Abstract
Background
Although e-coach support increases the effectiveness of Internet weight loss interventions, no studies have assessed influence of type of e-coach support.
Purpose
The effects of nondirective (collaborative, flexible) and directive (prescriptive, protocol driven) e-coach support on weight loss, dietary behavior, physical activity, and engagement were assessed in a 12-week weight loss e-coaching program.
Procedures
Overweight adults (N = 104) were randomly assigned to nondirective, directive, or minimal support. All received weekly lessons and feedback graphs via e-mail. Participants in the nondirective and directive support conditions received individualized nondirective or directive weight loss support.
Results
For females, weight loss (η 2 = 0.10) and changes in waist circumference (η 2 = 0.07) were greater in the directive than in the nondirective and minimal support conditions.
Conclusions
Differences in type of e-coach support are salient to participants. Directive support is beneficial to females in a 12-week e-coach weight loss program.
Introduction
The obesity epidemic—300 million obese adults worldwide [1]—drives the search for innovative methods of prevention and treatment that are effective, have wide reach, and go beyond the traditional in-person encounter. Numerous studies have shown that Internet interventions can produce meaningful increases in physical activity, changes in dietary behavior, and weight loss [2–8]. However, as with in-person interventions, not all Internet interventions produce equivalent results. Certain features have been found to improve outcomes. One feature that has consistently been found to improve outcomes is Internet support via an e-coach. When e-coach support is added to an educational website, it doubles the amount of weight loss [5, 9]. Although studies have illustrated that Internet interventions containing e-coach support can produce clinically significant weight losses, no studies have evaluated the effects of different types of e-coach support on weight loss. Therefore, studies are needed to better understand how internet coaches can provide support most efficiently and effectively to promote behavior change.
Within the broader social support literature, a distinction has been made between directive and nondirective support [10]. Directive support is prescriptive and guided by rules. The support provider takes over responsibility and tells the support recipient what to do. In contrast, nondirective support involves cooperation and accepting the support recipient’s thoughts and choices. When nondirective support is provided, the recipient retains responsibility for tasks and decisions about goals.
Several studies of in-person support have found that nondirective support is positively associated with successful disease management, healthy lifestyles, and support satisfaction [10–12]. In contrast, directive support is either unrelated or, often, negatively associated with these outcomes [11, 13, 14]. However, directive support can be advantageous in acute, stressful situations or when an individual lacks necessary skills or experience with a particular task or challenge. As with the rarity of experimental studies of different types of support, no studies have manipulated and compared nondirective and directive support in an intervention.
The current study compared directive and nondirective support in a 12-week weight-loss e-coaching program. The goal was to examine how different types of e-coach support influence weight loss, behavior change, and engagement in the intervention. Participants in an Internet-based weight-loss intervention were randomly assigned to one of three experimental conditions: a minimal e-coach support condition, a nondirective e-coach support condition, or a directive e-coach support condition. Primary outcomes included change in weight and waist circumference from baseline to 12 weeks. Secondary outcomes included change in physical activity, dietary behavior, and program engagement with the intervention. We hypothesized that participants in the nondirective and directive support conditions would have greater weight loss, improvements in dietary behavior and physical activity, and engagement than participants in the minimal support condition. In addition, due to the previously cited studies showing benefits of nondirective support for successful disease management, healthy lifestyles, and support satisfaction, we expected that participants in the nondirective support condition would show greater changes in these outcomes relative to participants in the directive support condition.
Methods
This randomized controlled trial contained three arms: minimal e-coach support, nondirective e-coach support, and directive e-coach support. Participants completed in-person assessments at baseline and at the end of the 12-week intervention. Participants also completed an on-line survey at 4 and 8 weeks. The study was implemented within the University of North Carolina Gillings Global School of Public Health, and procedures were approved by the University of North Carolina at Chapel Hill Institutional Review Board for Human Subjects. Written informed consent was obtained from all participants. The study was a single blind trial with participants blind to their treatment condition. Participants received $10 for completing the follow-up assessment.
Recruitment and Participants
Participants were recruited through an informational listserv e-mail announcement sent to employees of the University of North Carolina at Chapel Hill. Participants were informed that the purpose of the study was to assess the effects of different types and intensities of weight loss support delivered by e-mail on weight loss. Recruitment occurred over two periods of 3 to 4 weeks, one commencing in August 2006 and one commencing in January 2007. Interested participants completed a phone screen. Inclusion criteria were overweight [body mass index (BMI) 25–40 kg/m2], between 30 and 60 years old, and access to e-mail. Exclusion criteria were BMI >40 kg/m2; history of myocardial infarction, stroke, or cancer in the previous 5 years; joint problems that would make it difficult to exercise; pregnancy; psychiatric hospitalization in the previous year; weight loss of greater than 10 lb in the previous 6 months; use of weight loss medication in the previous 6 months; current use of medication in which substantial weight gain is a potential side effect; and inability to read and write English fluently.
Assessments and Randomization
Participants attended an in-person baseline assessment, completed on-line assessments at 4 and 8 weeks, and attended an in-person 12-week follow-up assessment. During the in-person assessments, weight, height (baseline only), waist circumference, and hip circumference were measured. A battery of written measures assessing demographic information, physical activity, and dietary behavior was then administered. The 12-week follow-up assessment also included a measure assessing perceptions of received e-coach support.
An on-line survey was administered at 4 and 8 weeks. As a check on the support manipulation, participants in the nondirective and directive support condition completed a questionnaire that assessed perceptions of support received from the e-coach. Upon completion of the baseline assessment, participants were randomly assigned by the principal investigator to a treatment condition by drawing a number. Given the distributed recruitment in two waves (August, 2006 and January, 2007) and to avoid confounding with season, randomization occurred so that for every nine participants enrolled in the study, three were randomized to each condition. Participants were blinded to their treatment condition, and no specific information was provided on the different types of support being assessed.
Weight Loss Intervention
Common Intervention Components
Table 1 shows a comparison of intervention components across conditions. Basic intervention components common to all three conditions were as follows: At the baseline assessment, all participants were given the CalorieKing Calorie, Fat, and Carbohydrate Counter book [15], which provided nutritional information on an extensive list of foods; a chart providing the energy expenditure of common physical activities; and 12 self-monitoring booklets, through each of which participants were instructed to record caloric intake, fat intake, exercise energy expenditure, and weight for a 7-day period.
Table 1.
Comparison of intervention features across conditions
| Intervention feature |
Minimal support condition |
Directive support condition | Nondirective support condition |
|---|---|---|---|
| Order of lessons | Protocol based | Protocol based | Tailored by participant |
| Goal Setting | N/A | Goals set by e-coach | Goals selected by participant |
| Topics of discussion |
N/A | Chosen by e-coach | Open to participant choice |
| When no contact |
N/A | Lack of communication pointed out. Participant told to complete weekly check in survey and is asked about goals from previous week |
Lack of communication pointed out. Participant told that e-coach is there if needed |
All participants, including those in the minimal treatment condition, received an Internet-based weight loss program with information and feedback delivered via e-mail. Each week for 12 weeks the e-coach sent participants two e-mails, a lesson e-mail and a feedback e-mail (see electronic supplementary material, Appendix A, for sample e-mails for each condition).
The 12 weight loss lessons delivered to all participants in this intervention were based on behavioral weight loss lessons used in the lifestyle intervention component of the Diabetes Prevention Program [16]. Previous Internet weight loss trials have successfully used lessons based on this program to assist individuals in losing weight (e.g., [17]). In the current study, these lessons provided all participants with information on basic behavioral weight loss principals including energy balance, goal setting, self-monitoring, making healthy food choices, reducing calories and fat, improving diet quality, eating in social situations, increasing physical activity, stimulus control, problem solving, cognitive restructuring, stress management, and relapse prevention. Each lesson contained a short quiz. Participants were instructed to send quiz answers to the e-coach.
The weekly lesson e-mail included a greeting using the participant’s first name, a brief description of the lesson, an Internet link to the on-line weekly check-in page, a positive closing statement (e.g., “Have a great week!”), and the e-coaches name. The lesson for that week was attached to the e-mail. The weekly check-in page was a web-based survey that allowed participants to report to the e-coach information from their self-monitoring booklet including weight; daily caloric intake; exercise duration, mode, and energy expenditure; number of times they ate out; grade for recording accuracy (A to F); and comments about the week. This information was obtained from the weekly self-monitoring books and based on protocols used in other Internet weight loss studies [5]. The e-coach used this information in providing feedback and support in the second e-mail.
A weekly feedback e-mail was sent 3 to 4 days after the lesson e-mail and contained feedback graphs and quiz answers. As with the weekly lesson e-mail, the weekly feedback e-mail was personalized and included a greeting using the participant’s first name. The graphs, based on the information the participant provided in the weekly check-in page, were also personalized and showed weekly trends in weight, average daily caloric intake, and total exercise energy expenditure. All participants were informed that the expected rate of weight loss for this type of behavioral weight loss program was 1 to 2 lb a week. The first author served as the e-coach in all conditions.
Minimal E-Coach Support
Participants received only the weekly lesson e-mail, sent in a standardized order, and the weekly feedback e-mail. No individualized support was provided. The feedback e-mail contained only feedback graphs and quiz answers.
Directive E-Coach Support
In keeping with the directive–nondirective distinction described in the “Introduction”, the directive version of e-coach support was structured to provide concrete, specific advice based on state-of-the-art knowledge of weight loss. Participant choice was not emphasized in favor of clearly recommending the best advice possible. Participants received weekly lesson e-mails in a standardized order. In the feedback e-mail, the e-coach reviewed the participant’s self-reported weight to determine whether the participant was losing weight at a rate of 1 to 2 lb a week and whether the participant was engaging in behaviors that would result in further weight loss and successful weight maintenance. Specific caloric intake and exercise goals were prescribed for the participant. Weekly short-term goals were established to help participants increase exercise so they were eventually expending 2,500 kcal a week through exercise. In addition, if the participant or e-coach identified other problems or barriers, the e-coach developed a plan for the participant to overcome this problem and, reflecting directive support, provided specific suggestions for handling it. If the participant did not communicate with the e-coach, the e-coach pointed out this lack of communication, asked the participant to check in, listed the previous week’s goals, and asked how the participant did on these goals.
Nondirective E-Coach Support
Again in keeping with the directive–nondirective distinction, the nondirective version of e-coach support was structured to heighten participant choice such as in the order of lessons, encouraging the participant to identify objectives and goals, and, whenever possible, in presenting several alternatives for addressing obstacles rather than one specific recommendation. All e-coach suggestions were based on the state-of-the-art knowledge of weight loss, but participants were allowed to decide what goals to set and what strategies they wanted to follow.
In their first e-mail, participants received a list of lessons in the standardized order and were told they could alter the order at any time. The e-coach encouraged the participant to set weekly goals related to physical activity, caloric intake, and weight loss. However, the participant was ultimately responsible for deciding on which, if any, goals to focus. If the participant was having difficulty setting appropriate weight loss goals, the e-coach suggested three to four potential goals. In the weekly feedback e-mail, the e-coach would check in with the participant to see if the participant’s weight loss needs were being met, if there was any assistance the e-coach could provide to help the participant, or if there were any questions. The e-coach was flexible with discussion topics and discussed any issues brought forth by the participant. The e-coach provided feedback on the participant’s behaviors and whether the goals the participant set were reached. If the participant did not communicate with the e-coach, the e-coach pointed out the lack of communication and let the participant know that she was available if any assistance was desired.
It is important that the nondirective condition not be construed as laissez-faire. Although highly flexible and responsive to the participant’s choices, the nondirective support was nevertheless persistent in maintaining contact with participants and promoting core weight loss messages of weight loss of 1 to 2 lb per week, decreasing caloric intake, and increasing energy expenditure; however, participants were encouraged to select their own goals and make their own decisions about what they should focus on during the ensuing week. This is consistent with other forms of treatment, such as motivational enhancement techniques, that support autonomy.
Measures
Anthropomorphic Measurements
A Tanita WB-300 digital scale with height rod was used to assess weight and height. Waist circumference was measured at the point below the rib cage and above the umbilicus which appeared to have the smallest circumference [18]. Hip circumference was measured at the point in the buttocks–hip area that had the largest circumference [18]. Measurements were taken until two identical measurements were obtained or three measurements were obtained that were within 0.5 cm.
Fat and Fiber Behavior
The Kristal Fat and Fiber Behavior Scale [19] was used to assess low-fat eating and high-fiber intake. This scale contains 29 items: Four items assess both fat-related and fiber-related dietary behavior, 17 items assess only fat-related dietary behavior, and eight assess only fiber-related dietary behavior. Participants indicate how frequently they perform each behavior using a four-point scale ranging from 1, usually or always, to 4, rarely or never. Items for each type of behavior are summed to produce a fat-related dietary behavior score and a fiber-related dietary behavior score. The validity of the Fat and Fiber Behavior Scale has been documented by its significant correlations with related measures such as a telephone administered Food Frequency Questionnaire based on the Food Frequency Questionnaire [19].
Physical Activity
The International Physical Activity Questionnaire Long Form was used to assess leisure time physical activity [20]. This 27-item survey assesses time spent in specific types of activities over the previous 7 days. Reliability and validity were established in a large validation study in 14 centers from 12 countries [20].
Engagement
As part of each intervention, participants completed on-line weekly check-in pages about food intake, exercise, and progress at the end of each of the first 11 weeks of intervention. Two indices of engagement in the intervention (range 0 to 11) were created from these by tabulating the number of weeks that participants reported their caloric intake on five or more days and the number of weekly check-in pages submitted. A third index for only the nondirective and directive support conditions was the number out of the 12 weeks that participants communicated with the e-coach via e-mail.
Perceived Receipt of Nondirective and Directive Support
Perceptions of e-coach support received were assessed with the Social Support Inventory which has been used in previous studies [10, 12]. The current study utilized a 16-item version of this measure (see electronic supplemental materials, Appendix B) which included questions about eight nondirective (i.e., “Cooperated with you to get things done” and “Made it easy to talk about anything you thought was important”) and eight directive support behaviors (i.e., “Solved problems for you” and “Pushed you to get going on things”). Items are rated on a five-point scale ranging from 1 (not at all typical) to 5 (very typical). Responses to items for each type of support are averaged to provide a nondirective and directive support score. At the 4-, 8-, and 12-week assessments, participants in the nondirective and directive conditions completed this with reference to support received from the e-coach. Internal consistency reliabilities were 0.88, 0.89, and 0.92 for the nondirective support scale at 4, 8, and 12 weeks, respectively, and 0.88, 0.89, and 0.80 for the directive support scale.
Statistical Analyses
All analyses controlled for age, education (college degree or no college degree), and ethnicity (Caucasian or non-Caucasian). First, analyses of covariance (ANCOVAs) with weight change as a dependent variable, treatment condition and gender as fixed factors, and baseline weight as an additional covariate assessed whether groups differed in weight loss and whether there was an interaction between gender and treatment condition on weight loss. Similar ANCOVAs, but with change in waist circumference as a dependent variable, treatment condition as a fixed factor, and baseline waist circumference as an additional covariate, assessed whether groups differed in changes in waist circumference. Chi-square analyses then assessed whether there were between-group differences in the percent of participants who achieved a 5% weight loss. Repeated measures ANCOVA of nondirective and directive support scales from the Social Support Inventory assessed the experimental manipulation of nondirective and directive support. In this analysis, the Social Support Inventory support scale (reported nondirective or directive support subscale) and time (4, 8, and 12 weeks) were entered as within-subject variables, and support condition (nondirective or directive support condition) was entered as a between-subjects variable. Due to the physical activity data being skewed and kurtotic, a nonparametric rank order analysis assessed between-group differences in physical activity [21]. A repeated measures ANCOVA of the Kristal Fat and Fiber Behavior Scale assessed whether groups differed in fat- and fiber-related dietary behavior. Type of dietary behavior (fat-related and fiber-related subscales) and time (baseline and 12-week follow-up) were entered as within-subject factors, and support condition (minimal, nondirective, or directive) was entered as a between-subjects factor. Finally, ANCOVAs with engagement scores as a dependent variable and treatment group as a fixed factor assessed whether groups differed on engagement.
Results
Recruitment and Attrition
One hundred and four participants enrolled in this study. Figure 1 shows a flow chart of participant attrition. Twelve-week follow-up data, which included objective weights, were missing from eight participants (7.69%). There were no differences in rates of completion by study condition: minimal n = 31 (91.2%), nondirective n = 33 (94.3%), and directive n = 32 (91.4%; χ 2 (2, N = 104) = 0.29, p = 0.86). Regarding on-line surveys, 92 (88.5%) completed the 4-week survey: minimal n = 32 (94.1%), nondirective n = 31 (88.6%), and directive n = 29 (82.9%). Ninety-three (89.4%) completed the 8-week survey: minimal n = 30 (88.2%), nondirective n = 32 (91.4%), and directive n = 31 (88.6%). There were no differences in rates of on-line survey completion across treatment condition (4-week χ 2 (2, N = 104) = 2.14, p = 0.34; 8-week χ 2 (2, N = 104) = 0.23, p = 0.89). One adverse event was reported that was unrelated to the intervention.
Fig. 1.
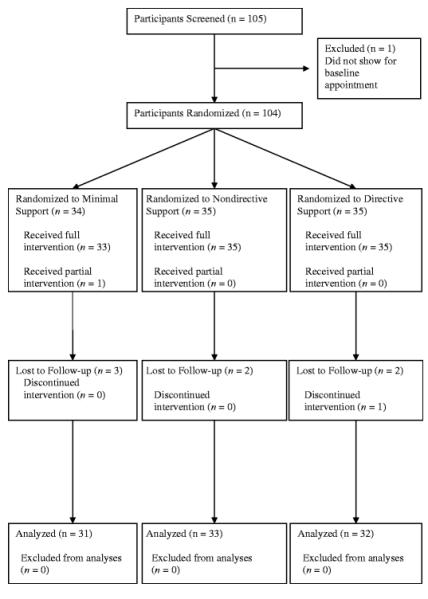
Flow chart of participant attrition
Participant Characteristics
Participants were between the ages of 30 and 59 (M = 45.40, SD = 8.68) and highly educated (68.3% college degree). A majority of participants were female (n = 87, 83.7%) and non-Hispanic White (n = 74; 71.2%). The mean baseline BMI of participants was 32.07 (SD = 4.33). Table 2 shows participant demographic attributes by treatment condition. ANOVAs assessed whether treatment groups differed significantly on age, weight, and BMI; chi-square analyses assessed whether treatment groups differed significantly on ethnicity, marital status, and education. No significant differences were found.
Table 2.
Means, standard deviations, and frequencies of participant characteristics by condition
| Minimal (n = 34) | Nondirective (n = 35) | Directive (n = 35) | Test of significant differences (p) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | n | % | M | SD | n | % | M | SD | n | % | ||
| Age (years) | 46.76 | 9.58 | 42.91 | 7.52 | 46.57 | 8.53 | 0.11 | ||||||
| Weight (kg) | 87.27 | 12.52 | 90.88 | 15.14 | 85.67 | 13.33 | 0.27 | ||||||
| BMI | 32.04 | 3.81 | 32.60 | 4.58 | 31.56 | 4.61 | 0.61 | ||||||
| Gender | 0.77 | ||||||||||||
| Women | 29 | 85.30 | 28 | 80.00 | 30 | 85.70 | |||||||
| Men | 5 | 14.70 | 7 | 20.00 | 5 | 14.30 | |||||||
| Ethnicity | 0.20 | ||||||||||||
| Caucasian | 26 | 76.47 | 27 | 77.14 | 21 | 60.00 | |||||||
| Non-Caucasian | 8 | 23.53 | 8 | 22.86 | 14 | 40.00 | |||||||
| Education | 0.70 | ||||||||||||
| Grade 12 or GED | 0 | 0.00 | 1 | 2.86 | 1 | 2.86 | |||||||
| College 1 to 3 years | 8 | 23.53 | 11 | 31.43 | 12 | 34.29 | |||||||
| College ≥4 years | 26 | 76.47 | 23 | 65.71 | 22 | 62.86 | |||||||
| Marital status | 0.80 | ||||||||||||
| Married/partnered | 24 | 70.59 | 23 | 65.71 | 24 | 68.57 | |||||||
| Divorced | 6 | 17.65 | 6 | 17.14 | 6 | 17.14 | |||||||
| Widowed | 1 | 2.94 | 0 | 0.00 | 0 | 0.00 | |||||||
| Never married | 3 | 8.82 | 6 | 17.14 | 5 | 14.29 | |||||||
Efficacy of Treatments on Weight Loss
Across conditions, participants in the study lost an average of 3.87 kg (SD = 4.08). Average percentage of weight lost was 4.41% (SD = 4.46). Of the 96 individuals who completed the follow-up assessment, 39.6% (n = 38) achieved a 5% weight loss. Assuming no weight loss among the eight participants not completing follow-up assessments, 36.5% of randomized participants achieved a 5% weight loss. There was no difference in weight loss based on recruitment period (fall 2006 or spring 2007, p = 0.27).
Table 3 shows the mean weight loss and percent weight loss by treatment condition. ANCOVAs, with weight change as the dependent variable and support condition and gender as fixed factors, assessed whether there was an interaction between treatment condition and gender on weight change. The interaction between gender and treatment was significant in both the intent-to-treat analysis with missing follow-up weights imputed as zero (F(2, 94) = 3.03, p = 0.05, η 2 = 0.06, observed power = 0.57) and in the completer’s analysis (F(2, 86) = 4.30, p = 0.02, η 2 = 0.09, observed power = 0.74). Males had a greater reduction in weight than females (−6.87 kg, SD = 5.80 vs. −3.36 kg, SD = 3.50, respectively). Males lost 6.67 (SD = 5.32), 9.20 (SD = 5.98), and 4.19 (SD = 6.44) kg in the minimal support, nondirective, and directive conditions, respectively. However, the small number of males provided insufficient power to adequately assess between-group differences.
Table 3.
Means and standard deviations of change in weight, percent weight loss, and waist circumference for all randomized participants and completers by condition and gender
| Treatment group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Minimal | Nondirective | Directive | ||||||||
| Range | M | SD | Range | M | SD | Range | M | SD | ||
| All randomized participants | ||||||||||
| Weight change (kg) | Female | −9.68 to 2.18 |
−2.44 | 3.04 | −11.32 to 3.86 |
−2.50 | 3.36 | −15.23 to 0.84 |
−4.50 | 3.73 |
| Male | −11.77 to 0.91 |
−6.67 | 5.32 | −18.32 to 0.00 |
−6.57 | 6.63 | −12.95 to 2.05 |
−3.35 | 5.88 | |
| Percent weight loss | Female | −11.73 to 3.51 |
−2.97 | −3.82 | −12.88 to 3.75 |
−2.94 | 3.96 | −14.19 to 1.10 |
−5.25 | 3.98 |
| Male | −11.17 to 1.03 |
−6.80 | 5.23 | −19.03 to 0.00 |
6.65 | 7.09 | −12.20 to 2.12 |
−3.43 | 5.75 | |
| Waist circumference change (cm) |
Female | −12.00 to 6.75 |
−2.45 | 4.59 | −25.00 to 4.50 |
−2.65 | 5.77 | −16.75 to 4.00 |
−4.80 | 5.14 |
| Male | −9.50 to −3.50 |
−6.50 | 2.21 | −16.55 to 0.00 |
−6.29 | 6.19 | −11.00 to 0.00 |
−4.70 | 4.49 | |
| Completers | ||||||||||
| Weight change (kg) | Female | −9.68 to 2.18 |
−2.72 | 3.09 | −11.32 to 3.86 |
−2.50 | 3.36 | −15.23 to 0.84 |
−4.82 | 3.65 |
| Male | −11.77 to 0.91 |
−6.67 | 5.32 | −18.32 to −2.50 |
−9.20 | 5.98 | −12.95 to 2.05 |
−4.19 | 6.44 | |
| Percent weight loss | Female | −11.73 to 3.51 |
−3.31 | 3.89 | −12.88 to 3.75 |
−2.94 | 3.96 | −14.19 to 1.10 |
−5.62 | 3.85 |
| Male | −11.17 to 1.03 |
−6.80 | 5.23 | −19.03 to −2.68 |
−9.32 | 6.66 | −12.20 to 2.12 |
−4.28 | 6.26 | |
| Waist circumference change (cm) |
Female | −12.00 to 6.75 |
−2.73 | 4.77 | −25.00 to 4.50 |
−2.65 | 5.77 | −16.75 to 4.00 |
−5.14 | 5.15 |
| Male | −9.50 to −3.50 |
−6.50 | 2.21 | −16.55 to −2.00 |
−8.81 | 5.46 | −11.00 to −1.00 |
−5.88 | 4.21 | |
All further analyses were conducted using only female participants. An intent-to-treat ANCOVA found a significant effect for treatment condition on weight change (F(2, 80) = 4.65, p = 0.01, η 2 = 0.10, observed power = 0.77). Table 4 shows adjusted means and between-group comparisons for this analysis. Post hoc analyses indicated that females in the directive support condition had a greater reduction in weight (M = −4.50 kg) than females in the minimal support (M = −2.44 kg) and nondirective support conditions (M = −2.50 kg). Across conditions, Caucasian females lost more weight than non-Caucasian females, −3.41 vs. −2.63 kg, respectively (F(2, 80) = 4.33, p = 0.04, η 2 = 0.05). An analysis using only completers revealed a similar treatment effect (F(2, 75) = 5.33, p < 0.01, η 2 = 0.13, observed power = 0.83). Females in the directive support condition lost more weight (M = −4.82 kg) than those in the minimal support (M = −2.72 kg) and nondirective support conditions (M = −2.50 kg). No significant differences were found between the minimal and nondirective support conditions.
Table 4.
Adjusted means and between-group comparisons for changes in weight for females
| Mean (SE) | Mean difference (SE) | 95% CI | p | |
|---|---|---|---|---|
| Group | ||||
| Minimal | −2.47 (.64) | −3.74 to −1.20 | ||
| Nondirective | −2.19 (.67) | −3.51 to −0.86 | ||
| Directive | −4.76 (.63) | −6.02 to −3.50 | ||
| Between-group comparisons | ||||
| Comparison | ||||
| Minimal vs. nondirective | −0.28 (0.94) | −2.14 to 1.58 | 0.77 | |
| Minimal vs. directive | 2.30 (0.90) | 0.50 to 4.10 | 0.01 | |
| Nondirective vs. directive | 2.58 (0.95) | 0.69 to 4.46 | 0.00 | |
Means adjusted based on baseline weight, age, ethnicity, and education. Means for participants who did not complete the follow-up assessment were imputed as 0
An ANCOVA was conducted to assess between-group differences in waist circumference. An intent-to-treat analysis using all randomized females with change in waist circumference for the five females who did not complete the follow-up assessment imputed as 0 found a significant group effect (F(2, 80) = 3.22, p = 0.045, η 2 = 0.07). Group differences were identical to those found for weight loss. The directive support condition had significantly greater changes in waist circumference (M = −4.80 cm) than the nondirective (M = −2.65 cm) and minimal (M = 2.45 cm) support conditions. In addition, Caucasian females had greater changes in waist circumference than non-Caucasian females, −3.83 vs. −2.19 cm (F(1, 80) = 4.16). Similar findings emerged in an analysis using only females who completed the follow-up assessment.
Clinically Significant Weight Loss
Clinically significant weight loss was defined as a weight loss of 5% or greater of baseline body weight. A 5% to 10% weight loss is associated with improvements in blood pressure, glycemic control, lipoprotein profiles, and mobility [22–24]. The lower endpoint of this range was selected as a criterion because it was more appropriate for a 12-week intervention.
An intent-to-treat chi-square analysis, with a 0% weight loss imputed for the five females who did not complete follow-up, found between-group differences in the frequency of clinically significant weight loss (χ 2 (2, N = 87) = 6.84, p = 0.03). More females in the directive support condition had a 5% weight loss than in the nondirective support condition, 50.00% vs. 17.86% (χ 2 (1, N = 58) = 6.62, p = 0.01). No differences were found between the directive and minimal support conditions (50.00% vs. 31.03%, χ 2 (1, N = 59) = 2.20, p = 0.14) or between the nondirective and minimal support conditions (χ 2 (1, N = 57) = 1.34, p = 0.25) in the number of females who had a clinically significant weight loss. Similar between-group differences were found in an analysis using only completers (χ 2 (2, N = 82) = 7.82, p = 0.02). More females in the directive support condition achieved a 5% weight loss (53.57%) than in the nondirective condition (17.86%; χ 2 (1, N = 56) = 7.78, p < 0.01). No significant differences were found between the directive support and minimal support conditions (34.60%) or between the nondirective support and minimal support conditions.
Check on Experimental Manipulation of Social Support
Participants in the nondirective conditions were given the option of changing their lesson order. Twelve participants (38.7%) chose to do this.
Analyses examined whether the experimental manipulation of nondirective and directive support was salient to females. These analyses used participants’ responses to the nondirective and the directive support subscales from the Social Support Inventory, completed with reference to their own perception of the support they received from their e-coach. That is, females in the nondirective condition rated the extent to which their e-coach provided support that was directive and nondirective and females in the directive condition similarly rated their e-coach support on both directive and nondirective dimensions. It was expected that levels of perceived support would match condition, i.e., higher nondirective in nondirective condition and higher directive in the directive condition. This was confirmed in a repeated measures ANCOVA in which the nondirective and the directive support subscales from the Social Support Inventory and time (4, 8, and 12 weeks) were entered as within-subject variables, and support treatment conditions—nondirective support condition or directive condition—were entered as a between-subjects variable.
A significant interaction between the Social Support Inventory and support treatment condition was found (F(1, 40) = 23.08, p < 0.01), indicating the two conditions differed in the pattern of nondirective vs. directive support reported. Females in the nondirective condition reported experiencing more nondirective support and a greater ratio of nondirective to directive support than females in the directive condition. Additional analyses utilized several approaches to impute missing data and found the same significant interaction.
Physical Activity
The distributions of leisure time physical activity (metabolic equivalent of task—minutes) scores were significantly skewed and kurtotic so a nonparametric rank order approach was used [21, 25]. A significant group-by-time interaction was found (L(2) = 7.20, p < 0.05), indicating that groups differed in their change in leisure time physical activity from baseline to follow-up. Post hoc analyses indicated that females in the directive support condition had greater changes in physical activity than females in the minimal support condition (L(1) = 7.02, p < 0.01). No other between-group differences were found.
Fat- and Fiber-Related Diet Behavior
Repeated measures ANCOVA found no significant time-by-group or time-by-group-by-type of behavior interactions for dietary behavior.
Engagement
Separate ANCOVAs were conducted for each measure of engagement. For weekly check-in pages, that is the number of times the participant submitted information via the on-line check-in page to the e-coach about weight, caloric intake, or physical activity, the effect of treatment group was significant (F(2, 81) = 3.28, p = 0.04). Post hoc analyses indicated that the directive support condition completed significantly more weekly check-in pages (M = 8.87, SD = 2.80) than the minimal support condition (M = 7.07, SD = 4.20) and the nondirective support condition (M = 7.11, SD = 3.54). No significant differences were found among the three conditions for number of weeks the participant reported their total daily caloric intake for at least 5 days (nondirective support condition, M = 7.90, SD = 3.66; directive support condition, M = 6.11, SD = 3.95; minimal support condition, M = 6.55, SD = 4.21). In addition, no significant differences were found between the nondirective (M = 7.39, SD = 3.15) and directive (M = 6.97, SD = 2.47) support conditions on the number of weeks females contacted the e-coach via e-mail.
Discussion
The results of this study show an orderly sequence of differential effects of type of support delivered by an e-coach. First, a gender-by-treatment interaction was found for weight change. However, the small number of males per condition (minimal = 5, nondirective = 7, directive = 5) made interpretation of this interaction difficult. Subsequent analyses in females showed that differences in e-coach support (a) were salient to females, (b) led to differences in physical activity, and (c) led to differences in amount of weight lost, changes in waist circumference, and numbers losing clinically significant amounts of weight. Reports of e-coach support received mirrored the experimental manipulation of nondirective and directive support. Females in the directive support condition reported greater increases in physical activity than the minimal support condition as well as lost more weight and had greater changes in waist circumference than females in the nondirective and minimal support conditions.
Results indicating that directive e-coach support is associated with more significant weight loss for females than nondirective support may be surprising given previous findings from cross-sectional studies suggesting advantages of nondirective support for disease management and quality of life [10, 11]. There are several potential explanations for this. From the perspective of the stages of change component of Prochaska’s transtheoretical model [26, 27], it should be noted that participants in this study volunteered for an e-mail intervention to begin losing weight. Though not measured specifically, volunteering to begin a weight loss program places participants in either the preparation or action stage of readiness to lose weight. As such, they may have been ready for a directive intervention that would give them clear, specific, and concrete advice regarding steps to take for weight loss. This raises the possibility that different types of e-coach support may be more or less appropriate at different stages of change with perhaps nondirective support more appropriate for those in precontemplation, contemplation, or maintenance.
Related to the readiness to change of participants, directive support may be most beneficial at some phases of behavior change and nondirective support more beneficial at others. In the current study, support was provided in the first 12 weeks of a weight loss program. During this time, participants are learning skills to lose weight. Previous studies have shown that individuals prefer directive support when they feel they lack skills to overcome a stressor or challenge. Nondirective support may be more effective at subsequent phases when individuals have acquired necessary skills but then need encouragement and help in applying them to maintain their progress. Future studies should assess the effects of different types of social support on health behavior at different points in the behavior change process as well as whether skill level moderates the effect of support type on health behavior.
A third reason directive support may have been most effective is that the present weight loss intervention had multiple targets of behavior change (e.g., amount of food consumed, types of food consumed, physical activity). With potential for confusions amidst multiple targets, directive support may be more effective by virtue of simplifying objectives for participants. This value of directive support may be heightened among those who are sufficiently motivated to enroll in an e-mail intervention but perhaps confused by conflicting information about weight loss in the popular media.
Fourth, the medium of e-mail may have influenced the effectiveness of nondirective support. The asynchronous nature of e-mail results in a time lag between responses that could disrupt the potency of nondirective support, which involves a certain amount of collaboration and give and take as provider and recipient agree upon a plan. In contrast, the lack of real-time dialogue would seem to present no obstacle to the delivery and receipt of direct advice. In fact, the ability of the recipient to control when an e-mail is read may reduce what otherwise may be experienced as an intrusive characteristic of directive support. E-mail also generates a record of exchanges between providers and recipients, allowing the participant to review messages at anytime. In in-person exchanges, a recipient of directive advice that seems impertinent or impractical may mentally leave the conversation and fail to retain the advice provided. The log of received e-mail allows the directive support recipient to reconsider advice at a later time, perhaps when a greater sense of need increases receptivity. In retrospect, this control the recipient has over when e-mail is read creates an implicit nondirective quality that is independent of the nondirective or directive characteristics of specific messages. Finally, norms and expectations for the kind of support e-mail might deliver may have been congruent with a directive style, softening any negative response it might engender in face-to-face interventions. Putting these together, the Internet as a medium to deliver support could soften directive support and potentially dilute nondirective support. Future studies could assess the effects of telephone and in-person nondirective and directive support on weight loss to determine if findings are replicated or if the medium influences findings.
Previous studies have shown that adding an e-coach to an Internet intervention can increase the amount of weight lost [5, 9]. The current study clarified aspects of e-coach that are particularly effective. Results from this study suggest that an e-coach provides more than accountability. A directive e-coach may be helpful by establishing an appropriate plan, setting expectations for appropriate goals, reinforcing positive behaviors, pointing out negative or counterproductive behaviors, and pushing the participant to move forward.
While the current study shows advantages to a directive e-coach support intervention, it is also worth noting that participants who received minimal support also improved. Participants in the minimal support condition lost on average 3.36 kg, and over 35% achieved a 5% weight loss. The minimal support intervention involved twice weekly e-mails with weight loss lessons and a feedback graph. E-mails were personalized by including the participant’s name and including feedback graphs based on the participant’s reported data. This simple, low-intensity intervention may be an efficient first step for a stepped care Internet approach to weight loss. Future studies could evaluate whether such a minimal intervention may be useful in a stepped care approach that also includes more intensive interventions for nonresponders. This stepped approach might improve cost-effectiveness and conserve resources for those who need greater levels of assistance.
Although there were between-group differences for leisure time physical activity, no between-group differences emerged for changes in dietary behavior. The discrepancy in findings for these behavioral outcomes may be due to the match between the outcome assessed by the measure and the outcome used in goal setting for the directive support condition. In the directive support condition, goals were often set to increase time spent in leisure time physical activity which was the same outcome measured by the International Physical Activity Questionnaire. However, goals for changing dietary behavior often focused on reducing caloric intake. The Fat and Fiber Behavior Scale assessed changes in dietary behavior specific to fat and fiber rather than reduction in calories. These discrepancies may also be related to measurement error in measuring dietary intake. Previous short-term, minimal contact weight loss counseling studies have observed changes in weight without corresponding changes in self-reported measures of dietary behavior [9, 28].
A limitation of this study is that only women were included in secondary analyses limiting the generalizability of findings. Future studies should assess whether an interaction exists between gender and treatment condition (minimal, nondirective, or directive support) on weight loss. Previous studies have cited differences in the ways in which men and women seek support, utilize support, and respond to support (e.g., [29, 30]). Specific to the nondirective and directive support distinction, a previous study found differences in the relationships of nondirective and directive support to knowledge about HIV risk in males and females [31]. In females, nondirective support was positively associated with knowledge and directive support negatively associated with knowledge. In males, there was no relationship between these types of support and knowledge. These findings suggest that women may rely on social interactions to get information whereas males may rely on other resources to get information. In the current study, males in the minimal support condition appeared to lose about the same amount of weight as males in the support conditions. It is possible that males received the information they needed to lose weight from the weekly lessons and did not need additional assistance from the e-coach in making changes.
Additional limitations of this study include the lack of assessment of reach (i.e., percentage of employees who received an e-mail that choose to participate in the study) and that the principal author served as the e-coach for all participants and was not blind to the study hypotheses. Due to the limited budget of this study, training and hiring separate e-coaches was not possible. However, study findings were the reverse of those anticipated from previous research, which had led to expected advantages of nondirective support. If a bias was present, it would have favored the nondirective condition. In addition, the principal endpoint, weight loss measured in person, is objective adding credibility to results. Nevertheless, there are multiple paths by which bias may influence results and the present use of the principal author as e-coach is a limitation. A limitation to the generalizability of study findings is that the sample was relatively well-educated with 64% having a college degree. Furthermore, the current study used self-report measures administered at baseline and follow-up to assess changes in physical activity and caloric intake. Objective methods of measuring physical activity and caloric intake that do not rely on participant recall may have provided a more reliable and valid assessment of physical activity and dietary behavior throughout the study.
In conclusion, this study shows that directive support delivered by an e-coach over the Internet is beneficial for modest weight loss, reducing waist circumference and improving physical activity in females during the first 12 weeks of a weight loss program. This study provides further evidence that Internet programs can be an effective means of assisting individuals in losing weight. From the perspective of an interest in social support, characteristics of support, such as its nondirective and directive character, can be manipulated in a manner that is salient to individuals and that leads to differential behavior change and weight loss. From the perspective of weight loss, distinctions like those between directive and nondirective support, although subtle, may have importance with directive support showing advantages, at least within the context of an e-mail intervention for initial phases of weight loss. For the field of health promotion in general, revision may be needed to the assumption that emphases on empowerment and individual choice are always advantageous.
Supplementary Material
Acknowledgments
This project was supported by the National Heart Lung Blood Institute (T32 HL007456) and Washington University Dissertation Fellowship. We are grateful to Moni Adefolalu, Alexis Cooke, Megan Jablonski, and Nerri Yamamoto for their assistance with this project.
Footnotes
Conflict of Interest Dr. Fisher is supported by Peers for Progress of the American Academy of Family Physicians Foundation and through the support of that program by the Eli Lilly and Company Foundation. The authors have no other conflicts of interest to disclose.
Electronic supplementary material Below is the link to the electronic supplementary material.
Electronic Supplemental Materials (DOC 103 kb)
References
- World Health Organization Obesity and Overweight. 2003 Retrieved from http://www.who.int/dietphysicalactivity/media/en/gsfs_obesity.pdf.
- McKay HG, Feil EG, Glasgow RE, et al. Feasibility and use of an Internet support service for diabetes self-management. Diabetes Educator. 1998;24:174–179. doi: 10.1177/014572179802400207. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, Pintauro S, Buzzell P, et al. Does using the Internet facilitate the maintenance of weight loss? International Journal of Obesity Related Metabolic Disorders. 2002;26:1254–1260. doi: 10.1038/sj.ijo.0802051. [DOI] [PubMed] [Google Scholar]
- Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Archives of Internal Medicine. 2006;166:1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. Journal of the American Medical Association. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- Veverka DV, Anderson J, Auld GW, et al. Use of the stages of change model in improving nutrition and exercise habits in enlisted Air Force men. Military Medicine. 2003;168:373–379. [PubMed] [Google Scholar]
- Napolitano MA, Fotheringham M, Tate D, et al. Evaluation of an Internet-based physical activity intervention: A preliminary investigation. Annals of Behavioral Medicine. 2003;25:92–99. doi: 10.1207/S15324796ABM2502_04. [DOI] [PubMed] [Google Scholar]
- Norman GJ, Zabinski MF, Adams MA, et al. A review of eHealth interventions for physical activity and dietary behavior change. American Journal of Preventive Medicine. 2007;33:336–345. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. Journal of the American Medical Association. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- Fisher EB, Jr., La Greca AM, Greco P, et al. Directive and nondirective support in diabetes management. International Journal of Behavioral Medicine. 1997;4:131–144. doi: 10.1207/s15327558ijbm0402_3. [DOI] [PubMed] [Google Scholar]
- Gabriele JM, Walker MS, Heins JM, et al. Neighborhood climate, nondirective and directive support, health behavior and emotional status. Annals of Behavioral Medicine. 2006;30:S063. [Google Scholar]
- Harber KD, Schneider JK, Everard KM, et al. Directive support, nondirective support, and morale. Journal of Social and Clinical Psychology. 2005;24:691–722. [Google Scholar]
- Gabriele JM, Walker MS, Gill DL, et al. Differentiated roles of social encouragement and social constraint on physical activity behavior. Annals of Behavioral Medicine. 2005;29:210–215. doi: 10.1207/s15324796abm2903_7. [DOI] [PubMed] [Google Scholar]
- Walker MS, Zona DM, Fisher EB. Depressive symptoms after lung cancer surgery: Their relation to coping style and social support. Psychooncology. 2005;15:684–693. doi: 10.1002/pon.997. [DOI] [PubMed] [Google Scholar]
- Borushek A. The Calorie King Calorie, Fat & Carbohydrate Counter. 2006 ed Family Health; Costa Mesa: 2006. [Google Scholar]
- Diabetes Prevention Program Research Group The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber KH, Tate DF, Michael Bowling J. A randomized comparison of two motivationally enhanced Internet behavioral weight loss programs. Behav Res Ther. 2008;46:1090–1095. doi: 10.1016/j.brat.2008.06.008. [DOI] [PubMed] [Google Scholar]
- Lohman T, Roche A, Martorell R. Anthropometric Standardization Reference Manual. Human Kinetics; Champaign: 1988. [Google Scholar]
- Shannon J, Kristal AR, Curry SJ, et al. Application of a behavioral approach to measuring dietary change: The fat- and fiber-related diet behavior questionnaire. Cancer Epidemiological Biomarkers & Prevention. 1997;6:355–361. [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Thomas JR, Nelson JK, Thomas KT. A generalized rank-order method for nonparametric analysis of data from exercise science: A tutorial. Research Quarterly for Exercise and Sport. 1999;70:11–23. doi: 10.1080/02701367.1999.10607726. [DOI] [PubMed] [Google Scholar]
- Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: A statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: Endorsed by the American College of Cardiology Foundation. Circulation. 2004;110:2952–2967. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- Klein S, Sheard NF, Pi-Sunyer X, et al. Weight management through lifestyle modification for the prevention and management of type 2 diabetes: Rationale and strategies. A statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. American Journal of Clinical Nutrition. 2004;80:257–263. doi: 10.1093/ajcn/80.2.257. [DOI] [PubMed] [Google Scholar]
- Olefsky J, Reaven GM, Farquhar JW. Effects of weight reduction on obesity. Studies of lipid and carbohydrate metabolism in normal and hyperlipoproteinemic subjects. ****Journal of Clinical Investigation. 1974;53:64–76. doi: 10.1172/JCI107560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JR, Thomas KT. Physical activity data: Odd distributions yield strange answers. In: Welk GJ, editor. Physical Activity Assessments for Health-Related Research. Human Kinetics; Champaign: 2002. pp. 73–80. [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Redding CA, Evers KA. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education. Jossey-Bass; San Francisco: 2002. pp. 99–120. [Google Scholar]
- Leermakers EA, Anglin K, Wing RR. Reducing postpartum weight retention through a correspondence intervention. Int J Obes Relat Metab Disord. 1998;22:1103–1109. doi: 10.1038/sj.ijo.0800734. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Klein LC, Lewis BP, et al. Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review. 2000;107:411–429. doi: 10.1037/0033-295x.107.3.411. [DOI] [PubMed] [Google Scholar]
- Seale C, Ziebland S, Charteris-Black J. Gender, cancer experience and internet use: A comparative keyword analysis of interviews and online cancer support groups. Social Science & Medicine. 2006;62:2577–2590. doi: 10.1016/j.socscimed.2005.11.016. [DOI] [PubMed] [Google Scholar]
- Gabriele JM, Williams C, Cavazos P, et al. Gender differences in relationships among social factors and self-efficacy for condom use. Annals of Behavioral Medicine. 2010;39:s141. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


