is likely to reinforce rumination and intrusive thoughts, activate fear circuitry, and perhaps contribute to development of flashbacks (11). Persistent cognitive processing of fear and worry may also enhance autonomic activation, significantly impacting several physiologic systems (e.g., cardiovascular, endocrine, immune), which could foster the development of stress-related disease (22–24). Both laboratory and population-based studies suggest negative health impacts of stress-related cognitive processing. For example, rumination about a stressful laboratory experience was associated with greater increases in heart rate and blood pressure that persisted over a 24-h period—long after the experiment was over—suggesting that cognitive processing of stress may prolong the physiologic stress response (25). Fears of future terrorism intensified the link between 9/11-related acute stress response and increased reports of cardiovascular ailments 3 y later (15). Ruminative thought has also been prospectively associated with greater risk for heart disease (26), impaired immune function, and poor daily functioning (24). In essence, extended, repetitive media exposure may turn what was an acute stress into a chronic stressor, with physiologic consequences associated with stress-related health problems (27).
Our findings are consistent with research that documented high levels of 9/11-related acute stress (9) and probable PTSD (5) in people who watched more 9/11-related television coverage in the week after the attacks, and research that demonstrated an association between social media exposure and posttraumatic stress symptoms following Superstorm Sandy (28). Indeed, earlier work following the 9/11 attacks suggests that some images (e.g., people jumping from the buildings) are more detrimental for mental health than others (5, 6). If widespread media coverage of events displays these images repeatedly, they may introduce “emotional contagion” that unintentionally spreads negative impacts beyond the directly exposed area (10, 28). Given the significance of media in our daily lives, its impact on our health is likely to grow as reality television blurs the line between fiction and reality and promotes social media use (29). When combined with research demonstrating the impact of media on health-related risk perception (30) and of television coverage of a national health scare on symptom reporting (31), our findings add to growing concerns about the potential for broader public health implications of mass media coverage of disasters (32).
We recognize that our correlational study cannot establish a definitive causal relationship between media exposure and mental or physical health impacts. However, prospective longitudinal data we collected after the 9/11 attacks suggested that 9/11-related television exposure in the week following the attacks was prospectively associated with increases in posttraumatic stress symptoms over 3 y, controlling for acute stress (9). However, it is impossible to know if BMB-related media exposure led to acute stress in the current, cross-sectional study. Indeed, the most plausible interpretation of the present findings would be that the relationship between media exposure and acute stress is recursive—people who are most distressed in the aftermath of such an event are probably more likely to engage media coverage as a way of coping with the experience. Although this may be beneficial initially, over time the repeated media-based reexposures may contribute to a self-perpetuating cycle of distress.
Nonetheless, by using a preexisting panel of respondents, we had the unique ability to demonstrate that our findings remained robust after controlling for pre-BMB television-watching behavior and mental health history (both collected before the bombings); this helps rule out the alternative position that only individuals with preexisting mental health difficulties or individuals who watched a great deal of television in general were at risk for the negative effects of media exposure. However, even though our mental health history measure had been benchmarked against the National Health Interview Survey, which itself has been validated against medical records (33), it was limited to self-reported physician-diagnosed anxiety and depression. However, the exact timing of these pre-BMB diagnoses remains unknown. Without prior assessments of lifetime or ongoing trauma history or PTSD, our pre- and postevent mental health measures are assessing different, but related, constructs (anxiety/depression and acute stress). Finally, because a large minority of the sample (28%) did not have pre-BMB mental health data available, their data were imputed (see below) to retain sample representativeness. Given these limitations, it is possible that our measure of mental health history reflected vulnerability to distress rather than actual preevent distress. That said, though our measure is imperfect, it provides a proxy control for preevent mental health—something that is both rare and essential for understanding the psychological impact of collective stressors.
Other limitations include not having direct assessments of mechanisms by which media may influence acute stress (e.g., perseverative cognition) (22) and not having parallel measures of exposure across all events (live media and subsequent media coverage for BMB, 9/11, Superstorm Sandy, and Sandy Hook shootings); future research should examine these factors. Finally, although data were collected very quickly after the bombings, respondents reconstructed their reports of media exposure 2–4 wk post-BMB; ongoing diary-based collection of media use or experience-sampling methods would provide more accurate assessments.
Our results should not be construed to imply that media serves no positive purpose when disaster strikes. Media outlets can disseminate information and promote messages of community solidarity and resilience—indeed, mass media can and should serve the affected communities by delivering these messages. Similarly, our findings should not be construed to suggest that repeated exposure is always detrimental. Prolonged exposure therapy (PET) using “repeated, prolonged imaginal exposure to the trauma memories (i.e., revising and recounting the trauma memory in imagery)” is considered first-line treatment after the development of PTSD (34). An important distinction is that PET is used after PTSD develops and in the context of a professional therapeutic relationship. We address the impact of early media exposure on acute stress reactions that occur before respondents develop PTSD and outside the context of a therapeutic relationship. Clearly, the timing and context of exposures are critical to understanding the association between repeated prolonged exposure and mental or physical health.
Media exposure to collective stress may have measurable negative psychological effects, and extensive, repeated exposure to event-related media coverage may be an important mechanism through which these negative impacts are spread beyond the directly affected population. Our results suggest that health care providers should advise people presenting with stress-related problems to limit time spent watching news coverage of events in the immediate aftermath of a highly publicized local or national trauma. Professionals who design public service announcements or other postdisaster services may also want to consider such recommendations. Most importantly, media outlets should recognize that repeatedly showing gruesome, distressing images is not in the public interest. The repetitive display of such images serves to keep the potentially traumatic experience and event-related distress alive. To limit the potential for harm, viewers should be warned when these images are about to be shown. Although we are not the first to suggest that media sources use cautionary statements about graphic coverage (35), we provide evidence that media exposure can be more strongly associated with acute stress than direct exposure to a collective event, thereby demonstrating the importance of this recommendation. As access to multiple media sources becomes easier and faster than ever, health professionals, policymakers, and media sources themselves should be sensitive to the possibility that extensive, repetitive exposure to threatening or upsetting content may have far-reaching consequences following collective stress.
Materials and Methods
Design, Sample, and Data Collection.
Between April 29 and May 13, 2013 (2–4 wk after the Boston Marathon bombings), we conducted an Internet-based survey with representative samples of residents from metropolitan Boston (n = 846), New York City (n = 941), and the remainder of the United States (n = 2,888), all drawn from the GfK KnowledgePanel. GfK uses address-based sampling methods to randomly sample and recruit people within households. To ensure panel representativeness, households without a computer or Internet connection are given a laptop with Internet service. KnowledgePanelists complete Web-based surveys in exchange for compensation or free Internet (an incentive for participation). The survey was fielded to 6,098 KnowledgePanelists; e-mail and telephone reminders were used to encourage response. A total of 4,822 responded, resulting in a 79.08% study completion rate; 147 respondents were dropped due to excessive missing outcome data or unreliably short survey completion times (<3 min), yielding 4,675 usable complete cases (76.66%). All procedures for this study were approved by the Institutional Review Board of the University of California, Irvine.
The panel sample selection methodology provides statistical control on the representativeness of GfK panel survey samples as measured by their proximity to population benchmarks. Poststratification weights were applied so that the final composition of our weighted sample closely matches US Census benchmarks (Table S1). The weighting process involved two major steps. Design weights that reflect unequal selection probabilities for different respondents were obtained from the KnowledgePanel, because each active panel member carries a measure of size used for sample selection. These measures reflect how many adults each panel member represents. Then, study design weights were adjusted to reported demographic distributions of the adult US population along several dimensions: age (18–29; 30–44; 45–59; 60+), sex, race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, non-Hispanic other, non-Hispanic multirace), education (less than high school, some college, BA/BS or higher), income ($0–$24,999, $25,000–$49,999, $50,000–$74,999, $75,000+), region (Northeast, Midwest, South, West), Internet access, and metro status (metro, nonmetro). The needed population distributions for these categories were obtained from the American Community Survey (36) separately by geographic location: Boston, New York, and the rest of the United States. When sample sizes permitted, variables were crossed (e.g., age and sex), so that joint distributions could be used to adjust weights. If needed, categories of weighting variables were collapsed to increase samples of available respondents and avoid creating extreme weights.
Measures.
The SASRQ (37) assessed acute stress responses to the BMB and their aftermath. Respondents used a six-point scale from 0 (not experienced) to 5 (very often experienced) to describe how often they had experienced 30 items “since the Boston Marathon bombings and their aftermath” (e.g., “I try to avoid thoughts about the Boston Marathon bombings and their aftermath,” and “I feel hypervigilant or ‘on edge’”). Two scores were created: a summed acute stress symptom score (30–180; alpha = .96) to allow fine-grained examination of the media-acute stress symptom association; and high vs. low acute stress using DSM-IV criteria B, C, D, and E to examine the potential clinical relevance of media exposure (3+ dissociative, 1+ avoidance, 1+ reexperiencing/intrusive, and 1+ arousal/anxiety symptoms; meeting all four criteria was considered high acute stress). Symptoms experienced at least “sometimes” were coded as present. Respondents were not assumed to have Acute Stress Disorder because most did not meet DSM-IV criterion A (direct exposure; for diagnostic criteria, see www.ptsd.va.gov/professional/pages/acute-stress-disorder.asp).
Exposure to the BMB was assessed by asking respondents whether they or someone close to them was at, injured in, or near the site of the Boston Marathon on Monday April 15; whether they knew someone who died in the BMB; whether they or someone close to them was in the locked down area during the search for suspects on Friday, April 19; and how many hours per day (0–11+) they spent engaged with BMB-related content from each of several media sources (i.e., television, radio, print, online, and social media) during the subsequent week. Total media exposure was computed in two ways: the continuous number of hours of daily use summed across types of media and categorical quartiles (0–1.49, 1.5–2.9, 3–5.9, 6+) to allow comparison across equivalently sized groups with different levels of media exposure.
Respondents were also asked about prior exposure to 9/11, Superstorm Sandy, and the Sandy Hook School shootings. Respondents were coded as either directly (e.g., “I was directly exposed at the time of the event”) or indirectly (e.g., “I watched this event as it occurred on live TV”) exposed to each event. Prior direct exposure was coded categorically for each event and as a cumulative stress score (0–3) to allow comparison of the impact of the type of event (e.g., violence, natural disaster) vs. cumulative prior stress. Prior indirect exposure was coded categorically for each event as “yes” or “no” live media exposure.
Preevent mental health was assessed using items modified from the Centers for Disease Control’s National Center for Health Statistics annual National Health Interview Survey (NHIS) (33). Respondents were asked “Has a medical doctor ever diagnosed you as suffering from any of the following ailments?” with prompts for depression and anxiety disorders (not including PTSD). Comparisons between NHIS and KnowledgePanel estimates indicated an average difference of less than 1.5% for several health outcomes, supporting the validity of these data (38). Over two-thirds of the sample had provided this information before the BMB (n = 3,351, 71.7%). To retain sample representativeness, missing values for anxiety and depression were imputed using Sequential Hot Deck Imputation (39, 40). This method identifies the best predictors of the disorders and appropriate donors using respondent survey data. Missing data are then replaced with values from donors. We then conducted analyses three ways: with and without imputed data and with 475 more respondents whose lifetime mental health data were collected post-BMB. The findings were substantively unchanged across all analyses. After carefully weighing the potential for having introduced bias with the imputed scores vs. the tradeoff of losing sample representativeness, final analyses were conducted with all respondents (n = 4,675). Prior mental health was coded 0, 1, 2 (none, one mental health ailment, both depression and anxiety) for the analyses. The pre-BMB television-watching habits of the vast majority of the sample (n = 4,383) were also measured before the bombings with 117 items assessing the frequency with which respondents watched broadcast and cable television networks using a five-point frequency scale. A pre-BMB television watching index was created as the mean frequency across all channels a respondent reported ever watching in the 6 mo prior to the assessment.
Analytic Strategy.
Statistical analyses were conducted using Stata, version 11.1 (Stata Corp.). Data were weighted to adjust for probability of selection in the GfK panel and for survey-specific participation. Poststratification weights were iteratively constructed from respondents’ design weights using probability estimates based on multiple demographic characteristics, region of residence, and Internet access. The weighted sample closely matches the December 2012 US census data (Table S1).
Acute stress symptoms were scored two ways. Logistic and ordinary least-squares regression analyses examined correlates of “high” acute stress and the total acute stress symptom score, respectively. Variables were screened in bivariate analyses (correlations, χ2); variables that reached P < 0.10 were tested for relative contribution in theoretically meaningful blocks: (i) demographic indicators (age, sex, ethnicity, education, income, marital status; substituting employment status for income produced similar results), (ii) prior mental health, (iii) exposure to the BMB and subsequent lockdown, (iv) daily hours of BMB-related media exposure coded in quartiles (conducting analyses with categorical tertiles and quintiles produced similar results), and (v) direct and indirect exposure to past collective traumas (9/11, Superstorm Sandy, and Sandy Hook). Trimmed blocks of variables were then entered hierarchically into multivariate analyses: (i) prior mental health and BMB-related media exposure, (ii) direct BMB exposure, (iii) exposure to previous collective traumas, and (iv) demographics. Although our measure of acute stress was designed for the DSM-IV, we also created a proxy for high acute stress using the DSM-5 count of nine or more positive symptoms. Because acute stress results were comparable when high acute stress was computed using both DSM-IV and DSM-5 criteria, and the SASRQ was created specifically for the DSM-IV diagnosis, only DSM-IV results are reported.
Supplementary Material
Acknowledgments
The authors thank the GfK Government and Academic Research team of J. Michael Dennis, Debra Vanni, Sergei Rodkin, Stefan Subias, Kathleen Connolley, Mansour Fahimi, Randall Thomas, Wendy Mansfield, and Curtiss Cobb for providing access to data collected on GfK KnowledgePanelists, preparing the Web-based version of our survey, creating the data file, general guidance on GfK KnowledgePanel methodology, and for survey research and sampling expertise. Project funding was provided by US National Science Foundation Grant BCS-1342637 (to R.C.S. and E.A.H.).
Footnotes
The authors declare no conflict of interest.
*This Direct Submission article had a prearranged editor.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1316265110/-/DCSupplemental.
References
- 1.Vasterman P, Yzermans CJ, Dirkzwager AJE. The role of the media and media hypes in the aftermath of disasters. Epidemiol Rev. 2005;27:107–114. doi: 10.1093/epirev/mxi002. [DOI] [PubMed] [Google Scholar]
- 2.Wright KM, Ursano RJ, Bartone PT, Ingraham LH. The shared experience of catastrophe: An expanded classification of the disaster community. Am J Orthopsychiatry. 1990;60(1):35–42. doi: 10.1037/h0079199. [DOI] [PubMed] [Google Scholar]
- 3.Pfefferbaum B, et al. Television exposure in children after a terrorist incident. Psychiatry. 2001;64(3):202–211. doi: 10.1521/psyc.64.3.202.18462. [DOI] [PubMed] [Google Scholar]
- 4.Cantor J, Mares ML, Oliver MB. In: Desert Storm and the Mass Media. Greenberg B, Gantz W, editors. Cresskill, NJ: Hampton; 1993. pp. 325–340. [Google Scholar]
- 5.Ahern J, et al. Television images and psychological symptoms after the September 11 terrorist attacks. Psychiatry. 2002;65(4):289–300. doi: 10.1521/psyc.65.4.289.20240. [DOI] [PubMed] [Google Scholar]
- 6.Schlenger WE, et al. Psychological reactions to terrorist attacks: Findings from the National Study of Americans’ Reactions to September 11. JAMA. 2002;288(5):581–588. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- 7.Schuster MA, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med. 2001;345(20):1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- 8.Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA. 2002;288(10):1235–1244. doi: 10.1001/jama.288.10.1235. [DOI] [PubMed] [Google Scholar]
- 9.Silver RC, et al. Mental- and physical-health effects of acute exposure to media images of the September 11, 2001, attacks and the Iraq War. Psychol Sci. 2013;24(9):1623–1634. doi: 10.1177/0956797612460406. [DOI] [PubMed] [Google Scholar]
- 10.Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: It’s not what you thought it was. Am Psychol. 2006;61(1):10–26. doi: 10.1037/0003-066X.61.1.10. [DOI] [PubMed] [Google Scholar]
- 11.Bourne C, Mackay CE, Holmes EA. The neural basis of flashback formation: The impact of viewing trauma. Psychol Med. 2013;43(7):1521–1532. doi: 10.1017/S0033291712002358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marshall RD, et al. The psychology of ongoing threat: Relative risk appraisal, the September 11 attacks, and terrorism-related fears. Am Psychol. 2007;62(4):304–316. doi: 10.1037/0003-066X.62.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holman EA, Silver RC. Getting “stuck” in the past: Temporal orientation and coping with trauma. J Pers Soc Psychol. 1998;74(5):1146–1163. doi: 10.1037//0022-3514.74.5.1146. [DOI] [PubMed] [Google Scholar]
- 14.Parsons RG, Ressler KJ. Implications of memory modulation for post-traumatic stress and fear disorders. Nat Neurosci. 2013;16(2):146–153. doi: 10.1038/nn.3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holman EA, et al. Terrorism, acute stress, and cardiovascular health: A 3-year national study following the September 11th attacks. Arch Gen Psychiatry. 2008;65(1):73–80. doi: 10.1001/archgenpsychiatry.2007.6. [DOI] [PubMed] [Google Scholar]
- 16.Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. J Health Soc Behav. 1995;36(4):360–376. [PubMed] [Google Scholar]
- 17.McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: A test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 2010;40(10):1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seery MD, Holman EA, Silver RC. Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. J Pers Soc Psychol. 2010;99(6):1025–1041. doi: 10.1037/a0021344. [DOI] [PubMed] [Google Scholar]
- 19. American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Assoc, Washington, DC), 4th Ed.
- 20.Bryant RA, et al. Hypnotherapy and cognitive behaviour therapy of acute stress disorder: A 3-year follow-up. Behav Res Ther. 2006;44(9):1331–1335. doi: 10.1016/j.brat.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Biddinger PD, et al. Be prepared—the Boston Marathon and mass-casualty events. N Engl J Med. 2013;368(21):1958–1960. doi: 10.1056/NEJMp1305480. [DOI] [PubMed] [Google Scholar]
- 22.Brosschot JF. Markers of chronic stress: Prolonged physiological activation and (un)conscious perseverative cognition. Neurosci Biobehav Rev. 2010;35(1):46–50. doi: 10.1016/j.neubiorev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Gerin W, et al. Rumination as a mediator of chronic stress effects on hypertension: A causal model. Int J Hypertens. 2012;2012:453–465. doi: 10.1155/2012/453465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watkins ER. Constructive and unconstructive repetitive thought. Psychol Bull. 2008;134(2):163–206. doi: 10.1037/0033-2909.134.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ottaviani C, Shapiro D, Fitzgerald L. Rumination in the laboratory: What happens when you go back to everyday life? Psychophysiology. 2011;48(4):453–461. doi: 10.1111/j.1469-8986.2010.01122.x. [DOI] [PubMed] [Google Scholar]
- 26.Kubzansky LD, et al. Is worrying bad for your heart? A prospective study of worry and coronary heart disease in the Normative Aging Study. Circulation. 1997;95(4):818–824. doi: 10.1161/01.cir.95.4.818. [DOI] [PubMed] [Google Scholar]
- 27.D’Andrea W, Sharma R, Zelechoski AD, Spinazzola J. Physical health problems after single trauma exposure: When stress takes root in the body. J Am Psychiatr Nurses Assoc. 2011;17(6):378–392. doi: 10.1177/1078390311425187. [DOI] [PubMed] [Google Scholar]
- 28.Goodwin R, Palgi Y, Hamama-Raz Y, Ben-Ezra M. In the eye of the storm or the bullseye of the media: Social media use during Hurricane Sandy as a predictor of post-traumatic stress. J Psychiatr Res. 2013;47(8):1099–1100. doi: 10.1016/j.jpsychires.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Stefanone MA, Lackaff D, Rosen D. The relationship between traditional mass media and “ social media”: Reality television as a model for social network site behavior. J Broadcast Electron Media. 2010;54(3):508–525. [Google Scholar]
- 30.Young ME, King N, Harper S, Karin R. The influence of popular media on perceptions of personal and population risk in possible disease outbreaks. Health Risk Soc. 2013;15(1):37–41. [Google Scholar]
- 31.Faasse K, Gamble G, Cundy T, Petrie KJ. Impact of television coverage on the number and type of symptoms reported during a health scare: A retrospective pre-post observational study. BMJ Open. 2012;2(4):1–7. doi: 10.1136/bmjopen-2012-001607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bass E, Kaplan-Liss E, Dorf D, Broderick JE. A challenging empirical question: What are the effects of media on psychogenic illness during a community crisis? J Community Med Health Educ. 2012;2(1):1–5. doi: 10.4172/jcmhe.1000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. US Department of Health and Human Services, National Center for Health Statistics (2000) National Health Interview Survey Questionnaire 2000. Available at www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm#2000_NHIS.
- 34.Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences. New York: Oxford Univ Press; 2007. [Google Scholar]
- 35.Putnam FW. Televised trauma and viewer PTSD: Implications for prevention. Psychiatry. 2002;65(4):310–312. doi: 10.1521/psyc.65.4.310.20241. [DOI] [PubMed] [Google Scholar]
- 36. US Department of Commerce, US Census Bureau (2012) American Community Survey. Available at www.census.gov/acs/www/
- 37.Cardeña E, Koopman C, Classen C, Waelde LC, Spiegel D. Psychometric properties of the Stanford Acute Stress Reaction Questionnaire (SASRQ): A valid and reliable measure of acute stress. J Trauma Stress. 2000;13(4):719–734. doi: 10.1023/A:1007822603186. [DOI] [PubMed] [Google Scholar]
- 38.Baker LC, Bundorf MK, Singer S, Wagner TH. Validity of the Survey of Health and Internet and Knowledge Network’s Panel and Sampling. Stanford, CA: Stanford Univ; 2003. [Google Scholar]
- 39.Andridge RR, Little RJ. A review of Hot Deck imputation for survey non-response. Int Stat Rev. 2010;78(1):40–64. doi: 10.1111/j.1751-5823.2010.00103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cox BG (1980) The weighted sequential hot deck imputation procedure. Proceedings of the Survey Research Methods Section (American Statistical Association, Chicago), pp 721–726.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.