Abstract
Fast biodegradable (12 h < half-life < 48 h) radioactive labeled microspheres are needed for PET and SPECT lung perfusion and radiomicrosphere therapy planning. An emulsion method was used to create 30.1 ±4.8 μm size range microspheres with biodegradable Chitosan glycol (CHSg). Microspheres were characterized and labeled with 99mTc or 68Ga as an alternative to MAA in perfusion PET and SPECT studies. Surface decoration of CHSg microspheres with p-SCN-Bn-NOTA was performed to increase 68Ga in vivo stability. 99mTc was labeled directly to the CHSg microspheres. Labeling yield and in vitro radiochemical stability were evaluated. In vitro CHSg microsphere degradation half-life was ~24 hours in porcine blood. Labeled microspheres were injected into Sprague Dawley rats and biodistribution was determined after 2 and 4 hours. Both 99mTc-CHSg and 68Ga-NOTA-CHSg were quickly allocated in the lungs after injection. 99mTc-CHSg showed 91.6 ± 6.5% and 83.2 ± 4.1% of the decay corrected injected activity remaining in the lungs after 2 and 4 hours, respectively. For the obtained 68Ga-NOTA-CHSg microspheres, lung allocation was very high with 98.9 ± 0.2% and 95.6 ± 0.9% after 2 and 4 hours, respectively. The addition of p-SCN-Bn-NOTA acts as a radioprotectant eliminating the released 68Ga activity from the lungs to the bladder protecting the other organs.
1. Introduction
Since 1974, the use of 99mTc-MAA (macroaggregated albumin) has been established as the gold standard for lung perfusion studies [1]. The availability of a MAA lyophilized kit [1] and the 99Mo/99mTc radio-isotopic generator [2] facilitated the use of 99mTc-MAA as a lung perfusion agent. The orientation of macroaggregates (which are seldom spherical) in the blood flow stream is important for determining “effective size,” making it difficult to predict their in vivo behavior. Aggregates rupturing into smaller pieces add another factor making the size distribution variable and unreliable [3]. The ideal (theoretical) perfusion particle should be spherical (size not to be dependent on particle orientation) with a practical size distribution of 30 ± 10 μm [3]. Polymeric spherical microparticles with narrow size distributions have been previously obtained [4]. The use of polymerical microspheres will also eliminate the risk of disease transmission due to human derived materials (such as MAA).
Another important application of 99mTc-MAA is in the radiomicrosphere therapy (RMT) planning [5]. Nonspherical macroaggregates (MAA, 10–90 μm) are used to predict the distribution behavior of the perfectly spherical therapy particles used for RMT which are commercially available (SirTEX and TheraSpheres ≈30 ± 10 μm). Despite the differences in size and morphology, MAA prediction of particle allocation has been shown to be a valuable tool in RMT planning; however, whether a better planning agent can ultimately produce a better clinical outcome is still an open question.
Many of the available biocompatible polymers have been labeled with 99mTc. Some examples are 99mTc-PLGA (poly (DL-lactide-co-glycolide)) nanoparticles [6], 99mTc-PLA (poly lactic acid) [7], and 99mTc-CHS (Chitosan) [8] among others. PLGA and PLA have known long degradation times (months). CHS has been found to have an in vitro half-life greater than 21 days [9]. This characteristic is relatively undesired when performing lung perfusion studies or for RMT planning, as the particles need to degrade fast (maximum 48 hour half-life) and restore normal blood flow.
A chitin derivate polysaccharide, chitosan (CHS), has recently emerged as a good material for drug delivery applications [10]. There are several commercially available CHS materials with both high and low solubility in water [11]. Particle degradation half-life is directly related to solubility of the polymer. There is a compromise in the ideal particle degradation rate: it has to be slow enough to allow allocation in the lungs and subsequent imaging, but fast enough to clear the vessels and restore blood flow afterwards (half-life 12–48 hours). One of the best candidates is Chitosan glycol (CHSg). CHSg has moderate (2 mg/mL) solubility in water, is well characterized, and commercially available (Sigma-Aldrich, CHSg ≥ 60%). Degradation can be manipulated using glutaraldehyde as a crosslinking agent.
Another important limitation of RMT planning is the difficulty quantifying biodistribution for dosimetric calculations when 99mTc is used. This is due to the fact that the 99mTc-MAA scintigraphy is a single photon emission tomography technique (SPECT) and creates difficulty in obtaining proper attenuation correction as compared to positron emission tomography (PET). The RMT planning will be greatly benefited by the inclusion of a positron emitter radioisotope, since absolute attenuation correction and potentially superior spatial and temporal resolution are available with PET. Important advances were made in early years by labeling the Pulmolite MAA kit with 68Ga [12–14], obtaining an 80% labeling yield and purity >95%. However since MAA is a poor surrogate of therapeutic microspheres, there is a need for fast biodegradable (12 h < half-life < 48 h) microspheres (30 ± 10 μm) that can be labeled with a PET isotope for proper RMT planning.
2. Materials and Methods
2.1. Particle Preparation and Surface Decoration
CHSg (Sigma-Aldrich, USA) particles were prepared using the water in oil (w/o) emulsion technique. One mL of CHSg solution (2% w/v solution in 2% v/v Acetic Acid) was added dropwise to a round bottom flask containing an egg-shaped magnetic stirrer, 20 mL of toluene, and 100 μL of Tween 80 (surfactant). Magnetic stirring rate was set at 1150 rpm (Model PC-410D, Corning-Cole Palmer, USA). The emulsion was stabilized for 15 minutes and 100 μL of glutaraldehyde (FisherSci, USA) was added. Stirring was continued for another 105 minutes. Later, toluene was decanted. Particles were washed three times with 200-proof ethanol (Sigma-Aldrich, USA) and centrifuged (1000 rcf, 30 seconds); the supernatant was removed and finally lyophilized for labeling (Model Freeze One Plus 6, LabConco, USA).
A stock solution of p-SCN-Bn-NOTA (Macrocyclics, USA) with concentration 1 mg/mL in Na2HCO3/NaH2CO3 (pH 9.3-9.4, Sigma-Aldrich, USA) was prepared. Microspheres were resuspended in 1 mL of the p-SCN-Bn-NOTA Stock solution. The suspension was stirred at room temperature for 4, 12, 24 and 48 hours (n = 3 per time point) to form the NOTA-CHSg particles [15]. After p-SCN-Bn-NOTA reaction, particles were washed 3 times with 200-proof ethanol and centrifuged (1000 rcf, 30 seconds); the supernatant was removed and finally lyophilized for labeling (Model Freeze One Plus 6, LabConco, USA). The reaction (Figure 1) yield was evaluated using a UV/Visible spectrophotometer (Cary 100 Bio, Varian/Agilent Technologies, Switzerland) at the 224 nm absorption peak of the p-SCN-Bn-NOTA.
Figure 1.
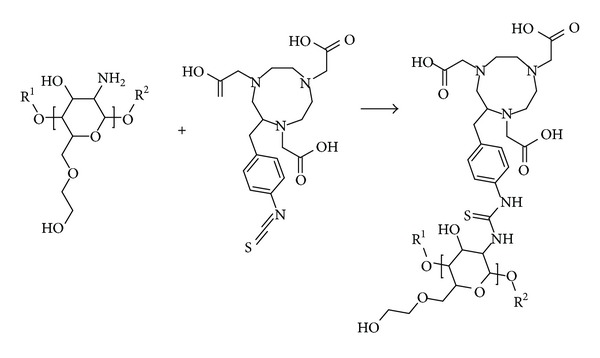
Surface decoration of CHSg microparticles with p-SCN-Bn-NOTA. R1 and R2 are repeated CHSg polymer chains (equal or different lengths).
2.2. 99mTc-CHSg 68Ga-CHSg and 68Ga-NOTA-CHSg Labeling
NA99mTcO4 was obtained from a local pharmacy (Triad Isotopes, Miami, USA). One mCi was used to label approximately 100,000 particles in a 15 mL centrifuge vial containing the lyophilized particles after addition of 100 μL of 1 mg/mL SnCl2 stock solution (Sigma-Aldrich, USA). 99mTc-CHSg labeling was performed during 30 minutes at 25°C and 750 rpm in a Thermomixer (Comfort 15 mL Block Thermomixer, Eppendorf, Germany). 68Ga was obtained by eluting the IGG-100 (Eckert and Ziegler, 50 mCi) 68Ge/68Ga generator with 5 mL of 0.1 M HCl solution (starting solution for buffering). 68Ga Labeling of 68Ga-NOTA-CHSg (pH ≈ 4, 0.25 mL of 3 N NaAc added to initial solution) and 68Ga-CHSg (pH ≈ 5.5, 0.3 mL of 3 N NaAc added to initial solution) was performed at room temperature for 15 minutes. Particles were later centrifuged (1000 rcf, 30 seconds) and the supernatant was removed using a 5′′ spinal needle. Both particles and supernatant were measured for labeling yield determination and radiochemical purity studies.
Labeled particles (n = 4) were resuspended in reconstituted (1% w/v) bovine hemoglobin lysate (Sigma-Aldrich, USA). Particles were stirred for 4 hours at 37°C in a thermomixer. Every hour the particles were centrifuged, decanted, and measured together with the supernatant to assess radiochemical stability.
2.3. CHSg Microspheres Degradation Studies
For the in vitro particle degradation studies, porcine blood was obtained from a local abattoir (Mataderos Cabrera, Miami, USA), sodium citrate was added as anticoagulant, and the blood was centrifuged at 3000 rcf for 30 minutes. Plasma was later decanted and used for microsphere degradation experiments. Lyophilized CHSg and NOTA-CHSg (unlabeled) were resuspended in the plasma. CHSg and NOTA-CHSg microsphere samples were extracted at 1, 2, 4, 12, 24, 48, and 72 hours. All samples (n = 3 per time point) were analyzed for size distribution and particle concentration using a hemacytometer (Reichert, USA) and an optical microscope (Micromaster, FisherSci, USA).
For in vivo particle degradation studies, lyophilized CHSg microparticles were resuspended in carbonate buffer (pH = 9.34). NHS-Fluorescein (Thermo Scientific, USA) was dissolved in dimethyl sulfoxide (DMSO, Thermo Scientific, USA) with a concentration of 10 mg/mL. A total 1 mg of NHS-fluorescein (100 μL of the stock solution) was added to the vial containing the particles and stirred for 2 hours (Figure 2). At the end of the reaction particles were centrifuged, washed three times with water, and finally lyophilized (lyophilized CHSg-fluorescein).
Figure 2.
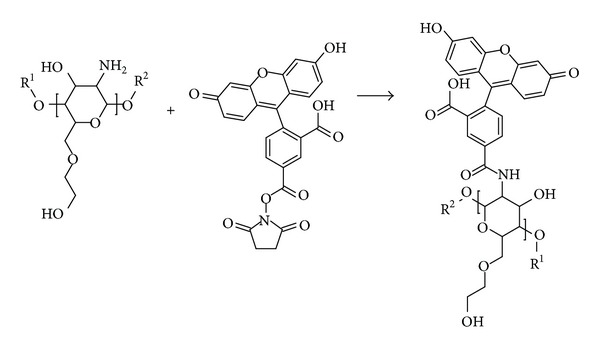
CHSg + NHS-Fluorescein reaction. R1 and R2 are repeated CHSg polymer chains (equal or different lengths).
Particles were resuspended in saline solution for injection (FisherSci, USA) and ≈10000 particles were injected to each Sprague Dawley rat (200–225 grams, Harlan, USA) in the lateral tail vein. Animals were euthanized at 2, 6, 12, and 24 hours (n = 2 per time point). Before extraction of the lungs, the trachea was isolated and a V cut was made. A syringe containing optimal cutting temperature (OCT, Tissue-Tek, USA) cryoembedding media was inserted in the trachea and the lungs were filled with 2 mL. Lungs were finally extracted and frozen in a plastic mold filled with OCT and dipped in liquid nitrogen. Specimens were obtained by cryosectioning the frozen samples (14 μm slices) in a Microtome (Leica, Japan). Lung cryospecimens (4 lung sections per animal) were analyzed with a florescence microscope (Olympus IX81 with a Q Imaging Retiga 1300 Camera, USA). The entire area of each specimen was imaged using a 4x objective. Obtained images were analyzed using in-house software and particles were measured and counted.
2.4. Lung Perfusion Experiments
Animals (Sprague Dawley rats, 200–225 grams, 2 per time point, Harlan, USA) were weighed before the procedure and anesthetized using an Ohmeda Isotec 3 isoflurane vaporizer (GE Healthcare, USA). Animals were restrained in the supine position (completely anesthetized) and a torso X-ray was obtained (Belmont Acuray 071A, USA). Later, 100 μL of the labeled microspheres (8,000–10,000 particles) with an activity ranging from 1.85 to 3.7 MBq (50 to 100 μCi) was injected through the lateral tail vein. Animals were euthanized at 2 or 4 hours. For both time-points lungs, liver, spleen, heart, kidneys, ribs, and 0.2 mL of blood and urine were collected, weighed, and measured for activity using a Cobra 5000 well counter (Packard, USA). Noncollimated autoradiography images (in the unaltered supine position the X-ray was obtained) were also taken at 1, 2, 3, and 4 hours (Packard Phosphorimager, Perkin Elmer, USA). In one group free 68Ga was injected as a control. The obtained X-rays and the autoradiography images were superimposed to provide anatomical and functional data.
3. Results and Discussion
3.1. Particle Preparation and Characterization
The emulsion method used created spherical particles (Figure 3). A size distribution of 30 ± 5 μm was obtained.
Figure 3.
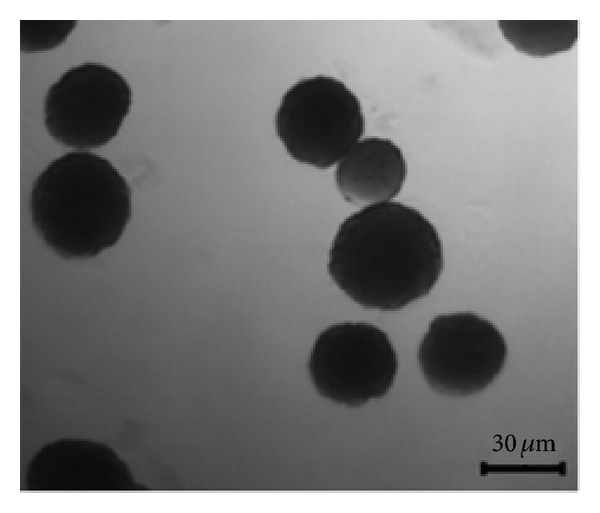
Prepared CHSg microspheres.
Lyophilization and labeling of the particles did not affect their size and morphology. CHSg microspheres swelled 20–25% when placed in contact with water, a feature that was taken into consideration when producing these particles.
The distribution did not change after the 12-hour reaction with p-SCN-Bn-NOTA (Figure 1) (P = 0.1, 95% confidence). The final size distribution obtained was 31 ± 5 μm (Figure 4). However many broken particles (no longer spherical) and small fragments were observed due to rupture of the original CHSg microspheres after 24 and 48 hours of p-SCN-Bn-NOTA reaction.
Figure 4.
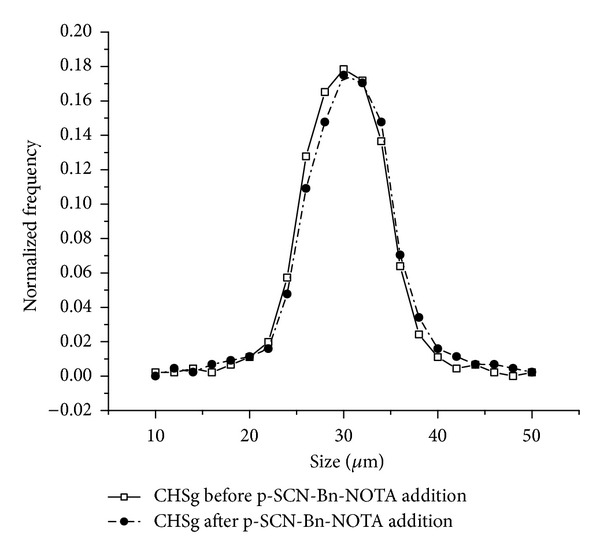
CHSg size distribution before and after p-SCN-Bn-NOTA surface decoration.
Around 260 ± 15 μg of p-SCN-Bn-NOTA (of the total 1 mg added, n = 3) was covalently attached to the surface of the CHSg microspheres after 12 hours of reaction. The net p-SCN-Bn-NOTA amount that bonded to the microspheres surface was increased to 297 ± 25 and 347 ± 40 μg after 24 and 48 hours of reaction (Figure 5).
Figure 5.
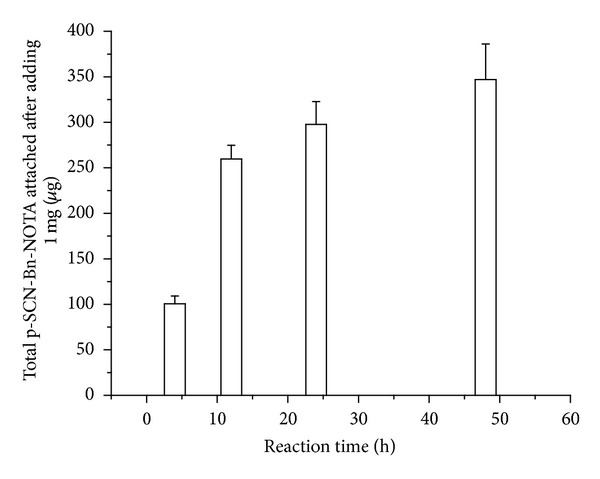
Surface decoration of CHSg with p-SCN-Bn-NOTA reaction yield at different reaction times.
Maximum reaction yield taking into consideration the totality of available NH2 groups was slightly over 1%. Nevertheless it is a skewed calculation since only a fraction of these groups are exposed for the p-SCN-Bn-NOTA reaction. Regardless of the yield, the addition of 260 micrograms of p-SCN-Bn-NOTA to the batch represents a theoretical loading capacity (assuming 95% labeling yield) of 12.8 μCi/particle (1.28 Ci for 100,000 particles). In molecular imaging only 3–5 mCi is used, 3 orders of magnitude less than the total available capacity.
3.2. 99mTc-CHSg 68Ga-CHSg and 68Ga-NOTA-CHSg Labeling and In Vitro Stability
Labeling yields of 94.7 ± 0.1%, 96.0 ± 3.5%, and 97.4 ± 3.0% for 99mTc-CHSg, 68Ga-CHSg, and 68Ga-NOTA-CHSg, respectively, were obtained (Figure 6). Over 97% radiochemical purity was found at all times for 68Ga-CHSg and 68Ga-NOTA-CHSg during the 4-hour study. Within the first hour 99mTc-CHSg microparticles quickly decreased in radiochemical purity to 82%, remaining fairly constant afterwards (being 80% after 4 hours) (Figure 6).
Figure 6.
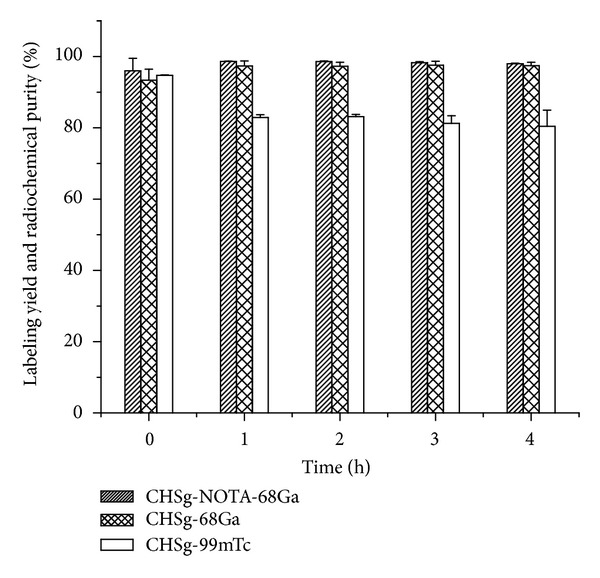
Labeling yield and in vitro radiochemical purity of 99mTc-CHSg 68Ga-CHSg and 68Ga-NOTA-CHSg.
Radiochemical purity in saline solution and PBS buffer was over 90% for 99mTc-CHSg, 68Ga-CHSg, and 68Ga-NOTA-CHSg after four hours. Even though the in vitro radiochemical purity of 99mTc-CHSg decreased rapidly to 80% in 1% reconstituted hemoglobin lysate one hour after labeling, the particles were tested in animals. For lung perfusion particles allocated in the vessels, the occlusion locally reduces the fluid in contact with the particles, potentially reducing the detachment of the 99mTc label and therefore increasing the chances of a successful image. Because of the high labeling yield obtained for 99mTc-CHSg (96.1 ± 0.3%) the particles did not need postlabeling purification.
3.3. CHSg Microspheres Degradation Studies
Porcine plasma studies showed fast (≈24 hours) microsphere degradation half-life (Figure 7). CHSg particles are initially swollen in plasma (effect not observed in PBS buffer or saline solution). The dramatic increase observed in particle concentration after 12 hours, together with the decrease in average particle size, is due to the rupture of the original particles into smaller fractions. These fractions are later dissolved (degraded) disappearing gradually from the suspension. The observed half-lives for CHSg and CHSg-NOTA were similar (≈24 hours), and there was no significant difference in their degradation profiles.
Figure 7.
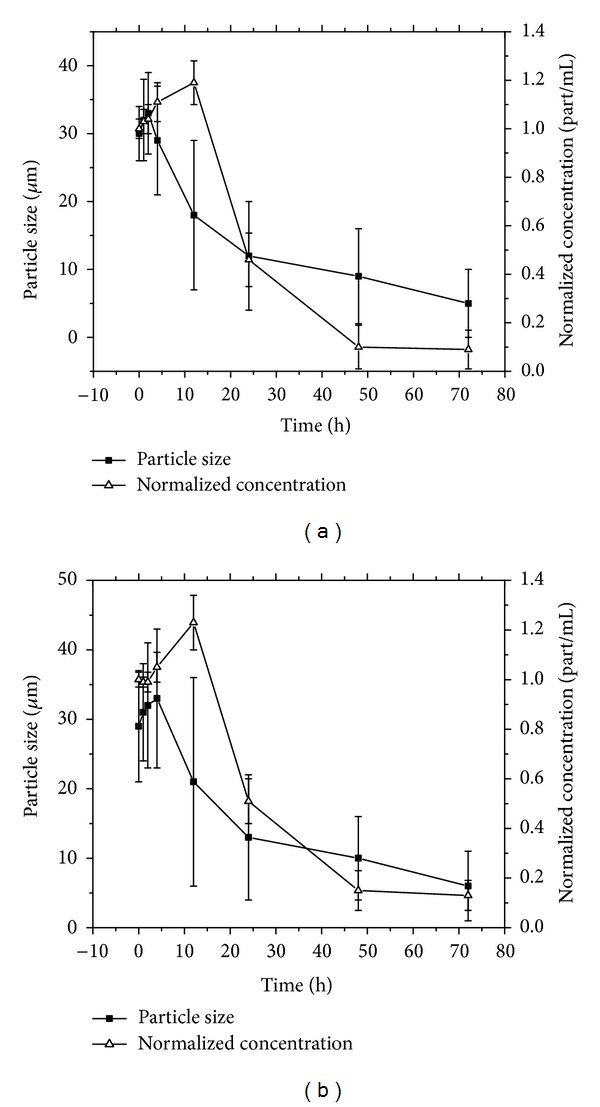
Porcine plasma microsphere degradation studies for (a) CHSg and (b) CHSg-NOTA (n = 3).
Particle degradation experiments performed in vivo show a similar degradation mechanism to that obtained in vitro (Figure 8).
Figure 8.
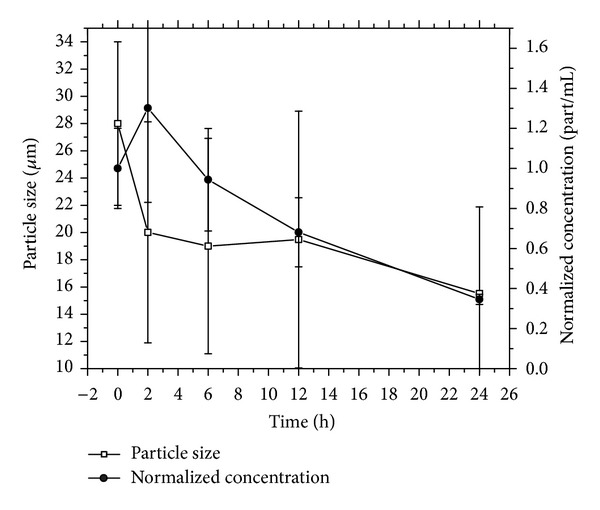
CHSg microspheres in vivo degradation studies (n = 2 per time point).
Particle concentration is initially increased because of microspheres rupture. Smaller pieces are later slowly dissolved. This dissolution results in a steady decrease of the particles average diameter and also in particle concentration in tissue (Figure 9). The in vivo half-life of the particles was determined to be 18–20 hours, since the time when the particle concentration is reduced to half (50% of initial particle concentration of any size occluding lung capillaries).
Figure 9.
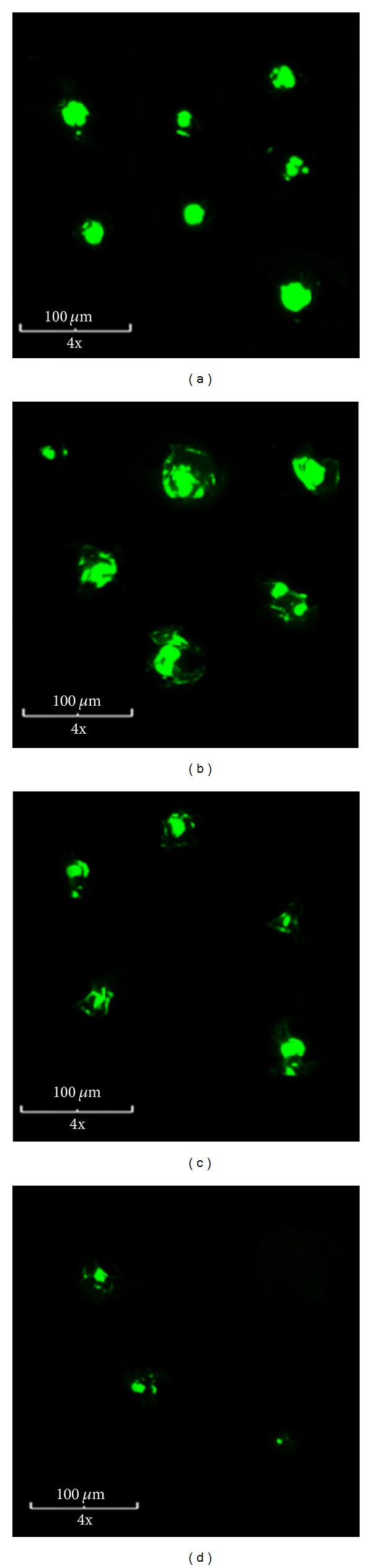
Representation of the in vivo CHSg microsphere degradation mechanism. Collage of representative microarticles found in the cryosections for different time points: (a) 2 hours, (b) 6 hours, (c) 12 hours, and (d) 24 hours. Relative particle amount in the images is related to the real particle concentration found in the tissue sections.
Results obtained in the in vivo experiments are highly qualitative since many assumptions were made for the calculations of average size and concentration. Particles concentration was assumed to be homogeneous in the entire lung, and particles under 10 micrometers were not included in the analysis since those should no longer occlude the vessels and therefore will not interfere with the later injection of the therapeutic particles in the final RMT phase of the procedure.
Furthermore, the average size calculation is only an estimate due to the artifacts inherent in the cryosectioning method; there is no way to know if a particle that is sized represents the whole cross-section or only a part of the particle, the latter being more likely. Therefore, the particle size distribution is probably an underestimate of the true in vivo size distribution. Nevertheless, by 24 hours, comparatively few particles were observed in the sections. Also, no particle clumping was observed as the particles were found to be evenly distributed and thus a good estimation of particles half-life was obtained. The particle degradation half-life was found to be between 18 and 20 hours, which makes the CHSg microspheres a potential candidate for lung perfusion imaging and RMT planning.
3.4. Lung Perfusion Experiments
Following tail vein injection, most of the 99mTc-CHSg activity was allocated in the lungs within the first 30 seconds (checked with Geiger counter, Victoreen ASM-990, Fluke, USA). After 2 hours, 91.6 ± 6.5% of the injected activity (decay corrected) was allocated in the lungs, and after 4 hours 83.2 ± 4.1% was still found in the lungs, as measured using a gamma-well counter (Cobra 5000 well counter, Packard, USA) (Table 1). The activity released from the lungs was almost exclusively excreted to the urine accounting for 4.9 ± 2.5% and 10.0 ± 2.1% decay corrected injected dose (DC-ID) after 2 hours and 4 hours, respectively. Less than 3% DC-ID/organ was detected in all the other organs at any given time point (Table 1). Lung perfusion images were obtained at several time points confirming the preferential lung allocation (Figure 11).
Table 1.
Biodistribution for 99mTc-CHSg and 68Ga-NOTA-CHSg at 2 and 4 hours and 68Ga-CHsg at 2 hours expressed as percent of decay corrected injected dose per organ (% DC-ID/organ).
| Organs | Biodistribution in % DC-ID/organ | |||||
|---|---|---|---|---|---|---|
| 68Ga-NOTA-CHSg | 99mTc-CHSg | 68Ga-CHSg | Free 68Ga | |||
| 2 hours | 4 hours | 2 hours | 4 hours | 2 hours | 2 hours | |
| Spleen | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.9 ± 0.2 | 0.6 ± 0.5 |
| Blood | 0.1 ± 0.1 | 0.5 ± 0.1 | 0.7 ± 0.5 | 0.8 ± 0.1 | 46.7 ± 1.2 | 84.9 ± 4.5 |
| Rib | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.4 ± 0.0 | 0.5 ± 0.4 |
| Urine | 0.5 ± 0.4 | 3.5 ± 0.6 | 4.9 ± 2.5 | 10.0 ± 2.1 | 10.9 ± 0.1 | 6.8 ± 2.9 |
| Right kidney | 0.1 ± 0.0 | 0.1 ± 0.0 | 1.1 ± 1.0 | 2.6 ± 0.8 | 0.9 ± 0.2 | 0.5 ± 0.5 |
| Left kidney | 0.1 ± 0.0 | 0.1 ± 0.0 | 1.2 ± 1.1 | 2.6 ± 0.8 | 0.8 ± 0.3 | 0.5 ± 0.5 |
| Heart | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 1.2 ± 0.2 | 0.7 ± 0.7 |
| Total lungs | 98.9 ± 0.2 | 95.6 ± 0.9 | 91.6 ± 6.5 | 83.2 ± 4.1 | 31.9 ± 1.3 | 3.1 ± 2.9 |
| Total liver | 0.2 ± 0.1 | 0.2 ± 0.1 | 0.3 ± 0.3 | 0.7 ± 0.3 | 6.3 ± 0.7 | 2.3 ± 1.9 |
Bold highlights the most important target organs. It is necessary to keep most of the activity in the lungs while the blood stays clear.
Figure 11.
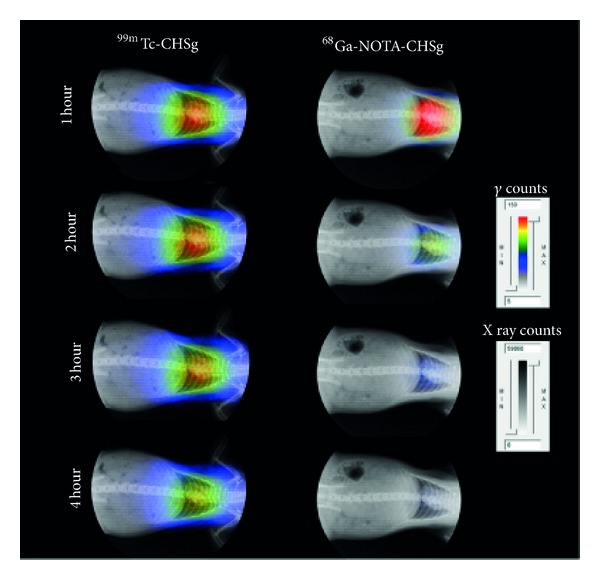
Uncollimated, non-decay-corrected full body X-ray/autoradiography of 99mTc-CHSg and 68Ga-NOTA-CHSg at 1, 2, 3, and 4 hours following injection.
Despite the excellent in vitro results obtained, 68Ga-CHSg did not perform well as a lung perfusion imaging agent. Strong evidence of 68Ga transchelation by native transferrin was observed (Figure 10).
Figure 10.
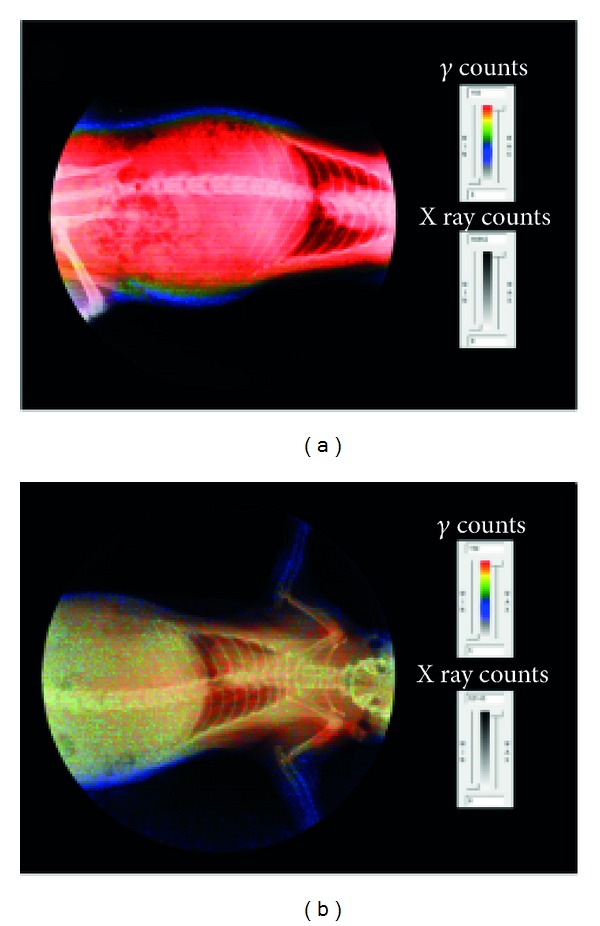
Comparison of images 10 minutes after injection for (a) free 68Ga and (b) 68Ga-CHSg.
Nevertheless, 68Ga-CHSg in vivo behavior was notably different from that of free 68Ga 2 hours after injection. After 2 hours 31.9 ± 1.3% DC-ID from the 68Ga-CHSg can be found in the lungs (Table 1), compared to the 3.1 ± 2.9% for the free 68Ga, but 46.7 ± 1.2% of the activity from the 68Ga-CHSg was already released to the blood. The 68Ga release from the CHSg to the blood was not expected since in vitro experiments showed minute leaching. This result (release of isotope from 68Ga-CHSg) made it necessary to coat the surface of the CHSg microspheres with a 68Ga specific chelator (NOTA) to increase in vivo stability of the labeling. Animal experiments performed with 68Ga-NOTA-CHSg showed high lung allocation and stability during the 4-hour study (Figure 11).
After 2 hours 98.9 ± 0.2% DC-ID of 68Ga-NOTA-CHSg was found in the lungs, decreasing to 95.6 ± 0.9% after 4 hours. The activity released from the lungs moved directly to the bladder (3.5 ± 0.6% after 4 hours). The absence of activity in the blood (0.1 ± 0.1% DC-ID at 2 hours and 0.5 ± 0.1% DC-ID after 4 hours) evidenced the high radiochemical stability of the NOTA-68Ga complex. The activity found in the urine must be due to early particle degradation releasing small polar fragments as frag-NOTA-68Ga. The addition of the NOTA chelator to the surface of the particles also served as an apparent radioprotectant to the rest of the organs, since less than one percent DC-ID was found in the blood at any given time. From the images (Figure 11) and the organ biodistribution data (Table 1), it can be concluded that in vivo stability of the prepared 68Ga-NOTA-CHSg and 99mTc-CHSg is remarkable and the labeled microspheres are good candidates for PET and SPECT lung perfusion imaging, respectively.
4. Conclusions
Chitosan glycol microspheres within the desired 30 ± 10 μm size range (to act as surrogates for the commercial SirSpheres and TheraSpheres, for treatment planning) were successfully obtained. Labeling was performed with >90% yield and in vitro radiochemical stability after 4 hours. High in vitro radiochemical purity was found for the labeled particles in the 4 hour study. In vitro degradation half-life was found to be ≈24 hours in porcine plasma, while in vivo half-life of the particles was found to be 18–24 hours. Both 99mTc-CHSg and 68Ga-NOTA-CHSg showed lung allocation quickly after injection. Biodistribution showed 91.6 ± 6.5% DC-ID and 83.2 ± 4.1% DC-ID of the 99mTc-CHSg injected activity remaining in the lungs after 2 and 4 hours, respectively. Lung allocation was very high for 68Ga-NOTA-CHSg microspheres, with 98.9 ± 0.2% DC-ID and 95.6 ± 0.9% DC-ID after 2 and 4 hours, respectively. The addition of p-SCN-Bn-NOTA acts as a 68Ga radioprotectant, since the microspheres degradation products are quickly eliminated to the bladder protecting the other organs, contrary to free 68Ga which remains in the blood pool bound to native transferrin.
Acknowledgements
The authors acknowledge the NIH Grant no. 1 R21 CA159073-01A1 and the Rinker Family Foundation.
Abbreviations
- MAA:
Macroaggregated albumin
- PET:
Positron emission tomography
- RMT:
Radiomicrosphere therapy
- SPECT:
Single photon emission tomography
- CHSg:
Chitosan glycol
- NOTA:
1,4,7-triazacyclononane-1,4,7-triacetic acid
- p-SCN-Bn-NOTA:
S-2-(4-Isothiocyanatobenzyl)-1,4,7-triazacyclononane-1,4,7-triacetic acid.
References
- 1.Chandra R, Shamoun J, Braunstein P, DuHov OL. Clinical evaluation of an instant kit for preparation of 99mTc MAA for lung scanning. The Journal of Nuclear Medicine. 1973;14(9):702–705. [PubMed] [Google Scholar]
- 2.Tucker WD, Greene MW, Weiss AJ, et al. Transactions of the 4th Annual Meeting American. New York, NY, USA: Academic Press; 1958. [Google Scholar]
- 3.Subramanian G, Rhodes BA, Cooper JF, Sodd VJ. Radiopharmaceuticals: International Symposium on Radiopharmaceuticals. Society of Nuclear Medicine; 1975. [Google Scholar]
- 4.Brannon-Peppas L. Recent advances on the use of biodegradable microparticles and nanoparticles in controlled drug delivery. International Journal of Pharmaceutics. 1995;116(1):1–9. [Google Scholar]
- 5.Gulec SA, Mesoloras G, Dezarn WA, McNeillie P, Kennedy AS. Safety and efficacy of Y-90 microsphere treatment in patients with primary and metastatic liver cancer: the tumor selectivity of the treatment as a function of tumor to liver flow ratio. Journal of Translational Medicine. 2007;5, article no. 15 doi: 10.1186/1479-5876-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevanović M, Maksin T, Petković J, Filipi M, Uskoković D. An innovative, quick and convenient labeling method for the investigation of pharmacological behavior and the metabolism of poly(DL-lactide-co-glycolide) nanospheres. Nanotechnology. 2009;20(33) doi: 10.1088/0957-4484/20/33/335102.335102 [DOI] [PubMed] [Google Scholar]
- 7.Ergün EL, Ercan MT, Selek H, et al. Evaluation of 99mTc labelled poly lactic acid microspheres for diagnostic radioembolization. Journal of Microencapsulation. 2000;17(4):509–518. doi: 10.1080/026520400405750. [DOI] [PubMed] [Google Scholar]
- 8.Bom H-S, Min J-J, Jeong H-J. Molecular nuclear imaging for targeting and trafficking. Nuclear Engineering and Technology. 2006;38(5):399–404. [Google Scholar]
- 9.Chitosan microspheres: therapeutic agent for liver-directed radiomicrosphere therapy. The Journal of Nuclear Medicine. 2012;53(supplement 1, article 1707) [Google Scholar]
- 10.Kumar MNVR, Muzzarelli RAA, Muzzarelli C, Sashiwa H, Domb AJ. Chitosan chemistry and pharmaceutical perspectives. Chemical Reviews. 2004;104(12):6017–6084. doi: 10.1021/cr030441b. [DOI] [PubMed] [Google Scholar]
- 11.Riva R, Ragelle H, des Rieux A, Duhem N, Jérôme C, Préat V. Chitosan and chitosan derivatives in drug delivery and tissue engineering. Advances in Polymer Science. 2011;244(1):19–44. [Google Scholar]
- 12.Even GA, Green MA. Gallium-68-labeled macroaggregated human serum albumin, 68Ga-MAA. International Journal of Radiation Applications and Instrumentation. 1989;16(3):319–321. doi: 10.1016/0883-2897(89)90014-7. [DOI] [PubMed] [Google Scholar]
- 13.Coarasa AA, Milera A, Carvajal DA, McGoron AJ. 99mTc-MAA versus 68Ga-MAA as Perfusion Agents. Proceedings of the 29th Southern Biomedical Engineering Conference (SBEC '13); May 2013; Miami, Fla, USA. [Google Scholar]
- 14.Wagner SJ, Welch MJ. Gallium-68 labelling of albumin and albumin microspheres. The Journal of Nuclear Medicine. 1979;20(5):428–433. [PubMed] [Google Scholar]
- 15.Jae MJ, Mee KH, Young SC, et al. Preparation of a promising angiogenesis PET imaging agent: 68Ga-labeled c(RGDyK)-isothiocyanatobenzyl-1,4,7-triazacyclononane-1, 4,7-triacetic acid and feasibility studies in mice. The Journal of Nuclear Medicine. 2008;49(5):830–836. doi: 10.2967/jnumed.107.047423. [DOI] [PubMed] [Google Scholar]


