Abstract
Eosinophilic fasciitis (EF) is scleroderma-like disease without Raynaud's phenomenon or visceral involvement. It is characterized by painful swelling of the extremities, accompanied by rapid weight gain, fever and myalgia. The acute state of disease is associated with significant peripheral blood eosinophilia, an elevated erythrocyte sedimentation rate and hypergammaglobulinemia. EF is also frequently associated with hematological abnormalities, including malignant lymphoproliferative diseases, but rarely associated with autoimmune thyroiditis. In the present study we report a case of eosinophilic fasciitis associated with autoimmune thyroiditis.
Keywords: Fasciitis, Eosinophilia, Autoimmune thyroiditis
INTRODUCTION
Eosinophilic fasciitis (EF) was first recognized by Shulman as scleroderma-like disease without Raynaud's phenomenon or visceral involvement1). It is characterized by painful and erythematous swelling of the extremities, accompanied by rapid weight gain, fever and myalgia. During acute period of the disease, most of the patients suffer from significant eosinophilia in peripheral blood, but is less commonly associated in affected tissues2). It has been reported that EF is usually related with various hematologic abnormalities, such as myelodysplastic syndrome and malignant lymphoproliferative disease3). The etiology of EF is still unclear, and its association with autoimmune disease has rarely been reported. In the present study, we report a case of eosinophilic fasciitis associated with autoimmune thyroiditis, with a review on the past literature.
CASE REPORT
A 45-year-old woman was referred to our hospital to evaluate the swelling on both the forearms lasting from past 3 months. She had intermittent cramp-like pain on both the forearms, which got aggravated by movement. The patient was placed on non-steroidal anti-inflammatory drugs intermittently. Raynaud's phenomenon was absent on past history.
Upon physical examination, both the upper extremities showed marked swelling without pitting or erythematous change, and there was no swelling in the hands. However, physician was able to pinch her skin on both the forearms. Laboratory findings revealed the white cell count of 7,200/mm3 with 13.8% of eosinophils (absolute counts 993/mm3), hemoglobin of 10.8 g/dl and platelet count of 319×103/mm3. Stool examination for the presence of parasites was negative. Peripheral blood smear showed normocytic and normochromic red blood cells and no atypical leukocytes were seen except for an increased level of eosinophils. Liver function test, renal function test, and levels of CRP, glucose, creatinine kinase, calcium, and phosphate were normal. Esophagogastroduodenoscopy, colonoscopy, ultrasonography, and chest radiography revealed no abnormal findings. The titer level of anti-nuclear antibody in IT-1 cell was 1:40 with speckled pattern, but rheumatoid factor and anti-neutrophil cytoplasmic antibody wrere negative.
Based on thyroid function test, the levels of thyroid stimulating hormone (TSH) and free thyroid hormone-4 (FT4), were 4.86 uIU/mL (normal 0.27~4.2 uIU/mL) and 0.85 ng/dL (normal 0.93-1.7 ng/dL), respectively. The titre values of antithyroglbulin antibodies and antimicrosomal antibodies were 1:1600 and 1:1600, respectively. No nodule was detected during ultrasonography of thyroid and there was no hot uptake by thyroid scan.
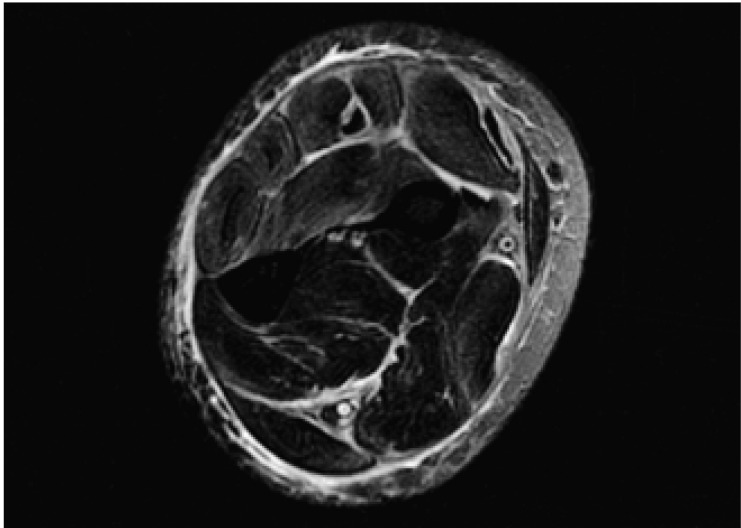
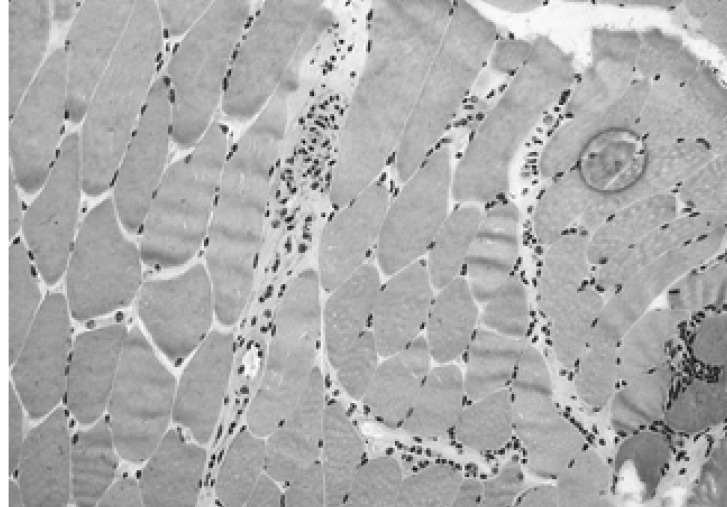
MRI demonstrated swelling and increased signal of muscles like extensor carpi ulnaris, extensor digitorum longus, and extensor carpi radialis, and there was thickening and edematous change of fascia around the muscles (Figure 1). Full-thickness wedge biopsy on extensor carpi radialis revealed the presence of thickened fibrous fascia with perivascular infiltration of lymphocytes, plasma cells and few eosinophils, and these findings were compatible with eosinophilic fasciitis (Figure 2). To the patient, we initially prescribed prednisone 30 mg/day, cetirizine 10 mg/day and levothyroxine sodium 0.1 mg/day. Hypereosinophilia disappeared immediately after treatment with prednisone and induration on both the forearms also improved gradually.
Figure 1.
MR of left forearm showing increased signal of extensor carpi ulnaris, extensor digitorum longus, and extensor carpi radialis muscles. There is thickening and edematous changes in fascia around these muscles.
Figure 2.
Muscle biopsy showing thickened fibrous fascia with perivascular infiltration of lymphocytes, plasma cells and few eosinophils (H&E, ×400).
DISCUSSION
Unlike scleroderma, the onset of EF is typically abrupt and in many cases occurs after excessive or unusual physical activity2). Induration is developed by progressive thickening of the skin and is common in the upper extremities with a symmetrical distribution4). Also, in contrast to scleroderma, the fingers, toes and the face are always the most affected padt. Laboratory investigations revealed significant peripheral blood eosinophilia in more than 60% of the patients5), an elevated erythrocyte sedimentation rate and hypergammaglobulinemia, whereas levels of muscle enzymes were normal6).
It has been reported that EF is usually related with various hematologic abnormalities, including myelodysplastic diseases and malignant lymphoproliferative disease3). It was demonstrated that the overall frequency of hematological disorders in EF was close to 10%4). Hematological diseases, such as thrombocytopenia and hemolytic anemia can be combined, and amongst them, aplastic anemia is the most commonly seen form2). Therefore, it is suggested that bone marrow aspirate may be essential if hematological diseases are suspected from laboratory findings. Murata et al.7) observed the presence of peripheral eosinophilia in 21% of adult T-cell leukemia/lymphoma, 11.1% of T-cell lymphoma and 10.5% of B-cell lymphoma. Rarely, peripheral neuropathy, carpal tunnel syndrome, and lymphadenopathy have been reported in association with EF3,8).
Autoimmune thyroiditis was reported in only 6 of the cases in English literatures. To date, 4 cases of EF were reported in Korea. One of them was associated with hematological disorder, but none of them were associated with autoimmune thyroid disorder9-12). In our case, the patient had no abnormal physical findings even in thyroid gland, except for abnormal thyroid hormone level. We could not find any other abnormal findings, although the patient was evaluated for hematologic malignancies. If on evaluation, the hematologic abnormalities are not accompanied with EF, it becomes still unclear whether bone marrow biopsy should be performed in all the EF patients. In those cases, we need to look for the appearance of hematologic malignancy.
Eventually, contracture could occur in 76% of the untreated patients with EF, and rarely there was any recovery2). Prednisolone at a daily dose of 1 mg/kg effectively improves edema and induration. Antihistamines, particularly cimetidine and cetirizine, have been anecdotally reported to be beneficial13). Treatment with other drugs such as penicillamine, methotrexate and psoralen-UVA have been reported to be beneficial14). In the present study we report the case of an EF patient associated with autoimmune thyroiditis. From the present study we contemplate that, when the diagnosis of EF is suspected, a careful investigation of the patient including thyroid function test is required.
References
- 1.Shulman LE. Diffuse fasciitis with hypergammaglobulinemia and eosinophilia: a new syndrome? J Rheumatol. 1984;11:569–570. [PubMed] [Google Scholar]
- 2.Doyle JA, Ginsburg WW. Eosinophilic fasciitis. Med Clin North Am. 1989;73:1157–1166. doi: 10.1016/s0025-7125(16)30625-3. [DOI] [PubMed] [Google Scholar]
- 3.Naschitz JE, Misselevich I, Rosner I, Yeshurun D, Weiner P, Amar M, Amato L, Ciompi ML, Boss JH. Lymph-node-based malignant lymphoma and reactive lymphadenopathy in eosinophilic fasciitis. Am J Med Sci. 1999;318:343–349. doi: 10.1097/00000441-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Lakhanpal S, Ginsburg WW, Michet CJ, Doyle JA, Moore SB. Eosinophilic fasciitis: clinical spectrum and therapeutic response in 52 cases. Semin Arthritis Rheum. 1988;17:221–231. doi: 10.1016/0049-0172(88)90008-x. [DOI] [PubMed] [Google Scholar]
- 5.Mori Y, Kahari VM, Varga J. Scleroderma-like cutaneous syndromes. Curr Rheumatol Rep. 2002;4:113–122. doi: 10.1007/s11926-002-0006-0. [DOI] [PubMed] [Google Scholar]
- 6.Helfman T, Falanga V. Eosinophilic fasciitis. Clin Dermatol. 1994;12:449–455. doi: 10.1016/0738-081x(94)90297-6. [DOI] [PubMed] [Google Scholar]
- 7.Murata K, Yamada Y, Kamihira S, Atogami S, Tsukasaki K, Momita S, Amagasaki T, Sadamori N, Tomonaga M, Kinoshita K. Frequency of eosinophilia in adult T-cell leukemia/lymphoma. Cancer. 1992;69:966–971. doi: 10.1002/1097-0142(19920215)69:4<966::aid-cncr2820690422>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 8.Farrell AM, Ross JS, Bunker CB. Eosinophilic fasciitis associated with autoimmune thyroid disease and myelodysplasia treated with pulsed methylprednisolone and antihistamines. Br J Dermatol. 1999;140:1185–1187. [PubMed] [Google Scholar]
- 9.Lee JB, Kim KS, Kim YK. Eosinophilic fasciitis: report of a case. Korean J Dermatol. 1980;18:361–365. [Google Scholar]
- 10.Park MK, Jeon SJ, Suh KS, Kim ST. A case of eosinophilic fasciitis. Korean J Dermatol. 1989;27:729–733. [Google Scholar]
- 11.Lee DH, Kim JH, Lee WB, Lee JS. A case of eosinophilic fasciitis. J Korean Pediatr Soc. 1996;39:120–125. [Google Scholar]
- 12.Kim H, Kim MO, Ahn MJ, Lee YY, Jung TJ, Choi IY, Kim IS, Park CK. Eosinophilic fasciitis preceding relapse of peripheral T-cell lymphoma. J Korean Med Sci. 2000;15:346–350. doi: 10.3346/jkms.2000.15.3.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solomon G, Barland P, Rifkin H. Eosinophilic fasciitis responsive to cimetidine. Ann Intern Med. 1982;97:547–549. doi: 10.7326/0003-4819-97-4-547. [DOI] [PubMed] [Google Scholar]
- 14.Blauvelt A, Falanga V. Idiopathic and L-tryptophan-associated eosinophilic fasciitis before and after L-tryptophan contamination. Arch Dermatol. 1991;127:1159–1166. [PubMed] [Google Scholar]