Abstract
Subarachnoid hemorrhage (SAH) represents a considerable health problem. To date, limited therapeutic options are available. In order to develop effective therapeutic strategies for SAH, the mechanisms involved in SAH brain damage should be fully explored. Here we review the mechanisms of SAH brain damage induced by the experimental endovascular puncture model. We have included a description of similarities and distinctions between experimental SAH in animals and human SAH pathology. Moreover, several novel treatment options to diminish SAH brain damage are discussed.
SAH is accompanied by cerebral inflammation as demonstrated by an influx of inflammatory cells into the cerebral parenchyma, upregulation of inflammatory transcriptional pathways and increased expression of cytokines and chemokines. Additionally, various cell death pathways including cerebral apoptosis, necrosis, necroptosis and autophagy are involved in neuronal damage caused by SAH.
Treatment strategies aiming at inhibition of inflammatory or cell death pathways demonstrate the importance of these mechanisms for survival after experimental SAH. Moreover, neuroregenerative therapies using stem cells are discussed as a possible strategy to repair the brain after SAH since this therapy may extend the window of treatment considerably. We propose the endovascular puncture model as a suitable animal model which resembles the human pathology of SAH and which could be applied to investigate novel therapeutic therapies to combat this debilitating insult.
Keywords: Cell death, Endovascular puncture, Inflammation, Neuroregeneration, Stem cells, Subarachnoid hemorrhage, Treatment options
Introduction
Subarachnoid hemorrhage (SAH) is a pathological condition in which arterial blood flows into the subarachnoid space of the brain and which is mostly caused by a ruptured aneurysm. SAH occurs at a relatively young age and has an unpredictable onset. In Western society, the incidence of SAH is 6 to 7 per 100,000 persons per year and half of the patients are under the age of 55 [1-4]. SAH is associated with a high mortality rate of 50% [1,4]. In surviving patients the insult has major consequences for quality of life. In 20 to 40% of the patients who survive the first insult, a second phase of brain damage occurs which is characterized by delayed cerebral ischemia (DCI) and is associated with increased morbidity and mortality [5-7]. DCI, also referred to as delayed ischemic neurological deficit, is a poorly understood complication of SAH in patients.
Directly after SAH, an immediate increase in both mean arterial blood pressure (MABP) and intracranial pressure (ICP) is observed. Cerebral blood flow (CBF), oxygen tension, and cerebral perfusion pressure (CPP) decrease dramatically after SAH [8-13]. These hemodynamic changes eventually contribute to initiation of cerebral inflammation and apoptotic and necrotic cell death. Cerebral vasospasm is thought to play an important role in the etiology of DCI. It has been hypothesized that several processes occurring as a result of SAH, like inflammation, oxidative stress and hemoglobin reacting with nitric oxide (NO), initiate vasospasm leading to DCI [14]. However, this hypothesis has been increasingly questioned over the last couple of years, because vasospasm does not necessarily lead to DCI and DCI can occur in the absence of vasospasm [6].
There are only limited therapeutic options available to diminish brain injury after SAH and unfortunately, treatments that are available have a short therapeutic window. In order to design new effective treatment strategies for SAH, the pathophysiology of SAH brain damage should be studied extensively. The latter necessitates application of animal models closely resembling human pathology.
Animal models for SAH
Several animal models of SAH are available, of which the single-hemorrhage model, the double-hemorrhage model and the endovascular puncture model are used most commonly. In the single-hemorrhage model, a standard amount (an average of 300 μl) of fresh syngeneic arterial blood is injected into the cisterna magna [15]. In the double-hemorrhage model, two injections with autologous arterial blood are given, in most cases 48 hours apart [15]. In the endovascular puncture, a suture is placed in the external carotid artery (ECA) and threaded through the internal carotid artery up to the middle cerebral artery (MCA) where the vessel is punctured. The suture is immediately retracted to limit an ischemic period in order to mimic the clinical situation as closely as possible. The endovascular puncture model is mainly performed in rats, although there are a few studies that describe the endovascular puncture model in mice. The single- and double-hemorrhage model is performed in dogs, rabbits, rats and mice. The mortality rate in the single- and double-hemorrhage experimental models is low (0 to 20%) and the models are fairly reproducible because a fixed amount of blood is injected into the subarachnoid space [10]. In contrast, the mortality of the endovascular puncture model is higher (approximately 35 to 50%), as in humans. A larger variation in severity of outcome is also observed, as the extent of the hemorrhage itself is variable after puncture [6,10,12,16,17]. We would like to suggest that the endovascular puncture model resembles human pathology, as an increase in mean arterial blood pressure and intracranial pressure are observed in both humans and animals after SAH. In the endovascular puncture model in rats, magnetic resonance imaging (MRI) showed a modest constriction of blood vessels two days after SAH, which might mimic vasospasms observed in human SAH pathology [18]. In this review, our main focus is on the endovascular puncture experimental model.
Aim of this review
The aim of this review is to give an overview of novel therapeutic approaches to prevent or treat the pathological consequences of SAH. Several other experimental therapies have been described earlier to combat brain injury. This review aims at describing a selection of anti-inflammatory, neuroprotective and neuroregenerative pathways in the endovascular puncture model. We will also focus on diagnostic and mechanistic similarities and distinctions between the endovascular puncture model in animals and the human pathology of SAH.
Current therapies
The few therapies currently available for SAH focus on prevention of re-bleeding and prophylaxis for vasospasm [19-21]. Occlusion of the aneurysm that causes SAH is usually sought surgically by clipping or by endovascular coiling. In 5 to 10% of cases, endovascular coiling is not possible due to morphological characteristics or location of the aneurysm. However, endovascular coiling is minimally invasive and therefore, it is preferred over traditional neurosurgical clipping [20,21]. Hypothermia has been shown to reduce edema formation and intracranial pressure after SAH and could be an important means to control fever in SAH. However, hypothermia has also been associated with shivering in SAH patients which is negatively related to outcome after SAH [22,23]. A more invasive treatment that is sometimes applied is decompressive craniectomy (DC) aimed at reducing intracranial pressure after SAH. However, there is continuing debate about the timing and laterality of DC and on the long-term consequences [24].
Nimodipine, a calcium channel blocker, is used as a prophylaxis for vasospasm and treatment with nimodipine is started for all patients at admission. However, the exact mechanism of the beneficial effect of nimodipine is unknown [21]. In addition, treatment with magnesium sulphate has been associated with a reduction in DCI, leading to an improvement of clinical outcome. However, these positive effects of magnesium sulphate have not been confirmed in all studies [25,26]. The symptomatic treatment of vasospasm consists of triple H therapy (hypertension, hypervolemia, and hemodilution) with the goal of increasing CBF, CPP and to improve blood flow and oxygen delivery to the cerebral circulation. Although triple H therapy improves CBF and CPP, it has not been proven to reduce the incidence of DCI and mortality [19,21].
Cerebral inflammation after SAH and possible therapeutic strategies
Influx of immune cells
Inflammation is invariably associated with brain insults and has been suggested to be a major contributor to brain damage after SAH. Increased levels of cytokines in plasma and cerebrospinal fluid (CSF) have been shown after SAH [27,28]. In rodents, SAH induces a systemic increase in pro-inflammatory cytokines and chemokines [29]. Inflammatory cells like granulocytes and macrophages are attracted to the injured brain by cerebral production of chemoattractants and expression of adhesion molecules like integrins and selectins on endothelial cells, leukocytes, microglia, and neurons [30,31]. In SAH patients, intercellular and vascular adhesion molecules-1 (ICAM-1 and VCAM-1) have been shown to be upregulated in both CSF and serum [32,33].
Moreover, increased blood brain barrier (BBB) permeability after SAH favors influx of peripheral immune cells into the brain [34]. Matrix metalloproteinase 9 (MMP9) has been shown to be increased after SAH in the endovascular puncture model [35]. MMP9 is a collagenase that facilitates transport of immune cells to site of injury by degrading tight junctions and basal membrane proteins of the extracellular matrix (ECM) [36].
Macrophages and neutrophils enter the subarachnoid space early after SAH (within hours) where they activate resident microglia, astrocytes and neurons [37,38]. Neutrophils are primarily engaged in phagocytosis of red blood cells in the subarachnoid space after which they degranulate and die [37]. Neutrophils are also detected in the CSF of SAH patients [39]. Migration to the lesion site and activation of macrophages/microglia seems to be an ongoing inflammatory process after SAH; our data show that active macrophages/microglia can still be detected even up to three weeks post-SAH in the endovascular puncture model (Kooijman, et al., unpublished data) [38,40]. T-cells also enter the damaged area after SAH but only two days after the SAH [38].
Cytokine production
Activated immune cells secrete cytokines, chemokines, and reactive oxygen species (ROS). Several cytokines in the systemic circulation and/or CSF have been reported to increase after SAH in humans [41-43].
Tumor necrosis factor (TNF)-α is one of the first cytokines that increases after SAH in the endovascular puncture model. TNF-α regulates various processes: the expression of other pro-inflammatory cytokines, immune cell function and trafficking, and initiation of cell death [44-46]. In the endovascular puncture model, TNF-α expression has been detected in the cortex after SAH [40,47]. An increase in TNF-α protein has also been demonstrated in plasma and CSF of SAH patients [44-46,48]. Moreover, inhibition of TNF-α via an anti-TNF-α antibody decreases vasospasm and reduces expression of pro-apoptotic proteins in the single-hemorrhage model [49,50]. In line with this, it is interesting to mention that a phase I study for the use of the TNF-α antagonist etanercept in SAH patients has been started [http://clinicaltrials.gov/show/NCT01865630].
Interleukin (IL)-6 is secreted as an acute phase protein by many cell types including macrophages, endothelial cells, and activated microglia [51,52]. Recently, it has been shown that IL-6 also stimulates ROS production in the brain [53]. In the rat endovascular puncture model, IL-6 is expressed early after SAH [47,54]. To the best of our knowledge, no specific IL-6 inhibitor has been used in experimental SAH models. However, the cytokine inhibitor CNI-1493 (semapimod) inhibits IL-6 and decreases vasospasm in an experimental vasospasm model [55]. Therefore, CNI-1493 could be a suitable option to investigate the importance of IL-6 in SAH (see Figure 1).
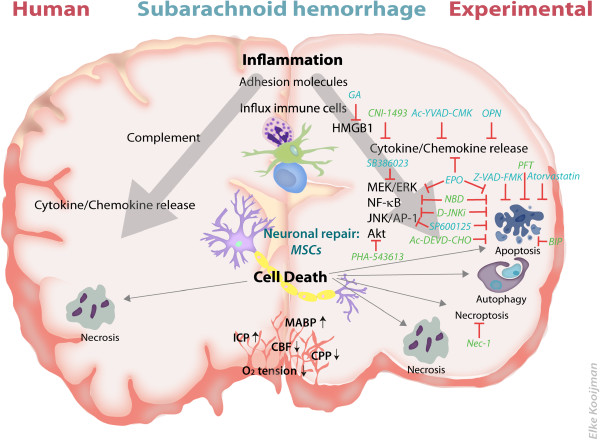
Figure 1.
Therapeutic targets and mechanisms of brain damage in human and experimental subarachnoid hemorrhage (SAH). Schematic overview of known brain damage mechanisms in humans (left side of the figure) and experimental animals models (right side of the figure). Possible therapeutic options which have been explored in the endovascular puncture model are depicted in light blue. Suggested novel therapeutic options strategies are depicted in green. The red lines depict the target of inhibition. From top to bottom: SAH induces inflammation in the brain reflected by increased expression of adhesion molecules, increased influx of immune cells (depicted are neutrophils, macrophages and T-cells), increased activity of complement system, high mobility group box-1 (HMGB-1) expression, increased expression of transcription factors and cytokine/chemokine production. Different forms of neuronal cell death after SAH are observed; that is, apoptosis, autophagy, necroptosis and necrosis. Lower section: physiological factors in the brain which are altered after SAH. Abbreviations: BIP, Bax-inhibiting peptide; CBF, cerebral blood flow; CPP, cerebral perfusion pressure; EPO, erythropoietin; GA, glycyrrhizic acid; ICP, intracranial pressure; MABP, mean arterial blood pressure; MSCs, mesenchymal stem cells; NBD, NEMO binding domain peptide; Nec-1, necrostatin-1; OPN, osteopontin; PFT, pifithrin.
IL-1β has many functions including induction of pro-inflammatory cytokines, attraction of leukocytes to the site of damage and activation of immune cells. There are contradicting results regarding whether IL-1β expression is increased in CSF and plasma of SAH patients; some studies claim no change in IL-1β after SAH [42,56] while others observed that IL-1β is increased five to nine days after SAH [41,57]. In the endovascular puncture model, expression of the precursor- and mature-form of IL-1β are elevated in the brain after SAH [35,54,58]. Greenhalgh et al. (2012) showed that next to IL-1β expression, IL-1α expression is increased in the brain after SAH [59].
The detrimental role of IL-1β in SAH brain damage has been demonstrated by Sozen et al. (2009) who showed that Ac-YVAD-CMK, a caspase-1 inhibitor, reduces mortality after SAH (see Figure 1) [35]. As caspase-1 proteolytically cleaves the precursor form of IL-1β, Ac-YVAD-CMK inhibits IL-1β maturation [35,60].
Molecular signaling pathways
Mitogen activated protein (MAP) kinases are important signaling pathways that are activated by a variety of stress stimuli and are involved in, for example, regulation of cytokine/chemokine expression. Activation of the MAP kinases extracellular signal-regulated kinases (ERK) and p38 have both been reported after experimental SAH [35,54,61,62]. Inhibition of the MEK/ERK pathway by the Raf inhibitor SB386023-b has been shown to reduce expression of MMP9 and pro-inflammatory cytokines IL-1β and IL-6 after SAH [62]. In line with this study, inhibition of the p38 pathway by SB203580 has been shown to reduce vasospasm, reduce TNF-α expression in CSF, reduce brain edema and improve behavior after experimental SAH [60,63].
Cell death mechanisms after SAH and possibilities for neuroprotection
Apoptosis
Apoptosis is the programmed form of cell death characterized by cell shrinkage, nuclear condensation and DNA fragmentation, membrane blebbing and loss of adhesion [64]. During apoptosis, activation of the caspase cascade is a key phenomenon, however, caspase-independent apoptosis can also be operative [65].
There are numerous reports showing activation of the extrinsic (death-receptor activated) and intrinsic (mitochondria-activated) routes of apoptosis after SAH in the endovascular puncture model but their relative contribution is still unclear. Several studies show increased terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) staining, significant increases in caspase-3, caspase-8, cytosolic p53 and cytosolic cytochrome c expression in the brain after SAH in the endovascular puncture model [66,67]. Possibly the severity of SAH directs the predominant use of the intrinsic or extrinsic route. Besides elevated levels of pro-apoptotic markers, DNA fragmentation was also shown to be increased in SAH rats [67,68]. In contrast, Thal et al. (2009) did not observe neuronal cell death after SAH [12].
There are several molecules within the apoptotic cascade that could be targeted for neuroprotection after SAH, for example, active caspases, p53, the mitochondrial membrane and death receptors [69,70]. We will describe a selection of strategies aimed at reducing apoptosis at various levels of the cascade below.
A decrease in apoptotic cell death, including decreased TUNEL staining, caspase-8 and caspase-3 expression after experimental SAH has been detected after pre-treatment with the statin atorvastatin (see Figure 1) [67]. Statins are already Food and Drug Administration (FDA)-approved drugs used by patients to lower cholesterol and are also known to have anti-inflammatory and anti-apoptotic actions [67]. Atorvastatin has been used in the rat endovascular puncture model using oral administration for 15 days prior to the insult. Although promising, only the effects of pre-treatment with atorvastatin have been studied, so it is not clear whether post-SAH treatment with atorvastatin could also lead to neuroprotection. If post-treatment with atorvastatin would not convey protection of cerebral tissue after SAH, the clinical implication would of course be minimal.
A promising target within the apoptotic cascade may be represented by p53, a tumor suppressor protein orchestrating apoptosis at multiple levels. In the nucleus, p53 acts as a transcription factor of pro-apoptotic proteins [71]. Treatment with pifithrin (PFT)-α, an inhibitor of transcriptional activity of p53, resulted in reduction of BBB permeability, decreased neuronal apoptosis and a decreased mortality rate in the endovascular puncture model of SAH [72-74]. More recently, a non-transcriptional role of p53 has been described depending on the association of p53 with mitochondria [75]. We have shown that PFT-μ, a specific small molecule inhibitor of the mitochondrial association of p53 with mitochondria, is potently neuroprotective and has greater neuroprotective potential than PFT-α treatment in a neonatal brain damage model [71]. PFT-μ treatment strongly decreased mitochondrial p53 levels and thereby significantly inhibited mitochondrial damage, caspase-3 activation and apoptotic cell death after brain damage [71]. In contrast however, recent studies have shown that PFT-μ inhibits Heat Shock Protein 70 (HSP70) independently of p53 in tumor cells [76]. HSP70 is expressed after cellular stressors like nutrition deprivation and oxidative stress, and cerebral expression of HSP70 has been shown to be upregulated in the endovascular puncture model from day one to day five after SAH and after neonatal ischemic brain injury [77,78]. Inhibition of HSP70 in leukemic cells from acute myeloid and acute lymphocytic leukemia patients has been shown to increase apoptosis and cell cycle arrest [79,80]. Moreover, Sekihara et al. (2013) have demonstrated that PFT-μ increases the anti-tumor effects of hyperthermia via inhibition of HSP70 by promoting a cell cycle arrest [81]. One explanation for this apparent discrepancy is that PFT-μ may interfere via inhibition of HSP70 and by inducing a cell cycle arrest only in actively cycling tumor cells. Adult neurons are non-dividing cells, an intracellular state which may divert the mechanistic action of PFT-μ to prevention of apoptosis. In conclusion, the use of PFT-μ for SAH brain injury seems promising by its capacity to inhibit neuronal cell death most probably via prevention of p53 accumulation at the mitochondria.
Pro- and anti-apoptotic members of the Bcl-2 family regulate Bax pore formation within the mitochondrial outer membrane, which is an early key step in setting of the apoptotic cascade. Moreover, mitochondria are a source of ROS production under cellular stress conditions. Several studies have shown that ROS production plays a role in acute brain injury and vasospasm after SAH and mitochondrial respiration and activity have been shown to be disrupted after experimental SAH [82]. Interestingly, in several studies using the endovascular puncture model, an increase in mitochondrial Bax expression and other pro-apoptotic Bcl-2 family members, like PUMA, with a concomitant release of cytochrome c from the mitochondria, was observed after SAH indicating that this route is operative during SAH-induced brain injury [83-85]. To the best of our knowledge, to date there are no studies that directly target Bax pore formation or aim at preservation of mitochondrial integrity after SAH, whereas this could be a potent upstream therapeutic target. Wang et al. (2010) have shown in a model of neonatal ischemic brain injury that a Bax-inhibiting peptide (BIP) potently reduced gray- and white matter damage, improved motor and cognitive behavior, reduced mitochondrial membrane permeability and subsequent caspase activation [86]. Together these data indicate that the use of BIP could be a serious option for treating SAH-induced brain injury.
Direct inhibition of caspases is an alternative possibility to inhibit cerebral apoptosis after SAH. Studies by Zhou et al., (2004) and Iseda et al., (2007) have shown that the caspase-3 inhibitor Ac-DEVD-CHO and the broad caspase inhibitor Z-VAD-FMK reduce apoptosis in endothelial cells and thereby exert an anti-vasospastic effect in the blood-injection models of SAH in dogs and rabbits [87,88]. Park et al. (2004) has shown in the endovascular puncture model that treatment with Z-VAD-FMK reduces caspase activity, BBB permeability, vasospasm, and edema formation in the brain after SAH and improves functional outcome in rats [89].
A prominent pro-survival pathway is the serine-threonine kinase Akt. Endo et al. (2006) showed that phosphorylation of Akt was significantly increased in the endovascular puncture model after SAH. Inhibition of Akt signaling increased cell damage and apoptotic cell death after SAH [68]. P-Akt inactivates GSK3β, and P-GSK3β has been shown to be increased after experimental SAH [68]. We propose inhibition of GSK3β as a realistic therapeutic option for SAH. Several GSK3β inhibitors are currently being explored, like lithium and PHA-543613 which is a selective α7nAChR agonist, activating the PI3-K/Akt pathway and thereby inhibiting GSK3β. PHA-543613 has been shown to reduce BBB permeability and increased sensorimotor function after intracerebral hemorrhage [90].
Necrosis, autophagy and necroptosis
Necrosis is another important form of cell death in the brain. Necrosis involves unregulated digestion of cell components, cell swelling, organelle dysfunction and cell lysis, thereby releasing cellular contents like lysosomes in the extracellular environment which may promote inflammation [64,91].
High mobility group box 1 (HMGB1) is a non-histone DNA-binding protein involved in diverse intracellular functions such as inflammation and has been described as being released from necrotic cells [92-94]. Interestingly, an increase in CSF HMGB1 has been shown in SAH patients [46]. In line, Murakami et al. (2011) showed an increase in HMGB1 expression in a rabbit SAH model using blood injection [95]. HMGB1 released during cell death may in its turn activate cerebral inflammation by interacting with the Receptor for Advanced Glycation End Products (RAGE) or by activating Toll like receptors (TLR) like TLR2 and TLR4 on microglia and neurons [96]. Apart from a direct interaction of HMGB1 with its receptors on the cell, the effects of HMGB1 can be potentiated by forming stable complexes with endotoxins, thereby enhancing the potential of HMGB1 to induce a pro-inflammatory milieu. Moreover, HMGB1 has been shown to be capable of enhancing the cleavage of pro-IL-1β to the mature, active form by activating caspase-1 especially in a disease relevant condition such as acidosis [97]. In this respect, it is of interest that a HMGB1 inhibitor, glycyrrhizic acid (GA), decreases inflammation in several models of brain damage which may imply that inhibiting HMGB1 action in SAH might be efficacious to prevent inflammation and subsequent neuronal damage [98].
Autophagy, which involves secretion of damaged organelles by cells such as macrophages/microglia [99] can either initiate cell death or be pro-survival [99]. Several studies showed an early upregulation of autophagy markers after SAH [100-102]. The positive or negative contribution of autophagy to brain damage observed after SAH is still unknown.
Recently, another mechanism of cell death has been described named necroptosis, which is a caspase-independent programmed form of cellular necrosis sharing characteristics of necrosis, apoptosis and autophagy [103]. It has been shown that necroptosis contributes to brain pathologies like traumatic brain injury, intracerebral hemorrhage and neonatal hypoxia-ischemia. Interestingly, in these models of brain injury, it has been shown that necrostatin-1, a potent inhibitor of necroptosis, reduced brain damage, improved behavior, reduced ROS production, reduced inflammation, preserved mitochondrial function, reduced caspase-3 activation and reduced markers of autophagy like LC3-II and Beclin [104-107]. Taken together, targeting necroptosis seems a promising strategy after SAH as it may possibly allow the inhibition of multiple routes of cell death simultaneously.
Molecular targets involved in both inflammation and cell death: possibilities for neuroprotection
JNK/AP-1 pathway
Inflammation and cell death are closely intertwined as inflammation often results in cell death and vice versa. One signaling pathway crucial for regulating both apoptosis and inflammation is the c-Jun N-terminal kinase (JNK)/activating protein-1 (AP-1) pathway. The JNK/AP-1 pathway is activated by a variety of cellular stress stimuli. The AP-1 transcription factor, when activated by JNK, regulates the upregulation of several pro-inflammatory target genes, like several cytokines and chemokines, as well as pro-apoptotic target genes, like Fas [108]. Moreover, JNK has been shown to phosphorylate several key players within the apoptotic cascade, like p53, PARP-1, Bcl-2 and Bcl-xL and Bim, which facilitates the induction of apoptosis.
Phosphorylation of JNK, as a marker of activation of the JNK/AP-1 pathway, is induced in brain tissue in the endovascular puncture model [35]. Treatment with Ac-YVAD-CMK treatment, a caspase-1 inhibitor, reduces JNK phosphorylation, leading to downregulation of the pro-inflammatory response [35]. Inhibition of JNK by SP600125, an ATP-competitive JNK inhibitor, results in neuroprotection measured as a decrease of cell death as shown by TUNEL staining and decreased cleaved caspase-3, reduced edema formation and BBB leakage, reduced MMP9 and improved functional outcome in the endovascular puncture model [109]. Additionally, in the blood injection model of SAH, it has also been shown that SP600125 can reduce caspase-3 activation, vasospasm, infiltration of leukocytes and IL-6 production [110,111].
More recently, a specific small peptide inhibitor of the JNK pathway, D-JNKi, has been shown to be neuroprotective in several brain damage models [112-116]. D-JNKi prevents interaction of JNK with its downstream and upstream targets, like the AP-1 transcription factor and MKK4/7 respectively. Moreover, D-JNKi was shown to strongly inhibit activation of mitochondrial JNK, which was identified as an important first step in setting off the apoptotic cascade [117]. Neuroprotection by D-JNKi in several models of brain injury is strongly associated with inhibition of pro-inflammatory cytokine/chemokine expression, inhibition of apoptotic cell death, reduction of brain injury and improvement of motor and cognitive behavior (see Figure 1) [112-116]. These data together indicate that inhibition of the JNK pathway might lead to inhibition of both inflammatory and cell death pathways, which might greatly enhance the efficacy of treatment.
NF-κB pathway
Nuclear factor-kappa B (NF-κB) is another transcription factor that regulates gene expression involved in inflammation, cell survival and apoptosis. NF-κB can increase pro-apoptotic factors in neurons and glial NF-κB activation induces expression of pro-inflammatory cytokines [118,119]. NF-κB seems to be a key regulator in the formation of cerebral aneurysms, which are probably at the origin of SAH [120,121]. SAH increases NF-κB activation in the brain during SAH in the endovascular puncture model, which is associated with an increased production of several inflammatory mediators [54,61,121]. You et al. (2013) have shown in the double-hemorrhage model of SAH that inhibition of NF-κB by PDTC, a proteasome inhibitor, reduces TNF-α, IL-1β and ICAM mRNA expression after SAH [121]. A more specific NF-κB inhibitor could be TAT-NBD, a small peptide inhibitor of the inhibitory kappa B kinase (IKK)/NF-κB pathway. TAT-NBD has been shown to strongly reduce neonatal brain injury, reduce cytokine/chemokine expression and improve long-term motor and cognitive behavioral outcome [122,123]. Moreover, we have shown previously that TAT-NBD strongly reduced apoptotic cell death, that is, caspase-3 activation and cytochrome c leakage, after ischemic brain injury [122,123].
Of interest, the possible effect of NF-κB inhibition and thereby the reduction of inflammation in SAH has also been shown by Suzuki et al. using recombinant-osteopontin (r-OPN) an endogenous extracellular matrix glycoprotein which is actively secreted after brain injury [61,124]. Besides NF-κB inhibition, OPN acts as a growth factor, increasing neural progenitor cell (NPC) proliferation and differentiation, allowing r-OPN to be a theoretically suitable therapy [125]. Suzuki et al. (2010) showed that r-OPN reduced NF-κB activation and MMP-9 expression in the endovascular puncture model [61]. Furthermore, r-OPN treatment improved the neurological score and decreased BBB permeability after SAH. In general, an increase in permeability of the BBB contributes to inflammation and neuronal damage, since it facilitates the trafficking of inflammatory cells and mediators across the BBB. MMP-9 favors BBB permeability by degrading the ECM. However, although the neurological score was improved early after SAH after r-OPN treatment, there was no significant difference in mortality between vehicle-treated animals and r-OPN-treated animals. Important to note is that besides the role of NF-κB in damaging pathways, NF-κB can also promote survival in neurons by the increase of anti-oxidants and anti-apoptotic molecules [119]. Thereby, NF-κB can have a dual role in brain damage and inhibition of NF-κB could reduce neuronal survival indicating that besides inhibiting inflammation, a more pronounced inhibition of cell death might be necessary to effectively decrease brain damage and mortality [61]. Since the NF-κB pathway is a classic example of a regulatory pathway of both inflammation and cell death, inhibition of this pathway by a specific inhibitor like TAT-NBD might be promising (see Figure 1).
Possible neuroregenerative strategies
An important drawback of neuroprotective interventions is the relatively short therapeutic window. Therefore, therapies to repair the already damaged brain would be an interesting goal for treatment of SAH patients.
Erythropoietin (EPO), a sialoglycoprotein, has recently been suggested as a possible therapeutic option for SAH [126-128]. EPO has been shown to reduce brain injury in various types of cerebral insults [128-132]. EPO enhances neurogenesis as a neuronal growth factor, but EPO can also counteract inflammation and apoptosis [133-137]. With respect to SAH, Grasso et al. (2002) and Cheng et al. (2009) showed that treatment with rhEPO improves neurological outcome and decreases cell death after SAH [138,139]. To our knowledge, rhEPO has not been tested in the endovascular puncture model. Interestingly, Helbok et al. (2012) showed in a pilot study that EPO increases cerebral blood flow and oxygen delivery to the brain after SAH in humans [127]. Especially in SAH patients with a severe lesion, EPO is suggested to have beneficial effects on outcome [127]. These data indicate that EPO might become a safe and realistic option for treatment of patients with SAH, but the robustness of the therapy still has to be proven in a larger study (Figure 1).
Another potential neuroregenerative strategy could be the use of stem cell transplantation. Mesenchymal stem cells (MSCs) are known to interact with many cell types in the brain, like neural stem cells, cerebral endothelial cells, astrocytes and neurons, thereby boosting endogenous neurogenesis, repair and axonal sprouting [140]. In several brain damage models, mortality and lesion size were decreased after MSC transplantation [140-146]. In mice, MSCs can be administered as late as ten days after induction of neonatal brain damage, underpinning the long time-window of MSC transplantation [147]. Another advantage is that the intranasal route can be used for MSC administration allowing a rapid, and effective route of administration [144,147]. Khalili et al. (2012) showed in a SAH model of autologous blood injection that MSC transplantation at 24 hours after SAH improves neurological function [148]. Preliminary experiments in our group indicate that MSC also improve neurological functioning in the endovascular puncture model, suggesting that MSC transplantation may become a promising therapy for SAH with a long time window (Figure 1) [146,147].
It is of importance to note that strategies aiming at inhibition of pro-inflammatory cytokine expression, including those described above, could potentially result in reduced neuroregeneration [149,150]. Synthesis of cytokines and growth factors is necessary for proliferation and differentiation of neural precursor cells (NPC) [149,150]. Moreover, inflammatory cells are responsible for migration of neuronal precursor cells towards the side of damage by the expression of cytokines and chemokines.
Towards clinical application
The studies reviewed here indicate that inflammation, as well as activation of multiple cell death pathways are important contributors to development of SAH brain injury. In this paper we review a hypothesis-driven selection of strategies that could potentially be used to combat SAH brain damage. We have focused on the endovascular puncture model as this animal model closely mimics SAH pathology in humans. The currently known inflammatory responses and cell death mechanisms that we described to be operative in the endovascular model of SAH are to a large extent also operative in other experimental models of SAH.
The actual clinical translation of the therapeutic strategies described in this review will be most effective when the drugs allow administration with a therapeutic window of at least a few hours. Moreover, as brain injury after SAH develops as a result of an interplay of several detrimental pathways, including inflammation and multiple routes of cell death, we suggest that neuroprotective inhibitors that target both inflammation and cell death, like D-JNKi or TAT-NBD, are promising candidates to combat SAH brain injury. When targeting cell death specifically, a strategy targeting the upstream in the apoptotic cascade, for example, PFT-μ, D-JNKi or BIP, would be preferable. These drugs inhibit damage to the mitochondrial outer membrane, thereby preventing activation of the downstream cascade, which is a more realistic option than targeting one specific caspase in the cascade. In this respect, it is important to realize that several forms of cell death might be operative in the SAH injured brain, so the use of necrostatin-1, which has been shown to inhibit multiple cell death pathways might also be a promising candidate.
Finally, we would like to underline the importance of neuroregenerative strategies like intranasal MSC administration to repair cerebral injury induced by SAH, especially when treatment cannot be started within a few hours after the insult. Moreover, regenerative strategies could also be considered as an add-on therapy of neuroprotective strategies for enhancing tissue repair.
Abbreviations
AP-1: Activating protein-1; BBB: Blood brain barrier; BIP: Bax-inhibiting peptide; CBF: Cerebral blood flow; CPP: Cerebral perfusion pressure; CSF: Cerebrospinal fluid; DC: Decompressive craniectomy; DCI: Delayed cerebral ischemia; ECA: External carotid artery; ECM: Extracellular matrix; EPO: Erythropoietin; ERK: Extracellular signal-regulated kinases; FDA: Food and Drug Administration; GA: Glycyrrhizic acid; HMGB1: High mobility group box 1; HSP70: Heat shock protein 70; ICAM-1: Intercellular adhesion molecule-1; ICP: Intracranial pressure; IκB: Inhibitory kappa B; IKK: IκB kinase; IL: Interleukin; JNK: c-Jun N-terminal kinase; MABP: Mean arterial blood pressure; MAP: Mitogen activated protein; MCA: Middle cerebral artery; MMP9: Matrix metalloproteinase 9; MRI: Magnetic resonance imaging; MSC: Mesenchymal stem cell; NBD: NEMO binding domain; NF-κB: Nuclear factor-kappa B; NO: Nitric oxide; NPC: Neural progenitor cell; OPN: Osteopontin; PFT: Pifithrin; r-OPN: recombinant osteopontin; RAGE: Receptor for advanced glycation end products; rhEPO: recombinant human erythropoietin; ROS: Reactive oxygen species; SAH: Subarachnoid hemorrhage; TLR: Toll like receptor; TNF: Tumor necrosis factor; TUNEL: Terminal deoxynucleotidyl transferase dUTP nick end labeling; VCAM-1: Vascular cell adhesion molecule-1.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
EK identified articles, drafted and edited the manuscript and drafted the figure. CHN co-wrote the manuscript and assisted in the planning and editing of the manuscript. CJH proposed the scope of the review and assisted in the planning and editing of the manuscript. CTJV, AK and JK assisted in the planning and editing of the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded in part by the Dirkzwager-Assink foundation and by the Friends of University Medical Center Utrecht foundation.
Contributor Information
Elke Kooijman, Email: e.kooijman-2@umcutrecht.nl.
Cora H Nijboer, Email: c.nijboer@umcutrecht.nl.
Cindy TJ van Velthoven, Email: c.vanvelthoven-2@umcutrecht.nl.
Annemieke Kavelaars, Email: AKavelaars@mdanderson.org.
Jozef Kesecioglu, Email: J.Kesecioglu@umcutrecht.nl.
Cobi J Heijnen, Email: CJHeijnen@mdanderson.org.
References
- Anderson CS. The ACROSS group. Epidemiology of aneurysmal subarachnoid hemorrhage in Australia and New Zealand: incidence and case fatality from the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS) Stroke. 2000;31:1843–1850. doi: 10.1161/01.str.31.8.1843. [DOI] [PubMed] [Google Scholar]
- de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid hemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78:1365–1372. doi: 10.1136/jnnp.2007.117655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrift AG, Dewey HM, Sturm JW, Srikanth VK, Gilligan AK, Gall SL, Macdonell RAL, McNeil JJ, Donnan GA. Incidence of stroke subtypes in the North East Melbourne Stroke Incidence Study (NEMESIS): differences between men and women. Neuroepidemiology. 2009;32:11–18. doi: 10.1159/000170086. [DOI] [PubMed] [Google Scholar]
- Van GJ, Kerr RS, Rinkel GJ. Subarachnoid hemorrhage. Lancet. 2007;369:306–318. doi: 10.1016/S0140-6736(07)60153-6. [DOI] [PubMed] [Google Scholar]
- Al-Tamimi YZ, Orsi NM, Quinn AC, Homer-Vanniasinkam S, Ross SA. A review of delayed ischemic neurologic deficit following aneurysmal subarachnoid hemorrhage: historical overview, current treatment, and pathophysiology. World Neurosurg. 2010;73:654–667. doi: 10.1016/j.wneu.2010.02.005. [DOI] [PubMed] [Google Scholar]
- Dankbaar JW, Rijsdijk M, Van DSI, Velthuis BK, Wermer MJ, Rinkel GJ. Relationship between vasospasm, cerebral perfusion, and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neuroradiology. 2009;51:813–819. doi: 10.1007/s00234-009-0575-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laskowitz DT, Kolls BJ. Neuroprotection in subarachnoid hemorrhage. Stroke. 2010;41:S79–S84. doi: 10.1161/STROKEAHA.110.595090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bederson JB, Levy AL, Ding WH, Kahn R, DiPerna CA, Jenkins AL III, Vallabhajosyula P. Acute vasoconstriction after subarachnoid hemorrhage. Neurosurgery. 1998;42:352–360. doi: 10.1097/00006123-199802000-00091. [DOI] [PubMed] [Google Scholar]
- Critchley GR, Bell BA. Acute cerebral tissue oxygenation changes following experimental subarachnoid hemorrhage. Neurol Res. 2003;25:451–456. doi: 10.1179/016164103101201841. [DOI] [PubMed] [Google Scholar]
- Prunell GF, Mathiesen T, Diemer NH, Svendgaard NA. Experimental subarachnoid hemorrhage: subarachnoid blood volume, mortality rate, neuronal death, cerebral blood flow, and perfusion pressure in three different rat models. Neurosurgery. 2003;52:165–175. doi: 10.1097/00006123-200301000-00022. [DOI] [PubMed] [Google Scholar]
- Prunell GF, Mathiesen T, Svendgaard NA. Experimental subarachnoid hemorrhage: cerebral blood flow and brain metabolism during the acute phase in three different models in the rat. Neurosurgery. 2004;54:426–436. doi: 10.1227/01.NEU.0000103670.09687.7A. [DOI] [PubMed] [Google Scholar]
- Thal SC, Sporer S, Klopotowski M, Thal SE, Woitzik J, Schmid-Elsaesser R, Plesnila N, Zausinger S. Brain edema formation and neurological impairment after subarachnoid hemorrhage in rats. J Neurosurg. 2009;111:988–994. doi: 10.3171/2009.3.JNS08412. [DOI] [PubMed] [Google Scholar]
- Westermaier T, Jauss A, Eriskat J, Kunze E, Roosen K. Time-course of cerebral perfusion and tissue oxygenation in the first six hours after experimental subarachnoid hemorrhage in rats. J Cereb Blood Flow Metab. 2009;29:771–779. doi: 10.1038/jcbfm.2008.169. [DOI] [PubMed] [Google Scholar]
- Pluta RM, Hansen-Schwartz J, Dreier J, Vajkoczy P, Macdonald RL, Nishizawa S, Kasuya H, Wellman G, Keller E, Zauner A. et al. Cerebral vasospasm following subarachnoid hemorrhage: time for a new world of thought. Neurol Res. 2009;31:151–158. doi: 10.1179/174313209X393564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marbacher S, Fandino J, Kitchen ND. Standard intracranial in vivo animal models of delayed cerebral vasospasm. Br J Neurosurg. 2010;24:415–434. doi: 10.3109/02688691003746274. [DOI] [PubMed] [Google Scholar]
- Gules I, Satoh M, Clower BR, Nanda A, Zhang JH. Comparison of three rat models of cerebral vasospasm. Am J Physiol Heart Circ Physiol. 2002;283:H2551–H2559. doi: 10.1152/ajpheart.00616.2002. [DOI] [PubMed] [Google Scholar]
- Ostrowski RP, Colohan ART, Zhang JH. Mechanisms of hyperbaric oxygen-induced neuroprotection in a rat model of subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2005;25:554–571. doi: 10.1038/sj.jcbfm.9600048. [DOI] [PubMed] [Google Scholar]
- van den Bergh WM, Schepers J, Veldhuis WB, Nicolay K, Tulleken CA, Rinkel GJ. Magnetic resonance imaging in experimental subarachnoid hemorrhage. Acta Neurochir (Wien) 2005;147:977–983. doi: 10.1007/s00701-005-0539-x. [DOI] [PubMed] [Google Scholar]
- Dankbaar JW, Slooter AJ, Rinkel GJ, Schaaf IC. Effect of different components of triple-H therapy on cerebral perfusion in patients with aneurysmal subarachnoid hemorrhage: a systematic review. Crit Care. 2010;14:R23. doi: 10.1186/cc8886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, Shi X, Tang Y, Peng Y. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke. 2013;44:29–37. doi: 10.1161/STROKEAHA.112.663559. [DOI] [PubMed] [Google Scholar]
- Priebe HJ. Aneurysmal subarachnoid hemorrhage and the anesthetist. Br J Anaesth. 2007;99:102–118. doi: 10.1093/bja/aem119. [DOI] [PubMed] [Google Scholar]
- Linares G, Mayer SA. Hypothermia for the treatment of ischemic and hemorrhagic stroke. Crit Care Med. 2009;37:S243–S249. doi: 10.1097/CCM.0b013e3181aa5de1. [DOI] [PubMed] [Google Scholar]
- Scaravilli V, Tinchero G, Citerio G. Fever management in SAH. Neurocrit Care. 2011;15:287–294. doi: 10.1007/s12028-011-9588-6. [DOI] [PubMed] [Google Scholar]
- Schirmer CM, Ackil AA Jr, Malek AM. Decompressive Craniectomy. Neurocrit Care. 2008;8:456–470. doi: 10.1007/s12028-008-9082-y. [DOI] [PubMed] [Google Scholar]
- Lee Y, Zuckerman SL, Mocco J. Current controversies in the prediction, diagnosis, and management of cerebral vasospasm: where do we stand? Neurol Res Int. 2013;2013:373458. doi: 10.1155/2013/373458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong GK, Poon WS. Magnesium sulphate for aneurysmal subarachnoid hemorrhage: why, how, and current controversy. Acta Neurochir Suppl. 2013;115:45–48. doi: 10.1007/978-3-7091-1192-5_10. [DOI] [PubMed] [Google Scholar]
- Fassbender K, Hodapp B, Rossol S, Bertsch T, Schmeck J, Schutt S, Fritzinger M, Horn P, Vajkoczy P, Kreisel S. et al. Inflammatory cytokines in subarachnoid hemorrhage: association with abnormal blood flow velocities in basal cerebral arteries. J Neurol Neurosurg Psychiatry. 2001;70:534–537. doi: 10.1136/jnnp.70.4.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naredi S, Lambert G, Friberg P, Zall S, Eden E, Rydenhag B, Tylman M, Bengtsson A. Sympathetic activation and inflammatory response in patients with subarachnoid hemorrhage. Intensive Care Med. 2006;32:1955–1961. doi: 10.1007/s00134-006-0408-y. [DOI] [PubMed] [Google Scholar]
- Yoshimoto Y, Tanaka Y, Hoya K. Acute systemic inflammatory response syndrome in subarachnoid hemorrhage. Stroke. 2001;32:1989–1993. doi: 10.1161/hs0901.095646. [DOI] [PubMed] [Google Scholar]
- Lee SJ, Benveniste EN. Adhesion molecule expression and regulation on cells of the central nervous system. J Neuroimmunol. 1999;98:77–88. doi: 10.1016/S0165-5728(99)00084-3. [DOI] [PubMed] [Google Scholar]
- Sercombe R, Dinh YR, Gomis P. Cerebrovascular inflammation following subarachnoid hemorrhage. Jpn J Pharmacol. 2002;88:227–249. doi: 10.1254/jjp.88.227. [DOI] [PubMed] [Google Scholar]
- Rothoerl RD, Schebesch KM, Kubitza M, Woertgen C, Brawanski A, Pina AL. ICAM-1 and VCAM-1 expression following aneurysmal subarachnoid hemorrhage and their possible role in the pathophysiology of subsequent ischemic deficits. Cerebrovasc Dis. 2006;22:143–149. doi: 10.1159/000093243. [DOI] [PubMed] [Google Scholar]
- Xie X, Wu X, Cui J, Li H, Yan X. Increase ICAM-1 and LFA-1 expression by cerebrospinal fluid of subarachnoid hemorrhage patients: involvement of TNF-α. Brain Res. 2013;1512:89–96. doi: 10.1016/j.brainres.2013.03.041. [DOI] [PubMed] [Google Scholar]
- Cahill J, Zhang JH. Subarachnoid hemorrhage: is it time for a new direction? Stroke. 2009;40:S86–S87. doi: 10.1161/STROKEAHA.108.533315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sozen T, Tsuchiyama R, Hasegawa Y, Suzuki H, Jadhav V, Nishizawa S, Zhang JH. Role of interleukin-1β in early brain injury after subarachnoid hemorrhage in mice. Stroke. 2009;40:2519–2525. doi: 10.1161/STROKEAHA.109.549592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamashita T, Abe K. Therapeutic approaches to vascular protection in ischemic stroke. Acta Med Okayama. 2011;65:219–223. doi: 10.18926/AMO/46846. [DOI] [PubMed] [Google Scholar]
- Chaichana KL, Pradilla G, Huang J, Tamargo RJ. Role of inflammation (leukocyte-endothelial cell interactions) in vasospasm after subarachnoid hemorrhage. World Neurosurg. 2010;73:22–41. doi: 10.1016/j.surneu.2009.05.027. [DOI] [PubMed] [Google Scholar]
- Kubota T, Handa Y, Tsuchida A, Kaneko M, Kobayashi H, Kubota T. The kinetics of lymphocyte subsets and macrophages in subarachnoid space after subarachnoid hemorrhage in rats. Stroke. 1993;24:1993–2000. doi: 10.1161/01.STR.24.12.1993. [DOI] [PubMed] [Google Scholar]
- Provencio J, Fu X, Siu A, Rasmussen P, Hazen S, Ransohoff R. CSF neutrophils are implicated in the development of vasospasm in subarachnoid hemorrhage. Neurocrit Care. 2010;12:244–251. doi: 10.1007/s12028-009-9308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simard JM, Geng Z, Woo SK, Ivanova S, Tosun C, Melnichenko L, Gerzanich V. Glibenclamide reduces inflammation, vasogenic edema, and caspase-3 activation after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2009;29:317–330. doi: 10.1038/jcbfm.2008.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendryk S, Jarzab B, Josko J. Increase of the IL-1 beta and IL-6 levels in CSF in patients with vasospasm following aneurysmal SAH. Neuro Endocrinol Lett. 2004;25:141–147. [PubMed] [Google Scholar]
- Osuka K, Suzuki Y, Tanazawa T, Hattori K, Yamamoto N, Takayasu M, Shibuya M, Yoshida J. Interleukin-6 and development of vasospasm after subarachnoid hemorrhage. Acta Neurochir. 1998;140:943–951. doi: 10.1007/s007010050197. [DOI] [PubMed] [Google Scholar]
- Sarrafzadeh A, Schlenk F, Gericke C, Vajkoczy P. Relevance of cerebral interleukin-6 after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2010;13:339–346. doi: 10.1007/s12028-010-9432-4. [DOI] [PubMed] [Google Scholar]
- Magnoni S, Stocchetti N, Colombo G, Carlin A, Colombo A, Lipton JM, Catania A. α-melanocyte-stimulating hormone is decreased in plasma of patients with acute brain injury. J Neurotrauma. 2003;20:251–260. doi: 10.1089/089771503321532833. [DOI] [PubMed] [Google Scholar]
- Mathiesen T, Edner G, Ulfarsson E, Andersson B. Cerebrospinal fluid interleukin-1 receptor antagonist and tumor necrosis factor α following subarachnoid hemorrhage. J Neurosurg. 1997;87:215–220. doi: 10.3171/jns.1997.87.2.0215. [DOI] [PubMed] [Google Scholar]
- Nakahara T, Tsuruta R, Kaneko T, Yamashita S, Fujita M, Kasaoka S, Hashiguchi T, Suzuki M, Maruyama I, Maekawa T. High-mobility group box 1 protein in CSF of patients with subarachnoid hemorrhage. Neurocrit Care. 2009;11:362–368. doi: 10.1007/s12028-009-9276-y. [DOI] [PubMed] [Google Scholar]
- Prunell GF, Svendgaard NA, Alkass K, Mathiesen T. Inflammation in the brain after experimental subarachnoid hemorrhage. Neurosurgery. 2005;56:1082–1092. [PubMed] [Google Scholar]
- Chou SH, Feske SK, Atherton J, Konigsberg RG, De Jager PL, Du R, Ogilvy CS, Lo EH, Ning M. Early elevation of serum tumor necrosis factor-alpha is associated with poor outcome in subarachnoid hemorrhage. J Investig Med. 2012;60:1054–1058. doi: 10.231/JIM.0b013e3182686932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Y, Liu DW, Han XY, Dong YN, Gao J, Du B, Meng L, Shi JG. Neuroprotective effects of anti-tumor necrosis factor-alpha antibody on apoptosis following subarachnoid hemorrhage in a rat model. J Clin Neurosci. 2012;19:866–872. doi: 10.1016/j.jocn.2011.08.038. [DOI] [PubMed] [Google Scholar]
- Vecchione C, Frati A, Di Pardo A, Cifelli G, Carnevale D, Gentile MT, Carangi R, Landolfi A, Carullo P, Bettarini U. et al. Tumor necrosis factor-α mediates hemolysis-induced vasoconstriction and the cerebral vasospasm evoked by subarachnoid hemorrhage. Hypertension. 2009;54:150–156. doi: 10.1161/HYPERTENSIONAHA.108.128124. [DOI] [PubMed] [Google Scholar]
- Seki S, Nakashima H, Nakashima M, Kinoshita M. Antitumor immunity produced by the liver Kupffer cells, NK cells, NKT cells, and CD8 CD122 T cells. Clin Dev Immunol. 2011;2011:868345. doi: 10.1155/2011/868345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voloboueva LA, Giffard RG. Inflammation, mitochondria, and the inhibition of adult neurogenesis. J Neurosci Res. 2011;89:1989–1996. doi: 10.1002/jnr.22768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrens MM, Ali SS, Dugan LL. Interleukin-6 mediates the increase in NADPH-oxidase in the ketamine model of schizophrenia. J Neurosci. 2008;28:13957–13966. doi: 10.1523/JNEUROSCI.4457-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakade C, King MD, Laird MD, Alleyne CH Jr, Dhandapani KM. Curcumin attenuates vascular inflammation and cerebral vasospasm after subarachnoid hemorrhage in mice. Antioxid Redox Signal. 2009;11:35–45. doi: 10.1089/ars.2008.2056. [DOI] [PubMed] [Google Scholar]
- Bowman G, Bonneau R, Chinchilli V, Tracey K, Cockroft K. A novel inhibitor of inflammatory cytokine production (CNI-1493) reduces rodent post-hemorrhagic vasospasm. Neurocrit Care. 2006;5:222–229. doi: 10.1385/NCC:5:3:222. [DOI] [PubMed] [Google Scholar]
- Kikuchi T, Okuda Y, Kaito N, Abe T. Cytokine production in cerebrospinal fluid after subarachnoid hemorrhage. Neurol Res. 1995;17:106–108. doi: 10.1080/01616412.1995.11740296. [DOI] [PubMed] [Google Scholar]
- Hirashima Y, Nakamura S, Endo S, Kuwayama N, Naruse Y, Takaku A. Elevation of platelet activating factor, inflammatory cytokines, and coagulation factors in the internal jugular vein of patients with subarachnoid hemorrhage. Neurochem Res. 1997;22:1249–1255. doi: 10.1023/A:1021985030331. [DOI] [PubMed] [Google Scholar]
- Sugawara T, Jadhav V, Ayer R, Chen W, Suzuki H, Zhang JH. Thrombin inhibition by argatroban ameliorates early brain injury and improves neurological outcomes after experimental subarachnoid hemorrhage in rats. Stroke. 2009;40:1530–1532. doi: 10.1161/STROKEAHA.108.531699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh AD, Brough D, Robinson EM, Girard S, Rothwell NJ, Allan SM. Interleukin-1 receptor antagonist is beneficial after subarachnoid hemorrhage in rat by blocking hem-driven inflammatory pathology. Dis Model Mech. 2012;5:823–833. doi: 10.1242/dmm.008557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, Ma Q, Krafft PR, Hu Q, Rolland W II, Sherchan P, Zhang J, Tang J, Zhang JH. P2X7R/cryopyrin inflammasome axis inhibition reduces neuroinflammation after SAH. Neurobiol Dis. 2013;58:296–307. doi: 10.1016/j.nbd.2013.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki H, Ayer R, Sugawara T, Chen W, Sozen T, Hasegawa Y, Kanamaru K, Zhang JH. Protective effects of recombinant osteopontin on early brain injury after subarachnoid hemorrhage in rats. Crit Care Med. 2010;38:612–618. doi: 10.1097/CCM.0b013e3181c027ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddahi A, Ansar S, Chen Q, Edvinsson L. Blockade of the MEK/ERK pathway with a raf inhibitor prevents activation of pro-inflammatory mediators in cerebral arteries and reduction in cerebral blood flow after subarachnoid hemorrhage in a rat model. J Cereb Blood Flow Metab. 2011;31:144–154. doi: 10.1038/jcbfm.2010.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan Y, Chen KF, Lin YX, Wu W, Zhou X, Zhang X, Zhang X, Shi J. Intracisternal administration of SB203580, a p38 mitogen-activated protein kinase inhibitor, attenuates cerebral vasospasm via inhibition of tumor-necrosis factor-alpha. J Clin Neurosci. 2013;20:726–730. doi: 10.1016/j.jocn.2012.09.012. [DOI] [PubMed] [Google Scholar]
- Ouyang L, Shi Z, Zhao S, Wang FT, Zhou TT, Liu B, Bao JK. Programmed cell death pathways in cancer: a review of apoptosis, autophagy and programmed necrosis. Cell Prolif. 2012;45:487–498. doi: 10.1111/j.1365-2184.2012.00845.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Pinzon MA, Stetler RA, Fiskum G. Novel mitochondrial targets for neuroprotection. J Cereb Blood Flow Metab. 2012;32:1362–1376. doi: 10.1038/jcbfm.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao C, Liu X, Liu W, Shi H, Zhao Z, Chen H, Zhao S. Anti-apoptotic and neuroprotective effects of tetramethylpyrazine following subarachnoid hemorrhage in rats. Auton Neurosci. 2008;141:22–30. doi: 10.1016/j.autneu.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Cheng G, Wei L, Zhi-dan S, Shi-guang Z, Xiang-zhen L. Atorvastatin ameliorates cerebral vasospasm and early brain injury after subarachnoid hemorrhage and inhibits caspase-dependent apoptosis pathway. BMC Neurosci. 2009;10:7. doi: 10.1186/1471-2202-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endo H, Nito C, Kamada H, Yu F, Chan PH. Akt/GSK3β survival signaling is involved in acute brain injury after subarachnoid hemorrhage in rats. Stroke. 2006;37:2140–2146. doi: 10.1161/01.STR.0000229888.55078.72. [DOI] [PubMed] [Google Scholar]
- Cahill J, Calvert JW, Zhang JH. Mechanisms of early brain injury after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2006;26:1341–1353. doi: 10.1038/sj.jcbfm.9600283. [DOI] [PubMed] [Google Scholar]
- Palade C, Ciurea AV, Nica DA, Savu R, Moisa HA. Interference of apoptosis in the pathophysiology of subarachnoid hemorrhage. Asian J Neurosurg. 2013;8:106–111. doi: 10.4103/1793-5482.116389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijboer CH, Heijnen CJ, van der Kooij MA, Zijlstra J, van Velthoven CTJ, Culmsee C, van Bel F, Hagberg H, Kavelaars A. Targeting the p53 pathway to protect the neonatal ischemic brain. Ann Neurol. 2011;70:255–264. doi: 10.1002/ana.22413. [DOI] [PubMed] [Google Scholar]
- Cahill J, Calvert JW, Solaroglu I, Zhang JH. Vasospasm and p53-induced apoptosis in an experimental model of subarachnoid hemorrhage. Stroke. 2006;37:1868–1874. doi: 10.1161/01.STR.0000226995.27230.96. [DOI] [PubMed] [Google Scholar]
- Cahill J, Calvert JW, Marcantonio S, Zhang JH. p53 may play an orchestrating role in apoptotic cell death after experimental subarachnoid hemorrhage. Neurosurgery. 2007;60:531–545. doi: 10.1227/01.NEU.0000249287.99878.9B. [DOI] [PubMed] [Google Scholar]
- Yan J, Chen C, Hu Q, Yang X, Lei J, Yang L, Wang K, Qin L, Huang H, Zhou C. The role of p53 in brain edema after 24 hours of experimental subarachnoid hemorrhage in a rat model. Exp Neurol. 2008;214:37–46. doi: 10.1016/j.expneurol.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Moll UM, Wolff S, Speidel D, Deppert W. Transcription-independent pro-apoptotic functions of p53. Curr Opin Cell Biol. 2005;17:631–636. doi: 10.1016/j.ceb.2005.09.007. [DOI] [PubMed] [Google Scholar]
- Kaiser M, Kuhnl A, Reins J, Fischer S, Ortiz-Tanchez J, Schlee C, Mochmann LH, Heesch S, Benlasfer O, Hofmann WK. et al. Antileukemic activity of the HSP70 inhibitor pifithrin-mu in acute leukemia. Blood Cancer J. 2011;1:e28. doi: 10.1038/bcj.2011.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matz PG, Sundaresan S, Sharp FR, Weinstein PR. Induction of HSP70 in rat brain following subarachnoid hemorrhage produced by endovascular perforation. J Neurosurg. 1996;85:138–145. doi: 10.3171/jns.1996.85.1.0138. [DOI] [PubMed] [Google Scholar]
- van den Tweel ER, Peeters-Scholte CM, Van BF, Heijnen CJ, Groenendaal F. Inhibition of nNOS and iNOS following hypoxia-ischemia improves long-term outcome but does not influence the inflammatory response in the neonatal rat brain. Dev Neurosci. 2002;24:389–395. doi: 10.1159/000069044. [DOI] [PubMed] [Google Scholar]
- Heck TG, Schaler CM, de Bittencourt PIH. HSP70 expression: does it a novel fatigue signaling factor from immune system to the brain? Cell Biochem Funct. 2011;29:215–226. doi: 10.1002/cbf.1739. [DOI] [PubMed] [Google Scholar]
- Turturici G, Sconzo G, Geraci F. Hsp70 and its molecular role in nervous system diseases. Biochem Res Int. 2011;2011:618127. doi: 10.1155/2011/618127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekihara K, Harashima N, Tongu M, Tamaki Y, Uchida N, Inomata T, Harada M. Pifithrin-mu, an inhibitor of Heat-Shock Protein 70, can increase the antitumor effects of hyperthermia against human prostate cancer cells. PLoS One. 2013;8:e78772. doi: 10.1371/journal.pone.0078772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayer RE, Zhang JH. The clinical significance of acute brain injury in subarachnoid hemorrhage and opportunity for intervention. Acta Neurochir Suppl. 2008;105:179–184. doi: 10.1007/978-3-211-09469-3_35. [DOI] [PubMed] [Google Scholar]
- Prunell GF, Svendgaard NA, Alkass K, Mathiesen T. Delayed cell death related to acute cerebral blood flow changes following subarachnoid hemorrhage in the rat brain. J Neurosurg. 2005;102:1046–1054. doi: 10.3171/jns.2005.102.6.1046. [DOI] [PubMed] [Google Scholar]
- Yan J, Li L, Khatibi NH, Yang L, Wang K, Zhang W, Martin RD, Han J, Zhang J, Zhou C. Blood-brain barrier disruption following subarachnoid hemorrhage may be facilitated through PUMA induction of endothelial cell apoptosis from the endoplasmic reticulum. Exp Neurol. 2011;230:240–247. doi: 10.1016/j.expneurol.2011.04.022. [DOI] [PubMed] [Google Scholar]
- Jing CH, Wang L, Liu PP, Wu C, Ruan D, Chen G. Autophagy activation is associated with neuroprotection against apoptosis via a mitochondrial pathway in a rat model of subarachnoid hemorrhage. Neuroscience. 2012;213:144–153. doi: 10.1016/j.neuroscience.2012.03.055. [DOI] [PubMed] [Google Scholar]
- Wang X, Han W, Du X, Zhu C, Carlsson Y, Mallard C, Jacotot E, Hagberg H. Neuroprotective effect of Bax-inhibiting peptide on neonatal brain injury. Stroke. 2010;41:2050–2055. doi: 10.1161/STROKEAHA.110.589051. [DOI] [PubMed] [Google Scholar]
- Zhou C, Yamaguchi M, Kusaka G, Schonholz C, Nanda A, Zhang JH. Caspase inhibitors prevent endothelial apoptosis and cerebral vasospasm in dog model of experimental subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2004;24:419–431. doi: 10.1097/00004647-200404000-00007. [DOI] [PubMed] [Google Scholar]
- Iseda K, Ono S, Onoda K, Satoh M, Manabe H, Nishiguchi M, Takahashi K, Tokunaga K, Sugiu K, Date I. Antivasospastic and antiinflammatory effects of caspase inhibitor in experimental subarachnoid hemorrhage. J Neurosurg. 2007;107:128–135. doi: 10.3171/JNS-07/07/0128. [DOI] [PubMed] [Google Scholar]
- Park S, Yamaguchi M, Zhou C, Calvert JW, Tang J, Zhang JH. Neurovascular protection reduces early brain injury after subarachnoid hemorrhage. Stroke. 2004;35:2412–2417. doi: 10.1161/01.STR.0000141162.29864.e9. [DOI] [PubMed] [Google Scholar]
- Krafft PR, Caner B, Klebe D, Rolland WB, Tang J, Zhang JH. PHA-543613 preserves blood brain barrier integrity after intracerebral hemorrhage in mice. Stroke. 2013;44:1743–1747. doi: 10.1161/STROKEAHA.111.000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumar RW. Molecular mechanisms of ischemic neuronal injury. Ann Emerg Med. 2000;36:483–506. doi: 10.1067/mem.2000.110995. [DOI] [PubMed] [Google Scholar]
- Harris HE, Andersson U, Pisetsky DS. HMGB1: a multifunctional alarmin driving autoimmune and inflammatory disease. Nat Rev Rheumatol. 2012;8:195–202. doi: 10.1038/nrrheum.2011.222. [DOI] [PubMed] [Google Scholar]
- Kang R, Livesey KM, Zeh HJ III, Lotze MT, Tang D. HMGB1 as an autophagy sensor in oxidative stress. Autophagy. 2011;7:904–906. doi: 10.4161/auto.7.8.15704. [DOI] [PubMed] [Google Scholar]
- Venereau E, Casalgrandi M, Schiraldi M, Antoine DJ, Cattaneo A, De MF, Liu J, Antonelli A, Preti A, Raeli L. et al. Mutually exclusive redox forms of HMGB1 promote cell recruitment or proinflammatory cytokine release. J Exp Med. 2012;209:1519–1528. doi: 10.1084/jem.20120189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murakami K, Koide M, Dumont TM, Russell SR, Tranmer BI, Wellman GC. Subarachnoid hemorrhage induces gliosis and increased expression of the pro-inflammatory cytokine high mobility group box 1 protein. Transl Stroke Res. 2011;2:72–79. doi: 10.1007/s12975-010-0052-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hreggvidsdottir HS, Lundberg AM, Aveberger AC, Klevenvall L, Andersson U, Harris HE. High mobility group box protein 1 (HMGB1)-partner molecule complexes enhance cytokine production by signaling through the partner molecule receptor. Mol Med. 2012;18:224–230. doi: 10.2119/molmed.2011.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edye ME, Lopez-Castejon G, Allan SM, Brough D. Acidosis drives damage-associated molecular pattern (DAMP)-induced interleukin-1 secretion via a caspase-1-independent pathway. J Biol Chem. 2013;288:30485–30494. doi: 10.1074/jbc.M113.478941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Q, Wang F, Li W, Li W, Hu Y, Li S, Zhu J, Zhou M, Hang C. Glycyrrhizic acid confers neuroprotection after subarachnoid hemorrhage via inhibition of high mobility group box-1 protein: a hypothesis for novel therapy of subarachnoid hemorrhage. Med Hypotheses. 2013;81:268–268. doi: 10.1016/j.mehy.2013.04.032. [DOI] [PubMed] [Google Scholar]
- Bialik S, Zalckvar E, Ber Y, Rubinstein AD, Kimchi A. Systems biology analysis of programmed cell death. Trends Biochem Sci. 2010;35:556–564. doi: 10.1016/j.tibs.2010.04.008. [DOI] [PubMed] [Google Scholar]
- Lee JY, He Y, Sagher O, Keep R, Hua Y, Xi G. Activated autophagy pathway in experimental subarachnoid hemorrhage. Brain Res. 2009;1287:126–135. doi: 10.1016/j.brainres.2009.06.028. [DOI] [PubMed] [Google Scholar]
- Wang Z, Shi XY, Yin J, Zuo G, Zhang J, Chen G. Role of autophagy in early brain injury after experimental subarachnoid hemorrhage. J Mol Neurosci. 2012;46:192–202. doi: 10.1007/s12031-011-9575-6. [DOI] [PubMed] [Google Scholar]
- Zhao H, Ji Z, Tang D, Yan C, Zhao W, Gao C. Role of autophagy in early brain injury after subarachnoid hemorrhage in rats. Mol Biol Rep. 2013;40:819–827. doi: 10.1007/s11033-012-2120-z. [DOI] [PubMed] [Google Scholar]
- Fayaz S, Suvanish KV, Rajanikant G. Necroptosis: who knew there were so many interesting ways to die? CNS Neurol Disord Drug Targets. 2013. in press. [DOI] [PubMed]
- Northington FJ, Chavez-Valdez R, Graham EM, Razdan S, Gauda EB, Martin LJ. Necrostatin decreases oxidative damage, inflammation, and injury after neonatal HI. J Cereb Blood Flow Metab. 2011;31:178–189. doi: 10.1038/jcbfm.2010.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez-Valdez R, Martin LJ, Flock DL, Northington FJ. Necrostatin-1 attenuates mitochondrial dysfunction in neurons and astrocytes following neonatal hypoxia-ischemia. Neuroscience. 2012;219:192–203. doi: 10.1016/j.neuroscience.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YQ, Wang L, Zhang MY, Wang T, Bao HJ, Liu WL, Dai DK, Zhang L, Chang P, Dong WW. et al. Necrostatin-1 suppresses autophagy and apoptosis in mice traumatic brain injury model. Neurochem Res. 2012;37:1849–1858. doi: 10.1007/s11064-012-0791-4. [DOI] [PubMed] [Google Scholar]
- Chang P, Dong W, Zhang M, Wang Z, Wang Y, Wang T, Gao Y, Meng H, Luo B, Luo C, Anti-necroptosis chemical necrostatin-1 can also suppress apoptotic and autophagic pathway to exert neuroprotective effect in mice intracerebral hemorrhage model. J Mol Neurosci. 2013. in press. [DOI] [PubMed]
- Wagner EF. AP-1 - Introductory remarks. Oncogene. 2001;20:2334–2335. doi: 10.1038/sj.onc.1204416. [DOI] [PubMed] [Google Scholar]
- Chen D, Wei X, Guan J, Yuan J, Peng Y, Song L, Liu Y. Inhibition of c-Jun N-terminal kinase prevents blood brain barrier disruption and normalizes the expression of tight junction proteins clautin-5 and ZO-1 in a rat model of subarachnoid hemorrhage. Acta Neurochir. 2012;154:1469–1476. doi: 10.1007/s00701-012-1328-y. [DOI] [PubMed] [Google Scholar]
- Yatsushige H, Yamaguchi M, Zhou C, Calvert JW, Zhang JH. Role of c-Jun N-terminal kinase in cerebral vasospasm after experimental subarachnoid hemorrhage. Stroke. 2005;36:1538–1543. doi: 10.1161/01.STR.0000170713.22011.c8. [DOI] [PubMed] [Google Scholar]
- Yatsushige H, Ostrowski RP, Tsubokawa T, Colohan A, Zhang JH. Role of c-Jun N-terminal kinase in early brain injury after subarachnoid hemorrhage. J Neurosci Res. 2007;85:1436–1448. doi: 10.1002/jnr.21281. [DOI] [PubMed] [Google Scholar]
- Borsello T, Clarke PGH, Hirt L, Vercelli A, Repici M, Schorderet DF, Bogousslavsky J, Bonny C. A peptide inhibitor of c-Jun N-terminal kinase protects against excitotoxicity and cerebral ischemia. Nat Med. 2003;9:1180–1186. doi: 10.1038/nm911. [DOI] [PubMed] [Google Scholar]
- Esneault E, Castagne V, Moser P, Bonny C, Bernaudin M. D-JNKi, a peptide inhibitor of c-Jun N-terminal kinase, promotes functional recovery after transient focal cerebral ischemia in rats. Neuroscience. 2008;152:308–320. doi: 10.1016/j.neuroscience.2007.12.036. [DOI] [PubMed] [Google Scholar]
- Michel-Monigadon D, Bonny C, Hirt L. c-Jun N-terminal kinase pathway inhibition in intracerebral hemorrhage. Cerebrovasc Dis. 2010;29:564–570. doi: 10.1159/000306643. [DOI] [PubMed] [Google Scholar]
- Nijboer CH, van der Kooij MA, van Bel F, Ohl F, Heijnen CJ, Kavelaars A. Inhibition of the JNK/AP-1 pathway reduces neuronal death and improves behavioral outcome after neonatal hypoxic -ischemic brain injury. Brain Behav Immun. 2010;24:812–821. doi: 10.1016/j.bbi.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Benakis C, Vaslin A, Pasquali C, Hirt L. Neuroprotection by inhibiting the c-Jun N-terminal kinase pathway after cerebral ischemia occurs independently of interleukin-6 and keratinocyte-derived chemokine (KC/CXCL1) secretion. J Neuroinflammation. 2012;9:76. doi: 10.1186/1742-2094-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijboer CH, Bonestroo HJ, Zijlstra J, Kavelaars A, Heijnen CJ. Mitochondrial JNK phosphorylation as a novel therapeutic target to inhibit neuroinflammation and apoptosis after neonatal ischemic brain damage. Neurobiol Dis. 2013;54:432–444. doi: 10.1016/j.nbd.2013.01.017. [DOI] [PubMed] [Google Scholar]
- Park GH, Jeon SJ, Ko HM, Ryu JR, Lee JM, Kim HY, Han SH, Kang YS, Park SH, Shin CY. et al. Activation of microglial cells via protease-activated receptor 2 mediates neuronal cell death in cultured rat primary neuron. Nitric Oxide. 2010;22:18–29. doi: 10.1016/j.niox.2009.10.008. [DOI] [PubMed] [Google Scholar]
- Shishodia S, Aggarwal BB. Nuclear factor-kappaB activation: a question of life or death. J Biochem Mol Biol. 2002;35:28–40. doi: 10.5483/BMBRep.2002.35.1.028. [DOI] [PubMed] [Google Scholar]
- Aoki T, Kataoka H, Shimamura M, Nakagami H, Wakayama K, Moriwaki T, Ishibashi R, Nozaki K, Morishita R, Hashimoto N. NF-κB is a key mediator of cerebral aneurysm formation. Circulation. 2007;116:2830–2840. doi: 10.1161/CIRCULATIONAHA.107.728303. [DOI] [PubMed] [Google Scholar]
- You WC, Wang C, Pan Y, Zhang X, Zhou X, Zhang X, Shi J, Zhou M. Activation of nuclear factor-κB in the brain after experimental subarachnoid hemorrhage and its potential role in delayed brain injury. PLoS One. 2013;8:e60290. doi: 10.1371/journal.pone.0060290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijboer CHA, Heijnen CJ, Groenendaal F, May MJ, van Bel F, Kavelaars A. Strong neuroprotection by inhibition of NF-κB after neonatal hypoxia-ischemia involves apoptotic mechanisms but is independent of cytokines. Stroke. 2008;39:2129–2137. doi: 10.1161/STROKEAHA.107.504175. [DOI] [PubMed] [Google Scholar]
- van der Kooij MA, Nijboer CH, Ohl F, Groenendaal F, Heijnen CJ, van Bel F, Kavelaars A. NF-κB inhibition after neonatal cerebral hypoxia-ischemia improves long-term motor and cognitive outcome in rats. Neurobiol Dis. 2010;38:266–272. doi: 10.1016/j.nbd.2010.01.016. [DOI] [PubMed] [Google Scholar]
- Suzuki H, Hasegawa Y, Chen W, Kanamaru K, Zhang JH. Recombinant osteopontin in cerebral vasospasm after subarachnoid hemorrhage. Ann Neurol. 2010;68:650–660. doi: 10.1002/ana.22102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sodek J, Ganss B, McKee MD. Osteopontin. Crit Rev Oral Biol Med. 2000;11:279–303. doi: 10.1177/10454411000110030101. [DOI] [PubMed] [Google Scholar]
- Grasso G, Tomasello F. Erythropoietin for subarachnoid hemorrhage: is there a reason for hope? World Neurosurg. 2012;77:46–48. doi: 10.1016/j.wneu.2011.01.028. [DOI] [PubMed] [Google Scholar]
- Helbok R, Shaker E, Beer R, Chemelli A, Sojer M, Sohm F, Broessner G, Lackner P, Beck M, Zangerle A. et al. High dose erythropoietin increases brain tissue oxygen tension in severe vasospasm after subarachnoid hemorrhage. BMC Neurol. 2012;12:32. doi: 10.1186/1471-2377-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner JD, Mammis A, Prestigiacomo CJ. Erythropoietin for the treatment of subarachnoid hemorrhage: a review. World Neurosurg. 2010;73:500–507. doi: 10.1016/j.wneu.2010.02.026. [DOI] [PubMed] [Google Scholar]
- Fan X, Heijnen CJ, van der Kooij MA, Groenendaal F, van Bel F. Beneficial effect of erythropoietin on sensorimotor function and white matter after hypoxia-ischemia in neonatal mice. Pediatr Res. 2011;69:56–61. doi: 10.1203/PDR.0b013e3181fcbef3. [DOI] [PubMed] [Google Scholar]
- Gonzalez FF, Larpthaveesarp A, McQuillen P, Derugin N, Wendland M, Spadafora R, Ferriero DM. Erythropoietin increases neurogenesis and oligodendrogliosis of subventricular zone precursor cells after neonatal stroke. Stroke. 2013. in press. [DOI] [PMC free article] [PubMed]
- Juul S. Neuroprotective role of erythropoietin in neonates. J Matern Fetal Neonatal Med. 2012;25:97–99. doi: 10.3109/14767058.2012.715025. [DOI] [PubMed] [Google Scholar]
- Xiong T, Qu Y, Mu D, Ferriero D. Erythropoietin for neonatal brain injury: opportunity and challenge. Int J Dev Neurosci. 2011;29:583–591. doi: 10.1016/j.ijdevneu.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Celik M, Gakmen N, Erbayraktar S, Akhisaroglu M, Konakc S, Ulukus C, Genc S, Genc K, Sagiroglu E, Cerami A. et al. Erythropoietin prevents motor neuron apoptosis and neurologic disability in experimental spinal cord ischemic injury. Proc Natl Acad Sci. 2002;99:2258–2263. doi: 10.1073/pnas.042693799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juul SE, Anderson DK, Li Y, Christensen RD. Erythropoietin and erythropoietin receptor in the developing human central nervous system. Pediatr Res. 1998;43:40–49. doi: 10.1203/00006450-199801000-00007. [DOI] [PubMed] [Google Scholar]
- Siren AL, Fratelli M, Brines M, Goemans C, Casagrande S, Lewczuk P, Keenan S, Gleiter C, Pasquali C, Capobianco A. et al. Erythropoietin prevents neuronal apoptosis after cerebral ischemia and metabolic stress. Proc Natl Acad Sci. 2001;98:4044–4049. doi: 10.1073/pnas.051606598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villa P, Bigini P, Mennini T, Agnello D, Laragione T, Cagnotto A, Viviani B, Marinovich M, Cerami A, Coleman TR. et al. Erythropoietin selectively attenuates cytokine production and inflammation in cerebral ischemia by targeting neuronal apoptosis. J Exp Med. 2003;198:971–975. doi: 10.1084/jem.20021067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Zhang Z, Wang Y, Zhang R, Chopp M. Treatment of stroke with erythropoietin enhances neurogenesis and angiogenesis and improves neurological function in rats. Stroke. 2004;35:1732–1737. doi: 10.1161/01.STR.0000132196.49028.a4. [DOI] [PubMed] [Google Scholar]
- Chen G, Zhang S, Shi J, Ai J, Hang C. Effects of recombinant human erythropoietin (rhEPO) on JAK2/STAT3 pathway and endothelial apoptosis in the rabbit basilar artery after subarachnoid hemorrhage. Cytokine. 2009;45:162–168. doi: 10.1016/j.cyto.2008.11.015. [DOI] [PubMed] [Google Scholar]
- Grasso G, Buemi M, Alafaci C, Sfacteria A, Passalacqua M, Sturiale A, Calapai G, De Vico G, Piedimonte G, Salpietro FM. et al. Beneficial effects of systemic administration of recombinant human erythropoietin in rabbits subjected to subarachnoid hemorrhage. Proc Natl Acad Sci. 2002;99:5627–5631. doi: 10.1073/pnas.082097299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang ZG, Chopp M. Neurorestorative therapies for stroke: underlying mechanisms and translation to the clinic. Lancet Neurol. 2009;8:491–500. doi: 10.1016/S1474-4422(09)70061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocsis JD, Honmou O. Chapter 6 - bone marrow stem cells in experimental stroke. Progress in Brain Research. 2012;201:79–98. doi: 10.1016/B978-0-444-59544-7.00005-6. [DOI] [PubMed] [Google Scholar]
- Scheibe F, Ladhoff J, Huck J, Grohmann M, Blazej K, Oersal A, Baeva N, Seifert M, Priller J. Immune effects of mesenchymal stromal cells in experimental stroke. J Cereb Blood Flow Metab. 2012;32:1578–1588. doi: 10.1038/jcbfm.2012.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakabayashi K, Nagai A, Sheikh AM, Shiota Y, Narantuya D, Watanabe T, Masuda J, Kobayashi S, Kim SU, Yamaguchi S. Transplantation of human mesenchymal stem cells promotes functional improvement and increased expression of neurotrophic factors in a rat focal cerebral ischemia model. J Neurosci Res. 2010;88:1017–1025. doi: 10.1002/jnr.22279. [DOI] [PubMed] [Google Scholar]
- Donega V, van Velthoven CT, Nijboer CH, Kavelaars A, Heijnen CJ. The endogenous regenerative capacity of the damaged newborn brain: boosting neurogenesis with mesenchymal stem cell treatment. J Cereb Blood Flow Metab. 2013;33:625–634. doi: 10.1038/jcbfm.2013.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onda T, Honmou O, Harada K, Houkin K, Hamada H, Kocsis JD. Therapeutic benefits by human mesenchymal stem cells (hMSCs) and Ang-1 gene-modified hMSCs after cerebral ischemia. J Cereb Blood Flow Metab. 2007;28:329–340. doi: 10.1038/sj.jcbfm.9600527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Velthoven CTJ, Kavelaars A, van Bel F, Heijnen CJ. Repeated mesenchymal stem cell treatment after neonatal hypoxia-ischemia has distinct effects on formation and maturation of new neurons and oligodendrocytes leading to restoration of damage, corticospinal motor tract activity, and sensorimotor function. J Neurosci. 2010;30:9603–9611. doi: 10.1523/JNEUROSCI.1835-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donega V, Van Velthoven CT, Nijboer CH, Van BF, Kas MJ, Kavelaars A, Heijnen CJ. Intranasal mesenchymal stem cell treatment for neonatal brain damage: long-term cognitive and sensorimotor improvement. PLoS One. 2013;8:e51253. doi: 10.1371/journal.pone.0051253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalili MA, Anvari M, Hekmati-Moghadam SH, Sadeghian-Nodoushan F, Fesahat F, Miresmaeili SM. Therapeutic benefit of intravenous transplantation of mesenchymal stem cells after experimental subarachnoid hemorrhage in rats. J Stroke Cerebrovasc Dis. 2012;21:445–451. doi: 10.1016/j.jstrokecerebrovasdis.2010.10.005. [DOI] [PubMed] [Google Scholar]
- Keohane A, Ryan S, Maloney E, Sullivan AM, Nolan YM. Tumor necrosis factor-α impairs neuronal differentiation but not proliferation of hippocampal neural precursor cells: role of Hes1. Mol Cell Neurosci. 2010;43:127–135. doi: 10.1016/j.mcn.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Turbic A, Leong SY, Turnley AM. Chemokines and inflammatory mediators interact to regulate adult murine neural precursor cell proliferation, survival and differentiation. PLoS One. 2011;6:e25406. doi: 10.1371/journal.pone.0025406. [DOI] [PMC free article] [PubMed] [Google Scholar]