Abstract
Research shows a strong association between traumatic life experience and mental health and important gender differences in that relationship in the Western European Diaspora, but much less is known about these relationships in other settings. We investigate these relationships in a poor rural Asian setting that recently experienced a decade-long armed conflict. We use data from 400 adult interviews in rural Nepal. The measures come from World Mental Health survey instruments clinically validated for this study population to measure Depression, Post Traumatic Stress Disorder (PTSD), and Intermittent Explosive Disorder (IED). Our results demonstrate that traumatic life experience significantly increases the likelihood of mental health disorders in this setting and that these traumatic experiences have a larger effect on the mental health of women than men. These findings offer important clues regarding the potential mechanisms producing gender differences in mental health in many settings.
Evidence for the widespread prevalence of mental health disorders continues to mount rapidly. New general population research in a large number of countries documents the substantial prevalence of mental health disorders across many different contexts (Herrman and Swartz 2007; Kessler and Üstün 2008; Neria, Galea, and Norris 2009), which constitutes a significant burden on health worldwide. Unfortunately, even though this research spans many countries, the vast majority of the empirical evidence comes from populations of the European Diaspora. With a small number of exceptions (Frankenberg et al. 2008; Gureje et al. 2010; Karam et al. 2008; Lopes et al. 2004; Myer et al. 2008; Sonis et al. 2009; Williams et al. 2007), empirical evidence regarding both the prevalence of mental health disorders is particularly rare from culturally distinct populations such as those in rural Africa and rural Asia (Herrman and Swartz 2007; Kessler and Üstün 2008). Because rural Asians account for an enormous fraction of the world’s population, empirical evidence from this population is an especially high scientific priority.
Research on mental health outside the European Diaspora also provides an important opportunity to advance our understanding of the mechanisms creating variations in mental health within populations. For example, a good deal of the research on the relationship between stress and mental health comes from settings in North America and focuses on marriage and family transitions as stressful events (Gove 1972; Simon 1992; Turner and Turner 1999; Umberson, Thomeer, and Williams 2012; Wheaton 1990). This literature repeatedly documents important gender differences in the relationship between stress and mental health and the most thorough longitudinal work supports the conclusion that women tend to respond to stress with increased psychological distress (internalizing) and men tend to respond to stress with increased substance use (externalizing) (Rosenfield, Lennon, and White 2005; Simon 2002; Umberson et al. 2012). However, the North American setting is characterized by a specific set of potentially stressful circumstances (Turner, Wheaton, and Lloyd 1995; Williams and Kurina 2002) and research on gendered responses to stress points toward both the specific nature of the stressful events and the specific gendered socialization of response to adversity as key elements (Simon 1992, 1995, 2002; Simon and Nath 2004; Turner and Avison 1989; Wheaton 1990). Research on settings outside of North America provides crucial opportunities to investigate both variations in the nature of stressful events and variations in gendered socialization.
This paper describes important new evidence about mental health disorders from rural Nepal and uses this evidence to provide a new window into the specific mechanisms likely to create gender differences in the mental health response to traumatic experiences. As evidence of substantial gender differences in response to trauma mounts, advance in reasoning regarding the likely mechanisms has been slow. This paper proposes three specific mechanisms likely to create gender differences in mental health consequence of trauma in Nepal and in other settings like Nepal. The Nepalese population is quite similar to the agrarian, rural populations found throughout South Asia, Southeast Asia, and China. The theoretical reasoning and empirical evidence we report provides a rare view of mental health in this highly populated region and the mechanisms we identify are likely to be relevant worldwide.
A fundamental obstacle to the construction of empirical evidence regarding mental health in the general population has been translation and medical validation of appropriate general population measures of mental health disorders (Bulmer 1998; Jowell 1998; Kuechler 1998; Lynn 2001). The World Mental Health (WMH) surveys are the largest international effort at general population measurement ever undertaken. Although successful across many nations in the European Diaspora (Kessler and Üstün 2008), even WMH surveys have struggled with translation and validation in Asia. The unique measures we report here build directly on WMH successes in European populations, but feature Nepal-specific methodology to measure a small subset of the most prevalent mental health disorders. The methodology itself is described elsewhere (Ghimire et al. 2013). The results here use general population measures of Depression, Post Traumatic Stress Disorder (PTSD), and Intermittent Explosive Disorder (IED) that were successfully validated by medical examination in rural Nepal. Though a thin slice of the total breadth of mental health disorders, these three disorders feature conditions likely to be associated with traumatic events surrounding recent political upheavals in Nepal.
Our work with these newly available measures examines the relationship between exposure to traumatic events and the prevalence of these disorders. The recent armed conflict involved widespread violence and terror throughout rural Nepal from 1998 –2006. These events created substantial individual-level variation in exposure to traumatic events, giving us the means to investigate associations between the experience of those events and mental health disorders.
BACKGROUND
The theoretical framework used to guide this investigation is the diathesis-stress model of psychopathology (Monroe and Simons 1991; Zuckerman 1999). In its most simplistic form this model poses that mental ill health arises out of an interaction between individual diathesis (vulnerability) to develop a mental disorder, and stressful life circumstances that activate this diathesis. This model is more dynamic than the name implies however in that stress can shape the diathesis as well as activate it (Ormel and Neeleman 2000). Exposure to severe stress during critical early periods of development can sensitize the individual both biologically and psychologically to respond to subsequent stress with greater reactivity (Heim, Plotsky, and Nemeroff 2004; Heim et al. 2010; Teicher et al. 2003). Environmental exposures can thus influence subsequent vulnerability, but the effect of environmental stressors at any stage in life is also partly a function of prior vulnerability. This prior vulnerability is shaped by a complex interplay of genetic, other biological, psychological and social factors (Belsky and Pluess 2009; Hyde, Mezulis, and Abramson 2008; Kendler, Gardner, and Prescott 2002).
Stress can therefore be part of the mix that determines individual vulnerability to mental disorders. It is also undoubtedly influential in activating that diathesis. There is a vast amount of research establishing stressful life events as risk factors for depression (Brown and Harris 1978; Hammen 2005; Kessler 1997; Mazure 1998; Turner and Lloyd 1999). Given this background, it is unsurprising that exposure to those stressful events specifically defined as traumatic (the focus this study) has been found to increase risk not just of PTSD but also of depression and other mental disorders (Basoglu et al. 1994; Karam et al. 1998, 2008; Lopes et al. 2004; Miller and Rasmussen 2010; Neria et al. 2009; Thapa and Hauff 2005; Turner and Lloyd 1995).
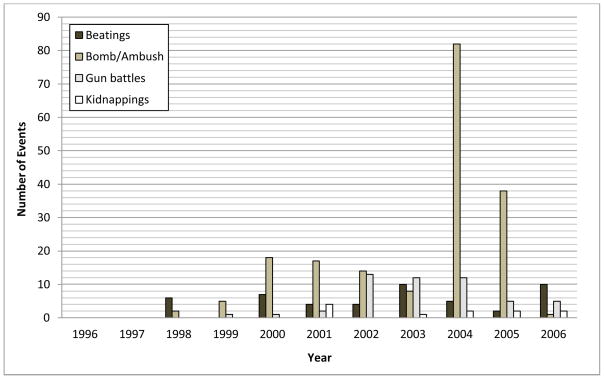
Rural Nepal provides an ideal non-European setting to examine the mental disorder consequences of traumatic stress because of the recent history of armed conflict in that setting. To illustrate this point, we document the recent history of violent events. Figure 1 provides a time line of the frequency of gun battles, bomb blasts, beatings, and kidnappings in Chitwan Valley in south central Nepal. More details about the nature of this conflict are available elsewhere (Williams et al. 2012), but clearly the conflict produced a large number of violent events over several years. These circumstances directly exposed many individuals in the population to traumatic events, and depending on physical location, exposed some individuals to multiple events over time. Notably, all individuals in the study area experienced secondary exposure to violence, meaning that violence was occurring all around them over a long period of time, most people understood that they could experience a traumatic event at any time, and this violence and the related economic instability likely created chronic stress in the population.
Figure 1.
Number of Conflict Events by Types over Time, 1996–2006.
We expect exposure to these types of traumatic events will increase the likelihood an individual reports of symptoms of Depression, PTSD, or IED (Neria et al. 2009; Thapa and Hauff 2005). Moreover, we expect that those individuals who experience many traumatic events over the course of this period will be much more likely to report symptoms than those who experience few or none of these events – “cumulative adversity” is known to be an especially significant influence on mental health (Lloyd and Turner 2003; Turner and Lloyd 1995). Of course the mental health response may vary across different types of traumatic events, but we do not investigate that possibility here. Instead, our main objective is documentation of the gross association between exposure to traumatic events and the report of symptoms of depression, PTSD, or IED.
Gender and Response to Trauma
The second key objective of this study is to investigate gender differences in the association between trauma exposure and mental disorders. Most studies on PTSD and depression find higher rates in women. Consistent with the dynamic diathesis-stress model outlined above, models of these gender differences suggest that there are neuroendocrine and psychological consequences of prior exposure to sexual abuse that confer vulnerability to the psychopathogenic effects of subsequent trauma and stress (Cortina and Kubiak 2006; DeSantis et al. 2011; Harkness, Bruce and Lumley 2006; Kendler, Kuhn, and Prescott 2004; Teicher et al. 2003; Weiss, Longhurst, and Mazure 1999). Female sex hormones (Olff et al. 2007; Parker and Brotchie 2010) and gendered socialization processes are also thought to augment female responsivity to trauma and to lead to less effective coping and greater sensitivity to lack of social support among women (Olff et al. 2007).
On the basis of these models of psychopathology and gender differences in response to trauma we hypothesise that Nepalese women may be at greater risk of psychopathological consequences of trauma than Nepalese men. The specific features of these models we consider of most relevance to Nepal are: (i) prior adversity (particularly sexual assault and domestic violence); (ii) socialization experiences; and (iii) social support as a moderator of the activation of that vulnerability by trauma.
Gender differences in earlier life experience of assault
Gender differences in early life course exposure to violent assaults may contribute to the observed gender differences in reactions to trauma, especially PTSD (Breslau and Anthony 2007). Prior research indicates that South Asian women are highly likely to experience violent assault, especially domestic violence (Kishor and Johnson 2006; Koenig et al. 2006; Naved et al. 2006). If so, according to the models above, it is quite likely that this prior exposure to violent assault will make Nepalese women more likely than men to experience PTSD after exposure to another trauma.
Gender differences in socialization: mismatch of expectations and experience
Longitudinal research demonstrates that women with life experiences quite different than their early life expectations have the highest levels of depressive symptoms (Carr 1997). The theoretical basis for this empirical outcome is clear – environmental mastery, or the ability to assert individual preferences in complex social environments, is a crucial factor determining psychological wellbeing (Ryff and Keyes 1995). When life circumstances unfold quite differently than early life expectations, an individual’s sense of environmental mastery is greatly reduced, with likely negative consequences for psychological wellbeing. Specifically, in the Nepalese setting many ethnic groups take substantial pride in socializing boys to expect exposure to, and participation in, dangerous activities including violent conflict and even war (Bista 1972; Gurung 1980). This is a fundamental dimension of a “Gorkhali” culture made famous by the British Gorkha soldiers, but also a significant source of nationalism throughout the country (Gellner, Pfaff-Czarnecka and Whelpton 1997; Gurung 1980; Rathaur 2001). In contrast, this expectation of exposure to violent conflict does not extend to women. This substantial gender difference in socialization toward armed conflict and the violence it entails creates an important gender difference in expectations for Nepalese men and women. When armed conflict entered into the everyday lives of rural Nepalese, it was a much greater violation of life expectations for women than it was for men – a difference that could contribute to significant gender differences in the experience of depression after exposure to the traumatic events of this violent conflict. Though different in both the specific form of gendered socialization and the specific type of stressful event than found in research on marriage in North America, this would be a clear example of gendered socialization produces gender differences in mental health response to stressful events (Simon 2002).
Gender differences in social support
Theoretical models of gender differences in PTSD suggest that women may be particularly affected by a lack of social support in times of trauma. Gender differences in social support from family relationships may therefore be an important dimension of gender differences in adverse mental health outcomes. For example, under various historical conditions researchers argue that men benefit more from marriage than women in the United States and European populations (Gove 1972; Rogers, Hummer, and Nam 2000; Waite and Gallagher 2000). Recent longitudinal evidence indicates that these differences may be exaggerated by failure to account for gender based differences in socialized responses to stress, so that higher rates of post-stress depression in women may be similar to higher rates of post-stress substance use in men (Simon 2002). Nevertheless, the social support provided by marriage may be greater for men, particularly if wives care for their husbands more often or more effectively than husbands care for their wives. This is important because family relationships are known to have protective effects on health in general and mental health in particular (Barrett and Turner 2005; Bonanno et al. 2007; Dressler 1985; Heymann 2006; House, Landis and Umberson 1988; Umberson et al. 1996). These protective effects are likely to be particularly important during times of armed conflict, such as in the recent history of Nepal. Gender differences in social support during the armed conflict may create greater resilience in response to trauma for men than for women.
In summary, extrapolation from models of psychopathology and gender differences in trauma response leads us to expect that traumatic exposures in Nepal will be associated with increased risk of depression, PTSD and IED and that there will be gender differences in the prevalence of these disorders in Nepal. This study tests these hypotheses.
RESEARCH SETTING
The data analysis described here comes from the Chitwan Valley of south-central Nepal. The administrative district of Chitwan borders India and is about 100 miles from Kathmandu. There is one large town, Narayanghat, and the rest of Chitwan’s population, like much of Nepal, lives in small, rural villages. The valley is flat, fertile, and dominated by agriculture. Eighty-two percent of households in the study area are involved in farming or animal husbandry.
There are several considerations that make Nepal an ideal location to study relationships between gender, traumatic events, and mental disorders. Over 85 percent of the population still lives in rural areas and practice caste-based patriarchal systems, creating inequality based on gender, caste and ethnicity (Bennett 1983; Bista 1972). Similar to other South Asian countries, Nepal also has a high degree of domestic violence against women (Paudel 2007). These factors combine to create significant differences between men and women in the level of threat each is likely to associate with armed conflict events. As a result, the mental health consequences of these events may well be different for men and women.
This setting also experienced significant armed conflict, creating a large number of traumatic events. Perhaps the most significant conflict is the ten years of insurgency and counterinsurgency that cost an estimated 13,000 lives and considerable physical, psychological, political, social and economic damage. Since that conflict ended in a peace agreement in 2006, Nepali society is undergoing a dramatic post-conflict socio-political transformation. Following the peace agreement, Nepal experienced a series of major political transitions and such events continue to expose the population to uncertainty and public security threats. Even today, most of the protest programs are using the same tactics used by the Maoists during the armed conflict: public demonstration and strike, intimidation, extortion, abduction, beating, and killing. The uncertain political and economic future and lapse of public security continue to create heavy psychological stress in the general population.
Although there is reason to suspect a high prevalence of mental health disorders, data on prevalence levels and service use are almost non-existent. There is currently no reliable source of information on the prevalence of mental health disorders in Nepal. The WHO report on Mental Health Systems of Nepal (World Health Organization 2006) states that although Nepal’s mental health policy was formulated in 1996, there is no mental health service available in terms of service areas. There is one mental hospital with a total of 0.20 beds per 100,000 population. The majority of patients are treated in outpatient facilities or not at all.
DATA AND METHODS
Measuring mental health outcomes and connections with trauma and gender is a complex task, which led us to use a multi-phasic multi-method approach. First, to identify the most common mental disorders in Nepal, we conducted a series of consultative meetings with a number of mental health professionals and an extensive review of literature on Nepal. These consultative meetings and reviews taught us lessons from previous efforts to measure mental health in Nepal and identified the disorders most likely to be associated with gender differences in response to trauma – Depression, PTSD, and IED. Second, we used cutting-edge tools in mental health research, including research instruments (WMH CIDI 3.0 - Composite International Diagnostic Interview), protocols, data entry and data coding and validation procedures (Structured Clinical Interview Diagnosis - SCID) that have been repeatedly tested, updated, and used extensively in 28 countries (Kessler and Üstün 2008). We adopted and translated these well-tested research instruments, protocols, and validation procedures to Nepali language and the cultural context of Nepali society. The details of this translation and validation process are described elsewhere (Ghimire et al. 2013). As documented there, this process produced high levels of clinical validation in our measures of Depression, PTSD and IED – levels of validation comparable to the most successful WMH country studies.
Sample Design
The final Nepali CIDI 3.0 questionnaire was administered to a general population, systematically selected sample of 400 individuals living in the Western Chitwan Valley. Using the Chitwan Valley Family Study (CVFS) sampling frame—a longitudinal panel study of 151 communities, 2,300 families, and 15,000 individuals—respondents were chosen using a two-stage sampling procedure. First, based on the distance to the urban center, the study area was divided into three distinct strata. Next, a sample of 4 to 6 neighborhoods each consisting of between 10 and 15 households were selected from each stratum. In addition, based on a local psychiatrist’s recommendation, we purposefully chose two additional neighborhoods from poor slum areas that are likely to have high prevalence of mental disorders. This process yielded 17 neighborhoods (communities) with 198 households. Once a neighborhood was selected, all the individuals age 18 and above residing in those households (eating and sleeping most of the time in the last month) within the neighborhoods were interviewed. This sampling procedure resulted in 400 individuals who were selected in a statistically representative manner that closely resembled the CVFS sample.
For validation purposes, we re-interviewed a subset of this sample. This subset included 100 percent of the respondents who were diagnosed positive for at least one disorder through the CIDI generated diagnosis (both DSM IV and ICD 10) and 10 percent of respondents who were diagnosed negative for all disorders through the CIDI generated diagnosis. This sampling procedure yielded 84 individuals, 50 positive cases and 34 negative cases. Out of 84 respondents, 80 of them were re-interviewed using the Nepali translation of SCID questionnaire in a clinical setting by a psychiatrist. Of the four respondents that we could not interview, two were refusals, one moved to India, and one suffered from severe substance abuse and could not get to the clinic for medical diagnosis.
Measures
Mental health disorders
The analysis we present investigates three mental disorders measured using this Nepali translation of WMH CIDI 3.0: Depression, PTSD, and IED. The measures of Depression, PTSD, and IED are based on the life time positive diagnosis for those disorders using the DSM IV criteria. If the respondent was diagnosed by the CIDI as ever positive for that specific disorder it is coded as ‘1’ and ‘0’ otherwise. Further, we created another dichotomous measure of ‘any disorder’ that is coded ‘1’ if an individual displayed symptoms of at least one of the three disorders.
Traumatic experiences
Our measures of traumatic experience are based on a series of questions that record if a respondent ever experienced the following: participated in combat as a soldier or peacekeeper (note both men and women may have had this experience); lived as an unarmed civilian during a period of war, revolution, military coup, invasion, or during a period of on-going terror of civilians; been a refugee, kidnapped, mugged, raped, sexually assaulted, or stalked; caused serious injury to another person (purposely or accidentally); extorted; conscripted; left home due to fear of abduction; experienced a man-made disaster including bomb explosions, a natural disaster, or a life-threatening car or other accident; been exposed to toxic chemicals; been beaten by parents, spouse, or someone else; witnessed serious physical fights at home; had a life threatening illness or a child with a life-threatening illness; seen atrocities or carnage such as mutilated bodies or mass killings; seen someone badly injured or killed; unexpectedly seen a dead body; had someone close to you die unexpectedly; or had your property seized or looted. We use an interval-level measure that records the number of these different events a respondent had ever experienced. To investigate the potential for outliers to exert a high influence on our results, we tested several different functional forms of this measure. These include versions truncated at 5 or more, 6 or more, 7 or more, 8 or more and 9 more types of traumatic experience and the natural log of the number of types of traumatic experience. We also investigate a dichotomous measure indicating whether or not a respondent ever experienced at least one of these traumatic events.
Family Characteristics
To examine family based social support we examine marital status and access to children. In our analyses marital status is a dichotomous measure, where never married, divorced, separated, and widowed are all coded as not married. Those from larger families also appear to enjoy greater social support (Dressler 1985; Mowbray et al. 2005). We expect those living in large families to have more social support, and therefore lower prevalence of mental health disorders, than those living in smaller families. We operationalize this with a dichotomous variable that is coded ‘1’ if at least four people live in the respondent’s household, otherwise coded as ‘0’.
Demographic Characteristics
Finally, we also use measures of age, gender, and education to control for other demographic influences on mental health outcomes. Education records the number of years of formal schooling the respondent had completed.
Analytic Methods
We use a series of multi-level logistic regression models to predict the outcomes: depression, PTSD, IED, or any disorder. The equation for these models is as follows:
| (1) |
where Y is the mental disorder, α is the intercept, Bk is the effect of the independent variables, Xk is the value of these independent variables, and ε is the error. We estimate multilevel models that include an adjustment for the neighborhood level clustering of cases (in SAS glimmix). Note this neighborhood level clustering includes clustering of multiple individuals in the same home. We first predict the effect of gender, family, and demographic characteristics on any disorder in the full sample (men and women). We then predict the effects of the dichotomous measure of any traumatic experience ever and lifetime number of different types of traumatic experiences (we present the version of this measure truncated at 5 or more, because it is the most analytically conservative, but all the versions we tested yield the same substantive conclusions). In order to test whether gender conditions the effect of traumatic experience on the prevalence of mental disorders, we use a model on the full sample that includes an interaction term between trauma and gender.
Next, to estimate the effects of traumatic experience on specific mental disorders, we estimate models predicting depression, PTSD, and IED separately, contingent on trauma, gender, a gender and trauma interaction, and demographic characteristics. As described below, the low levels of PTSD and IED and strong gender differences in the prevalence of these disorders limit the opportunity to test multivariate models of these outcomes.
RESULTS
There were 165 men and 235 women in the sample (see Table 1). The greater number of women in the sample is a result of the high prevalence of out-migration for labor from this area amongst men and not women (Massey et al. 2010; Williams 2009). The average age was 42 years for men, and 34 years for women. Again, the older average age of men is likely a result of high male out-migration concentrated in the younger adult ages, leaving older men at home. Most respondents were married: 81% of men and about 84% of women. Seventy percent of respondents (male and female) lived in households with at least four people. As is common in Nepal, men had more education, having completed an average of 5.7 years compared to women who had completed an average of 4.3 years of school.
Table 1.
Descriptive Statistics from the Chitwan Health and Stress Study (N=400).
| Range | Men (N=165) Frequency/Mean |
Women (N=235) Frequency/Mean |
|
|---|---|---|---|
| Demographic Characteristics | |||
| Age (mean) | 18–90 | 42 | 34 |
| Married (%) | 0,1 | 81 | 84 |
| Household Size (% 4+ people) | 0,1 | 70 | 71 |
| Education (mean yrs completed) | 0–16 | 5.73 | 4.30 |
| Traumatic Experience | |||
| Any Trauma (%) | 0,1 | 75 | 63 |
| Number of Traumas (mean) | 0–14 | 2.18 | 1.41 |
| Number of Traumas topcoded to 5 (mean) | 0–5 | 1.96 | 1.37 |
| Mental Disorders | |||
| Any Disorder (%) | 0,1 | 7.88 | 8.51 |
| Depression (%) | 0,1 | 4.85 | 5.96 |
| PTSD (%) | 0,1 | 1.21 | 5.96 |
| Intermittent Explosive Disorder (%) | 0,1 | 2.42 | .85 |
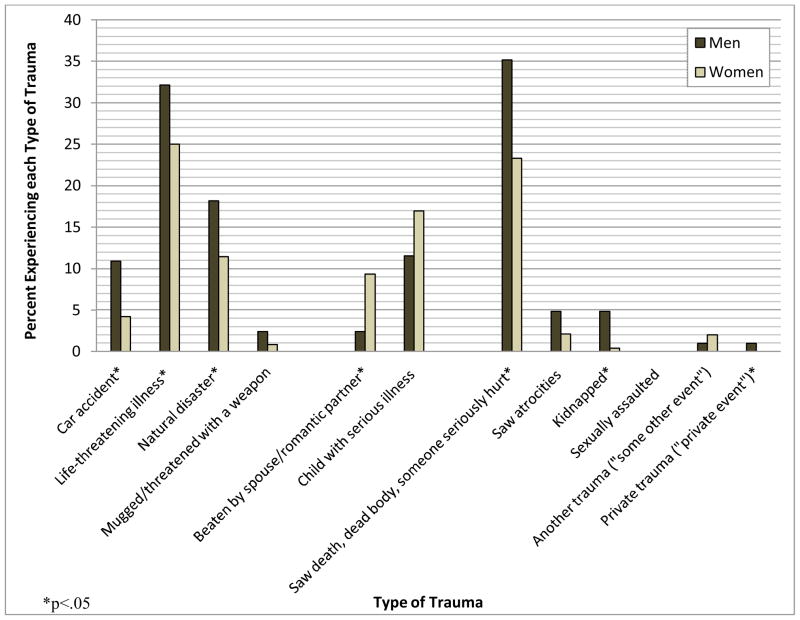
Men also experienced more trauma. Seventy-five percent experienced any of the traumatic events measured, whereas only 63% of women had experienced any traumatic event. Similarly, men had experienced an average of 2.18 traumatic events, compared to an average of 1.41 events for women. More detailed analysis of the reports of traumatic events also reveals that Nepalese men were more likely to experience many different specific types of traumatic events and often this difference was statistically significant. Figure 2 shows these results for the most commonly reported traumatic experiences (see Figure 2).
Figure 2.
Percentage Ever Experienced Type of Trauma (N=400).
We have organized these gender differences into some interesting groups in Figure 2. The first group is common traumatic experiences that are not connected with armed conflict. Men were significantly more likely than women to report experiencing a car accident, a life-threatening illness, or a natural disaster. Women, on the other hand, were significantly more likely to report being beaten by a spouse and slightly more likely to report having a child with a serious illness. Men were more likely to report all types of trauma associated with the armed conflict and no one reported rape or sexual assault in these data. Official data about the conflict indicate many rapes occurred, but it is quite likely that the social stigma associated with sexual assault in Nepal prevented respondents from admitting this experience. The CIDI instrument allows respondents to report “another trauma” or a “private trauma” and these may reflect sexual assault. More advanced survey methods, such as Audio-Computer Assisted Self Interviewing (ACASI), are likely needed to obtain measures of such experience (Potdar and Koenig 2005; Tourangeau and Smith 1996). This result means these data likely reflect under reports of traumatic experience, especially violent sexual assaults on women.
Among the mental health disorders we investigate, women experienced a slightly higher prevalence of mental disorders than men; 8.51% of women ever experienced any disorder, but only 7.88% of men ever experienced any disorder (Table 1). However the gender differences in specific disorders are more complex. Women are more likely than men to report depression, but the difference is not big – 5.96% of women compared to 4.85% of men. Women were much more likely to experience PTSD than men – 5.96% of women compared to 1.21% of men. Thus the prevalence of PTSD was nearly five times higher for women even though men were more likely to experience trauma. By contrast, IED was much more common among men – 2.42% of men compared to only 0.85% among women. This difference in the opposite direction is also substantial, with men nearly three times more likely than women to experience IED. Thus in this setting of armed conflict with widespread traumatic experience we find a substantial gender difference in two key disorders running in opposite directions.
Note the overall rates of disorders appear relatively low compared to other settings with recent armed conflict (Kessler and Üstün 2008). One possibility is that Nepalese are particularly resilient. Relative to armed conflict this may be true. Nepal is among the poorest countries in the world (UNDP 2011), mortality data demonstrate daily life is arduous and risky (UNDP 2011), and those who survive to every specific age are selected for survival and highly resilient. This survival resilience may well apply to mental health as well as physical health. However, it is also relevant that this study is geographically located in an area of Nepal that was not the most violent during the conflict. It may be that though traumatic events occurred and individuals report their exposure, the overall level violence was low enough these events did not promote the level of mental health reaction seen in more violent settings.
Results from Multivariate Models
Next we turn to multivariate models predicting the consequences of trauma, demographic, and family characteristics on mental disorders. Table 2 presents the results from models predicting any disorder, including depression, PTSD, and IED. As shown in Model 1, which includes the demographic and family measures, there were no significant predictors of any mental disorder.
Table 2.
Results from Logistic Regression Models Predicting any Mental Disorder (Depression, PTSD, Intermittent Explosive Disorder).
| Model 1 Any disorder |
Model 2 Any disorder |
Model 3 Any disorder |
Model 4 Any disorder |
|
|---|---|---|---|---|
| Traumatic Experience | ||||
| Any trauma | 5.32 ** (2.66) | |||
| Number of traumas | 1.85 *** (4.74) | 1.35 * (1.67) | ||
| Number of traumas * female | 1.75 * (2.26) | |||
| Demographic Characteristics | ||||
| Age | 1.01 (.71) | 1.01 (.40) | 1.02 (.95) | 1.01 (.86) |
| Female | 1.17 (.37) | 1.25 (.53) | 1.82 ^ (1.32) | .37 (1.23) |
| Married | 1.85 (.95) | 1.81 (.92) | 1.38 (.48) | 1.24 (.32) |
| Household Size (4+) | .76 (.71) | .74 (.76) | .58 ^ (1.31) | .53 ^ (1.50) |
| Education | 1.00 (.01) | .98 (.43) | .98 (.36) | .96 (.62) |
|
| ||||
| −2 res log pseudo-likelihood No. of Obs. = 400 |
2186 | 2338 | 2490 | 2368 |
Note: Odds ratios are reported, with Z-statistics shown in parentheses.
p<.10
p<.05
p<.01
p<.001(one-tailed tests)
The effect of traumatic experience is tested in Models 2 and 3 of Table 2. As shown in Model 2, ever having experienced any traumatic event increases the likelihood of developing a mental disorder by more than five times. The effect of the number of different kinds of traumatic experiences, shown in Model 3, is somewhat smaller, with an odds ratio of 1.85. However, odds ratios are multiplicative, so that someone who experienced two types of events would be 3.43 times (1.85*1.85) more likely to develop a mental disorder and those who experienced four types of events are over ten times more likely.
Model 3 also shows that controlling for the number of different kinds of trauma reveals a statistically significant gender difference, in which women were almost two times more likely to experience any mental disorder, independent of trauma. That is, failure to control for the gender differences in experiencing multiple kinds of trauma masks the underlying gender difference in the likelihood of mental illness. In Nepal, once we control for men’s higher likelihood of experiencing multiple kinds of trauma, we reveal a strong association between gender and mental illness.
Next we explore the interaction between gender and trauma. Model 4 includes an additional term for the interaction between gender and trauma. The interaction term is statistically significant, with an odds ratio of 1.75. The statistically significant interaction term means that Nepalese women are significantly more likely to respond to trauma this way than their male counterparts who also experienced traumatic events. Overall, traumatic experience had large and significant effects on mental health and a larger influence on the mental health of women than men.
To address specific mental disorders, we turn to analysis of each individual disorder. Unfortunately, because the incidence of PTSD and IED are low but the gender differences are high, it is difficult to test the same gender interactions in models of PTSD and IED. Instead, we begin by investigating models of depression, as displayed in Table 3. As shown in Model 6, traumatic experience significantly increased the likelihood of reporting depression, and the magnitude of this effect is nearly the same as the effect on all three disorders presented in Table 2. Also similar to the results displayed in Table 2, the interaction between gender and traumatic experience was positive and significant as well as of a similar magnitude (Model 7 of Table 3). Traumatic experience had a large and significant effect, increasing reports of depression, but this effect was much stronger among women than among men. Finally, note that as expected, those from larger households were significantly less likely to report depression independent of the experience of trauma.
Table 3.
Results from Logistic Regression Models Predicting Depression.
| Model 5 Depression |
Model 6 Depression |
Model 7 Depression |
|
|---|---|---|---|
| Traumatic Experience | |||
| Number of traumas | 1.84 *** (3.75) | 1.34 (1.23) | |
| Number of traumas * female | 1.70 * (1.75) | ||
| Demographic Characteristics | |||
| Age | 1.02 (1.20) | 1.03 (1.23) | 1.03 (1.18) |
| Female | 1.50 (.77) | 2.12 ^ (1.35) | .49 (.74) |
| Married | 1.69 (.67) | 1.28 (.31) | 1.16 (.18) |
| Household Size (4+) | .58 (1.17) | .39 * (1.87) | .36 * (2.00) |
| Education | 1.02 (.28) | .98 (.23) | .97 (.43) |
|
| |||
| −2 res log pseudo-likelihood No. of obs. = 400 |
2340 | 2563 | 2511 |
Note: Odds ratios are reported, with Z-statistics shown in parentheses.
p<.10
p<.05
p<.01
p<.001(one-tailed tests)
We find similar results for the impact of gender and trauma on PTSD, but because PTSD is so rare among men, we do not show a multivariate model estimation with both genders. Among women, however, we estimate each additional type of traumatic experience increases the odds of reporting PTSD by 2.15 times (not shown in tables). This large and statistically significant effect means that women who experience four types of trauma are more than ten times more likely to report PTSD. By contrast, among men only, traumatic experience had no statistically significant influence on reports of PTSD (not shown in tables). Traumatic experience dramatically increases reports of PTSD among Nepalese women, but not among Nepalese men.
We also tested the influence of traumatic experience and demographic characteristics on IED. Because the prevalence of IED amongst women was very low (only 0.85% of women), we used a sample of only men. An odds ratio of 1.53, results (not shown) indicates that traumatic experience increased the likelihood of experiencing IED for men by about 50%. This effect was statistically significant. Demographic characteristics had no significant influence on IED reports for men.
DISCUSSION
Overall these results demonstrate that social experiences shape the incidence of mental health disorders in a rural Asian population in the way theory predicts. Traumatic events increase the likelihood of disorders, at least among the disorders we investigate here. Rural Nepal was a place of significant armed conflict over the past decade, giving many in the population exposure to chronic stress as well as violent traumatic events, including gun battles, bombings, beatings, and abductions. Any exposure to these events significantly increased the likelihood of experiencing a mental health disorder and exposure to many events produced much higher likelihoods of disorders than exposure to few events. Though the stressful events themselves are different, this finding is consistent with North American research regarding the consequences of stressful experiences and the cumulative consequences of multiple stressful experiences (Turner and Lloyd 1995; Wheaton 1990).
Equally interesting, even in rural Nepal there is an important gender interaction with experiencing traumatic events. Both men and women who experienced traumatic events were more likely to report a mental health disorder, but the consequence of traumatic experience was significantly stronger among women than among men. Even though women were significantly less likely to be exposed to traumatic events during this armed conflict, when they did have traumatic experiences they were much more likely than men to suffer mental illness. Though this replicates a result already documented in a handful of other settings, the result is the most important contribution of our findings.
In fact it is precisely because this finding replicates results documented in other settings that it is important. It was nearly twenty years ago that research documented this same type of result for PTSD and other disorders in North America (Kessler et al. 1995; Turner and Lloyd 1995). Studies of trauma and PTSD have replicated this result under a variety of different circumstance in the United States, in Northern Ireland, in Israel and in Indonesia (Bonanno et al. 2007; Breslau 2002; Frankenberg et al. 2008; Palmieri et al. 2007; Stuber et al. 2006). A similar gender difference has also been documented for depression (Hall et al. 2008). Our findings from Nepal do not mean this gender difference is universal, but they certainly do mean this difference is wide spread. Spread across cultures, economies, and sources of trauma. This topic deserves a higher priority in future research.
Of course many limitations of the study we report prevent it from answering key questions about the mechanisms responsible. First, the data are cross-sectional and does not measure change in mental health status over time. It is unlikely that prior mental health conditions produced exposure to traumatic events, but mental health conditions may have preceded exposure to traumatic experience and may have influenced reporting of exposure to such events. Multiple measures across time would provide a significantly stronger research design. Second, as noted above, these measures of traumatic experience appear to be underestimates, with no reports of sexual assault related trauma. This not only attenuates estimates of trauma experience, it also limits our ability to test a key hypothesis – the possibility that prior experience of violent assault increases the likelihood of a mental health reaction to trauma for women (Breslau and Anthony 2007). Other measurement limitations also prevent comprehensive investigation of the competing hypotheses. These limitations leave plenty of room for future contributions.
Nevertheless, the findings do offer a few intriguing clues regarding the potential mechanisms at work. First, we find similar gender interactions with respect to both PTSD and depression, and in this setting the effect sizes appear stronger for depression than for PTSD. Mechanisms more closely associated with depression, such as mismatch between socialized expectations and later experience, may well be an important element in the creation of the gender differences we observe (Carr 1997). This finding supports the more general argument that early life gender differences in socialization contribute to later life mental health responses to stress or traumatic experience (Simon 2002). In this Nepalese case the subject matter of gendered socialization – expectations for direct participation in violent armed conflict – are quite a bit different than gendered socialization about family roles, but the consequence for gender differences in mental health may be similar.
Second, though limited in our measures to investigate family social support, the measures of marital status and family size we use do little to explain this important gender difference in response to trauma. Though important gender differences in the social support from family relationships are highly likely in Nepal, and we find living in larger families reduces reports of depression, these differences may not help us understand the gender differences in mental health response to traumatic events. Again, though the setting and stressful events are different, this result echoes North American findings that the relationships between family support, family roles and mental health may be quite complex and dependent on the specific nature of the stressful events themselves (Umberson et al. 2012).
Third, just as US research on gender differences in the relationship between stress and mental health supports the conclusion that men and women tend to respond to stress differently, we also discovered an important gender difference in response to the stress associated with traumatic experience in Nepal. Research in the US indicates women respond to stress with increased psychological distress (internalizing) and men tend to respond to stress with increased substance use (externalizing) (Rosenfield et al. 2005; Simon 2002; Umberson et al. 2012). In Nepal we find both men and women respond to stressful traumatic experience with elevated reports of PTSD, but this effect is stronger for women than men. We also find that women are much more likely than men to respond to traumatic experience with depression, but men are much more likely than women to respond to traumatic experience with IED. That is, male reactions to traumatic experience may be as strong as female reactions to traumatic experience, but expressed through different symptoms. This possibility deserves more research.
The North American setting is characterized by a specific set of potentially stressful circumstances (Turner et al. 1995; Williams and Kurina 2002) and research in that setting on gendered responses to stress points toward both the specific nature of the stressful events and the specific gendered socialization of response to adversity as key elements (Simon 1992, 1995, 2002; Simon and Nath 2004; Turner and Avison 1989; Wheaton 1990). Research on settings outside of North America provides crucial opportunities to investigate both variations in the nature of stressful events and variations in gendered socialization. Thus research on the mental health response to stress in a wide range of settings – advancing the investigation we begin here – is a high priority complement to research on North America.
Moreover, by the mid-1990s World Health Organization identified depression as the leading cause of disease related disability among women in the world (Kessler 2006; Murray and Lopez 1996). This health problem is enormous and worldwide. The evidence we present here is consistent with the possibility that differential response to traumatic events is part of the gender difference in occurrence of depression. The topic deserves our highest scientific priority. Investigation of the multiple potential mechanisms is a high priority in the study of differential response to traumatic experience. The clues provided here point us toward the research designs we need: detailed longitudinal studies with carefully crafted measures of each rival hypothesis are a high scientific and health policy priority.
Acknowledgments
This research was jointly supported by the University of Michigan Population Studies Center Small Grant program and the University of Michigan Global Health Research and Training Initiative. The authors gratefully acknowledge use of the services and facilities of the Population Studies Center, funded by NICHD Center Grant R24 HD041028. The authors thank Cathy Sun at the Population Studies Center and Nancy Sampson at the Department of Health Care Policy, Harvard Medical School for their assistance creating analysis files, constructing measures, and conducting analyses. Additionally, the authors thank Jennifer Mamer and Austin Kozlowski for their assistance preparing this manuscript, the staff of the Institute for Social and Environment Research—Nepal, and the residents of the Western Chitwan Valley for their contributions to the research reported here. The authors alone remain responsible for any errors or omissions.
Biographies
William G. Axinn is a professor of sociology and the director of the Survey Research Center at the University of Michigan. He studies community and intergenerational influences on marriage and fertility behavior, mixed methods approaches for measuring population change and variation, population and environment dynamics, and mental health in Nepal and the United States.
Dirgha J. Ghimire is an associate research scientist in the Population Studies Center at the University of Michigan and director of the Institute for Social and Environmental Research in Nepal. His research focuses on social change, family and demography, migration, population health, mental health, and population and environment dynamics in Nepal and the United States.
Nathalie E. Williams is an assistant professor in the Jackson School of International Studies and the Department of Sociology at the University of Washington. Her research focuses on migration, population change, and mental health during armed conflict and natural disasters, and on developing new data collection and analytical strategies for the study of migration. Her work is primarily based in Nepal, Thailand, Cambodia, and the Persian Gulf.
Kate M. Scott is an associate professor in psychological medicine in the Dunedin School of Medicine, University of Otago, New Zealand. She is a clinical psychologist and psychiatric epidemiologist. She is a principal investigator of the New Zealand arm of the World Mental Health Surveys and her current research interests include gender differences in mental disorders and associations between mental and physical health.
References
- Barrett Anne E, Jay Turner R. Family Structure and Mental Health: The Mediating Effects of Socioeconomic Status, Family Process, and Social Stress. Journal of Health and Social Behavior. 2005;46(2):156–69. doi: 10.1177/002214650504600203. [DOI] [PubMed] [Google Scholar]
- Basoglu Metin, Paker Murat, Ozmen Erdogan, Tasdemit Ozgun, Sahin Dogan. Factors Related to Long-term Traumatic Stress Responses in Survivors of Torture in Turkey. Journal of the American Medical Association. 1994;272(5):357–63. doi: 10.1001/jama.1994.03520050037027. [DOI] [PubMed] [Google Scholar]
- Belsky Jay, Pluess Michael. Beyond Diathesis Stress: Differential Susceptibility to Environmental Influences. Psychological Bulletin. 2009;135:885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Bennett Lynn. Dangerous Wives and Sacred Sisters. New York, NY: Columbia University Press; 1983. [Google Scholar]
- Bista Dor B. People of Nepal. Kathmandu, Nepal: Ratna Pustak Bhandar; 1972. [Google Scholar]
- Bonanno George A, Galea Sandro, Bucciarelli Angela, Vlahov David. What Predicts Psychological Resilience After Disaster? The Role of Demographics, Resources, and Life Stress. Journal of Consulting and Clinical Psychology. 2007;75(5):671–82. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- Breslau Naomi. Gender Differences in Trauma and Posttraumatic Stress Disorder. Journal of Gender Specific Medicine. 2002;5(1):34–40. [PubMed] [Google Scholar]
- Breslau Naomi, Anthony James C. Gender Differences in the Sensitivity to Posttraumatic Stress Disorder: An Epidemiological Study of Urban Young Adults. Journal of Abnormal Psychology. 2007;116(3):607–11. doi: 10.1037/0021-843X.116.3.607. [DOI] [PubMed] [Google Scholar]
- Brown George W, Harris Tirril. Social Origins of Depression. New York: The Free Press; 1978. [Google Scholar]
- Bulmer Martin. Introduction: The Problem of Exporting Social Survey Research. American Behavioral Scientist. 1998;42(2):153–67. [Google Scholar]
- Carr Deborah. The Fulfillment of Career Dreams at Midlife: Does it Matter for Women’s Mental Health? Journal of Health and Social Behavior. 1997;38(4):331–44. [PubMed] [Google Scholar]
- Cortina Lilia M, Kubiak Sheryl P. Gender and Posttraumatic Stress: Sexual Violence as an Explanation for Women’s Increased Risk. Journal of Abnormal Psychology. 2006;115:753–59. doi: 10.1037/0021-843X.115.4.753. [DOI] [PubMed] [Google Scholar]
- DeSantis Stacia M, Baker Nathaniel L, Back Sudie E, Spratt Eve, Ciolino Jody D, Maria Megan Moran-Santa, Dipankar Bandyopadhya, Brady Kathleen T. Gender Differences in the Effect of Early Life Trauma on Hypothalamic–Pituitary–Adrenal Axis Functioning. Depression and Anxiety. 2011;28:383–92. doi: 10.1002/da.20795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler William W. Extended Family Relationships, Social Support, and Mental Health in a Southern Black Community. Journal of Health and Social Behavior. 1985;26(1):39–48. [PubMed] [Google Scholar]
- Frankenberg Elizabeth, Friedman Jed, Gillespie Thomas, Ingwersen Nicholas, Pynoos Robert, Rifai Iip, Sikoki Bondan, Sumantri Cecep, Suriastini Wayan, Thomas Duncan. Mental Health in Sumatra after the Tsunami. American Journal of Public Health. 2008;98(9):1671–77. doi: 10.2105/AJPH.2007.120915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gellner David N, Pfaff-Czarnecka Joanna, Whelpton John. Nationalism and Ethnicity in a Hindu Kingdom. Newark, NJ: Harwood Academic Publisher; 1997. [Google Scholar]
- Ghimire Dirgha J, Chardoul Stephanie, Kessler Ronald C, Axinn William G, Adhikari Bishnu P. Modifying and Validating the Composite International Diagnostic Interview (CIDI) for Use in Nepal. International Journal of Methods in Psychiatric Research. 2013;22(1):71–81. doi: 10.1002/mpr.1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gove Walter R. The Relationship between Sex Roles, Marital Status, and Mental Illness. Social Forces. 1972;51(1):34–44. [Google Scholar]
- Gureje Oye, Uwakwe Richard, Oladeji Bibilola, Makanjuola Victor O, Esan Oluyomi. Depression in Adult Nigerians: Results from the Nigerian Survey of Mental Health and Well-being. Journal of Affective Disorders. 2010;120:158–64. doi: 10.1016/j.jad.2009.04.030. [DOI] [PubMed] [Google Scholar]
- Gurung Harka B. Vignettes of Nepal. Kathmandu, Nepal: Sajha Prakashan; 1980. [Google Scholar]
- Hall Brian J, Hobfoll Stevan E, Palmieri Patrick A, Canetti-Nisim Daphna, Shapira Oren, Johnson Robert J, Galea Sandro. The Psychological Impact of Impending Forced Settler Disengagement in Gaza: Trauma and Posttraumatic Growth. Journal of Traumatic Stress. 2008;21(1):22–29. doi: 10.1002/jts.20301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen Constance. Stress and Depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Harkness Kate L, Bruce Alanna E, Lumley Margaret N. The Role of Childhood Abuse and Neglect in the Sensitization to Stressful Life Events in Adolescent Depression. Journal of Abnormal Psychology. 2006;115:730–41. doi: 10.1037/0021-843X.115.4.730. [DOI] [PubMed] [Google Scholar]
- Heim Christine, Plotsky Paul M, Nemeroff Charles B. Importance of Studying the Contributions of Early Adverse Experience to Neurobiological Findings in Depression. Neuropsychopharmacology. 2004;29:641–48. doi: 10.1038/sj.npp.1300397. [DOI] [PubMed] [Google Scholar]
- Heim Christine, Shugart Margaret, Edward Craighead W, Nemeroff Charles B. Neurobiological and Psychiatric Consequences of Child Abuse and Neglect. Developmental Psychobiology. 2010;52:671–90. doi: 10.1002/dev.20494. [DOI] [PubMed] [Google Scholar]
- Herrman Helen, Swartz Leslie. Promotion of Mental Health in Poorly Resourced Countries. Lancet. 2007;370(9594):1195–97. doi: 10.1016/S0140-6736(07)61244-6. [DOI] [PubMed] [Google Scholar]
- Heymann Jody. Forgotten Families: Ending the Growing Crisis Confronting Children and Working Parents in the Global Economy. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- House James S, Landis Karl R, Umberson Debra. Social Relationships and Health. Science. 1988;241(4865):540–45. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hyde Janet S, Mezulis Amy H, Abramson Lyn Y. The ABCs of Depression: Integrating Affective, Biological, and Cognitive Models to Explain the Emergence of the Gender Difference in Depression. Psychological Review. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- Jowell Roger. How Comparative is Comparative Research? American Behavioral Scientist. 1998;42(2):168–77. [Google Scholar]
- Karam Elie G, Howard Diantha B, Karam Aimee N, Ashkar Alice, Shaaya Monique, El-Khoury Nazek. Major Depression and External Stressors: The Lebanon Wars. European Archives of Psychiatry and Clinical Neuroscience. 1998;248(5):225–30. doi: 10.1007/s004060050042. [DOI] [PubMed] [Google Scholar]
- Karam Elie G, Mneimneh Zeina N, Dimassi Hani, Fayyad John A, Karam Aimee N, Nasser Soumana C, Chatterji Somnath, Kessler Ronald C. Lifetime Prevalence of Mental Disorders in Lebanon: First Onset, Treatment, and Exposure to War. PLoS Medicine. 2008;5(4):e61. doi: 10.1371/journal.pmed.0050061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler Kenneth S, Gardner Charles O, Prescott Carol A. Toward a Comprehensive Developmental Model for Major Depressive Disorder in Women. American Journal of Psychiatry. 2002;159:1133–45. doi: 10.1176/appi.ajp.159.7.1133. [DOI] [PubMed] [Google Scholar]
- Kendler Kenneth S, Kuhn Jonathan W, Prescott Carol A. Childhood Sexual Abuse, Stressful Life Events and Risk for Major Depression in Women. Psychological Medicine. 2004;34:1475–82. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C. The Effects of Stressful Life Events on Depression. Annual Review of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C. The Epidemiology of Depression Among Women. In: Keyes CLM, Goodman Sherryl H, editors. Women and Depression: A Handbook for the Social, Behavioral, and Biomedical Sciences. New York: Cambridge University Press; 2006. pp. 22–37. [Google Scholar]
- Kessler Ronald C, Sonnega Amanda, Bromet Evelyn, Hughes Michael, Nelson Christopher B. Posttraumatic Stress Disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C, Bedirhan Üstün T. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York: Cambridge University Press; 2008. [Google Scholar]
- Kishor Sunita, Johnson Kiersten. Reproductive Health and Domestic Violence: Are the Poorest Women Uniquely Disadvantaged? Demography. 2006;43:293–307. doi: 10.1353/dem.2006.0014. [DOI] [PubMed] [Google Scholar]
- Koenig Michael A, Stephenson Rob, Ahmed Saifuddin, Jejeebhoy Shireen J, Cambell Jacquelyn. Individual and Contextual Determinants of Domestic Violence in North India. American Journal of Public Health. 2006;96(1):132–38. doi: 10.2105/AJPH.2004.050872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd Donald A, Jay Turner R. Cumulative Adversity and Posttraumatic Stress Disorder: Evidence from a Diverse Community Sample of Young Adults. American Journal of Orthopsychiatry. 2003;73(4):381–91. doi: 10.1037/0002-9432.73.4.381. [DOI] [PubMed] [Google Scholar]
- Lopes Cardozo Barbara, Bilukha Oleg O, Gotway Crawford Carol A, Shaikh Irshad, Wolfe Mitchell I, Gerber Michael L, Anderson Mark. Mental Health, Social Functioning, and Disability in Postwar Afghanistan. Journal of the American Medical Association. 2004;292(5):575–84. doi: 10.1001/jama.292.5.575. [DOI] [PubMed] [Google Scholar]
- Lynn Peter. The Impact of Incentives on Response Rates to Personal Interview Surveys: Role and Perceptions of Interviewers. International Journal of Public Opinion Research. 2001;13(3):326–37. [Google Scholar]
- Massey Douglas S, Williams Nathalie, Axinn William G, Ghimire Dirgha J. Community Services and Out-Migration. International Migration. 2010;48(3):1–41. doi: 10.1111/j.1468-2435.2009.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazure Carolyn M. Life Stressors as Risk Factors in Depression. Clinical Psychology: Science and Practice. 1998;5:291–313. [Google Scholar]
- Miller Kenneth E, Rasmussen Andrew. War Exposure, Daily Stressors, and Mental Health in Conflict and Post-Conflict Settings: Bridging the Divide between Trauma-Focused and Psychosocial Frameworks. Social Science & Medicine. 2010;70(1):7–16. doi: 10.1016/j.socscimed.2009.09.029. [DOI] [PubMed] [Google Scholar]
- Monroe Scott M, Simons Anne D. Diathesis-Stress Theories in the Context of Life Stress Research: Implications for the Depressive Disorders. Psychological Bulletin. 1991;110:406–25. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Mowbray Carol T, Bybee Deborah, Hollingsworth Leslie, Goodkind Sara, Oyserman Daphna. Living Arrangements and Social Support: Effects on the Well-being of Mothers with Mental Illness. Social Work Research. 2005;29(1):41–55. [Google Scholar]
- Murray CJL, Lopez AD. The Global Burden of Diseases: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Boston: Harvard School of Public Health, WHO and World Bank; 1996. [Google Scholar]
- Myer Landon, Stein Dan J, Grimsrud Anna, Seedat Soraya, Williams David R. Social Determinants of Psychological Distress in a Nationally-Representative Sample of South African Adults. Social Science & Medicine. 2008;66(8):1828–40. doi: 10.1016/j.socscimed.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naved Ruchira T, Azim Safia, Bhuiya Abbas, Persson Lars A. Physical Violence by Husbands: Magnitude, Disclosure, and Help Seeking Behavior of Women in Bangladesh. Social Science and Medicine. 2006;62(12):2917–29. doi: 10.1016/j.socscimed.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Neria Yuval, Galea Sandro, Norris Fran H. Mental Health and Disasters. Cambridge, MA: Cambridge University Press; 2009. [Google Scholar]
- Olff Miranda, Langeland Willie, Draijer Nel, Gersons Berthold P. Gender Differences in Posttraumatic Stress Disorder. Psychological Bulletin. 2007;133:183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Ormel Johan, Neeleman Jan. Towards a Dynamic Stress-Vulnerability Model of Depression: The Role of Neuroticism, Life Events, and Gender. In: Harris Tirril., editor. Where Inner and outer Worlds Meet: Psychological Research in the Tradition of George W. Brown. Florence, KY: Routledge; 2000. pp. 151–69. [Google Scholar]
- Palmieri Patrick A, Weathers Frank W, Difede JoAnn, King Daniel W. Confirmatory Factor Analysis of the PTSD Checklist and the Clinician-Administered PTSD Scale in Disaster Workers Exposed to the World Trade Center Ground Zero. Journal of Abnormal Psychology. 2007;116(2):329–41. doi: 10.1037/0021-843X.116.2.329. [DOI] [PubMed] [Google Scholar]
- Parker Gordon B, Brotchie Heather L. Gender Differences in Depression. International Review of Psychiatry. 2010;22:429–36. doi: 10.3109/09540261.2010.492391. [DOI] [PubMed] [Google Scholar]
- Paudel Giridhari S. Domestic Violence against Women in Nepal. Gender, Technology and Development. 2007;11(2):199–233. [Google Scholar]
- Potdar Rukmini, Koenig Michael A. Does Audio-CASI Improve Reports of Risky Behavior? Evidence From a Randomized Field Trial among Young Urban Men in India. Studies in Family Planning. 2005;36(2):107–16. doi: 10.1111/j.1728-4465.2005.00048.x. [DOI] [PubMed] [Google Scholar]
- Rathaur Kamal Raj Sing. British Gurkha Recruitment: A Historical Perspective. Voice of History. 2001;16(2):19–24. [Google Scholar]
- Rogers Richard G, Hummer Robert A, Nam Charles B. Living and Dying in the USA. San Diego, CA: Academic Press; 2000. [Google Scholar]
- Rosenfield Sarah, Lennon Mary Clare, White Helene Raskin. The Self and Mental Health: Self-salience and the Emergence of Internalizing and Externalizing Problems. Journal of Health and Social Behavior. 2005;46:323–40. doi: 10.1177/002214650504600402. [DOI] [PubMed] [Google Scholar]
- Ryff Carol D, Keyes Corey LM. The Structure of Psychological Well-being Revisited. Journal of Personality and Social Psychology. 1995;69(4):719–27. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Simon Robin W. Parental Role Strains, Salience of Parental Identity and Gender Differences in Psychological Distress. Journal of Health and Social Behavior. 1992;33(1):25–35. [PubMed] [Google Scholar]
- Simon Robin W. Gender, Multiple Roles, Role Meaning, and Mental Health. Journal of Health and Social Behavior. 1995;36(2):182–94. [PubMed] [Google Scholar]
- Simon Robin W. Revisiting the Relationships among Gender, Marital Status, and Mental Health. American Journal of Sociology. 2002;107(4):1065–96. doi: 10.1086/339225. [DOI] [PubMed] [Google Scholar]
- Simon Robin W, Nath Leda E. Gender and Emotion in the United States: Do Men and Women Differ in Self-Reports of Feelings and Expressive Behavior? American Journal of Sociology. 2004;109(5):1137–76. [Google Scholar]
- Sonis Jeffrey, Gibson James L, de Jong Joop TVM, Field Nigel P, Hean Sokhom, Komproe Ivan. Probable Posttraumatic Stress Disorder and Disability in Cambodia: Associations With Perceived Justice, Desire for Revenge, and Attitudes Toward the Khmer Rouge Trials. Journal of the American Medical Association. 2009;302(5):527–36. doi: 10.1001/jama.2009.1085. [DOI] [PubMed] [Google Scholar]
- Stuber Jennifer, Galea Sandro, Boscarino Joseph A, Schlesinger Mark. Was There Unmet Mental Health Need After the September 11, 2001 Terrorist Attacks? Social Psychiatry and Psychiatric Epidemiology. 2006;41(3):230–40. doi: 10.1007/s00127-005-0022-2. [DOI] [PubMed] [Google Scholar]
- Teicher Martin H, Andersen Susan L, Polcari Ann, Anderson Carl M, Navalta Carryl P, Kim Dennis M. The Neurobiological Consequences of Early Stress and Childhood Maltreatment. Neuroscience and Biobehavioral Reviews. 2003;27:33–44. doi: 10.1016/s0149-7634(03)00007-1. [DOI] [PubMed] [Google Scholar]
- Thapa Suraj Bahadur, Hauff Edvard. Psychological Distress Among Displaced Persons During an Armed Conflict in Nepal. Social Psychiatry and Psychiatric Epidemiology. 2005;40:672–79. doi: 10.1007/s00127-005-0943-9. [DOI] [PubMed] [Google Scholar]
- Tourangeau Roger, Smith Tom W. Asking Sensitive Questions. Public Opinion Quarterly. 1996;60(2):275–304. [Google Scholar]
- Turner R Jay, Avison William R. Gender and Depression: Assessing Exposure and Vulnerability to Life Events in a Chronically Strained Population. Journal of Nervous & Mental Disease. 1989;177(8):443–55. doi: 10.1097/00005053-198908000-00001. [DOI] [PubMed] [Google Scholar]
- Turner R Jay, Lloyd Donald A. Lifetime Traumas and Mental Health: The Significance of Cumulative Adversity. Journal of Health and Social Behavior. 1995;36(4):360–76. [PubMed] [Google Scholar]
- Turner R Jay, Lloyd Donald A. The Stress Process and the Social Distribution of Depression. Journal of Health and Social Behavior. 1999;40(4):374–404. [PubMed] [Google Scholar]
- Turner Heather A, Jay Turner R. Gender, Social Status, and Emotional Reliance. Journal of Health and Social Behavior. 1999;40(4):360–73. [PubMed] [Google Scholar]
- Turner R Jay, Wheaton Blair, Lloyd Donald A. The Epidemiology of Social Stress. American Sociological Review. 1995;60(1):104–25. [Google Scholar]
- Umberson Debra J, Chen Meichu D, House James S, Hopkins Kristine L, Slaten Ellen. Social Relationships and Their Effects on Psychological Well-being: Are Men and Women Really so Different? American Sociological Review. 1996;61(5):836–56. [Google Scholar]
- Umberson Debra, Thomeer Mieke B, Williams Kristi. Family Status and Mental Health: Recent Advances and Future Directions. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the Sociology of Mental Health. 2. New York: Springer; 2012. pp. 405–31. [Google Scholar]
- United Nations Development Programme (UNDP) Human Development Report. Sustainability and Equity: A Better Future for All. 2011 Retrieved July 12, 2012 ( http://www.gm.undp.org/HDR_2011_EN_Complete.pdf)
- Waite Linda J, Gallagher Maggie. The Case for Marriage: Why Married People are Happier, Healthier, and Better Off Financially. New York: Doubleday; 2000. [Google Scholar]
- Wheaton Blair. Life Transitions, Role Histories, and Mental Health. American Sociological Review. 1990;55:209–23. [Google Scholar]
- World Health Organization. WHO-AIMS Report on Mental Health Systems in Nepal. Kathmandu, Nepal: Ministry of Health and Population Nepal; 2006. [Google Scholar]
- Williams Kristi, Kurina Lianne M. The Social Structure, Stress, and Women’s Health. Clinical Obstetrics and Gynecology. 2002;45(4):1099–118. doi: 10.1097/00003081-200212000-00018. [DOI] [PubMed] [Google Scholar]
- Williams Nathalie. Education, Gender, and Migration in the Context of Social Change. Social Science Research. 2009;38(4):883–896. doi: 10.1016/j.ssresearch.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams Nathalie E, Ghimire Dirgha J, Axinn William G, Jennings Elyse A, Pradhan Meeta S. A Micro-Level Event-Centered Approach to Investigating Armed Conflict and Population Responses. Demography. 2012;49:1521–46. doi: 10.1007/s13524-012-0134-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams Stacy L, Williams David R, Stein Dan J, Seedat Soraya, Jackson Pamela B, Moomal Hashim. Multiple Traumatic Events and Psychological Distress: The South Africa Stress and Health Study. Journal of Traumatic Stress. 2007;20(5):845–55. doi: 10.1002/jts.20252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss Erica L, Longhurst James G, Mazure Carolyn M. Childhood Sexual Abuse as a Risk Factor for Depression in Women: Psychosocial and Neurobiological Correlates. American Journal of Psychiatry. 1999;156:816–28. doi: 10.1176/ajp.156.6.816. [DOI] [PubMed] [Google Scholar]
- Zuckerman M. Vulnerability to Psychopathology: A Biosocial Model. Washington DC: American Psychological Association; 1999. [Google Scholar]