Abstract
Background
The N-terminal fragment of pro Brain Natriuretic Peptide (NT-pro BNP) is a neuro-hormone synthesized in the cardiac ventricles in response to increased wall tension. The purpose of this study was to assess the correlation between the NT-pro BNP levels and the New York Heart Association function class (NYHA Fc) of dyspnea and echocardiographic findings for the patients who visited our cardiology departments.
Methods
From October, 2002 to April, 2003, serum NT-pro BNP levels were measured in 348 patients who visited the Samsung Medical Center and the Jong Koo Lee Heart Clinic.
Results
The NT-pro BNP levels were increased with the progression of NYHA Fc of dyspnea (p<0.001 by ANOVA), the increase in the systolic left ventricular internal dimension (p<0.05), and the decrease in the ejection fraction (p<0.01). For the NYHA Fc I patients, the NT-pro BNP levels were positively correlated with age (p<0.001) and left atrial size (p<0.001). For the patients with ischemic heart disease, the NT-pro BNP levels were also positively correlated with the NYHA Fc (p<0.001 by ANOVA). The NT-pro BNP levels were increased with the increase in the systolic (p<0.001) and diastolic pressure (p=0.017), the left ventricular internal dimension as well as the decrease in the ejection fraction (p<0.001). The area under the receiver operating characteristic (ROC) curve for the NT-pro BNP levels was 0.994 (95% confidence interval, 0.979-0.999), and the most reliable cut-off level for the NT-pro BNP was 293.6 pg/mL.
Conclusion
The NT-pro BNP levels were positively correlated with the NYHA Fc of dyspnea and the systolic dysfunction for the patients who visited our cardiology departments. A 300 pg/mL value for the NT-pro BNP cut-off point appears to be a sensitive level to differentiate dyspnea originating from an ailing heart or not for the patients who visited our cardiology departments.
Keywords: Natriuretic peptides, Heart failure, Myocardial ischemia
INTRODUCTION
The N-terminal fragment of pro Brain Natriuretic Peptide (NT-pro BNP) is a neuro-hormone synthesized in the cardiac ventricles in response to increased wall tension. NT-pro BNP levels are positively correlated with the NYHA Fc of dyspnea and the systolic dysfunction, and NT-pro BNP levels are a well-known prognostic factor for the long-term mortality and morbidity of heart failure1-9). Brain natriuretic peptide (BNP) is a neuro-hormone synthesized in the cardiac ventricles, and it is especially increased for patients with systolic dysfunction10). BNP is different from the atrial natriuretic peptide (ANP), which is synthesized in the cardiac atria.
BNP is synthesized by the cardiac myocytes, and it is formed as a pro-hormone that is made of 108 amino-acids. After BNP is secreted from the cardiac myocytes, it is then divided into the physiologically inactive N-terminal fragment (76 amino-acids) and the physiologically active BNP (32 aminoacids)10).
The current tests for the measurement of BNP or NT-pro BNP levels are known be sensitive and specific to differentiate whether or not the dyspnea is the result of an ailing heart. Especially, measurements of NT-pro BNP levels are more reliable and less expensive for diagnosing heart failure and for guiding the physician's decisions on follow-up treatment11-15).
The purpose of this study was to assess the correlation between NT-pro BNP levels and the New York Heart Association function classes (NYHA Fc), and we wished to assess the correlation between the NT-pro BNP levels and the echocardiographic findings of the patients who visited our cardiology departments. We also wished to find the most reliable cut-off level of NT-pro BNP to differentiate whether or not a patient's dyspnea is the result of an ailing heart.
MATERIALS AND METHODS
Subjects
This prospective study was performed from October, 2002 to April, 2003 on 348 patients who visited the Samsung Medical Center and the Jong Koo Lee Heart Clinic. An informed consent was not obtained from each patient. The serum NT-pro BNP levels were measured for all the subjects.
The study's exclusion criteria disallowed those patients having dyspneas of a non-cardiac-origin such as chronic obstructive pulmonary disease, bronchial asthma, pneumonia and anemia.
After reviewing the subjects' past history, current illnesses, physical examination and blood tests, all the subjects are categorized in subgroups: 1) patients with normal cardiovascular testing 2) hypertensive patients 3) patients with arrhythmias 4) patients with acute myocardial infarction 5) patients with old myocardial infarction 6) patients with dilated cardiomyopathy 7) patients with angina pectois and 8) patients with valvular heart disease.
The degree of the dyspnea for each subject at the time of admission was described by the status of their NYHA functional classes (Fcs). The individual patients at the time of admission were using diuretics, calcium channel antagonists, angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, beta blockers and aldosterone receptor antagonists.
Methods
We took blood samples using lithium heparin tubes, and the blood samples were next centrifuged. The blood samples were then stored at minus 70℃ until further analysis. Serum NT-pro BNP levels were measured with an Elecsys pro BNP reagent kit (Roche Diagnostics, USA) and an Elecsys 2010 (Roche Diagnostics, USA)12-14). Echocardiography was performed within 2 days of the blood sampling for the NT-pro BNP; we also measured the systolic and diastolic left ventricular internal dimension, the ejection fraction and the left atrial size.
Statistics
A statistical analysis was performed using SPSS Pc+ 10.0 software. One-way ANOVA testing and the student's t-test were used to compare the mean subgroup values. Chi-square testing was used to compare the categorical variables. Pearson's correlation was used to estimate the correlation between two variables. For the analysis of the receiver operating characteristic (ROC) curve, we used MedCalc version 4.20 (Frank Schoonjans, Belgium). Differences were considered significant when the p values were less than 0.05.
RESULTS
Clinical characteristics
Of the total 348 patients, there were 191 males and 157 females, with the overall mean age being 54.9 years. On the analysis of the underlying diseases, 134 patients were normal on the cardiovascular tests, 45 patients had hypertension, 18 patients had arrhythmias, 30 patients had acute myocardial infarction, 4 patients had old myocardial infarction, 35 patients had dilated cardiomyopathy, 71 patients had angina pectolis and 11 patients had valvular heart diseases.
Correlation between NT-pro BNP levels and NYHA Fc of dyspneas
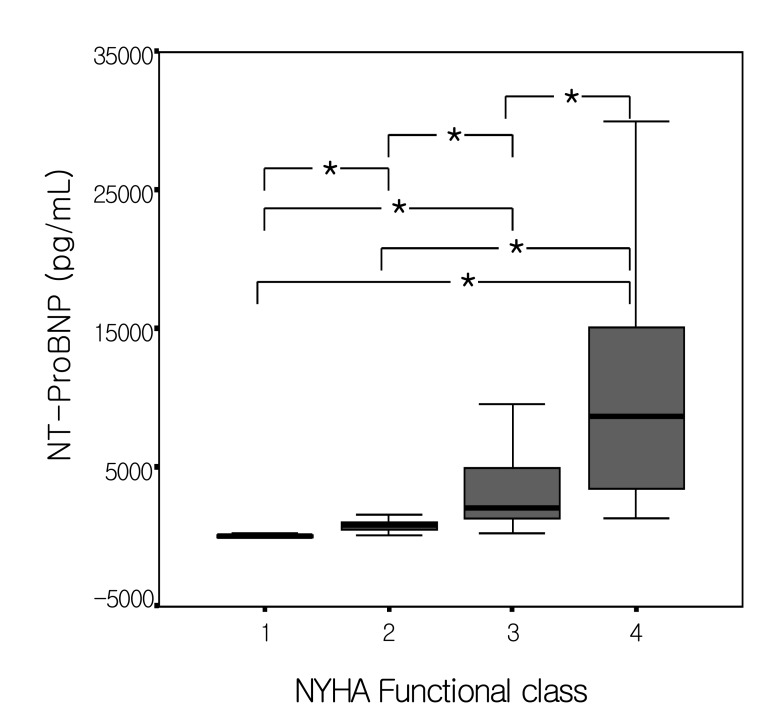
The mean serum level of NT-pro BNP for the 217 patients with NYHA Fc I dyspnea was 87.9±7.59 pg/mL, the mean NT-pro BNP serum level of the 53 patients with NYHA Fc II dyspnea was 992.8±98.58 pg/mL, the mean NT-pro BNP serum level of the 50 patients with NYHA Fc III dyspnea was 2937.9±451.49 pg/mL, and the mean NT-pro BNP serum level of the 28 patients with NYHA Fc IV dyspnea was 12127.8±2291.95 pg/mL. The mean NT-pro BNP serum levels were increased with the progression of the NYHA Fc of dyspnea (p<0.001 by ANOVA)(Figure 1). When comparing the mean NT-pro BNP serum levels for the 217 patients with NYHA Fc I dyspnea and the 131 patients with NYHA Fc II~IV dyspnea, the mean NT-pro BNP serum levels of the patients with NYHA Fc I dyspnea and having no evidence of heart failure was 87.9±7.59 pg/mL: however, the mean NT-pro BNP serum levels of the patients with NYHA Fc II~IV dyspnea and having evidence of heart failure was 4443.3±644.3 pg/mL.
Figure 1.
Correlation between NYHA functional classes (Fc) and the NT-pro BNP levels. NT-pro BNP levels are positively correlated with the NYHA Fc. (*p<0.05, and p<0.001 by ANOVA)
Correlation between NT-pro BNP levels and echocardiographic findings
Of the 348 patients, the NT-pro BNP serum levels were positively correlated with the increase of the systolic left ventricular internal dimension (r=0.238, p=0.011), and the decrease of the ejection fraction (r=-0.333, p<0.001) (Table 1).
Table 1.
Correlation between NT-pro BNP levels and echocardiographic findings. NT-pro BNP levels are positively correlated with systolic left ventricular internal dimension and negatively correlated with ejection fraction.
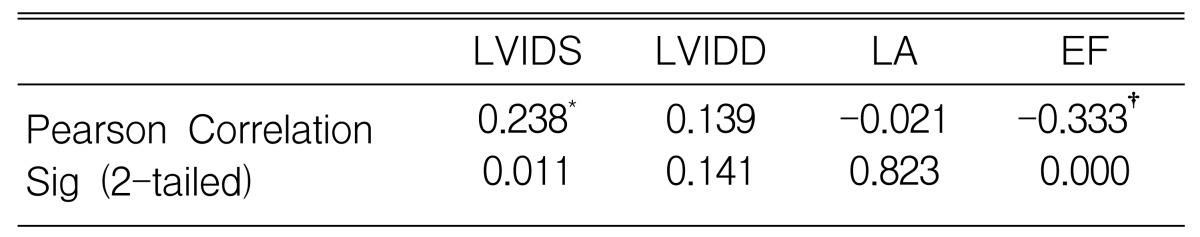
LVIDS, left ventricular systolic internal dimension; LVIDD, left ventricular diastolic internal dimension; LA, left atrium; EF, ejection fraction
*Correlation is significant at the 0.05 level (2-tailed).
†Correlation is significant at the 0.01 level (2-tailed).
In the analysis of correlation between the NT-pro BNP serum levels and echocardiographic findings in the 217 patients with NYHA Fc I dyspnea and having no evidence of heart failure, the NT-pro BNP serum levels were positively correlated with age (r=0.295, p<0.001) and the left atrial size (r=0.263, p<0.001) (Table 2).
Table 2.
Correlation between NT-pro BNP levels and echocardiographic findings and age in patients with NYHA Fc 1 dyspnea. NT-proBNP levels are increased with age and positively correlated with LA size.
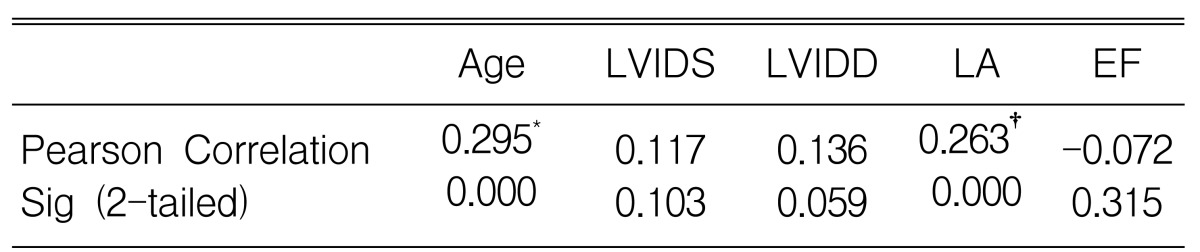
LVIDS, left ventricular systolic internal dimension; LVIDD, left ventricular diastolic internal dimension; LA, left atrium; EF, ejection fraction
*Correlation is significant at the 0.05 level (2-tailed).
†Correlation is significant at the 0.01 level (2-tailed).
Correlation between NT-pro BNP levels and the NYHA Fc of dyspneas in patients with ischemic heart diseases
For the 101 patients having ischemic heart diseases, the mean NT-pro BNP serum levels of the 64 patients with NYHA Fc I dyspnea was 149.4±21.6 pg/mL, the mean NT-pro BNP serum levels of the 23 patients with NYHA Fc II dyspnea was 1121.9±182.7 pg/mL, the mean NT-pro BNP serum levels of the 9 patients with NYHA Fc III dyspnea was 2701.4±586.8 pg/mL, the mean NT-pro BNP serum levels of the 5 patients with NYHA Fc IV dyspnea was 18662.2±763.4 pg/mL. Therefore, the NT-pro BNP serum levels were also positively correlated with the NYHA Fc (p<0.001 by ANOVA). On the analysis of correlation between the NT-pro BNP serum levels and the echocardiographic findings, the NT-pro BNP serum levels were increased with the increase in the systolic (r=0.426, p<0.001) and diastolic pressures (r=0.273, p=0.017), the left ventricular internal dimension as well as the decrease in the ejection fraction (r=-0.482, p<0.001)(Table 3). Therefore, we proposed that NT-Pro BNP serum levels may be an indicator of ventricular function and long-term prognosis for the patients with ischemic heart diseases.
Table 3.
Correlation between the NT-pro BNP levels and echocardiographic findings and age in patients with ischemic heart diseases. NT-pro BNP levels are increased with age and positively correlated with the systolic left ventricular internal dimension and the diastolic left ventricular internal dimension. The NT-pro BNP levels are negatively correlated with the ejection fraction.
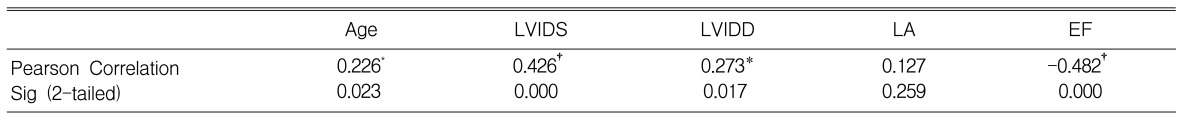
LVIDS, left ventricular systolic internal dimension; LVIDD, left ventricular diastolic internal dimension; LA, left atrium; EF, ejection fraction
*Correlation is significant at the 0.05 level (2-tailed).
†Correlation is significant at the 0.01 level (2-tailed).
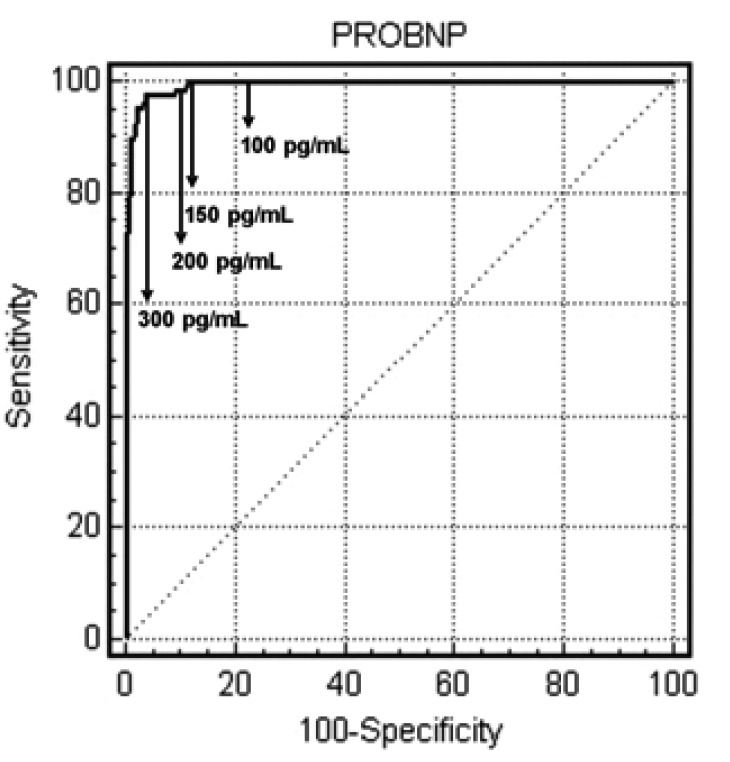
The area under the receiver operating characteristic (ROC) curve for the NT-pro BNP levels.
Of the total 348 patients, 131 patients had NYHA Fc II-IV dyspneas (37.6%). When we analyzed the ROC curve of the NT-pro BNP serum levels in patients with NYHA Fc II-IV dyspneas with the use of 37.6% as the prevalence rate of symptomatic heart failure, the area under the curve was 0.994 (Figure 2).
Figure 2.
The area under the receiver operating characteristic (ROC) curve for the NT-pro BNP levels. The ROC curve for the NT-pro BNP levels was 0.994 (95% confidence interval, 0.979-0.999) and the most reliable cut-off levels of NT-pro BNP to differentiate dyspnea originating from an ailing heart or not is 293.6 pg/mL for patients with heart disease.
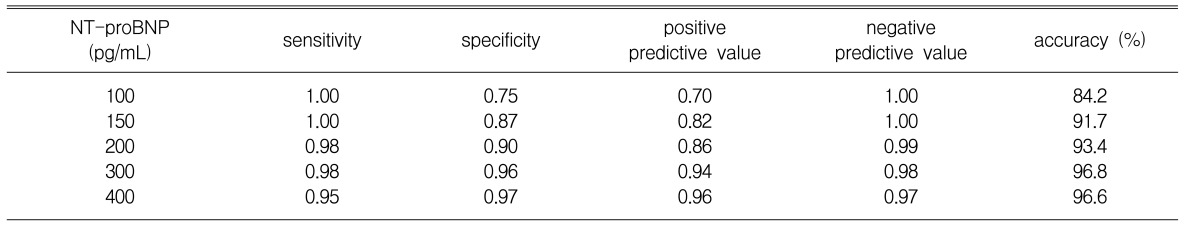
The sensitivity and specificity according to the cut-off level of NT-pro BNP is shown in Table 4, and the most reliable cut-off level of NT-pro BNP is 293.6 pg/mL. Therefore, we propose that a 300 pg/mL of NT-pro BNP is a sensitive level to differentiate if a patient's dyspnea is the result of an ailing heart or not for the patients who visited the cardiology departments in our study.
Table 4.
Comparison of sensitivity, specificity, positive predictive value, negative predictive value and accuracy of the various NT-pro BNP levels.
DISCUSSION
The prevalence rate of the heart failure is increasing and it's mortality is sill high despite many drugs and surgical device have been developed recently. Since a half of the patients with heart failure have no symptoms, furthermore, the symptoms and signs of heart failure are not specific nor sensitive, the diagnosis of heart failure is often difficult2-6).
In the clinical setting, the medical personnel must subjectively differentiate whether a patient who visits the emergency room has dyspnea originating from an ailing heart or not, and the diagnostic accuracy rate for the origins of dyspneas by clinical decisions alone is under 80%7). Recently, serum BNP levels have been shown to be highly sensitive, specific and simple for diagnosing heart failure; therefore, measurements of serum BNP levels are being frequently carried out to diagnose heart failure and to guide the follow-up treatment2-7).
Because the proto-motor region of the BNP gene has a rapid turn-over sequence known as TATTTAT, BNP mRNA has a rapid turn-over rate and it is explosively secreted in proportion to the intraventricular volume or pressure overload16-18).
For patients with ventricular dysfunction, NT-pro BNP is absolutely and relatively more prominently increased than BNP, and NT-pro BNP has been shown to be superior to BNP for diagnosing ventricular dysfunction. Recently, with the use of the more reliable and less expensive radio-immunoassay technique, NT-pro BNP is often used to diagnose, treat and follow-up ventricular dysfunction and heart failure12, 14, 15).
Our study has shown that NT-pro BNP levels were increased with the progression of the NYHA Fc of dyspnea, The results of our study are in excellent agreement with the previous reported studies1-10). The NT-pro BNP serum levels of the patients with NYHA Fc II~IV dyspnea and having evidence of heart failure were more significantly increased than the NT-pro BNP serum levels of the patients of NYHA Fc I dyspnea who don't have any symptoms or they have minimal symptoms of heart failure. This result of our study is in excellent agreement with the previous reported studies2-7).
The BNP or NT-Pro BNP serum levels were increased in patients with systolic dysfunction and also in patients with diastolic dysfunction. The BNP or NT-Pro BNP serum levels of patients with systolic dysfunction and diastolic dysfunction were more significantly increased than the BNP or NT-pro BNP serum levels of patients having only systolic dysfunction or diastolic dysfunction, Moreover, the BNP or NT-Pro BNP serum levels of patients having a past history of heart failure or if they have any symptoms of heart failure and ventricular dysfunction upon echocardiography were more significantly increased than the BNP or NT-pro BNP serum levels of patients having no past history of heart failure or if they had any symptoms of heart failure and ventricular dysfunction upon echocardiography 18-21).
Our study showed that the NT-pro BNP serum levels were positively correlated with the systolic left ventricular internal dimension and negatively correlated with the ejection fraction These results of our study are in excellent agreement with the previous reported studies (Table 1).
For the 217 patients with NYHA Fc I dyspnea, the NTproBNP levels were increased with age and were positively correlated with LA size (Table 2). These results show that the NT-pro BNP serum levels may be correlated with diastolic left ventricular dysfunction, but this correlation was not statistically significant in our study.
For patients with ischemic heart diseases, the NT-pro BNP serum levels were correlated with regional wall motion abnormalities upon echocardiography, and the NT-pro BNP serum levels were significantly decreased for patients with improved regional wall motion abnormalities after their treatment for ischemic heart diseases21-24). For patients with ischemic heart diseases, the increased NT-pro BNP serum levels correlated with increased mortality rates and the increased incidence rates of myocardial infarction and heart failure; therefore, for patients with high NT-pro BNP serum levels, more aggressive and precise treatment is needed. The prognosis for patients with significantly decreased NT-pro BNP serum levels after treatment for ischemic heart diseases is much better than the prognosis for patients with no or minimally decreased NT-pro BNP serum levels after their treatment for ischemic heart diseases; therefore, the NT-pro BNP serum level is an independent prognostic factor for patients with ischemic heart diseases23, 24).
Our study showed that the NT-pro BNP levels were increased with age, and they were positively correlated with the systolic left ventricular internal dimension and diastolic left ventricular internal dimension. The NT-pro BNP levels were negatively correlated with the ejection fraction for the 101 patients having ischemic heart diseases.
The NT-pro BNP levels positively correlated with the diastolic left ventricular internal dimension for the 101 patients having ischemic heart diseases, and the NT-pro BNP levels didn't show any statistical correlation with the diastolic left ventricular internal dimension between the patients with NYHA Fc I dyspnea and all of the other subjects.
However, the NT-pro BNP levels showed statistical tendencies with the diastolic left ventricular internal dimension for the patients with NYHA Fc I dyspnea, yet these different results were probably derived from the small number of subjects in our study, and therefore, further analyses is needed with a larger number of subjects. We also need further analyses on the correlations between the NT-Pro BNP serum levels and the long-term prognosis. In 2002, Hobbs reported that the most reliable cut-off level for the NT-pro BNP to differentiate whether dyspnea was from an ailing heart heart or not in patients was 36 pg/mL.
131 patients had NYHA Fc II-IV dyspneas of the total 348 patients for a prevalence rate 37.7%. When we analyzed the ROC curve of the NT-pro BNP levels for patients with NYHA Fc II-IV dyspneas with the use of 37.6% as the prevalence rate for symptomatic heart failure, the most reliable cut-off level for NT-pro BNP was 300 pg/mL; this cutoff value had a sensitivity of 0.98, a specificity of 0.96, a positive predictive value of 0.94, and a negative predictive value of 0.98. The cut-off level for NT-pro BNP in our study was higher than that of the NT-pro BNP in the previously reported studies in which all the subjects were not confirmed as patients with cardiovascular diseases.
In conclusion, the prevalence rate of dyspnea originating from an ailing heart for the patients who visited or who were admitted to the cardiology departments was higher than that of the general population, Therefore, we might propose that our cut-off point for the NT-pro BNP level to differentiate dyspnea originating from an ailing heart or not in patients who visited or who were admitted to the cardiology departments was much higher than the NT-pro BNP level cut-off point in the previously reported studies in which all the subjects were from the general population.
ACKNOWLEDGEMENT
We would like to thank Roche Diagnostics for their technical supports to measure NT-proBNP for this study.
References
- 1.Mukoyama M, Nakao K, Saito Y, Ogawa Y, Hosoda K, Suga S, Shirakami G, Jougasaki M, Imura H. Increased human brain natriuretic peptide in congestive heart failure. N Engl J Med. 1990;323:757–758. doi: 10.1056/NEJM199009133231114. [DOI] [PubMed] [Google Scholar]
- 2.Davis M, Espiner E, Richards G, Billings J, Town I, Neill A, Drennan C, Richards M, Turner J, Yandle T. Plasma brain natriuretic peptide in assessment of acute dyspnoea. Lancet. 1994;343:440–444. doi: 10.1016/s0140-6736(94)92690-5. [DOI] [PubMed] [Google Scholar]
- 3.Cowie MR, Struthers AD, Wood DA, Coats AJ, Thompson SG, Poole-Wilson PA, Sutton GC. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet. 1997;350:1349–1353. doi: 10.1016/S0140-6736(97)06031-5. [DOI] [PubMed] [Google Scholar]
- 4.Dao Q, Krishnaswamy P, Kazanegra R, Harrison A, Amirnovin R, Lenert L, Clopton P, Alberto J, Hlavin P, Maisel AS. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent-care setting. J Am Coll Cardiol. 2001;37:379–385. doi: 10.1016/s0735-1097(00)01156-6. [DOI] [PubMed] [Google Scholar]
- 5.Lee SC, Stevens TL, Sandberg SM, Heublein DM, Nelson SM, Jougasaki M, Redeld MM, Burnett JC., Jr The potential of brain natriuretic peptide as a biomarker for New York Heart Association class during the outpatient treatment of heart failure. J Card Fail. 2002;8:149–154. doi: 10.1054/jcaf.2002.125368. [DOI] [PubMed] [Google Scholar]
- 6.Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, Omland T, Storrow AB, Abraham WT, Wu AH, Clopton P, Steg PG, Westheim A, Knudsen CW, Perez A, Kazanegra R, Herrmann HC, McCullough PA. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347:161–167. doi: 10.1056/NEJMoa020233. [DOI] [PubMed] [Google Scholar]
- 7.McCullough PA, Nowak RM, McCordJ, Hollander JE, Herrmann HC, Steg PG, Duc P, Westheim A, Omland T, Knudsen CW, Storrow AB, Abraham WT, Lamba S, Wu AH, Perez A, Clopton P, Krishnaswamy P, Kazanegra R, Maisel AS. B-type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from Breathing Not Properly (BNP) Multinational Study. Circulation. 2002;106:416–422. doi: 10.1161/01.cir.0000025242.79963.4c. [DOI] [PubMed] [Google Scholar]
- 8.Morrison LK, Harrison A, Krishnaswamy P, Kazanegra R, Clopton P, Maisel A. Utility of a rapid B-natriuretic peptide assay in differentiating congestive heart failure from lung disease in patients presenting with dyspnea. J Am Coll Cardiol. 2002;39:202–209. doi: 10.1016/s0735-1097(01)01744-2. [DOI] [PubMed] [Google Scholar]
- 9.Tsutamoto T, Wada A, Maeda K, Hisanaga T, Maeda Y, Fukai D, Ohnishi M, Sugimoto Y, Kinoshita M. Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation. 1997;96:509–516. doi: 10.1161/01.cir.96.2.509. [DOI] [PubMed] [Google Scholar]
- 10.Wilkins MR, Redondo J, Brown LA. The natriureticpeptide family. Lancet. 1997;349:1307–1310. doi: 10.1016/S0140-6736(96)07424-7. [DOI] [PubMed] [Google Scholar]
- 11.Davidson NC, Coutie WJ, Struthers AD. N-terminal proatrial natriuretic peptide and brain natriuretic peptide are stable for up to 6 hours in whole blood in vitro. Circulation. 1995;91:1276–1277. [PubMed] [Google Scholar]
- 12.Davidson NC, Naas AA, Hanson JK, Kennedy NS, Coutie WJ, Struthers AD. Comparison of atrial natriuretic peptide B-type natriuretic peptide, and N-terminal proatrial natriuretic peptide as indicators of left ventricular systolic dysfunction. Am J Cardiol. 1996;77:828–831. doi: 10.1016/S0002-9149(97)89176-X. [DOI] [PubMed] [Google Scholar]
- 13.Murdoch DR, Byrne J, Morton JJ, McDonagh TA, Robb SD, Clements S, Ford I, McMurray JJ, Dargie HJ. Brain natriuretic peptide is stable in whole blood and can be measured using a simple rapid assay: implications for clinical practice. Heart. 1997;78:594–597. doi: 10.1136/hrt.78.6.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hammerer-Lercher A, Neubauer E, Muller S, Pachinger O, Puschendorf B, Mair J. Head-to-head comparison of N-terminal pro-brain natriuretic peptide, brain natriuretic peptide and N-terminal pro-atrial natriuretic peptide in diagnosing left ventricular dysfunction. Clin Chim Acta. 2001;310:193–197. doi: 10.1016/s0009-8981(01)00578-2. [DOI] [PubMed] [Google Scholar]
- 15.Hobbs F, Davis R, Roalfe A, Kenkre J, Trawinski J, Davies M. Performance characteristics of N terminal pro brain natriuretic peptide (NT-proBNP) and BNP assays in the diagnosis of symptomatic and asymptomatic left ventricular systolic dysfunction in primary care. J Am Coll Cardiol. 2001;37:I-648A. [Google Scholar]
- 16.Krishnaswamy P, Lubiden E, Clopton P, Koon J, Kazanegra R, Wanner E, Gardetto N, Garcia A, DeMaria A, Maisel AS. Utility of B-natriuretic peptide levels in identifying patients with left ventricular systolic or diastolic dysfunction. Am J Med. 2001;111:274–279. doi: 10.1016/s0002-9343(01)00841-5. [DOI] [PubMed] [Google Scholar]
- 17.Maisel AS, Koon J, Krishnaswamy P, Kazenegra R, Clopton P, Gardetto N, Morrisey R, Garcia A, Chiu A, de Maria A. Utility of B-natriuretic peptide as a rapid, point-of-care test for screening patients undergoing echocardiography to determine left ventricular dysfunction. Am Heart J. 2001;141:367–374. doi: 10.1067/mhj.2001.113215. [DOI] [PubMed] [Google Scholar]
- 18.Lubien E, DeMaria A, Krishnaswamy P, Clopton P, Koon J, Kazanegra R, Gardetto N, Wanner E, Maisel AS. Utility of B-natriuretic peptide in detecting diastolic dysfunction: comparison with Doppler velocity recordings. Circulation. 2002;105:595–601. doi: 10.1161/hc0502.103010. [DOI] [PubMed] [Google Scholar]
- 19.Bay M, Kirk V, Parner J, Hassager C, Nielsen H, Krogsgaard K, Trawinski J, Boesgaard S, Aldershvile J. NT-proBNP: a new diagnostic screening tool to differentiate between patients with normal and reduced left ventricular systolic function. Heart. 2003;89:150–154. doi: 10.1136/heart.89.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hobbs FD, Davis RC, Roalfe AK, Hare R, Davies MK, Kenkre JE. Reliability of N-terminal pro-brain natriuretic peptide assay in diagnosis of heart failure: cohort study in representative and high risk community populations. BMJ. 2002;324:1498. doi: 10.1136/bmj.324.7352.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bonarjee VV, Omland T, Nilsen DW, Caidahl K, Sundsfjord JA, Dickstein K. Plasma proatrial natriuretic factor (1-98) concentration after myocardial infarction: relation to indices of cardiac and renal function. Br Heart J. 1995;73:511–516. doi: 10.1136/hrt.73.6.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Richards AM, Nicholls MG, Yandle TG, Frampton C, Espiner EA, Turner JG, Buttimore RC, Lainchbury JG, Elliott JM, Ikram H, Crozier IG, Smyth DW. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: new neurohormonal predictors of left ventricular function and prognosis after myocardial infarction. Circulation. 1998;97:1921–1929. doi: 10.1161/01.cir.97.19.1921. [DOI] [PubMed] [Google Scholar]
- 23.de Lemos JA, Morrow DA, Bentley JH, Omland T, Sabatine MS, McCabe CH, Hall C, Cannon CP, Braunwald E. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med. 2001;345:1014–1021. doi: 10.1056/NEJMoa011053. [DOI] [PubMed] [Google Scholar]
- 24.Omland T, Aakvaag A, Bonarjee VV, Caidahl K, Lie RT, Nilsen DW, Sundsfjord JA, Dickstein K. Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long term survival after acute myocardial infarction. Circulation. 1996;93:1963–1969. doi: 10.1161/01.cir.93.11.1963. [DOI] [PubMed] [Google Scholar]