Abstract
Chronic myelogenous leukemia (CML) is a malignant clonal disorder of hemopoietic stem cells characterized by abnormal proliferation and accumulation of immature granulocyte. Leukostasis is one of the complications of CML and is characterized by partial or total occlusion of microcirculation by aggregation of leukemic cells and thrombi leading to respiratory, ophthalmic or neurologic symptoms. We experienced a rare case of avascular necrosis of the femoral head as the initial presentation of chronic myelogenous leukemia. A 24-year-old male patient was admitted to our hospital with pain in the right hip joint. The patient was diagnosed to be suffering from chronic myelogenous leukemia by packed marrow with granulocytic and megakaryocytic hyperplasia and the presence of Philadelphia chromosome. The right hip joint pain was attributed to avascular necrosis of the femoral head. And the avascular necrosis could be considered as the complication of chronic myelogenous leukemia due to microcirculatory obstruction of the femoral head. The avascular necrosis of the right femoral head was treated with bipolar hemiarthoplasty.
Keywords: Femur Head, Osteonecrosis; Leukostasis; Leukemia, Myeloid, Chronic
INTRODUCTION
Chronic myelogenous leukemia (CML) is a malignant clonal disorder of hemopoietic stem cells characterized by abnormal proliferation and accumulation of immature granulocytes. CML is consistently associated with translocation t (9;22), the Philadelphia chromosome.
CML is prevalent in adults with a median age of onset around 50 years. Leukostasis is one of the complications of CML and is characterized by partial or total occlusion of microcirculation by aggregation of leukemic cells and thrombi leading to respiratory, ophthalmic or neurologic symptoms. Avascular necrosis of bone occurs in the areas with poor collateral circulation when the only branch supplying blood is unable to fulfill the requirements of the bone. Commonly affected areas are head of the femur, head of the humerus, femoral condyles and tibial plateau. Very few cases dealing with CML and avascular necrosis due to leukostasis have been reported. Here, we report a rare case of 21 year-old male patient with avascular necrosis of right femoral head owing to leukostasis as the initial presentation of CML.
CASE REPORT
A 21-year-old male patient was presented with pain in the right hip joint for 2 months. He was a soldier and went to the dispensary of the unit that he belonged to. He was referred to our hospital for further evaluation of abnormal complete blood cell count which was performed at the dispensary. The patient suffered from weight loss, mild dyspnea, fatigue, intermittent fever, and night sweat. The further history was uneventful.
Upon physical examination, it was observed that the patient was in poor general condition with pallor skin and anemic conjunctiva. There were no signs of hemorrhagic diathesis or icterus. The spleen was palpable below the umbilicus and had a firm consistency. Cervical and inguinal lymph nodes were palpable. Heart and lungs were without any pathologic findings. The chest X-ray and electrocardiography were normal.
Laboratory investigations revealed leukocytosis with leukocyte count of 96,800/mm3, increased platelets with a count of 684,000/mm3, and hemoglobin level of 10.4 g/dL. The peripheral blood smear revealed 1% blast cells. Microbiology findings were sterile cultures of blood and urines.
Bone marrow examination revealed that the entire marrow space was packed with granulocytes and megakaryocytes. The bone marrow biopsy showed marked hypercellularity and the estimated cellularity was near 100%. The bone marrow aspiration showed 0.4% myeloblasts, 6% promyelocytes, 13.2% myelocytes, 15.2% metamyelocytes, 14.7% band neutrophils, 40% segmented neutrophils, 2.7% eosinophils, 0% basophils, 0.8% monocytes, 0.4% pronormoblasts, 0% lymphoblasts, 0% immature lymphocytes, 0.4% lymphocytes, 0.4% plasma cells, and 0% histiocytes suggesting chronic phase of CML. Chromosomal analysis of bone marrow revealed Philadelphia chromosome, t (9;22) and molecular cytogenetics also showed bcr-abl positive.
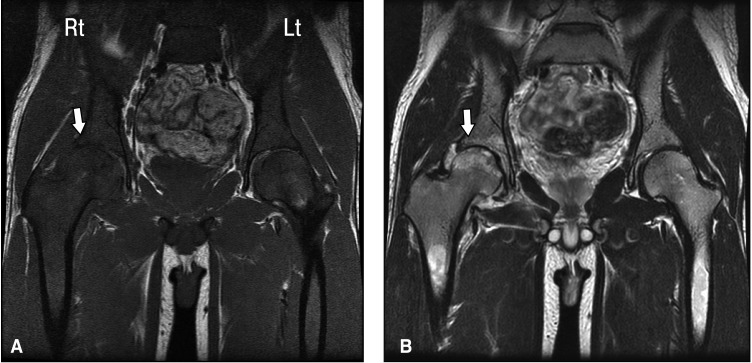
Treatment with hydroxyurea was induced, combined with immediate evaluation of right hip joint pain. Radiolucency superimposing the right femoral head was seen on the pelvic X-ray (Figure 1). Whole body bone scan showed increased uptake of the right hip joint. Magnetic resonance imaging (MRI) of both the hips revealed inhomogenously decreased signal intensity in the both proximal femur and acetabulum on T1 weighted images. The outer areas surrounding these areas had increased signal densities on T2 weighted images (Figure 2). On application of contrast medium, area with former decreased signal density on the cranial part of the right femoral head and some smaller areas of the left femoral head, showed a lack of signal enhancement. Bilateral joint effusion, worse in the right than the left, was also seen. All together, MRI showed signs of necrosis of both the femoral heads.
Figure 1.
Pelvic radiography. Radiolucency superimposing the right femoral head can be observed.
Figure 2.
MRI of both the hip joints. (A) The left picture shows inhomogenously decreased signal intensity in the both proximal femur and acetabulum on T1 weighted images. (B) In the right picture, the outer areas of these areas had increased signal densities on T2 weighted images.
The leukocyte count decreased from 96,800/ul to 26,300/mm3 with the treatment of hydroxyurea (3 g/day) for 2 weeks and subsequently hydroxyurea was replaced with imatinib mesyalte. With this treatment leukocytes were reduced from 96,800/mm3 to 8,900/mm3 within 3 weeks. The size of the spleen decreased to 3 cm below the costal margin within 1 month.
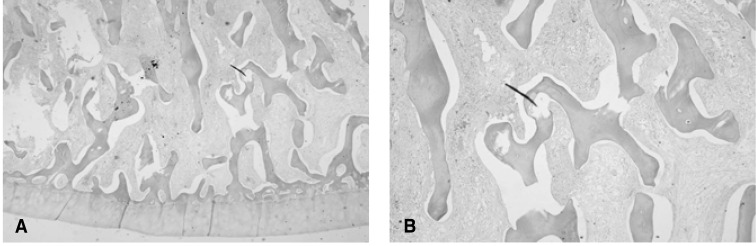
Following normalization of the peripheral blood counts, the patient was transferred to the department of Orthopedics. He underwent a bipolar hemiarthoplasty of the right hip joint, because the necrosis of the right hip joint was more severe than the left and he had no pain in the left hip joint. The postoperative course was complicated due to bleeding from the operative site possibly due to thrombocytopenia which may have been induced by imatinib mesylate. Temporarily, the medication of imatinib mesylate was stopped, and the patient was transfused with platelets and packed red cells. The biopsy revealed focal subchondral necrotic areas in the right hip joint (Figure 3).
Figure 3.
Biopsy of the right hip joint. The cut surface shows focal subchondral necrotic area with pale yellow color, (A) H&E, ×20, (B) H&E, ×40.
The patient was on a continuous follow up and showed no complications with complete cytogenetic response and has been on medication of imatinib mesylate (400 mg/day).
DISCUSSION
CML is characterized by a chronic phase which lasts from months to years, and is followed by accelerated myeloproliferative phase and subsequently blast crisis. In the chronic phase, manifestations include anemia, splenomegaly, bleeding, and constitutional symptoms such as fatigue, lethargy, weight loss, or low-grade fever. As in the present case study our case of a 21-year-old male, symptoms secondary to leukostasis may also be the presenting features1).
Leukostasis is defined as a pathological entity. Since there are no reliable clinical criteria, in practice, leukostasis is empirically diagnosed when patients present with leukemia, hyperleukocytosis and respiratoy or neurologic distress2). However, some patients have clinically suspected or pathologically proven leukostasis with leukemic blast counts significantly lower than 100,000/mm33).
The biological mechanism underlying development and progression of leukostasis still remains unclear. Litchmann proposed a pathophysiological model of leukostasis, based on the rheological consequences of hyperleukocytosis. He determined that the viscosity of leukocyte suspensions in vitro increased dramatically when the fractional volume of leukocytes (also known as leukocrit) exceeded 12~15 mL/dL4). The concentration of leukocytes necessary to produce such leukocrits is a function of the mean cell volume (MCV) of the cells. Since leukemic myeloblasts have larger MCV than leukemic lymphoblasts, leukostasis is more frequently observed in patients with acute or chronic myelogenous leukemia than in patients with acute or chronic lymphoblastic leukemia5). However, leukemic blast concentrations necessary to reach leukocrit of 12~15 mL/dL are rarely seen. Therefore, additional factors possibly related to the adhesive or invasive properties of leukemic blasts, may be more important. There are indications that leukemic blast-endothelial cell interactions may be triggered by locally released chemoattractant factors6). Complement-induced granulocyte aggregation is a well documented mechanism of leukostasis7). Several adhesion molecules (CD54, CD62E, CD62P, CD106) are up-regulated in endothelial cell of AML patients with leukocytosis6). Blasts appear to have the ability to secrete cytokines such as TNF-α and interleukin-1β and therefore bring about the activation of endothelium. For instance, activation of vascular endothelium by tumor necrosis factor-alpha (TNF-α) has been reported to increase the adhesion of myeloid blasts8).
Once leukocytosis is developed, signs and symptoms are usually related to the involvement of the respiratory or central nervous system. Additional but less common clinical findings include neck vein distension, gallop rhythm and electrocardiographic sign of right ventricular overload, myocardial ischemia, priapism, acute limb ischemia, bowel infarctions, renal vein thrombosis, sudden bilateral deafness and avascular necrosis of bone2). Until now, in CML, avascular necrosis of femoral head due to leukostasis has not been adequately documented, probably due to the rarity of its occurrence. After reviewing the world medical literature, we encountered only few cases of CML associated with avascular necrosis of femoral head9-13).
The current standard of care for hyperleukocytosis and leukostasis should be the immediate initiation of intravenous fluids, allopurinol, hydroxyurea and the correction of coagulopathy and thrombocytopenia2). Due to paucity of data on the efficacy of leukapheresis in reducing early mortality and/or improving overall survival, leukapheresis cannot be recommended as routine therapy14). Unfortunately there are no evidences to prove that any of these measures have produced a reduction in the number of early deaths.
A variety of traumatic and nontraumatic factors contribute to the etiology of avacular necrosis. In adult patients, corticosteroid use and excessive alcohol intake are reported to account for more than 90 percent of cases15). Additionally, other causes of avascular necrosis are systemic lupus erythematus, antiphospholipid antibody, trauma, sickle cell hemoglobinopathes, Gaucher's disease, Caisson disease (dysbarism), transplantation, interferon-α, inherited thrombophilia, or HIV infection16-19). Avascular necrosis usually occurs in the anterolateral femoral head, although it may also affect the humeral head, femoral condyles, proximal tibia, vertebrae, and small bones of the hand and foot20). Many patients have bilateral involvement at the time of diagnosis, including disease of the hips, knees, and shoulders. The goal of therapy for avascular necrosis is to preserve the naive joint for as long as possible. However, the optimal treatment has yet to be determined.
References
- 1.Enlight H, McGrave P. Chronic myelogenous leukemia. In: Hoffman R, Benz EJ Jr, Shattil SJ, Furie B, Cohen HJ, Silberstein LE, McGrave P, editors. Hoffman's hematology: basic principles and practice. 3rd ed. Churchill Livingstone; 2000. pp. 1156–1171. [Google Scholar]
- 2.Porcu P, Cripe LD, Ng EW, Bhatia S, Danielson CM, Orazi A, McCarthy LJ. Hyperleukocytic leukemias and leukostasis: a review of pathophysiology, clinical presentation and management. Leuk Lymphoma. 2000;39:1–18. doi: 10.3109/10428190009053534. [DOI] [PubMed] [Google Scholar]
- 3.Soares FA, Landell GA, Cardoso MC. Pulmonary leukostasis without hyperleukocytosis: a clinicopathologic study of 16 cases. Am J Hematol. 1992;40:28–32. doi: 10.1002/ajh.2830400106. [DOI] [PubMed] [Google Scholar]
- 4.Lightman MA. Rheology of leukocytes, leukocyte suspensions, and blood in leukemia. J Clin Invest. 1973;52:350–358. doi: 10.1172/JCI107191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lichtman MA, Heal J, Rowe JM. Hyperleukocytic leukemia: rheological and clinical features and management. Baillieres Clin Haematol. 1987;1:725–746. doi: 10.1016/s0950-3536(87)80022-7. [DOI] [PubMed] [Google Scholar]
- 6.Stucki A, River AS, Gikic M, Monai N, Schapira M, Spertini O. Endothelial cells activation by myeloblast : molecular mechanism of leukostasis and leukemic cell dissemination. Blood. 2001;97:2121–2129. doi: 10.1182/blood.v97.7.2121. [DOI] [PubMed] [Google Scholar]
- 7.Kubo H, Graham L, Doyle NA, Quinlan WM, Hogg JC, Doershuck CM. Complement fragment-induced release of neutrophils from bone marrow and sequestration within pulmonary capillaries in rabbits. Blood. 1998;92:283–290. [PubMed] [Google Scholar]
- 8.Stucki A, Rivier AS, Gikic M, Monai N, Schapira M, Spertini O. Endothelial cell activation by myeloblasts: molecular mechanisms of leukostasis and leukemic cell dissemination. Blood. 2001;97:2121–2129. doi: 10.1182/blood.v97.7.2121. [DOI] [PubMed] [Google Scholar]
- 9.Kraemer M, Weissinger F, Kraus R, Beer M, Kunzmann V, Wilhelm M. Aseptic necrosis of both femoral heads as first symptom of chronic myelogenous leukemia. Ann Hematol. 2003;82:44–46. doi: 10.1007/s00277-002-0576-y. [DOI] [PubMed] [Google Scholar]
- 10.Alabi ZO, Durosinmi MA. Legg-Calve-Perthes' disease associated with chronic myeloid leukemia in a child: case report. East Afr Med J. 1989;66:556–559. [PubMed] [Google Scholar]
- 11.Gibson J, Joshua DE, Collis D, Kronenberg H. Chronic myeloid leukaemia presenting as femoral head necrosis. Scand J Haematol. 1984;32:376–378. doi: 10.1111/j.1600-0609.1984.tb00691.x. [DOI] [PubMed] [Google Scholar]
- 12.Salimi Z, Vas W, Sundaram M. Avascular bone necrosis in an untreated case of chronic myelogenous leukemia. Skeletal Radiol. 1988;17:353–355. doi: 10.1007/BF00367182. [DOI] [PubMed] [Google Scholar]
- 13.Gupta D, Gaiha M, Siddaraju N, Daga MK, Anuradha S. Chronic myeloid leukemia presenting with avascular necrosis of femur head. J Assoc Physicians India. 2003;51:214–215. [PubMed] [Google Scholar]
- 14.Porcu P, Farag S, Marcucci G, Cataland SR, Kennedy MS, Bissell M. Leukocytoreduction for acute leukemia. Ther Apher. 2002;6:15–23. doi: 10.1046/j.1526-0968.2002.00402.x. [DOI] [PubMed] [Google Scholar]
- 15.Mont MA, Hungerford DS. Non-traumatic vascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459–474. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Abbott KC, Oglesby RJ, Agodoa LY. Hospitalized avascular necrosis after renal transplantation in the United States. Kidney Int. 2002;62:2250–2256. doi: 10.1046/j.1523-1755.2002.00667.x. [DOI] [PubMed] [Google Scholar]
- 17.Tauchmanova L, de Rosa G, Serio B, Fazioli F, Mainolfi C, Lombardi G, Colao A, Salvatore M, Rotoli B, Selleri C. Avascular necrosis in long-term survivors after allogeneic or autologous stem cell transplantation: a single center experience and a review. Cancer. 2003;97:2453–2461. doi: 10.1002/cncr.11373. [DOI] [PubMed] [Google Scholar]
- 18.Miller KD, Masur H, Jones EC, Joe GO, Rick ME, Kelly GG, Mican JM, Liu S, Gerber LH, Blackwelder WC, Falloon J, Davey RT, Polis MA, Walker RE, Lane HC, Kovacs JA. High prevalence of steonecrosis of the femoral head in HIV-infected adults. Ann Intern Med. 2002;137:17–25. doi: 10.7326/0003-4819-137-1-200207020-00008. [DOI] [PubMed] [Google Scholar]
- 19.Mankin HJ. Nontraumatic necrosis of bone. N Engl J Med. 1992;326:1473–1479. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 20.Chang CC, Greenspan A, Gershwin ME. Osteonecrosis: current perspectives on pathogenesis and treatment. Semin Arthritis Rheum. 1993;23:47–69. doi: 10.1016/s0049-0172(05)80026-5. [DOI] [PubMed] [Google Scholar]