Abstract
Main partnerships represent one context in which HIV transmission may occur that has been insufficiently addressed to date for gay and bisexual men, but few studies have focused on the acceptability of couples-based voluntary HIV counseling and testing (CVCT) for male couples in the U.S. Our aim in this study was to explore the acceptability of CVCT among a national U.S. sample of 1532 gay and bisexual men surveyed online using a sexual networking site. We examined the role of demographic (i.e., geographic region, age, relationship status, sexual orientation, race/ethnicity) and HIV risk (i.e., substance use, number of sexual partners, unprotected anal intercourse, sexual role identity, and sexual compulsivity) factors that may be associated with CVCT among the full sample and among partnered men separately. We found that single men expressed higher interest in CVCT than partnered men and that greater age was more strongly associated with lower interest in CVCT for partnered men than for single men. The intersection of sexual orientation and race/ethnicity was also significantly associated with CVCT interest, with a higher proportion of Black bisexual men being interested than White bisexual men. These findings suggest that the uptake of CVCT may be less impacted by HIV risk factors than by demographic factors and that young gay and bisexual men of color–for whom rates of HIV continue to rise–may be the group with the highest levels of interest in CVCT.
Keywords: HIV testing, gay and bisexual men, gay couples, HIV prevention for couples, sexual orientation
INTRODUCTION
Gay, bisexual, and other men who have sex with men (MSM) are one of the only populations for whom HIV prevention efforts have been unable to stabilize the growing trends in national HIV incidence over the last decade (Prejean et al., 2011). MSM are 44 times more likely to contract HIV than other men (Centers for Disease Control and Prevention, 2010), accounting for 61% of all new HIV diagnoses in 2009 (Centers for Disease Control and Prevention, 2011). Estimates indicate that the incidence rate of HIV among young MSM in the U.S. is 2.4% per year, which, if sustained in a cohort of MSM, will result in 40% of them being HIV-positive by age 40 (Ackers et al., 2012; Stall et al., 2009). Taken together, these rates suggest that there remains an urgent need to create innovative, evidence-based, and tailored approaches to HIV prevention among this highly vulnerable group. Although a variety of factors likely underlie the disproportionate burden of HIV faced by MSM, a focus on the role of relationships (compared with casual sex) and factors such as intimacy in the transmission of HIV has primarily been absent from the literature until recently.
Main partnerships represent one context in which HIV transmission may occur that has been insufficiently addressed to date for gay and bisexual men (Sullivan, Salazar, Buchbinder, & Sanchez, 2009). Research has recently shown that same-sex couples may be an important target for HIV intervention, as both intradyadic (within the relationship) and extradyadic (outside of the relationship) sexual behavior play crucial roles in HIV transmission (Sullivan et al., 2009). In the Sullivan et al. study of MSM in five major U.S. cities, for example, the majority of HIV infections were from main sex partners. These high rates may be attributable to increased levels of unprotected anal intercourse (UAI), increased sex acts, more frequent receptive anal sex, and less frequent condom use within both newly established and long-term, non-monogamous main partnerships (Mitchell & Petroll, 2012a, 2012b; Sullivan et al., 2009).
Couples-based voluntary HIV counseling and testing (CVCT) is an intervention through which couples receive pre- and post-test counseling, health education, and test results together (Allen et al., 2003; Painter, 2001). Recent studies suggest that CVCT may ease serostatus disclosure, increase trust and communication between partners, and encourage and promote condom use (Allen et al., 2003; Painter, 2001). CVCT has been shown to be an efficacious HIV prevention strategy and findings suggest that it may be an appropriate and effective method for reducing transmission within male couples (Burton, Darbes, & Operario, 2010; El-Bassel et al., 2010). The World Health Organization (WHO) (2012) has issued guidance for implementing CVCT, which has been used effectively with heterosexual couples in Africa (Allen et al., 1992; Chomba et al., 2008; Farquhar et al., 2004; Guthrie, de Bruyn, & Farquhar, 2007; Painter, 2001), and findings suggest this is a promising strategy for prevention among MSM couples (Coates, 2000; Painter, 2001; Stephenson, Rentsch, & Sullivan, 2012a; Stephenson et al., 2011, 2012b).
Few studies have focused on the acceptability of CVCT for male couples in the U.S. One qualitative study with men across three major cities in the U.S. that was conducted in 2010 found that almost all participants were accepting of and had positive attitudes toward CVCT (Stephenson et al., 2011). Participants reported several potential benefits of CVCT: increased ease when discussing sex risk and safer sex, facilitation of serostatus disclosure within main partnerships, and increased opportunities through counseling to promote intimacy and emotional support within partnerships (Stephenson et al., 2011). Another study of a national sample of Internet-using MSM in the U.S. recruited in 2009 from a social networking site (MySpace) found that 81.5% of participants expressed acceptability of CVCT.Wagenaar et al. (2012) explored demographic and sexual risk characteristics associated with willingness to participate in CVCT and found several meaningful demographic and behavioral factors: race/ethnicity, age, recent relationship status, HIV testing history, and number of male sexual partners were associated with acceptability of CVCT. However, this study was conducted several years ago when CVCT was less well-known and utilized men recruited from a social networking site where individuals may be engaging in sexual risk behavior less often than those recruited from sexual networking sites. Given the role that time and sample composition may have played in the findings of Wagenaar and colleagues, we sought to provide an additional analysis with similar data collected using a different recruitment venue.
Current Study
Our aim in this study was to explore the acceptability of CVCT among a large, national sample of gay and bisexual men surveyed online. These data were gathered from a popular gay male sexual networking site (compared to a social networking site), which may be utilized by men with different levels of sexual activity or different profiles of risk behavior than those recruited from a social networking site. Because few data exist concerning the acceptability of CVCT for male couples in the U.S., we sought to replicate and build upon the existing research. In doing so, we also examined the influence of sexual role identity, sexual compulsivity, and sexual orientation, as well as focus on the interaction of racial/ethnic identity and sexual orientation on the acceptability of CVCT. Further, we sought to examine whether trends among men overall and those currently in a relationship differed. A more in-depth understanding of which subgroups of gay and bisexual men may be most open to receiving CVCT may provide crucial information about the most feasible strategies for implementing efficacy and effectiveness trials as well as efforts to scale up CVCT interventions among male couples.
METHOD
Participants and Procedure
For a 30-day period in the spring of 2012, we advertised on a popular sexual networking website for MSM that we selected because, unlike many similar sites, membership is free of charge and the site attracts a membership that is diverse with regard to race, ethnicity, and age. Those clicking the link were redirected to the secure online survey which began with a welcome page that directed people to a page containing the informed consent information. The online consent form indicated that the survey was an opportunity to participate in an online study and to be simultaneously pre-screened for other studies they might be eligible for. The survey itself had no incentive, though participants were told they could be reimbursed for participation in additional studies. The survey took approximately 10 minutes to complete. All procedures were approved by the City University of New York Institutional Review Board.
The sample included in analyses consisted of 1,532 sexually active gay and bisexual men. We configured the survey to count the number of times it was opened (i.e., how many times people clicked on the banner ad) and from this we estimated that the survey link was clicked on 10,900 times. Approximately one-third (n = 3,334) of the survey clicks resulted in a participant providing informed consent and beginning the survey. From this, participants were excluded for being under the age of 18 (n = 11), providing insufficient data for analysis (n = 1,048), residing outside of the U.S (n = 108), being assigned a non-male gender at birth (n = 4), having a gender identity other than male (n = 15), or reporting no sex with another man in the last 90 days (n = 97). Of the remaining 2,051 men, we removed those for whom CVCT would not apply–HIVpositive men (n = 451, 22.0%) and men in known serodiscordant relationships (n = 30, 1.5%). Because the numbers of men who identified as queer (n = 24) and straight (n = 14) were too small to allow for comparisons, we restricted analyses to only those men who identified as gay or bisexual.
Measures
Our primary aim was to build upon existing research that has examined the role of demographic and behavioral factors in their association with CVCT interest by including previously examined variables. Additionally, because sexual compulsivity and substance use are associated with risk behavior, we sought to explore their potential associations with CVCT interest.
Demographic characteristics
Participants responded to items asking about various demographic characteristics including age, zip code (which was converted to geographic region), relationship status, sexual orientation, and race/ethnicity.
Substance use
Men were asked to report whether or not they had used alcohol, cocaine, crystal meth, ecstasy/MDMA, GHB, ketamine, marijuana, crack, heroin, poppers (nitrite inhalants), or erectile drugs within their lifetime. Those reporting lifetime use were asked whether or not they had used that drug in the past 3 months. Because frequency of use was not assessed and we sought an indicator of more problematic substance use, we excluded those for which use is relatively common (i.e., alcohol, marijuana, and poppers) or those for which men could have a prescription (i.e., erectile drugs). For the purposes of these analyses, we created a dichotomous indicator of whether or not they had used any cocaine, methamphetamine, ecstasy, GHB, ketamine, crack, or heroin in the prior 3 months.
Sexual behavior
Participants were asked to report how they would identify their sexual positioning role for anal sex with response options of “Top (100%),” “Versatile Top,” “Versatile (50/50),” “Versatile Bottom,” and “Versatile (100%).” For the purposes of analyses, all versatile categories were collapsed. Participants were also asked to report the total number of unique male sexual partners they had (1) within a given week, (2) in the prior 30 days, and (3) in the prior 90 days. For the purposes of our analyses, the number of sexual partners from the last 90 days was recoded to indicate whether they had fewer than 1 partner per month on average (1 to 2 partners in 90 days), approximately one per month on average (3 to 5 partners in 90 days), two to four per month on average (6 to 12 partners in 90 days), or more than one per week on average (13 or more partners in 90 days). They then indicated how many of the partners from the last 90 days were anal sex partners. Those reporting anal sex indicated the number of times they had anal sex without a condom (i.e., UAI) with a male partner in the prior 90 days. The number of times participants had engaged in UAI was recoded into a dichotomous indicator of whether they had any UAI in the prior 90 days.
Sexual compulsivity
Participants completed the 10-item Sexual Compulsivity Scale (Kalichman et al., 1994; Kalichman & Rompa, 2001), the most widely used measure of sexual compulsivity among gay and bisexual men (Hook, Hook, Davis, Worthington, & Penberthy, 2010). Participants responded on a Likert-type scale from 1 (not at all like me) to 4 (very much like me), and responses to the 10 items were summed to get an overall score ranging from 10 to 40. The scale had strong reliability in the sample (α = 0.91). A score of 24 or higher has been found to distinguish those with the highest levels of sexual compulsivity (SC) across multiple studies (Benotsch, Kalichman, & Pinkerton, 2001; Cooper, Delmonico, & Burg, 2000; Grov, Parsons, & Bimbi, 2010; Parsons, Bimbi, & Halkitis, 2001; Rendina, Golub, Grov, & Parsons, 2012). As such, this was considered a reliable cutoff for classifying those men who were experiencing high levels of sexual compulsivity symptomology.
Interest in CVCT
Prior to answering questions about their interest in CVCT, participants were presented the following description of what it entails: “Couples-based HIV testing involves going to a doctor’s office or clinic and receiving HIV testing together. This means that you and your partner would receive pre-test counseling, have the tests conducted, and receive the results together in the same room at the same time.” Following the instructions, men who reported being in a relationship were asked, “Would you ever want to be offered couples HIV testing services?” Men who were not in a relationship were asked, “If you should enter a relationship in the future, would you be interested in couples HIV testing services?” Because both questions assessed interest in CVCT rather than intentions to engage in CVCT, we considered them sufficiently similar and combined responses for partnered and non-partnered men into one dichotomous indicator of interest in CVCT for analyses of the full sample. Finally, men who were in a relationship were also asked “Have you ever been tested for HIV with your partner?”
Data Analysis Plan
We began by examining demographic differences in CVCT interest using chi-square tests. We compared the two groups (interested in CVCT vs. not interested) by their ages using independent samples t-tests. We then analyzed all demographic, behavioral, and psychosocial variables in a multivariable logistic regression with interest in CVCT entered as the outcome. In doing so, we examined the role of age, geographic region, relationship status, recent substance use, number of recent sexual partners, recent UAI, sexual role, and SC symptomology as categorical main effects with the exception of age, which was entered as a continuous variable. Because sexual identity may operate differently within different racial and ethnic groups, we also sought to investigate the intersecting role of sexual orientation identity and race/ethnicity. In order to ease interpretation, we created a four-group categorical variable that compared White bisexual men with bisexual men of color, White gay men, and gay men of color (the four-group variable is comparable to entering two dichotomous indicators and their interaction). Finally, because CVCT is specifically an intervention for couples, we ran a second multivariable logistic regression restricted to only those men who reported being partnered at the time of the survey to examine any differences in patterns of prediction.
RESULTS
The demographic distribution of the sample and bivariate associations with interest in CVCT are shown in Table 1. Overall, the sample of 1,533 men was distributed relatively evenly across the four geographic regions of the U.S. with the highest proportion of men living in the Southern U.S.; there were no significant geographic differences with regard to interest in CVCT. Fewer than one-third (29.0%) of men reported being in a relationship and a significantly lower proportion of men in a relationship (61.7%) reported interest in CVCT compared to those who were single (85.9%). A majority (75.5%) of the sample identified as gay and a higher proportion of gay-identified men reported being interested in CVCT (82.5%) compared with bisexual men (68.4%). Nearly two-thirds (63.7%) of the sample reported being White; fewer than half (40.3%) of the sample reported drug use in the prior 3 months; nearly one-third (30.8%) reported more than one male sexual partner per week on average in the prior 3 months; and more than half (58.4%) reported UAI in the prior 3 months. There were no significant associations between interest in CVCT and race/ethnicity, recent drug use, number of recent male sexual partners, and recent UAI. Three quarters (74.2%) of the sample identified their sexual role as versatile and the remaining 25% were split evenly between top- and bottom-identified men, with no significant differences in CVCT interest by sexual role. Slightly more than one-third (34.8%) of the sample was classified as experiencing high levels of SC symptomology, and a smaller proportion (75.2%) of those men reported interest in CVCT compared with those without symptoms of SC (81.0%). Finally, the average age of the sample was 35 years and men who were interested in CVCT were younger, on average.
Table 1.
Demographic and behavioral characteristics of the total sample and comparisons by CVCT interest.
| CVCT Interest |
|||||||
|---|---|---|---|---|---|---|---|
| Full Sample (N = 1532) |
Not Interested (n = 321) |
Interested (n = 1211) |
|||||
| n | % | n | % | n | % | Test Statistic | |
| Geographic region | χ2(3) = 1.27 | ||||||
| Northeast | 320 | 20.9 | 67 | 20.9 | 253 | 20.9 | |
| Midwest | 303 | 19.8 | 70 | 21.8 | 233 | 19.2 | |
| South | 557 | 36.4 | 115 | 35.8 | 442 | 36.5 | |
| West | 352 | 23.0 | 69 | 21.5 | 283 | 23.4 | |
| In a relationship | χ2(1) = 107.62*** | ||||||
| No | 1088 | 71.0 | 153 | 47.7 | 935 | 77.2 | |
| Yes | 444 | 29.0 | 168 | 52.3 | 276 | 22.8 | |
| Sexual orientation | χ2(1) = 34.42*** | ||||||
| Gay | 1156 | 75.5 | 202 | 62.9 | 954 | 78.8 | |
| Bisexual | 376 | 24.5 | 119 | 37.1 | 257 | 21.2 | |
| Race/ethnicity | χ2(3) = 7.76† | ||||||
| Black | 194 | 12.7 | 30 | 9.3 | 164 | 13.5 | |
| Hispanic/Latino | 167 | 10.9 | 30 | 9.3 | 137 | 11.3 | |
| White | 976 | 63.7 | 225 | 70.1 | 751 | 62.0 | |
| Other | 195 | 12.7 | 36 | 11.2 | 159 | 13.1 | |
| Recent drug use (3 mos.) | χ2(1) < 1 | ||||||
| No | 915 | 59.7 | 192 | 59.8 | 723 | 59.7 | |
| Yes | 617 | 40.3 | 129 | 40.2 | 488 | 40.3 | |
| Number of recent male sex partners (3 mos.) | χ2(3) = 2.26 | ||||||
| 1 to 2 (less than one per month) | 295 | 19.3 | 62 | 19.3 | 233 | 19.2 | |
| 3 to 5 (approximately 1 per month) | 360 | 23.5 | 85 | 26.5 | 275 | 22.7 | |
| 6 to 12 (2–4 per month) | 406 | 26.5 | 79 | 24.6 | 327 | 27.0 | |
| 13 or more (more than 1 per week) | 471 | 30.7 | 95 | 29.6 | 376 | 31.0 | |
| Recent UAI with male partner (3 mos.) | χ2(1) < 1 | ||||||
| No | 636 | 41.6 | 130 | 40.5 | 506 | 41.8 | |
| Yes | 896 | 58.4 | 191 | 59.5 | 705 | 58.2 | |
| Sexual role | χ2(2) = 1.60 | ||||||
| Bottom (100%) | 198 | 12.9 | 41 | 12.8 | 157 | 13.0 | |
| Versatile | 1137 | 74.2 | 232 | 72.3 | 905 | 74.7 | |
| Top (100%) | 197 | 12.9 | 48 | 15.0 | 149 | 12.3 | |
| Sexual compulsivity symptomology | χ2(1) = 7.17** | ||||||
| Low | 999 | 65.2 | 189 | 58.9 | 810 | 66.9 | |
| High | 533 | 34.8 | 132 | 41.1 | 401 | 33.1 | |
| M | SD | M | SD | M | SD | ||
| Age | 35.2 | 12.4 | 37.4 | 12.7 | 34.6 | 12.3 | t(1570) = 3.69*** |
Note.
p = .05.
p < .05.
p < .01.
p < .001.
As mentioned previously, we created a four-category variable for the intersection of sexual orientation and race for the multivariable logistic regression shown in Table 2. All variables were entered simultaneously into the model and results were largely consistent with the bivariate analyses, suggesting most variables maintained an independent effect after adjusting for the impact of the others. Table 2 contains the model for the full sample as well as the one conducted with the subsample of men who were partnered. As can be seen in Table 2, results were highly consistent regardless of whether we examined partnered men with or without the single men.
Table 2.
Multivariable logistic regression predicting interest in CVCT.
| Full Sample (N = 1532) |
Partnered Men (n = 444) |
|||||
|---|---|---|---|---|---|---|
| B | AOR | 95% CI | B | AOR | 95% CI | |
| Age | −0.01 | 0.99* | [0.98, 1.00] | −0.03 | 0.97** | [0.96, 0.99] |
| Geographic region | ||||||
| Northeast | Ref. | 1.00 | -- | Ref. | 1.00 | -- |
| Midwest | −0.13 | 0.88 | [0.59, 1.32] | −0.04 | 0.96 | [0.52, 1.79] |
| South | −0.01 | 0.99 | [0.69, 1.42] | 0.17 | 1.19 | [0.69, 2.06] |
| West | 0.07 | 1.07 | [0.72, 1.61] | 0.02 | 1.02 | [0.56, 1.86] |
| In a relationship | ||||||
| No | Ref. | 1.00 | -- | N/A | -- | -- |
| Yes | −1.29 | 0.28*** | [0.21, 0.36] | N/A | -- | -- |
| Sexual orientation × Race | ||||||
| White, bisexual | Ref. | 1.00 | -- | Ref. | 1.00 | -- |
| White, gay | 0.98 | 2.67*** | [1.89, 3.79] | 1.06 | 2.88*** | [1.66, 5.01] |
| Man of color, bisexual | 0.77 | 2.16** | [1.30, 3.60] | 0.82 | 2.27* | [1.04, 4.98] |
| Man of color, gay | 1.10 | 3.01*** | [2.00, 4.53] | 0.99 | 2.70** | [1.44, 5.07] |
| Recent drug use (3 mo.) | ||||||
| No | Ref. | 1.00 | -- | Ref. | 1.00 | -- |
| Yes | −0.01 | 0.99 | [0.75, 1.31] | −0.07 | 0.93 | [0.61, 1.43] |
| No. of recent male sexual partners (3 mos.) | ||||||
| 1 to 2 | Ref. | 1.00 | -- | Ref. | 1.00 | -- |
| 3 to 5 | −0.29 | 0.75 | [0.50, 1.12] | −0.28 | 0.76 | [0.42, 1.36] |
| 6 to 12 | −0.03 | 0.97 | [0.64, 1.46] | −0.24 | 0.79 | [0.44, 1.42] |
| 13 or more | −0.12 | 0.88 | [0.59, 1.33] | −0.60 | 0.55* | [0.31, 0.99] |
| Recent UAI with male (3 mos.) | ||||||
| No | Ref. | 1.00 | -- | Ref. | 1.00 | -- |
| Yes | −0.16 | 0.85 | [0.65, 1.13] | −0.21 | 0.81 | [0.53, 1.24] |
| Sexual role | ||||||
| Versatile | 0.14 | 1.15 | [0.76, 1.72] | 0.04 | 1.04 | [0.52, 2.09] |
| Top | −0.22 | 0.80 | [0.48, 1.34] | −0.09 | 0.92 | [0.38, 2.23] |
| Sexual compulsivity symptomology | ||||||
| Low | Ref. | 1.00 | -- | Ref. | 1.00 | -- |
| High | −0.19 | 0.83 | [0.63, 1.09] | −0.21 | 0.81 | [0.53, 1.24] |
| Model χ2(df) | 156.11*** (16) | 38.87*** (15) | ||||
| Nagelkerke R2 | 0.15 | 0.11 | ||||
| −2 Log Likelihood | 1416.75 | 550.11 | ||||
Note.
p < .05.
p < .01.
p < .001.
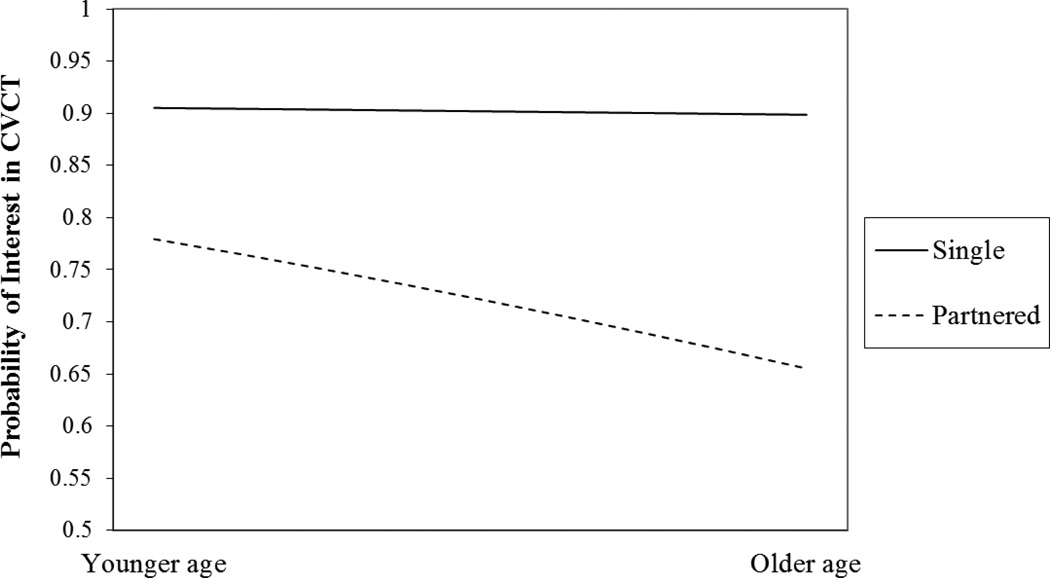
Age, the only continuous variable in the model, remained significant, with a 1% decrease in the odds of expressing interest in CVCT for each additional year of age within the full sample. Put another way, a 10-year increase in age was associated with a 10% decrease in the odds of being interested in CVCT. We tested for and found no evidence of a non-linear association between age and the odds of interest in CVCT. Relationship status was significantly associated with interest in CVCT, with single men having 3.6 times the odds of being interested in CVCT (this is the inverse of the effect reported in Table 2).
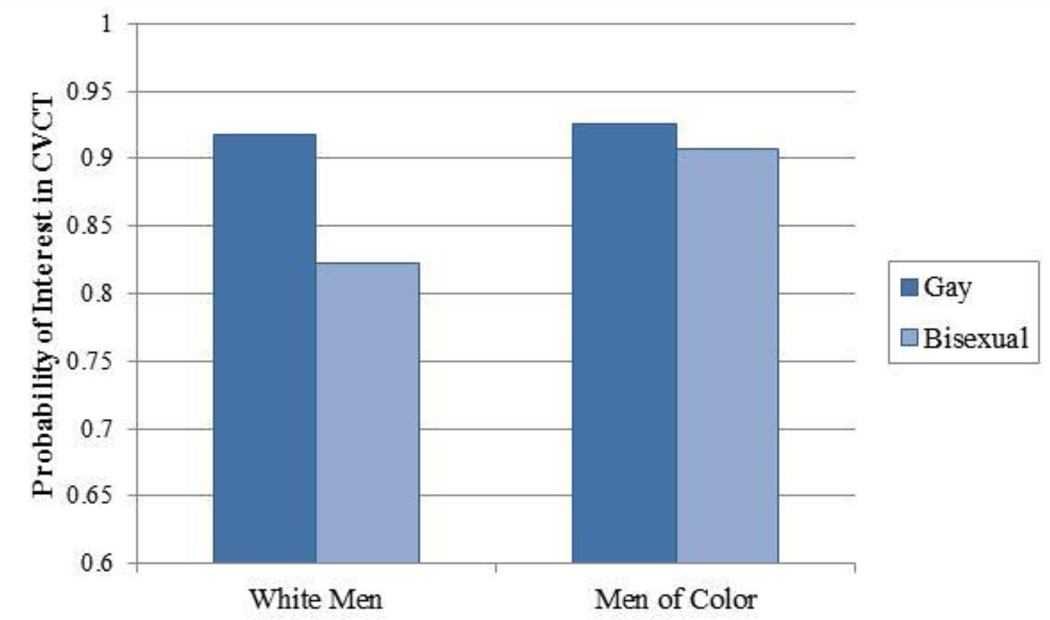
The four-category variable for the intersection of gay identity and race was significant, with White gay men, gay men of color, and bisexual men of color differing significantly from White bisexual men in their interest in CVCT. Using dichotomous indicators for sexual orientation and race and a statistical interaction between the two, we calculated the predicted probabilities for the four groups with regards to interest in CVCT and present them in Fig. 1. As can be seen, both gay-identified men and men of color had a higher probability of being interested in CVCT, but the disparity between gay and bisexual men is more pronounced for White men than for men of color.
Figure 1.
Graphical representation of the intersecting role of gay identity and race predicting interest in CVCT (adjusted based on the multivariable model).
The only variable that was significant in bivariate analyses but did not maintain an independent effect after adjusting for the other variables was sexual compulsivity. In a set of post-hoc chi square tests, we found that sexual compulsivity was significantly associated with several of the other variables (relationship status, sexual orientation identity, recent substance use, number of recent male sexual partners, recent UAI, and sexual role), and thus its independent effect in the multivariable model was likely to be non-significant as a result of its association with several of the significant predictors. None of the other variables associated with HIV risk (recent substance use, number of recent male sexual partners, recent UAI, and sexual role) were significant among the full sample. However, in the model of men in relationships only, we found that men who had one or more partners per week on average had significantly lower odds of being interested in CVCT compared with men who had 1 partner in the prior 3 months.
Because both age and relationship status had significant independent effects in the model, partnered men were significantly older than single men t(5131) = −2.91, p < .01, and the strength of the association between age and interest in CVCT was greater in the model for partnered men only, we conducted a post-hoc examination of a possible interaction between the two variables. The two main effects for age and relationship status became non-significant in a multivariable model with the full sample (not shown) after accounting for the significant interaction between the two, B = −0.02, AOR = 0.98, 95% CI[0.96, 1.00], p < .05. As can be seen in Fig. 1, interest in CVCT was nearly constant across age for men who were single while CVCT interest declined steadily with increased age for men who were in a relationship.
Given that men in a relationship expressed less interest in CVCT than those who were asked to imagine a future relationship, it was worth characterizing this association further. Of the 444 men in relationships, more than one-third (34.5%, n = 153) reported they had been tested with their partners in the past (not via CVCT, specifically). Having been tested with a partner in the past was significantly associated with interest in CVCT, such that 71% (n = 108) of men who had previously tested with a partner expressed interest in CVCT compared with slightly more than half (57.7%, n = 168) of those who had not tested previously with a partner, χ2(1) = 7.05, p = .005. Having been tested before was associated with a 76% increase in the odds of being interested in CVCT in the future, OR = 1.76, 95% CI[1.16, 2.67).
DISCUSSION
Our analyses of a large, national U.S. sample of gay and bisexual men recruited from a sexual networking website revealed that nearly 80% of the men would be interested in receiving CVCT. In both bivariate and multivariable analyses, we found that age, relationship status, sexual orientation, and race/ethnicity were associated with interest in CVCT–younger age, being single, identifying as gay, and being a man of color were all associated with greater interest in CVCT, and that effects were consistent whether partnered men were grouped with single men or examined separately. We found that sexual compulsivity was associated with greater interest in CVCT at the bivariate level, but this effect did not emerge as independent within the multivariable model, suggesting demographic differences in sexual compulsivity may drive the association between sexual compulsivity and interest in CVCT. We also found that the intersection of sexual orientation and race/ethnicity meaningfully influenced interest in CVCT, with White, bisexual men expressing the least interest in CVCT and gay men of color expressing the greatest interest; bisexual men of color and White gay men expressed similar levels of interest in CVCT. Finally, among men in relationships, only two-thirds of partnered men expressed interest in CVCT; among those who expressed interest, half had already received some form of HIV testing with their current partner. We found that men who had one or more sexual partners per week were less interested in CVCT than those who reported only one partner in the prior three months.
The results of this study were largely consistent with another analysis of a national sample of internet-using MSM in the U.S. conducted in early 2009 (Wagenaar et al., 2012). Three years later, we found that nearly an identical proportion of men in our sample would be interested in receiving CVCT. The current study replicated the findings that White gay and bisexual men were less interested in CVCT than men of color and that older men were less interested than younger men. Further, the lower interest among White men was particularly driven by White bisexual men, who constituted the group with the least interest in receiving CVCT. Consistent with the findings of Wagenaar et al., interest in CVCT did not appear to differ by geographic region.
We found that age had a significant independent association with CVCT interest that was consistent withWagenaar et al. (2012), but the main effect for the role of relationship status was opposite than found in their sample. Although their results suggested that being in a relationship was associated with greater interest in CVCT, our results suggested that being single was associated with significantly greater interest in CVCT. However, after examining a potential interaction between age and relationship status in post hoc analyses, we found that both main effects were non-significant but that age and relationship status interacted with each other. Increasing age was associated with declining interest in CVCT for partnered men but was essentially constant for single men. It is unclear whether this finding for age was a result of cohort effects or declining interest in CVCT that occurs as men age, though the interaction suggests that these are more likely to be within-person changes. It is also likely that unmeasured relationship dynamics play a role in CVCT interest. For example, older men may be in relationships that have lasted longer and relationship length may be associated with interest in CVCT–men who have been together briefly may see it as a sign of commitment that they have are not yet ready for, while men who have been together for longer periods of time may view it as an indicator of lack of trust or of broken relationship agreements with regards to outside sexual partners (Stephenson et al., 2011). More research is needed to examine the mechanisms through which age, relationship status, and their intersection work to influence interest in CVCT. Given that partnered men are those who will ultimately be the targets for CVCT, these findings suggest that interventions to increase acceptability among older partnered men and, potentially, men in longer-term relationships, may be warranted.
Inconsistent with the findings of Wagenaar et al. (2012), we found no significant associations between the number of sexual partners and CVCT interest among the full sample, while Wagenaar et al. found that men with higher numbers of partners reported less interest in CVCT. These findings may be purely methodological given that the variable was assessed differently across the two studies–although both samples included only men who reported recent sexual activity, Wagenaar et al. assessed number of partners over the prior 12 months, while we assessed the number in the prior 3 months. More importantly, however, the men in our sample appear to have been more highly sexually active–approximately one-fifth of the men in the Wagenaar et al. sample reported 7 or more partners in the past 12 months, while more than half reported this number in the prior three months in the present study. This is likely a result of the methods of recruitment for the two studies–Wagenaar et al. utilized a social networking site, while we utilized a sexual networking site for the present study. As such, we may have been oversampling the group of men in the Wagenaar et al. study who had the highest level of sexual activity and expressed the least interest in CVCT. Given these differences in samples, it is again worth pointing out that we found no differences in the overall interest in CVCT across the two studies.
When examining the subsample of partnered men in a separate model, we found that those who were most sexually active–having approximately one or more partners per week–had significantly less interest in CVCT than those who reported only one partner in the prior 3 months (and it is worth noting this could have been their main partner). This finding may again highlight the important ways in which relationship dynamics may influence interest and engagement in CVCT. Specifically, these findings may suggest that men who are in nonmonogamous relationships with more frequent outside sex partners may be qualitatively different than those who are in monogamous relationships or non-monogamous relationships with less frequent sexual activity with outside partners. Previous studies have examined different relationship arrangements and their association with sexual practices and satisfaction (Grov, Starks, Rendina, & Parsons, 2012; Parsons, Starks, Gamarel, & Grov, 2012), and the present findings suggest that these groups may differ with regard to monogamy arrangements may also have different levels of interest in CVCT.
Two other findings from the study deserve attention. First, we found that the role of sexual orientation identity and race/ethnicity interacted in their association with CVCT interest, such that both White men and bisexual men expressed less interest in CVCT, with the difference between gay and bisexual men being more pronounced among White men than men of color. Notably, both gay and bisexual men of color had levels of interest that were similar to or exceeded those of White gay men. Second, we found that several demographic characteristics of the sample were independently associated with interest in CVCT, but that none of the indicators of HIV risk that we included were significant–substance use, number of sexual partners, engaging in UAI, and sexual role all had non-significant associations with CVCT even at the bivariate level, and sexual compulsivity was associated at the bivariate level but was not independently associated in the multivariable model.
Taken together, these findings provide several insights for future prevention work utilizing CVCT. First, these results hint at the challenges of engaging in CVCT within the context of a real relationship. Partnered men were less interested in CVCT than single men. While the relatively high level of interest among gay men (single and partnered) supports the acceptability of CVCT within the gay community, the significant difference in interest between currently single and partnered men suggests the importance of understanding how relationship functioning contextualizes the decision to engage in HIV testing together. Further research is needed to better understand how relationship functioning influences partners’ interest and engagement in CVCT. This work would help to identify (1) couples likely to utilize CVCT, (2) couples for who CVCT needs to be specifically tailored to address deficits in relationship functioning, and (3) couples for whom CVCT is unlikely to be acceptable or for whom it may be contraindicated.
Findings related to demographic predictors of interest in CVCT among partnered men (who represent the portion of the sample who could be currently targeted to receive CVCT) provide preliminary data about the utility of such investigations. Those partnered men engaging in the highest levels of HIV sexual risk behavior were less interested in CVCT than those who were engaging in the least such behavior. It is possible that high levels of sexual risk directly reduce interest in CVCT. It is also possible that factors associated with high levels of HIV risk may simultaneously represent barriers to CVCT. For example, research related to goal concordance has found that discordant preferences and compromise motivated by avoidance of conflict have been associated with decreased relationship commitment and satisfaction among gay men (Gere, Schimmack, Pinkus, & Lockwood, 2011; Houts & Horne, 2008; Kurdek, 2007). Low relationship satisfaction has been associated with HIV sexual risk, while high relationship commitment has been associated with the use of dyadic risk reduction strategies i.e., negotiated safety between partners (Davidovich, Wit, & Strobbe, 2006). From the perspective of interdependence theory, engaging in CVCT represents shared action towards a mutual goal. Couples in which one or both members are engaging in large amounts of sexual activity with other partners may find it less desirable to then engage in HIV testing together (Kelley & Thibaut, 1978; Lewis, Gladstone, Schmal, & Darbes, 2006; Rusbult & Van Lange, 2003). The finding that older age was associated with reduced interest in CVCT is significant in light of Sullivan et al.’s (2009) finding that main partner HIV transmission risk as greater for younger men. CVCT messaging may need to be tailored based upon age in order to increase appeal across the lifespan. Such efforts may be useful given that younger men may be partnered with older men and that risk of main partner transmission also increases with relationship duration (which is correlated with age) (Sullivan et al., 2009). This may also suggest developmental differences, whereby younger individuals may view CVCT as a ritual that signifies the seriousness of or commitment within their relationships and acts as an important step in their relationship development that may be viewed as unnecessary or insignificant for older men in relationships.
Finally, the reduced interest among White, bisexual identified individuals suggests that identity has a complex relationship with CVCT interest. This finding highlights the need to examine both individual and relationship factors when studying uptake of CVCT. HIV prevention efforts may benefit from understanding the factors which increase the acceptability of CVCT for both individuals within the couple and in addition to understanding the relationship processes involved in testing successfully together. Perhaps most importantly, these findings indicate that some of the groups at the highest risk for HIV infection, such as young gay and bisexual men of color, appear to also have the highest levels of interest in CVCT, suggesting this may be a particularly acceptable and feasible intervention among those groups.
The results of this study were not without limitations. Although these data were collected nationwide, they were unlikely to be a nationally representative sample of gay and bisexual men. For example, we found that they were more highly sexually active than a sample from a social networking site. Despite being non-representative, the sample may, in fact, constitute one that is at higher risk for HIV as well as easy to reach via the internet for participation in research and prevention efforts. Further, since unlike other sexual networking sites in which MSM are required to pay a membership fee (and which tend to be much less heterogeneous with regard to important demographic characteristics), the site we used attracts a more diverse group of MSM, perhaps due to the lack of a membership fee. For example, studies reporting on MSM frequenting a sexual networking site that does require a fee tend to be overwhelmingly white, well educated, financially well off, and older than the men in our sample (Margolis, Joseph, Belcher, Hirshfield, & Chiasson, 2012; Rosenberger et al., 2011). The outcome variable was a dichotomous indicator of interest in CVCT that may have masked variability that could have been achieved by using a multiple-item scale or by providing participants with Likert-type response options.
Behavioral data on sexual risk were collected using single-item, free-response questions that may be subject to recall bias and may be less valid than other methods. These data were collected as part of a larger survey that was intended to pre-screen potential participants for research studies at our research center. As such, the survey contained items that were primarily for the purpose of assessing potential eligibility. We were unable to include many other variables of interest, including contextual variables about the relationship characteristics of partnered men (e.g., sexual agreements) and additional information regarding current HIV testing patterns. Further research is needed to provide more nuanced analyses of the mechanisms that influence the lower levels of interest in CVCT among partnered men. As with all studies on hypothetical interest in a prevention technique, levels reported in this study may overestimate the proportion of participants who would ultimately agree to engage in the technique upon implementation. Finally, a technical error prevented IP addresses from being recorded and thus we were unable to identify potentially duplicate responses in the data. However, given that there was no incentive for the survey and was posted selectively on a membership-based site, we do not believe that this had a significant impact on the quality of the data.
Conclusions
As rates of HIV infection continue to rise among gay and bisexual men, novel approaches to intervention that acknowledge the contextual factors driving infections are necessary. One such context is transmission within main partnerships, for which CVCT may serve as one potential prevention technique, particularly in combination with other behavioral and biomedical approaches. This study provided the second analysis of a national sample of gay and bisexual men which suggested that CVCT is acceptable and may prove to be highly feasible among gay and bisexual men in the U.S. The uptake of CVCT may be less impacted by HIV risk factors than by demographic factors, suggesting that there may be relatively straightforward groups for whom efforts to increase acceptability of CVCT may be useful. Some demographic subgroups of the HIV epidemic among MSM, such as young gay and bisexual men of color, may constitute groups with the highest levels of interest in CVCT, and future studies are needed to examine the relative acceptability and efficacy within and across different risk groups. Acknowledging the intersecting roles of sexual orientation identity and race/ethnicity may provide additional insight into future attempts to understand acceptability and feasibility of CVCT and other prevention techniques for gay and bisexual men. Finally, future research is needed to better understand the dynamics that occur within main partnerships to determine how factors such as relationship length, quality, and monogamy arrangements are associated with CVCT interest and engagement.
Figure 2.
Graphical representation of the interaction between age and relationship status in predicting interest in CVCT.
ACKNOWLEDGEMENTS
Data for this study were gathered in concert with online recruitment efforts to identify and screen potential participants to enroll in one of the following studies: Pillow Talk (R01-MH087714; PI: Parsons), MiChat (R03-DA031607; PI: Weinberger), Brotha (U01-PS000707 PI: Nanin), and W.I.S.E. (R01-DA029567; PI: Parsons). H. Jonathon Rendina was supported in part by a National Institute of Mental Health Individual Predoctoral Fellowship (F31-MH095622). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to give special thanks for the contributions of Andrea Vial, Anna Johnson, Chris Hietikko, Joshua Guthals, and Ruben Jimenez.
REFERENCES
- Ackers ML, Greenberg AE, Lin CY, Bartholow BN, Goodman AH, Longhi M, Gurwith M. High and persistent HIV seroincidence in men who have sex with men across 47 U.S. cities. PLoS ONE. 2012;7:e34972. doi: 10.1371/journal.pone.0034972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen S, Meinzen-Derr J, Kautzman M, Zulu I, Trask S, Fideli U, Haworth A. Sexual behavior of HIV discordant couples after HIV counseling and testing. AIDS. 2003;17:733–740. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- Allen S, Serufilira A, Bogaerts J, Ven de Perre P, Nsengumuremyi F, Lindan C, Hulley S. Confidential HIV testing and condom promotion in Africa: Impact on HIV and gonorrhea rates. Journal of the American Medical Association. 1992;268:3338–3343. [PubMed] [Google Scholar]
- Benotsch EG, Kalichman SC, Pinkerton SD. Sexual compulsivity in HIVpositive men and women: Prevalence, predictors, and consequences of high-risk behaviors. Sexual Addiction and Compulsivity. 2001;8:83–99. [Google Scholar]
- Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of HIV: Systematic review of the state of evidence. AIDS and Behavior. 2010;14:1–10. doi: 10.1007/s10461-008-9471-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC analysis provides new look at disproportionate impact of HIV and syphilis among U.S. gay and bisexual men. Atlanta: U.S. Department of Health and Human Services; 2010. Retrieved from http://www.cdc.gov/nchhstp/Newsroom/msmpressrelease.html. [Google Scholar]
- Centers for Disease Control and Prevention. HIV surveillance report, 2009. Atlanta: U.S. Department of Health and Human Services; 2011. Retrieved from http://www.cdc.gov/hiv/pdf/statistics_2009_HIV_Surveillance_Report_vol_21.pdf. [Google Scholar]
- Chomba C, Allen S, Kaweka W, Tichacek A, Cox G, Shutes E the Rawanda Zambia HIV Research Group. Evolution of couples' voluntary counseling and testing for HIV in Lusaka, Zambia. Journal of Acquired Immune Deficiency Syndrome. 2008;47:108–115. doi: 10.1097/QAI.0b013e31815b2d67. [DOI] [PubMed] [Google Scholar]
- Coates TJ. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: A randomised trial. Lancet. 2000;356:103–112. [PubMed] [Google Scholar]
- Cooper A, Delmonico DL, Burg R. Cybersex users, abusers, and compulsives: New findings and implications. Sexual Addiction & Compulsivity. 2000;7:5–29. [Google Scholar]
- Davidovich U, Wit J, Strobbe W. Relationship characteristics and risk of HIV infection: Rusbult's investment model and sexual risk behavior of gay men in steady relationships. Journal of Applied Social Psychology. 2006;36:22–40. [Google Scholar]
- El-Bassel N, Gilbert L, Witte S, Wu E, Hunt T, Remien RH. Couple-based HIV prevention in the United States: Advantages, gaps, and future directions. Journal of Acquired Immune Deficiency Syndromes. 2010;55:S98–S101. doi: 10.1097/QAI.0b013e3181fbf407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar C, Kiarie JN, Richardson BA, Kabura M, Francis J, Nduati R, John-Stewart GC. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. Journal of Acquired Immune Deficiency Syndrome. 2004;37:1620–1626. doi: 10.1097/00126334-200412150-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gere J, Schimmack U, Pinkus RT, Lockwood P. The effects of romantic partners' goal congruence on affective well-being. Journal of Research in Personality. 2011;45:549–559. [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual compulsivity and sexual risk in gay and bisexual men. Archives of Sexual Behavior. 2010;39:940–949. doi: 10.1007/s10508-009-9483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Starks TJ, Rendina HJ, Parsons J. Rules about casual sex partners, relationship satisfaction, and HIV risk in partnered gay and bisexual men. Journal of Sex & Marital Therapy. 2012 doi: 10.1080/0092623X.2012.691948. [DOI] [PubMed] [Google Scholar]
- Guthrie BL, de Bruyn G, Farquhar C. HIV-1 discordant couples in sub-Saharan Africa: Explanations and implications for high rates of discordancy. Current HIV Research. 2007;5:416–429. doi: 10.2174/157016207781023992. [DOI] [PubMed] [Google Scholar]
- Hook JN, Hook JP, Davis DE, Worthington EL, Penberthy JK. Measuring sexual addiction and compulsivity: A critical review of instruments. Journal of Sex and Marital Therapy. 2010;36:227–260. doi: 10.1080/00926231003719673. [DOI] [PubMed] [Google Scholar]
- Houts CR, Horne SG. The role of relationship attributions in relationship satisfaction among cohabiting gay men. The Family Journal. 2008;16:240–248. [Google Scholar]
- Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: Scale development and predicting AIDS-risk behavior among homosexually active men. Journal of Personality Assessment. 1994;62:385–397. doi: 10.1207/s15327752jpa6203_1. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. The Sexual Compulsivity Scale: Further development and use with HIV-positive persons. Journal of Personality Assessment. 2001;76:379–395. doi: 10.1207/S15327752JPA7603_02. [DOI] [PubMed] [Google Scholar]
- Kelley HH, Thibaut JW. Interpersonal relations: A theory of interdependence. New York: Wiley; 1978. [Google Scholar]
- Kurdek LA. Avoidance motivation and relationship commitment in heterosexual, gay male, and lesbian partners. Personal Relationships. 2007;14:291–306. [Google Scholar]
- Lewis MA, Gladstone E, Schmal S, Darbes LA. Health-related social control and relationship interdependence among gay couples. Health Education Research. 2006;21:488–500. doi: 10.1093/her/cyh075. [DOI] [PubMed] [Google Scholar]
- Margolis AD, Joseph H, Belcher L, Hirshfield S, Chiasson MA. 'Never testing for HIV' among men who have sex with men recruited from a sexual networking website, United States. AIDS and Behavior. 2012;16:23–29. doi: 10.1007/s10461-011-9883-4. [DOI] [PubMed] [Google Scholar]
- Mitchell JW, Petroll AE. Factors associated with men in HIV-negative gay couples who practiced UAI within and outside of their relationship. AIDS and Behavior. 2012a;17:1329–1337. doi: 10.1007/s10461-012-0255-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, Petroll AE. HIV testing rates and factors associated with recent HIV testing among male couples. Sexually Transmitted Diseases. 2012b;39:379–381. doi: 10.1097/OLQ.0b013e3182479108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Painter TM. Voluntary counseling and testing for couples: a high-leverage intervention for HIV/AIDS prevention in sub-Saharan Africa. Social Science & Medicine. 2001;53:1397–1411. doi: 10.1016/s0277-9536(00)00427-5. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Bimbi DS, Halkitis PN. Sexual compulsivity among gay/bisexual male escorts who advertise on the Internet. Sexual Addiction & Compulsivity. 2001;8:101–112. [Google Scholar]
- Parsons JT, Starks TJ, Gamarel KE, Grov C. Non-monogamy and sexual relationship quality among same-sex male couples. Journal of Family Psychology. 2012;26:669–677. doi: 10.1037/a0029561. [DOI] [PubMed] [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, Lansky A. Estimated HIV incidence in the United States: 2006–2009. PLoS ONE. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina HJ, Golub SA, Grov C, Parsons JT. Stigma and sexual compulsivity in a community-based sample of HIV-positive gay and bisexual men. AIDS and Behavior. 2012;16:741–750. doi: 10.1007/s10461-011-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberger JG, Reece M, Schick V, Herbenick D, Novak DS, Van Der Pol B, Fortenberry JD. Sexual behaviors and situational characteristics of most recent male-partnered sexual event among gay and bisexually identified men in the United States. Journal of Sexual Medicine. 2011;8:3040–3050. doi: 10.1111/j.1743-6109.2011.02438.x. [DOI] [PubMed] [Google Scholar]
- Rusbult CE, Van Lange PAM. Interdependence, interaction, and relationships. Annual Review of Psychology. 2003;54:351–375. doi: 10.1146/annurev.psych.54.101601.145059. [DOI] [PubMed] [Google Scholar]
- Stall R, Duran L, Wisniewski SR, Friedman MS, Marshal MP, McFarland W, Mills TC. Running in place: Implications of HIV incidence estimates among urban men who have sex with men in the United States and other industrialized countries. AIDS and Behavior. 2009;13:615–629. doi: 10.1007/s10461-008-9509-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Rentsch C, Sullivan PS. High levels of acceptability of couples-based HIV testing among MSM in South Africa. AIDS Care. 2012a;24:529–535. doi: 10.1080/09540121.2011.617413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Rentsch C, Sullivan PS, McAdams-Mahmoud A, Jobson G, Struthers H, McIntyre J. Attitudes toward couples-based HIV counseling and testing among MSM in Cape Town, South Africa. AIDS and Behavior. 2012b;17:43–50. doi: 10.1007/s10461-012-0293-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Sullivan PS, Salazar LF, Gratzer B, Allen S, Seelbach E. Attitudes towards couples-based HIV testing among MSM in three US cities. AIDS and Behavior. 2011;15:80–87. doi: 10.1007/s10461-011-9893-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Salazar LF, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- Wagenaar BH, Christiansen-Lindquist L, Khosropour C, Salazar LF, Benbow N, Prachand N, Sullivan PS. Willingness of US men who have sex with men (MSM) to participate in couples HIV voluntary counseling and testing (CVCT) PLoS ONE. 2012;7:e42953. doi: 10.1371/journal.pone.0042953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Guidance on couples HIV testing and counseling including antiretroviral therapy for treatment and prevention in serodiscordant couples. Geneva: World Health Organization HIV/AIDS Programme; 2012. Retrieved from http://www.who.int/hiv/pub/guidelines/9789241501972/en/. [PubMed] [Google Scholar]