Almost a half century ago, Wolff et al wrote,
“During the course of studies of hypertensive patients, including a double blind study, observations were made concerning the diabetogenic activity of benzothiadiazine derivatives. This activity was observed to occur in nonobese patients without a family history of diabetes as well as in obese hypertensives with such a family history. These observations suggest that benzothiadiazines should not be given to young or middle-aged hypertensives in whom there is a lengthy life expectancy and for whom alternative hypotensive therapy is feasible.” [1]
Despite these insightful recommendations, benzothiadiazine derivatives (most often hydrochlorothiazide [HCTZ]) are the first line recommended therapy for hypertension regardless of glycemic status [2]. Epidemiologic data as well as data from randomized controlled trials have associated a new diagnosis of diabetes with hypertension treatment that contains a thiazide diuretic, including chlorthalidone [3,4], HCTZ [5,6] and bendroflumethiazide [7]. There is controversy over the long-term significance of diuretic-induced diabetes [8], primarily related to the benefit of BP lowering vs. the hazard of dysglycemia. Recent data from ALLHAT indicate there is no increased risk for cardiovascular outcomes in those with chlorthalidone induced hyperglycemia or diabetes [9]. However, this may, in fact, be due to lack of power to detect a difference in outcomes in this subset of patients since ALLHAT was not designed a priori to for this comparison [10] and less than a quarter of the patients had a fasting glucose measured during follow-up, with just over three years follow up. In hypertensive patients followed for 15 years, diabetes associated with diuretics is associated with significant CV risk, which is the same as diabetes of other causes [5].
Although half a century ago the mechanism of thiazide-induced glucose elevation was not well understood, the inverse relationship between potassium and glucose levels in which lower potassium is associated with higher glucose is now well documented [11]. There is also an association between hypokalemia and impaired insulin secretion which may partially explain this inverse relationship [12], but this is unlikely to be the only mechanism. Although it has been suggested [11,13] that maintenance of potassium homeostasis by supplementation or concomitant use of an ACE inhibitor or ARB may reduce or prevent the dysglycemia associated with thiazide diuretics, this has not been prospectively evaluated. We have observed that ACE inhibition is protective from diabetes in hypertensive coronary artery disease taking a calcium antagonist but not in those taking a beta blocker plus a thiazide diuretic even at low or moderate dose [14]. Because it is not known if potassium supplementation modifies the increased risk for thiazide induced dysglycemia or diabetes, the National Heart Lung and Blood Institute recently convened a working group to develop a clinical trial specifically designed to shed light on the association and correlation between glucose, potassium and thiazide induced dysglycemia and diabetes [12].
Prediabetes is characterized by either impaired fasting glucose (fasting plasma glucose of 100 mg/dl to 125 mg/dl) or impaired glucose tolerance (2-hour plasma glucose of 140 mg/dl to 199 mg/dl after a 75-g glucose load) [15]. Prediabetes is a component of the metabolic syndrome, which is a constellation of risk factors including abdominal adiposity, hyperglycemia, hypertension, and dyslipidemia [16]. Cardiovascular disease risk in patients with metabolic syndrome is increased 2 to 4-fold compared to those without metabolic syndrome [17,18]. Internists and cardiologist alike should be aware that use of agents that negatively impact glucose homeostasis in hypertensive patients, especially in those who also have prediabetes or metabolic syndrome may hasten diabetes development. This is especially relevant when these patients are relatively young, have a lengthy life expectancy, and perhaps may be most susceptible to the worsening glucose tolerance often associated with thiazide diuretics. These patients are likely to receive antihypertensive therapy for decades, and the implications of thiazide-induced diabetes may not be fully understood in the relatively short-term clinical trial data available to date [19].
Cases In Point
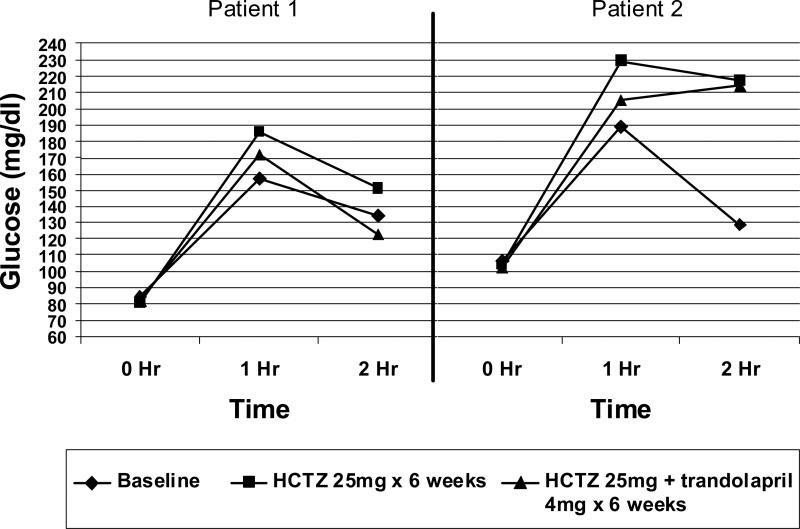
Cases from our hypertension research clinic illustrate the impact of metabolically active drugs in metabolically sensitive patients. Patients 1 (a 62-year-old woman) and 2 (a 53-year-old woman) have hypertension and metabolic syndrome according to criteria outlined by the National Cholesterol Education Panel [16]. Following a 75-g glucose load, fasting glucose, 1-hour and 2-hour glucose tolerance were assessed at baseline, after 6 weeks of treatment with HCTZ daily and after 6 weeks of HCTZ and trandolapril daily (Figure). Potassium and blood pressure values were also assessed at each time point (Table).
Figure.
Glucose levels measured over time of two patients taking hydrochlorothiazide and hydrochlorothiazide plus trandlolapril.
Table.
Blood pressure and potassium measurements of two patients at baseline, after taking HCTZ and HCTZ plus trandolapril.
| Baseline | Week 6 After HCTZ 25mg daily | Week 12 After HCTZ 25mg + Trandolapril 4mg daily | |
|---|---|---|---|
| Patient 1 | |||
| BP (mmHg) | 146/95 | 134/81 | 123/72 |
| Potassium (mEq/dl) | 4.0 | 3.7 | 3.5 |
| Patient 2 | |||
| BP (mmHg) | 148/97 | 136/87 | 125/84 |
| Potassium (mEq/dl) | 4.2 | 3.9 | 3.9 |
At baseline, Patient 1 (Figure, left side) had normal fasting glucose (glucose < 100 mg/dl) while Patient 2 (Figure, right side) had impaired fasting glucose (glucose 100-125 mg/dl), but neither patient had prediabetes (2 hr glucose 140-199 mg/dl). Although both patients achieved considerable blood pressure reduction during the 12 week period, after just 6 weeks of HCTZ (25 mg daily), Patient 1 had a 2-hour glucose diagnostic of prediabetes, while Patient 2 had a 2-hour glucose diagnostic of diabetes (glucose > 200 mg/dl). With continuation of HCTZ (25 mg) and addition of the ACE inhibitor trandolapril (4 mg daily) for an additional 6 weeks, Patient 1 had 2-hour glucose returned to normal (glucose < 139 mg/dl) while in Patient 2, 2-hour glucose remained diagnostic of diabetes. Importantly, in both of these patients, fasting glucose (0 hour value) was not altered from baseline after either the HCTZ alone or in combination with trandolapril, yet there were clear increases in the 2 hour glucose values, suggesting monitoring fasting glucose alone may be insufficient to fully assess the dysglycemic effect of HCTZ. Neither patient had a significant diuretic induced hypokalemia, nor was the observed modest reduction in potassium associated with an increase in fasting glucose.
These 2 cases demonstrate the heightened susceptibility to the dysmetabolic effects of HCTZ in patients with metabolic syndrome over a short period of treatment. Patient 1 would likely progress to diabetes with continued exposure to HCTZ over the long term [5]. Although these data are limited, they suggest further study of the impact of thiazide diuretics in patients with metabolic syndrome is warranted, and until more data are available, caution should be exercised if long-term thiazide diuretic use is planned. A 2 hour oral glucose tolerance test should be used to routinely monitor the dysglycemic effects rather than fasting glucose alone in patients at risk for developing diabetes, including those of Hispanic ethnicity and black race, and those with increased body mass index, left ventricular hypertrophy, history of stroke, and elevated blood pressure [14,20,21].
The prevalence of prediabetes and metabolic syndrome continues to increase, driven largely by obesity and physical inactivity. The cardiovascular consequences associated with these conditions have led to important changes to hypertension treatment guidelines recently. The European Society of Hypertension/European Society of Cardiology no longer endorse thiazide diuretics in hypertensive patients with diabetes [22] and the American Association of Clinical Endocrinologists (AACE) recommends thiazide diuretics only at low dosage and only with adequate potassium replacement in patients with diabetes [23]. Additionally, the American College of Endocrinology and the AACE recommend an annual glucose tolerance test in patients with prediabetes, and even more careful monitoring in patients with prediabetes and metabolic syndrome. The National Institute for Health and Clinical Excellence, together with the British Hypertension Society, recommend use of renin angiotensin system inhibitors as first line in younger patients, with diuretics reserved for the elderly or black patients of any age [24]. While thiazide diuretics remain an inexpensive antihypertensive choice, the long-term costs of diabetes that may result far outweigh the short-term medication cost savings.
Acknowledgments
This work is supported in part by NIH grants 1K23HL086558 and M01 RR000082. No writing assistance was utilized in the production of this manuscript.
Footnotes
Financial & competing interests disclosure
The author has no relevant affiliations or financial involvement with any organization or entity with financial interest in or financial conflict with the subject matter or materials discussed in this manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
References
- 1.Wolff FW, Parmley WW, White K, Okun R. Drug-Induced Diabetes. JAMA. 1963;185:568–574. [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.Barzilay JI, Davis BR, Cutler JA, et al. Fasting glucose levels and incident diabetes mellitus in older nondiabetic adults randomized to receive 3 different classes of antihypertensive treatment: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2006;166:2191–201. doi: 10.1001/archinte.166.20.2191. [DOI] [PubMed] [Google Scholar]
- 4.Davey Smith G, Bracha Y, Svendsen KH, Neaton JD, Haffner SM, Kuller LH. Incidence of type 2 diabetes in the randomized multiple risk factor intervention trial. Ann Intern Med. 2005;142:313–22. doi: 10.7326/0003-4819-142-5-200503010-00006. [DOI] [PubMed] [Google Scholar]
- 5.Verdecchia P, Reboldi G, Angeli F, et al. Adverse prognostic significance of new diabetes in treated hypertensive subjects. Hypertension. 2004;43:963–9. doi: 10.1161/01.HYP.0000125726.92964.ab. [DOI] [PubMed] [Google Scholar]
- 6.Pepine CJ, Cooper-Dehoff RM. Cardiovascular therapies and risk for development of diabetes. J Am Coll Cardiol. 2004;44:509–12. doi: 10.1016/j.jacc.2004.03.071. [DOI] [PubMed] [Google Scholar]
- 7.Gupta AK, Dahlof B, Dobson J, Sever PS, Wedel H, Poulter NR. Determinants of new-onset diabetes among 19,257 hypertensive patients randomized in the Anglo-Scandinavian Cardiac Outcomes Trial--Blood Pressure Lowering Arm and the relative influence of antihypertensive medication. Diabetes Care. 2008;31:982–8. doi: 10.2337/dc07-1768. [DOI] [PubMed] [Google Scholar]
- 8.Cutler JA. Thiazide-associated glucose abnormalities: prognosis, etiology, and prevention: is potassium balance the key? Hypertension. 2006;48:198–200. doi: 10.1161/01.HYP.0000231339.51310.b3. [DOI] [PubMed] [Google Scholar]
- 9.Wright JT, Jr., Harris-Haywood S, Pressel S, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168:207–17. doi: 10.1001/archinternmed.2007.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verdecchia P, Angeli F, Reboldi G. New-onset diabetes, antihypertensive treatment, and outcome. Hypertension. 2007;50:459–60. doi: 10.1161/HYPERTENSIONAHA.107.096966. [DOI] [PubMed] [Google Scholar]
- 11.Zillich AJ, Garg J, Basu S, Bakris GL, Carter BL. Thiazide diuretics, potassium, and the development of diabetes: a quantitative review. Hypertension. 2006;48:219–24. doi: 10.1161/01.HYP.0000231552.10054.aa. [DOI] [PubMed] [Google Scholar]
- 12.Carter BL, Einhorn PT, Brands M, et al. Thiazide-induced dysglycemia: call for research from a working group from the national heart, lung, and blood institute. Hypertension. 2008;52:30–6. doi: 10.1161/HYPERTENSIONAHA.108.114389. [DOI] [PubMed] [Google Scholar]
- 13.Helderman JH, Elahi D, Andersen DK, et al. Prevention of the glucose intolerance of thiazide diuretics by maintenance of body potassium. Diabetes. 1983;32:106–11. doi: 10.2337/diab.32.2.106. [DOI] [PubMed] [Google Scholar]
- 14.Cooper-Dehoff R, Cohen JD, Bakris GL, et al. Predictors of development of diabetes mellitus in patients with coronary artery disease taking antihypertensive medications (findings from the INternational VErapamil SR-Trandolapril STudy [INVEST]). Am J Cardiol. 2006;98:890–4. doi: 10.1016/j.amjcard.2006.04.030. [DOI] [PubMed] [Google Scholar]
- 15.Standards of medical care in diabetes--2007. Diabetes Care. 2007;30(Suppl 1):S4–S41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- 16.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 17.Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 18.Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP. National Cholesterol Education Program versus World Health Organization metabolic syndrome in relation to all-cause and cardiovascular mortality in the San Antonio Heart Study. Circulation. 2004;110:1251–7. doi: 10.1161/01.CIR.0000140762.04598.F9. [DOI] [PubMed] [Google Scholar]
- 19.Black HR, Davis B, Barzilay J, et al. Metabolic and clinical outcomes in nondiabetic individuals with the metabolic syndrome assigned to chlorthalidone, amlodipine, or lisinopril as initial treatment for hypertension: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Diabetes Care. 2008;31:353–60. doi: 10.2337/dc07-1452. [DOI] [PubMed] [Google Scholar]
- 20.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–90. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 21.Lindholm LH, Ibsen H, Borch-Johnsen K, et al. Risk of new-onset diabetes in the Losartan Intervention For Endpoint reduction in hypertension study. J Hypertens. 2002;20:1879–86. doi: 10.1097/00004872-200209000-00035. [DOI] [PubMed] [Google Scholar]
- 22.Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007;28:1462–536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 23.American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of hypertension. Endocr Pract. 2006;12:193–222. [PubMed] [Google Scholar]
- 24.Sever P. New hypertension guidelines from the National Institute for Health and Clinical Excellence and the British Hypertension Society. J Renin Angiotensin Aldosterone Syst. 2006;7:61–3. doi: 10.3317/jraas.2006.011. [DOI] [PubMed] [Google Scholar]