Abstract
Pertussis is a vaccine-preventable disease that generates a large number of cases and hospitalizations. In Catalonia, the vaccination schedule includes three doses of vaccine at 2, 4 and 6 mo and two booster doses at 18 mo and 4–6 y. In 2002, DTPw was replaced by DTPa. The aim of this study was to determine how the vaccination status affects pertussis hospitalizations. Cases were obtained from the epidemiological surveillance system of the Generalitat of Catalonia from 2003 to 2009. Hospitalization, immunization status and type of vaccine received in reported cases were analyzed. OR and 95% confidence intervals (CI) were calculated. To control the effect of age (< 6 mo and ≥ 6 mo) Mantel-Haenszel OR (ORMH) were calculated; statistical significance was established as p < 0.05. During the study period, 1538 cases were reported. Cases below vaccination age (< 2 mo) were excluded. A total of 265 cases were hospitalized: 137 (51.7%) had no vaccine administrated, 104 (39.2%) were correctly vaccinated according to age and 24 (9.1%) were poorly vaccinated. Correct vaccination protected against hospitalization (ORMH: 0.33; 95%CI: 0.23–0.47). Of hospitalized cases, 38 (14.3%) had received DTPw and 91 (34.2%) DTPa. Both vaccines were effective in avoiding hospitalization, and comparison showed no differences (ORMH: 0.73; 95%CI: 0.46–1.14). We highlight the importance of a correct follow-up immunization schedule in reducing the number of cases and hospitalizations.
Keywords: pertussis, hospitalization, surveillance
Introduction
Pertussis is an infectious disease with a high incidence in Catalonia, a region with more than 7.5 million inhabitants in the northeast of Spain. The temporal distribution of pertussis shows epidemic peaks every 3–4 y.1 Pertussis is more frequent and severe in children than in young people and adults.2 In young people and adults, cough ≥ 15 d is the most-frequent single symptom.
Pertussis generates a large number of hospitalized cases that imply substantial health costs. The whole-cell vaccine (DTPw) was introduced in Catalonia in 1965 and the schedule used was 3, 5 and 7 mo. The schedule changed to 2, 4 and 6 mo in 1999 and two new booster doses were included, the first at 18 mo and the second between 4 and 6 y of age. The acellular vaccine (DTPa) became available in 2000 and replaced the DTPw in 2002. The second booster vaccine was replaced by an acellular vaccine with less antigenic charge in 2012.3-5
In other European countries, the vaccination schedule includes an additional dose administered in young people. In the Americas, countries such as the United States, Argentina and Canada include a booster dose for young people, as do Australia and New Zealand.6-10
Pertussis incidence is higher in infants aged < 3 mo. This age group has received only one dose of vaccine and is not protected against pertussis.
The vaccination schedule has undergone various changes in the time of administration and the type of vaccine, and these changes could affect the epidemiology of the disease.
The aim of this study was to evaluate the relationship between pertussis vaccination and pertussis hospitalization.
Results
A total of 1538 cases were reported to the surveillance system, of which 244 cases aged < 2 mo were excluded. Table 1 shows the incidence of pertussis cases by year. There were 271 hospitalized cases and 1023 outpatient cases. The incidence rate of hospitalized cases was 0.54 per 100,000 persons/y. Of the 271 hospitalized cases, 137 (50.6%) were unvaccinated, 24 (8.9%) were poorly vaccinated, 105 (38.7%) correctly vaccinated and in 5 cases the vaccination status was unknown. The incidence rate of outpatient cases was 2.06 per 100,000 persons/y. Of the 1023 outpatient cases, 205 (22.2%) were unvaccinated, 227 (25%) poorly vaccinated, 472 (52.5%) correctly vaccinated and in 119 cases the vaccination status was unknown. Figure 1 shows incidence rates by sex in hospitalized and outpatient cases. The incidence rate of hospitalized cases was the same in males and females: 0.27 per 100,000 persons/y. However, in outpatient cases, the incidence rate in females was 1.14 (566 cases), slightly higher than the 0.92 (457 cases) found in males.
Table 1. Number of pertussis cases and incidence rates by year. Catalonia, 2003–2009.
| Year | Hospitalized cases | Outpatient cases | ||
|---|---|---|---|---|
| Number of cases | Incidence rate* | Number of cases | Incidence rate* | |
| 2003 | 30 | 0.45 | 172 | 2.59 |
| 2004 | 31 | 0.46 | 96 | 1.41 |
| 2005 | 16 | 0.23 | 59 | 0.85 |
| 2006 | 24 | 0.34 | 82 | 1.16 |
| 2007 | 63 | 0.87 | 151 | 2.08 |
| 2008 | 47 | 0.64 | 237 | 3.22 |
| 2009 | 60 | 0.81 | 226 | 3.05 |
*per 100,000 persons
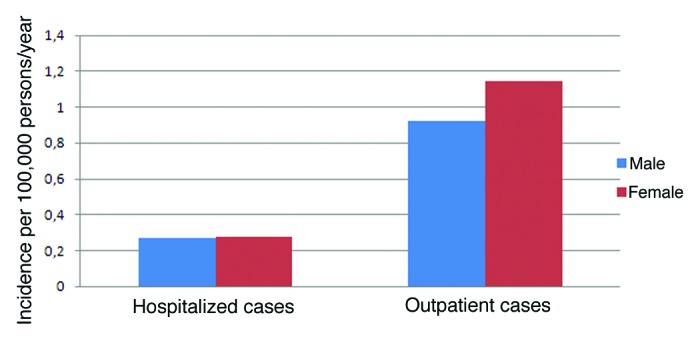
Figure 1. Hospitalized and outpatient cases of pertussis according to sex. Catalonia, 2003–2009.
There were 224 hospitalized cases aged < 1 y. The incidence rate was 39.37 per 100,000 persons/y in hospitalized and 54.66 in outpatient cases aged < 1 y. The incidence rate was 0.78 in hospitalized and 9.68 in outpatient cases aged 1–4 y, 0.46 in hospitalized and 5.22 in outpatient cases aged 5–9 y, 0.40 in hospitalized and 6.82 in outpatient cases aged 10–14 y, and 0.02 in hospitalized and 0.54 in outpatient cases aged > 15 y.
The mean length of stay in hospitalized cases was 7.72 d.
After analyzing the association between vaccination in hospitalized cases and vaccination in correctly vaccinated and unvaccinated cases, the Mantel-Heanszel odds ratios (ORMH) considering two groups (aged < 6 mo and ≥ 6 mo) were 0.33 (95%CI: 0.23–0.47; p < 0.001) (Table 2). The ORMH between cases vaccinated with DTPw and unvaccinated cases was 0.27 (95% CI: 0.17–0.42; p < 0.001). The ORMH between cases vaccinated with DPTa and unvaccinated cases was 0.36 (95% CI: 0.24–0.52; p < 0.001). The ORMH between cases vaccinated with DPTw and with DPTa was 0.73 (95%CI: 0.45–1.17) p = 0.21.
Table 2. Association between vaccination and hospitalization for pertussis.
| Hospitalized cases | Outpatient cases | OR | 95% CI | p value | ORMH | 95% CI | p value | ||
|---|---|---|---|---|---|---|---|---|---|
| Cases < 6 mo | Correctly vaccinated | 83 | 126 | 0.32 | 0.20–0.50 | < 0.001 | 0.33 | 0.23–0.47 | < 0.001 |
| Non vaccinated | 111 | 54 | |||||||
| Cases ≥ 6 mo | Correctly vaccinated | 21 | 346 | 0.35 | 0.18–0.67 | < 0.001 | |||
| Non vaccinated | 26 | 151 |
CI, Confidence Interval; p, level of significance; ORMH, Mantel-Heanszel odds ratio. Catalonia, 2003–2009.
The reporting delay was 15–21 d in 80.4% of hospitalized cases (mean = 19.91 d; SD = 17.71) and in 56.6% of outpatient cases (mean = 29.56 d; SD = 36.19). The difference was statically significant (p < 0.001).
The reporting delay was > 45 d in 3.4% of hospitalized cases and 16% of outpatient cases.
Discussion
The results of this study show that the DTPa and DTPw vaccines are effective in preventing hospitalization due to pertussis. However, the incidence of pertussis has increased in recent years, both in Catalonia and other countries.10-13
The rate of hospitalized cases < 1 y was 39 per 100,000 persons/y, compared with the 196 per 100,000 persons/y found by Somerville et al.14 or the 56 per 100,000 persons/y found by Elliot et al.15
In our study, 38.7% of hospitalized cases were correctly vaccinated, compared with the 66% found in an Australian study,15 although another Australian study in New South Wales found that only 3% of hospitalized cases were correctly vaccinated,16 and a German study found a rate of 4.5%.17 A higher percentage of unvaccinated cases than vaccinated cases may be expected to be found in hospitalized cases, as vaccination should prevent both infection and the severity of cases. Our findings support this expectation.
Of hospitalized cases, 50.8% were unvaccinated, a higher percentage than that of correctly vaccinated cases. Spokes et al.16 found that only 10% of hospitalized cases were unvaccinated, a much lower percentage.
As found by other studies, incidence rate in hospitalized cases aged < 1 y was higher than incidence rate in other age groups,15,18-20 reflecting the fact that clinical symptoms are more severe in infants than in young people and adults, who require fewer hospitalizations. The clinical symptoms and the severity of cases may also justify the differences in the reporting delay between hospitalized and outpatient cases.
We found no differences in the incidence rate of hospitalized and outpatient cases according to sex, although the incidence rate was non-significantly higher in females, similar to other reports including Somerville et al.14 in Canada, O’Brien19 in New Zealand, and Juretzko et al.17 in Germany.
The mean length of hospital stay was 7.72 d compared with 4 d in New Zealand19 and 6 d in Canada.14 A German study in children aged < 16 y found a much longer hospital stay of 14.90 d.17
Our results confirm that vaccination with DTPw or DTPa protects against hospitalization. An Australian study found that vaccination prevented 37 cases of hospitalization15 and that there was no difference in the notification of cases between cellular and acellular vaccines.
Of outpatient cases, 52.5% were correctly vaccinated, suggesting that vaccination confers protection against hospitalization, as found by other studies,15 and it is also supported by the results obtained in the Mantel Heanszel test considering vaccinated and non-vaccinated cases in hospitalized and outpatient cases.
We also found a correlation between diagnostic delay and hospital stay. The mean diagnostic delay was too long for a public health system and should be shortened: laboratory tests should be performed more rapidly to enable earlier prophylaxis. In epidemiologically linked cases laboratory confirmation of the disease is more rapid and the length of hospital stay is shorter than in sporadic cases. The difference in reporting delay in hospitalized and outpatient cases shows improvements are necessary: suspected cases should be tested as rapidly as possible in order to reduce disease transmission.
An Argentinian study has found that the circulating pertussis strain differed from the vaccine strain, and that disease severity increased.21 Spanish and Catalan researchers should be aware of this possibility.
Pertussis in young people and adults could be misdiagnosed and this may have affected our results and resulted in unreported cases.
In conclusion, pertussis vaccination protects against hospitalization. The type of vaccine administered is not a decisive factor in the risk of hospitalization.
Methods
We performed an epidemiological surveillance study of pertussis in Catalonia between 2003 and 2009.
Pertussis cases must be reported to the Department of Public Health of Catalonia. Data on study variables was obtained from the information contained in reported cases surveillance system.22 Data were collected from a specific report form that was sent by physicians to the Department of Public Health. The variables included in the study were age, sex, hospitalization, length of hospital stay, vaccination status, number of doses and type of vaccine received.
The clinical case definition of a suspected case of pertussis was: cough lasting 2 weeks or at least 1 week with either paroxysmal coughing, posttussive vomiting, inspiratory whoop or apnoea without other apparent cause. A confirmed case was defined as a case that met the clinical case definition and was confirmed by laboratory tests or was epidemiologically linked to a laboratory-confirmed case.23
Cases aged < 2 mo were excluded from the study because they were below vaccination age. Cases who had received all vaccination doses corresponding to their age were classified as correctly vaccinated. Cases who had received fewer doses than those corresponding to their age were classified as poorly vaccinated. Cases who had received no dose of vaccine were classified as unvaccinated.
We compared different characteristics between hospitalized and outpatient cases. To control for the age effect in comparing between two heterogenic groups, a Mantel Heanszel test was performed, separating cases into two age groups (< 6 mo and ≥ 6 mo). The 95% confidence intervals (CI) were calculated.
The reporting delay was calculated in days in hospitalized and outpatient cases according to the date of confirmation of the case and the date of symptom onset. We classified the delay in different grades from low to high (15 to 21 d; 22 to 30 d, 31 to 45 d and ≥ 45 d). The Students t test was used to compare the mean reporting delay between hospitalized and outpatient cases. The level of statistical significance was established at p < 0.05. The denominators used for incidence rates came from the population estimated by Idescat (Statistical Institute of Catalonia).23
Acknowledgments
The authors thank the other members of the Pertussis Surveillance Group of Catalonia, which is composed of Inma Crespo, Pedro Plans, Glòria Carmona, Maria Campany, Yolanda Jordan, Irena Barrabeig, César Arias, Mònica Carol, Neus Camps, Miquel Alsedà, Pere Godoy, José Álvarez y Àngela Dominguez. The authors thank the reporting physicians and staff of the epidemiological surveillance units who participated in the notification of cases and in collecting vaccination histories. This study was partially funded by CIBER Epidemiología y Salud Pública (CIBERESP), FEDER and AGAUR (expedient 2009 SGR 42).
Glossary
Abbreviations:
- DTPw
diphtheria, tetanus, whole cell pertussis vaccine
- DTPa
diphtheria, tetanus, acellular pertussis vaccine
- ORMH
Mantel-Heanszel odds ratio
- CI
confidence intervals
Submitted
10/19/12
Accepted
11/02/12
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/23263
References
- 1.Gregory DS. Pertussis: a disease affecting all ages. Am Fam Physician. 2006;74:420–6. [PubMed] [Google Scholar]
- 2.Forsyth K. Pertussis, still a formidable foe. Clin Infect Dis. 2007;45:1487–91. doi: 10.1086/522660. [DOI] [Google Scholar]
- 3.Peña I, Martínez MV. Situación de la Tos Ferina en España. Red Nacional de la Vigilancia Epidemiológica de España. Informe 2009. [Google Scholar]
- 4.Cardeñosa N, Romero M, Quesada M, Oviedo M, Carmona G, Codina G, et al. Pertussis Working Group of Catalonia Is the vaccination coverage established enough to control pertussis, or it is a re-emerging disease? Vaccine. 2009;27:3489–91. doi: 10.1016/j.vaccine.2009.01.046. [DOI] [PubMed] [Google Scholar]
- 5.de Catalunya G. Departament de Sanitat i Seguretat Social. Manual de vacunacions. 3rd ed. Generalitat de Catalunya. Barcelona; 2000. [Google Scholar]
- 6.Forsyth KD, Wirsing von Konig CH, Tan T, Caro J, Plotkin S. Prevention of pertussis: recommendations derived from the second Global Pertussis Initiative roundtable meeting. Vaccine. 2007;25:2634–42. doi: 10.1016/j.vaccine.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Public Health Agency of Canada. Immunization schedules. Canadian Immunization Guide, 7th Ed. 2006. Date Modified: 07 March 2012. http://www.phac-aspc.gc.ca/im/is-cv/index-eng.php#a Accessed 14 September 2012.
- 8.Department of Health and Human Services. Centers of Disease Control and Prevention. May 31, 2012. http://www.cdc.gov/vaccines/schedules/index.html Accessed 18 September 2012.
- 9.Department of Health and Ageing. National immunisation program schedule. Page last modified: 28 July, 2012. http://www.immunise.health.gov.au/ http://immunise.health.gov.au/internet/immunise/publishing.nsf/Content/nips2 Accessed 18 September 2012.
- 10.Ministry of Health. New Zealand Immunisation Schedule. http://www.health.govt.nz/our-work/preventative-health-wellness/immunisation/new-zealand-immunisation-schedule Accessed 14 September 2012.
- 11.Skowronski DM, Janjua NZ, Tsafack EP, Ouakki M, Hoang L, De Serres G. The number needed to vaccinate to prevent infant pertussis hospitalization and death through parent cocoon immunization. Clin Infect Dis. 2012;54:318–27. doi: 10.1093/cid/cir836. [DOI] [PubMed] [Google Scholar]
- 12.Bamberger ES, Srugo I. What is new in pertussis? Eur J Pediatr. 2008;167:133–9. doi: 10.1007/s00431-007-0548-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hellenbrand W, Beier D, Jensen E, Littmann M, Meyer C, Oppermann H, et al. The epidemiology of pertussis in Germany: past and present. BMC Infect Dis. 2009;9:22. doi: 10.1186/1471-2334-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Somerville RL, Grant CC, Grimwood K, Murdoch D, Graham D, Jackson P, et al. Infants hospitalised with pertussis: estimating the true disease burden. J Paediatr Child Health. 2007;43:617–22. doi: 10.1111/j.1440-1754.2007.01154.x. [DOI] [PubMed] [Google Scholar]
- 15.Elliott E, McIntyre P, Ridley G, Morris A, Massie J, McEniery J, et al. National study of infants hospitalized with pertussis in the acellular vaccine era. Pediatr Infect Dis J. 2004;23:246–52. doi: 10.1097/01.inf.0000116023.56344.46. [DOI] [PubMed] [Google Scholar]
- 16.Spokes PJ, Quinn HE, McAnulty JM. Review of the 2008-2009 pertussis epidemic in NSW: notifications and hospitalisations. N S W Public Health Bull. 2010;21:167–73. doi: 10.1071/NB10031. [DOI] [PubMed] [Google Scholar]
- 17.Juretzko P, Fabian-Marx T, Haastert B, Giani G, von Kries R, Wirsing von König CH. Pertussis in Germany: regional differences in management and vaccination status of hospitalized cases. Epidemiol Infect. 2001;127:63–71. doi: 10.1017/S0950268801005593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenberg D, Bamberger E, Ben-Shimol S, Gershtein R, Golan D, Srugo I. Pertussis is under diagnosed in infants hospitalized with lower respiratory tract infection in the pediatric intensive care unit. Med Sci Monit. 2007;13:CR475–80. [PubMed] [Google Scholar]
- 19.O’Brien JA, Caro JJ. Hospitalization for pertussis: profiles and case costs by age. BMC Infect Dis. 2005;5:57. doi: 10.1186/1471-2334-5-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gil A, Oyagüez I, Carrasco P, González A. Hospital admissions for pertussis in Spain, 1995-1998. Vaccine. 2001;19:4791–4. doi: 10.1016/S0264-410X(01)00213-4. [DOI] [PubMed] [Google Scholar]
- 21.Fingermann M, Fernández J, Sisti F, Rodríguez ME, Gatti B, Bottero D, et al. Differences of circulating Bordetella pertussis population in Argentina from the strain used in vaccine production. Vaccine. 2006;24:3513–21. doi: 10.1016/j.vaccine.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 22.Handbook of reporting of notifiable diseases. Government of Catalonia. Department of Public Health. [Catalan] ISSN: 1576-4311. 5th ed: Barcelona, December 2011.Gràfiques Cuscó, S.A.
- 23.Idescat. Statistical Institute of Catalonia. http://www.idescat.cat/cat/poblacio/poblestimacions.html Accessed 14 September 2012.


