Abstract
Background:Recently, Mikulicz’s disease has been defined as an IgG-4 related disease, a systemic condition, where the hallmark pathology findings are lymphoplasmacytic infiltrates, immunoglobulin (Ig)G4-positive plasma cells, modest tissue eosinophilia, and intense fibrosis.
Case:We present a case of 63-year-old man who showed epigastralgia and elevated serum lipase levels. Computed tomography of the abdomen revealed a bulky mass of the pancreas, so he underwent bilious-digestive anastomosis, and biopsy of the pancreas revealed massive infiltration of lymphocytes and plasma cells. The patient was therefore diagnosed with sclerosing chronic pancreatitis (Kuttner’s tumour). After one year, the patient began to exhibit signs of “sicca syndrome”, and at the same time, he demonstrated progressive renal failure. Immunological tests showed hypocomplementemia, and the renal biopsy specimen demonstrated interstitial inflammation, in which infiltrate was composed of lymphocytes, while infiltrating plasma cells showed immunoreactivity to IgG4. Sialography revealed severe involvement of the salivary glands, and Schirmer’s test resulted positive.
Conclusions: Here, we report successful treatment of the first case in Italy of a patient with hypocomplementemic tubulointerstitial nephritis in IgG4-related disease.
Keywords: Hypocomplementemic tubulointerstitial nephritis, Mikulicz’s disease, IgG-4 related disease
Introduction
Mikulicz’s disease (MD) has always been considered a subtype of Sjogren’s syndrome (SS), and refers to bilateral and symmetrical swelling of the parotid, submandibular and lacrimal glands, associated with autoimmune pancreatitis. Recently, it was also confirmed that MD patients show infiltration of plasmacytes, which express IgG4 in several tissues. Furthermore, since many patients also show elevated serum immunoglobulin IgG4, it has been defined as a systemic IgG4-related plasmacytic syndrome (SIPS), IgG4+ multiorgan lymphoproliferative syndrome (IgG4+ MOLPS) or IgG-4 related disease (1,2). The last term has been coined by Umehara group in Japan in 2010 (3). The incidence rate of new cases is 2.63-10.2 per 1 million people. The male-female ratio is approximately 5:1. The possible complications of IgG-4 related disease include autoimmune pancreatitis, tubulointerstitial nephritis, retroperitoneal fibrosis, prostatitis, hypophysitis, and Riedel’s thyroiditis. Hypocomplementemia was observed in 30% of cases, and antinuclear antibodies were only found in 15% of these patients, while neither anti-SS-A nor anti-SS-B antibodies were detected (4).
The typical histopathological finding is a lymphoplasmacytic infiltrate in the great majority of cases. A cuff of lymphocytes surrounding ducts tends to be present when the disease involves glands such as the pancreas or salivary glands. T cells, specifically CD8+ T-suppressor cells, dominate the lymphoid infiltrate. No clonality has been demonstrated in T- or B-cell subsets. The lymphoplasmacytic infiltrates are associated with fibrosis that generally occurs in a storiform pattern. The cytoplasm of a high percentage of plasma cells within tissue of patient with IgG4– related disease stain intensely for IgG4. The nucleus is unstained and readily visible. Positive staining for IgG4 can clinch the diagnosis in the appropriate clinical setting. The numbers and percentages of IgG4-positive cells probably vary from tissue to tissue and by stage of disease. In general, however, one can feel comfortable about diagnosis in the setting of 30 IgG4-positive plasma cells or greater per high-power field, and an IgG4: total IgG ratio of greater than 50%.
The proposed diagnostic criteria for systemic IgG4-related disease are:
-
1. Elevated serum IgG4 (> 135 mg/dl).
AND
2. Histopathological features including lymphocyte and IgG4+ plasma cell infiltration (IgG4+ plasma cells/ IgG+ plasma cells> 40%) with typical tissue fibrosis or sclerosis.
Between diagnostic guideline for suspicious IgG4-related disease, the presence of only one can be enough for the diagnosis:
1) Symmetrical swelling of one of the lacrimal, parotid or submandibular glands.
2) Autoimmune pancreatitis.
3) Inflammatory pseudotumor.
4) Retroperitoneal fibrosis.
5) Histopathological findings are similar to lymphoplasmacytosis or suspected Castleman’s disease.
Renal involvement is referred as “IgG4-related kidney disease”, as proposed in the nomenclature consensus statement from International Symposium on IgG4-related disease, held in Boston, USA, in October 2011 (5).
Here, we report on the successful treatment of the first case in Italy of a patient with hypocomplementemic tubulointerstitial nephritis in IgG4-related disease.
Case
A 63-year-old obese, hypertensive male was admitted to our hospital in October 2007, because of epigastralgia and elevated serum lipase levels. Computed tomography of the abdomen revealed tumour-like (Kuttner’s tumour) swelling of the pancreatic tail. Serum gamma globulin levels had increased to 36%. The patient underwent bilious-digestive anastomosis, and biopsy of the pancreas revealed massive infiltration of lymphocytes and plasma cells. The patient was therefore diagnosed with sclerosing chronic pancreatitis (Fig. 1). In January 2008, the patient began to show signs of “sicca syndrome” with xerostomia, xerophthalmia and chronic rhinitis. At the same time, he suffered from symptoms of prostatitis. In December 2008, laboratory tests revealed severe renal failure (sCr, 3.9 mg/dl) and the amount of proteinuria over 24 hours was 0.5 g. Therefore, he was referred to our division for further examination. The patient’s medical records showed that his sCr was 1.1 mg/dl in January and 2.9 mg/dl in September. Immunological tests revealed hypocomplementemia (C3= 60 mg/dl; C4= 3 mg/dl), speckled positivity for antinuclear antibodies (1:160), hypersedimentation (120 mm per 1st hour) and polyclonal increase of IgG (3002 mg/dl). Other serological markers were negative, including anti–RNP, anti SS-A, anti SS-B, and antineutrophil cytoplasmic antibodies.
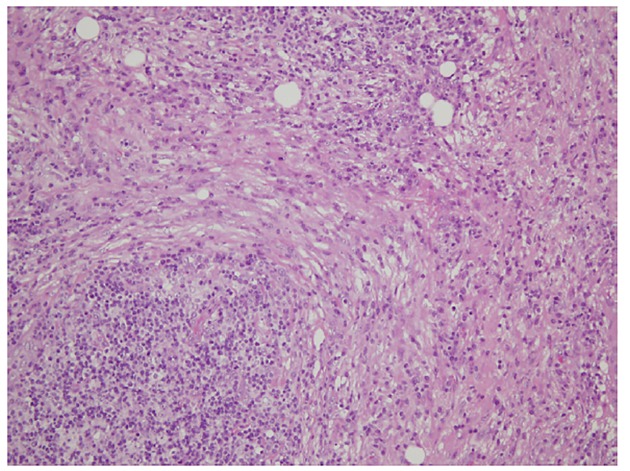
Figure1.
sclerosing chronic pancreatitis
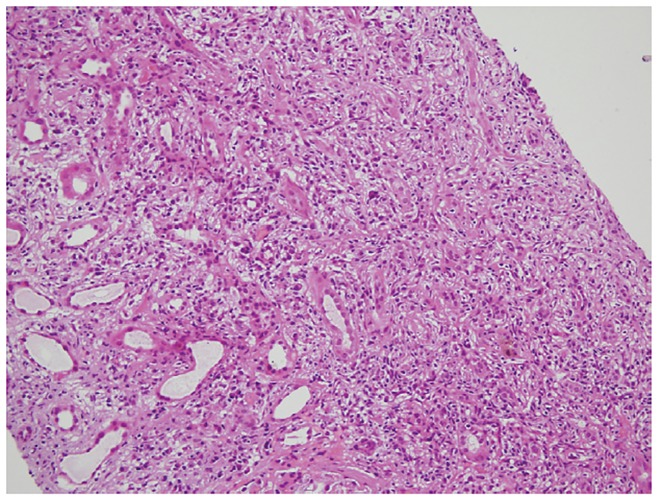
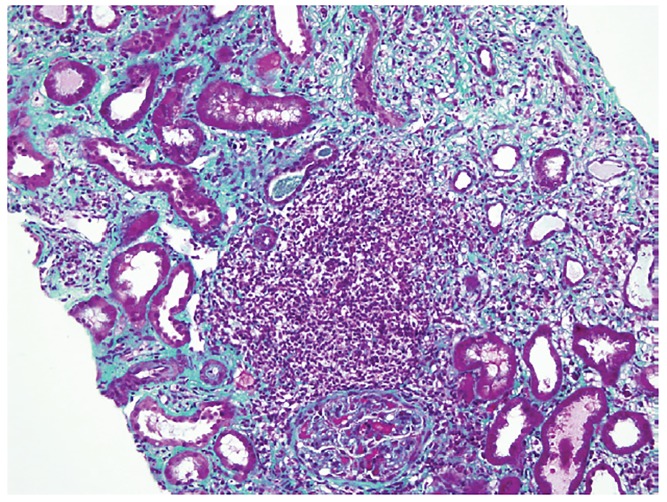
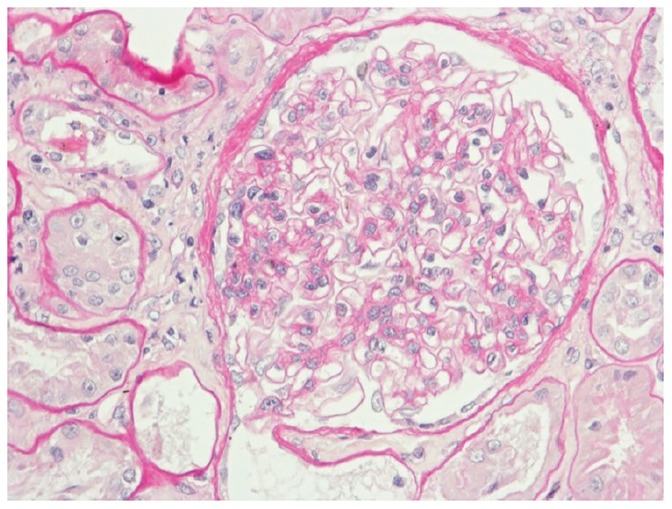
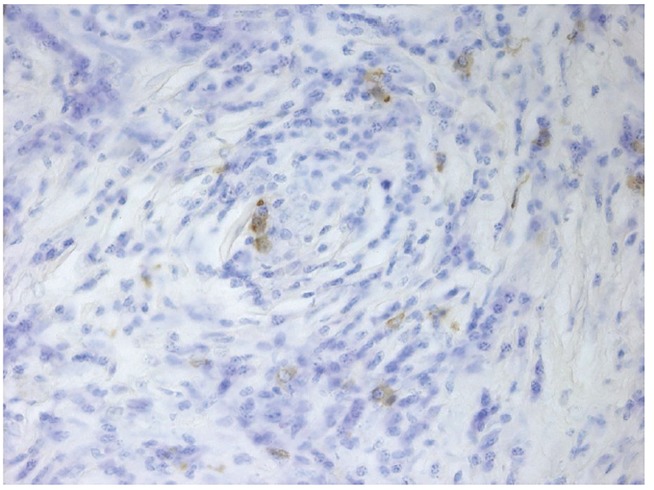
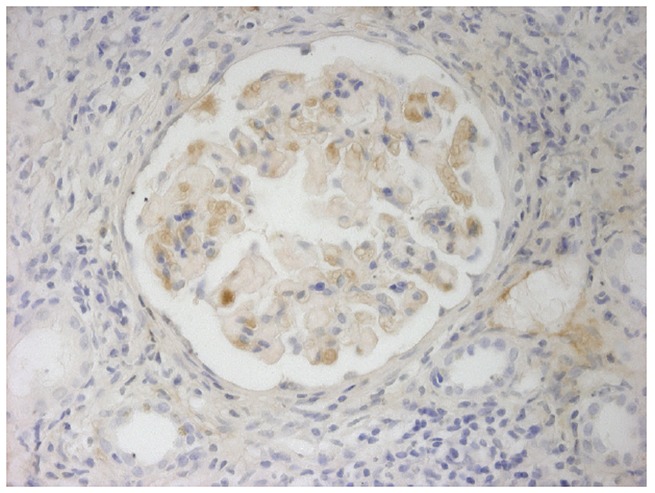
The renal biopsy specimen demonstrated diffuse interstitial inflammation in which the inflammatory cell infiltrate was composed of lymphocytes (mostly CD20+ B-cells) and plasma cells (Fig. 2-3-4). The only unusual feature of the glomeruli was the thickened Bowman’s capsule. Immunofluorescence examination showed no immunoglobulin deposits or complement components, but immunostaining of paraffin-embedded sections, using anti-IgG4 antibody, revealed infiltration of plasmacytes with IgG4 (Fig.5A-B).
Figures 2,3,4.
Renal biopsy specimen demonstrated diffuse interstitial inflammation in which the inflammatory cell infiltrate was composed of lymphocytes (mostly CD20+ B-cells) and plasma cells.
Figure 5 (A-B).
Immunostaining of paraffin-embedded sections, using anti-IgG4 antibody, revealed infiltration of plasmacytes with IgG4
Electron microscopy showed foot process fusion with microvillous transformation and segmental collapse of the capillary tufts.
Sialography using a radioisotope revealed severe involvement of the salivary glands. Schirmer’s test resulted positive, and showed 12 mm wetting per 5 min in both eyes, which is an expression of severe lacrimal hyposecretion.
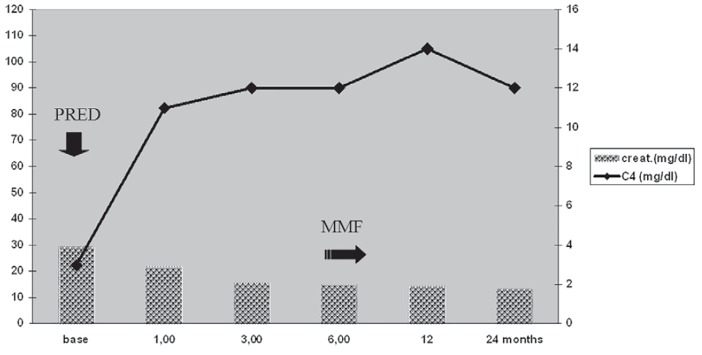
Therefore, we made a diagnosis of hypocomplementemic tubulointerstitial nephritis in IgG-4 related disease. Therefore, our patient received oral prednisone (0.5 mg/Kg for two months, then 5 mg/day as daily maintenance) following three courses of intravenous methylprednisolone pulse therapy (125 mg). After beginning therapy, we observed rapid improvement, including disappearance of the “sicca syndrome” and progressive amelioration of renal function. C3 and C4 normalised, as did the erythrocyte sedimentation rate (Fig. 6).
Figure 6.
Rapid improvement, including disappearance of the “sicca syndrome” and progressive amelioration of renal function.
After six months, we discontinued steroid administration and started mycophenolate mofetil (500 mg twice daily) to maintain a low degree of immunosuppression. Follow-up after two years showed that this therapy continued to be quite effective in our patient.
Discussion
In 1888, Johann von Mikulicz reported a patient who showed bilateral, painless, and symmetrical swelling of the lacrimal, parotid, and submandibular glands. On the other hand, in 1933, Sjogren analysed 19 cases with keratoconjunctivitis sicca, 2 of whom showed swelling of the major salivary glands (4). Subsequently, Mikulicz’s disease (MD) came to be considered as a subtype of Sjogren syndrome (SS), and patients with MD were no longer reported. Recently, Yamamoto et al reported that patients with MD have significantly higher serum IgG4 levels than do patients with SS. Clinical analyses performed on 40 patients (mainly middle-aged or elderly females) with systemic IgG4-related plasmacytic syndrome revealed 33 cases with MD and so a new conceptualisation of MD as an IgG4-related disease was made (1). Among their forty patients, the systemic complications revealed autoimmune pancreatitis (Kuttner’s tumour), retroperitoneal fibrosis, prostatitis, hypophysitis, Riedel’s thyroiditis and tubulointerstitial nephritis. Hardly any of the patients had anti-SS-A or anti-SS –B antibodies. Antinuclear antibodies were detected in 15% of the cases, and, very interestingly, hypocomplementemia was identified in 30% of the 40 patients. The cause of hypocomplementemia is not clear, since IgG-4 is unable to activate the classical pathway.
Immunoglobulin G4 (IgG4), the rarest of the IgG subclasses to be expressed, is a T-helper 2–dependent isotype, and IL-4 drives human B cells to switch to IgG4 and IgE production. It is unable to bind c1q complement and therefore it cannot activate the classic complement pathway. Nonetheless, some kinds of IgG4 have an Fc-binding reactivity in the constant region, and, in immune complexes, IgG4 may appear as a rheumatoid factor to other subclasses of IgG, thus possibly inducing hypocomplementemia (6). Immune-mediated tubulointerstitial nephritis with no significant glomerular involvement has been reported in antitubular basement membrane antibody-related disease, in SS and in a small subset of lupus nephritis.
Our case, the first in Italy, showed almost all the symptoms of IgG-4 related disease (“sicca syndrome” associated with autoimmune pancreatitis, prostatitis, hypocomplementemia, speckled pattern ANA positivity, progressive renal failure), and renal biopsy revealed tubulointerstitial nephritis with infiltrating plasma cells that showed immunoreactivity to IgG4.
Takeda et al described a similar case, which was associated with autoimmune pancreatitis, and the biopsy showed positive staining of IgG4 with C3c along the tubular basement membrane (7).
In 2001, Kambham et al reported eight cases of idiopathic hypocomplementemic interstitial nephritis, and the clinical pathological features were similar to those of IgG4-related disease (8). In particular, two of their eight patients had sclerosing cholangitis and three out of six patients were positive for ANA. The results of the renal biopsies ranged from evidence of tubulointerstitial nephritis to atypical lymphoid hyperplasia. It is likely that all these findings were consistent with a diagnosis of IgG-4 related disease.
The disease is a multifaceted disorder and early diagnosis is mandatory.
Steroid administration is the most common type of treatment for IgG-4 related disease, and, in our case, such treatment induced rapid improvement, including the disappearance of the “sicca syndrome”, normalisation of C3 and C4, and progressive amelioration of renal function (9).
In conclusion, this case underscores the need for keeping a high index of suspicion for the diagnosis of this challenging group of disorders with involvement of a multitude of organs and protean manifestations. Its early diagnosis and management can help save the patients from considerable morbidity.
Authors’ contributions
DR prepared the primary draft. JLR, MPR and PS reported the pathology. DB and GP provided extensive intellectual contribution. DR prepared the final manuscript.
Conflict of interest
The author declared no competing interests.
Funding/Support
None declared
Implication for health policy/practice/research/medical education:
Recently, Mikulicz’s disease has been defined as an IgG-4 related disease, a systemic condition, where the hallmark pathology findings are lymphoplasmacytic infiltrates, IgG-4-positive plasma cells, modest tissue eosinophilia, and intense fibrosis.
Please cite this paper as:Rolla D, Bellino D, Peloso GC, Rastaldi MP, Simonini P, Ravetti JL. The first case of IgG4-related disease in Italy.J Nephropathology. 2013; 2(2): 144-149. DOI: 10.5812/nephropathol.10549
References
- 1.Yamamoto M, Takahashi H, Ohara M, Suzuki C, Naishiro Y, Yamamoto H, Shinomura Y, Imai K. A new conceptualization for Mikulicz’s disease as an IgG4-related plasmacytic disease. Mod Rheumatol. 2006;16(6):335–40. doi: 10.1007/s10165-006-0518-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neild GH, Rodriguez-Justo M, Wall C, Connolly JO. Hyper-IgG4 disease: report and characterisation of a new disease. BMC Med. 2006;4:23. doi: 10.1186/1741-7015-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masaki Y, Kurose N, Umehara H. IgG4-related disease: a novel lymphoproliferative disorder discovered and established in Japan in the 21st century. J ClinExpHematop. 2011;51(1):13–20. doi: 10.3960/jslrt.51.13. [DOI] [PubMed] [Google Scholar]
- 4.Sjogren H. ZurKenntnis der Kerato-conjunctivitis sicca (Keratitis filiformisbeihypofunktion der Tranendrusen) ActaOphthalmol. 1933;11:1–151. [Google Scholar]
- 5.Cornell LD. IgG4-related kidney disease. CurrOpinNephrolHypertens. 2012;21(3):279–88. doi: 10.1097/MNH.0b013e32835265ac. [DOI] [PubMed] [Google Scholar]
- 6.Punnonen J, Aversa G, Cocks BG, McKenzie AN, Menon S, Zurawski G. et al. Interleukin 13 induces interleukin 4-independent IgG4 and IgE synthesis and CD23 expression by human B cells. Proc Natl Acad Sci U S A. 1993;90(8):3730–4. doi: 10.1073/pnas.90.8.3730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takeda S, Haratake J, Kasai T, Takaeda C, Takazakura E. IgG4-associated idiopathic tubulointerstitial nephritis complicating autoimmune pancreatitis. Nephrol Dial Transplant. 2004;19(2):474–6. doi: 10.1093/ndt/gfg477. [DOI] [PubMed] [Google Scholar]
- 8.Kambham N, Markowitz GS, Tanji N, Mansukhani MM, Orazi A, D’Agati VD. Idiopathichypocomplementemic interstitial nephritis with extensive tubulointerstitial deposits. Am J Kidney Dis. 2001;37(2):388–99. doi: 10.1053/ajkd.2001.21320. [DOI] [PubMed] [Google Scholar]
- 9.Chacko S, Taskapan H, Roscoe J, Stein J, Woods E, Denton T, etal etal. Treatment of hyper-IgG4 disease with sequential corticosteroids and tamoxifen - case report and review of the literature. ClinNephrol. 2009;72(5):414–7. doi: 10.5414/cnp72414. [DOI] [PubMed] [Google Scholar]