Abstract
Background:
Standard treatment of advanced cervical cancer is concurrent chemoradiation. Radical radiotherapy for carcinoma cervix includes pelvic external beam radiotherapy (EBRT) with the concomitant platinum based chemotherapy followed by intracavitary brachytherapy (ICBT) to boost central disease. Management of patients who are suboptimally treated, especially, after unsuccessful ICBT insertion is not well-defined. This study explores the role of hysterectomy in these patients.
Materials and Methods:
From January 2006 to December 2011, 38 patients with locally advanced cervical cancer, in whom ICBT insertion was unsuccessful, were analyzed retrospectively. Operable patients with no parametrial involvement underwent hysterectomy and outcomes (recurrence free and overall survival) were noted.
Results:
The major complications in post operative period were wound infection, paralytic ileus and bladder atony all of which were conservatively managed with no mortality. At median follow-up of 36 months (range 12-60 months) there was no recurrence in patients with stage 1B2 and stage IIA, 25 out of 38 (65.8%) were event free and the overall survival was 71%.
Conclusion:
Many patients in Indian scenario receive suboptimal therapy in locally advanced cervical cancer. EBRT with chemotherapy followed by type 1 extra-fascial hysterectomy can be a good alternative for these patients.
Keywords: Carcinoma cervix, hysterectomy, unsuccessful intracavitary brachytherapy
Introduction
Cervical cancer is the third most common malignancy in women worldwide, and it is the second most common cause of cancer related death in women in developing countries.[1] Standard treatment of advanced cervical cancer is concurrent chemoradiation.[2] Radical radiotherapy for carcinoma cervix includes pelvic external beam radiotherapy (EBRT) with concomitant platinum based chemotherapy followed by intracavitary brachytherapy (ICBT) to boost central disease. Application of brachytherapy reduces the local failure rate[3] by 25% and nearly doubles the survival rate.[4] Without ICBT, the risk of recurrences increases due to suboptimal treatment. Management of patients who are suboptimally treated, especially after unsuccessful ICBT insertion is not well defined. The treatment options for these patients include hysterectomy or radiotherapy boost using the pelvic EBRT. The latter method may not be feasible as the risk of major complications nearly doubles for every 4 Gy increase in the dose of EBRT delivered above standard dose.[4] There is limited published evidence to guide subsequent treatment, after unsuccessful ICBT insertion.
The purpose of this study was to explore the role of hysterectomy in locally advanced cervical carcinoma after unsuccessful ICBT insertion.
Materials and Methods
From January 2006 to December 2011, 38 patients with locally advanced cervical cancer, in whom ICBT insertion was unsuccessful, were analyzed. This was a single institution retrospective study. In the absence of any published evidence, it was the institutional policy to refer patients for hysterectomy after unsuccessful ICBT, if the tumor had been rendered operable after the initial EBRT.
The case records of these patients were analyzed in detail for-the primary staging, causes of unsuccessful ICBT insertion, the response to the initial chemoradiation, subsequent surgery performed, histological diagnosis, morbidity, recurrence rates and survival. These patients were followed up every 3 monthly for initial 2 years and 6 monthly thereafter. The outcome (recurrence free and overall survival) was evaluated for all patients using the Kaplan-Meier curve (Statistical Package for the Social Science [SPSS], 16 - SPSS Inc, USA).
The radiotherapy technique used was pelvic EBRT given to a dose of 45 Gy in 25 daily fractions using the 6-18 MV photons, given via the four field pelvic box technique. Concomitant intravenous cisplatin was given weekly at a dose of 40 mg/m2. After the completion of chemoradiation, all patients were planned for ICBT insertion, as long as the central tumor was encompassable by brachytherapy. ICBT was planned to be delivered using a single intra-uterine tube and two ovoids, via manual after-loading technique at a dose rate of 130-150 cGy/h.
When ICBT insertion was unsuccessful, patients who had a good response to initial chemoradiotherapy were referred to gynec-oncosurgeon within 2 months of primary treatment. Patients who did not have parametrial involvement were considered operable. Hysterectomy was carried out at our center after ruling out distant metastasis. The surgery performed was type 1 extra-fascial hysterectomy with pelvic lymphadenectomy.
Results
The initial stage and the causes of failed brachytherapy are given in Table 1. Majority of these patients had stage IIB at initial diagnosis. The median dose of EBRT given was 48Gy (range 34-58 Gy) and the median time required for the same was 40 days (35-55 days). Inability to dilate cervix, gross residual disease, and patients defaulting for brachytherapy were the most common causes for failed brachytherapy [Figure 1]. These patients underwent type 1 extra-fascial hysterectomy. The mean blood loss during surgery was 400 ml. Only 27% had good response with external beam radiotherapy alone. Majority of patients (73%) had residual tumor on post operative histopathological examination. Mean size of the residual tumor was 1.5cm. Squamous cell carcinoma (63%) was the most common histological variety seen in patients with residual tumor [Table 2]. Eight patients had more than half thickness of cervical stromal involvement. Five patients had isthmic involvement. Obturator nodes were positive in four patients and vaginal cut margins were positive in three patients.
Table 1.
Comparison of baseline characteristics
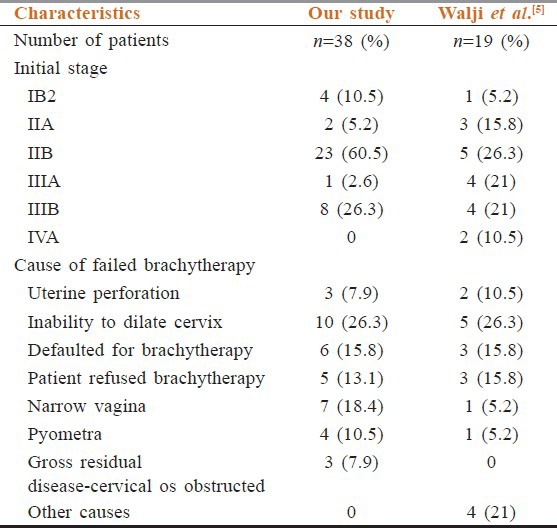
Figure 1.
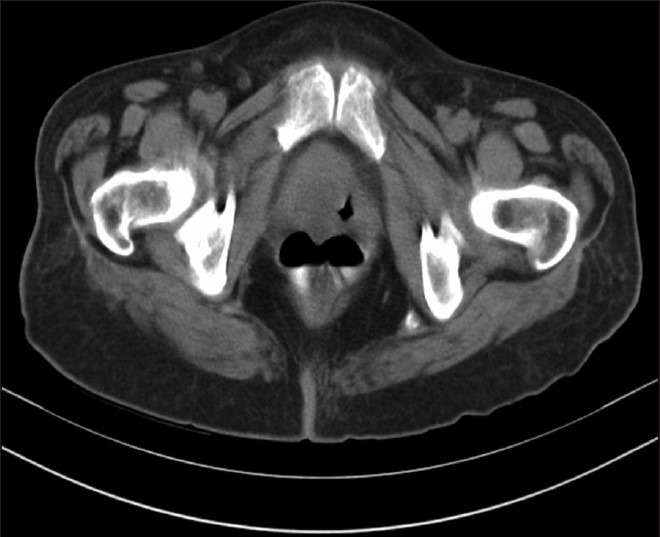
Post-external beam radiotherapy with a small cervical residual disease, in a patient who defaulted intracavitary brachytherapy
Table 2.
Post-operative characteristics
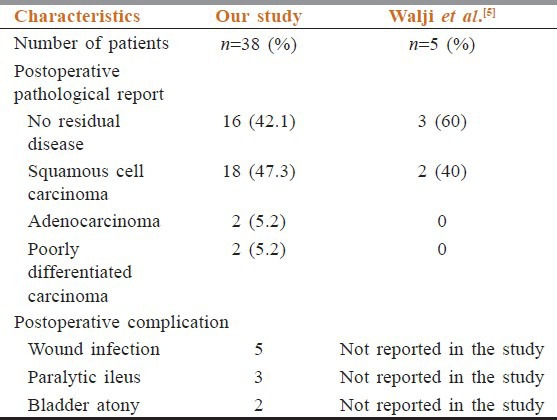
Wound infection was the most common complication in the post-operative period. Other complications included bladder atony, and paralytic ileus as shown in Table 2. All these were managed conservatively and no morbidity was seen due to these complications.
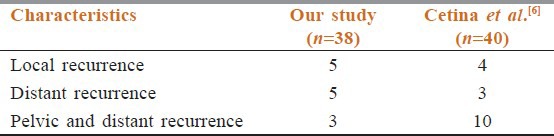
At median follow-up of 36 months (range 12-60 months) there was no recurrence in patients with stage 1B2 and stage IIA. Seven patients with stage IIB and 6 patients with stage III had recurrence. The site of recurrence is given in Table 3. The median time for recurrence was 16 months. The most common site of recurrence was para aortic lymph node followed by the lungs. Patients with recurrent disease received palliative carboplatin and paclitaxel chemotherapy. A total of 9 (3 in stage IIb and 6 in stage III) deaths were noted due to progressive disease.
Table 3.
Pattern of relapse
At final follow-up, 25 out of 38 patients (65.8%) were event free and the overall survival was 71% [Figure 2].
Figure 2.
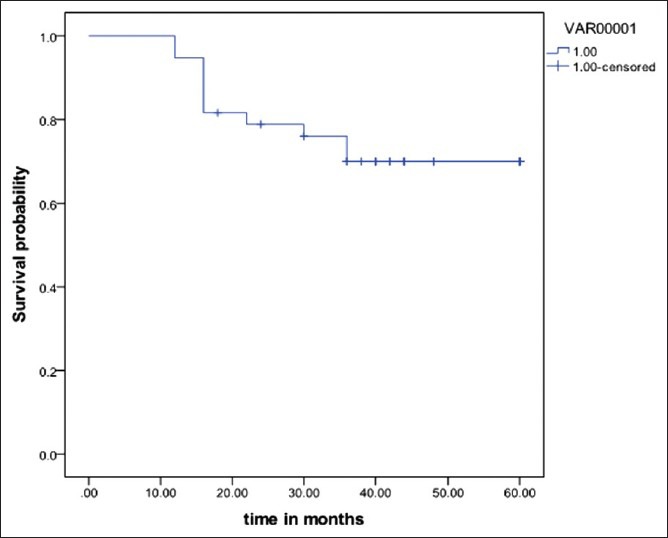
Overall survival
Discussion
After EBRT with chemotherapy in locally advanced cervical cancer, brachytherapy may be unsuccessful for a variety of reasons. There is dearth of published data regarding the management of these patients, especially those with good response to EBRT with concurrent chemotherapy. To the best of our knowledge this is the first study from India exploring the role of hysterectomy in locally advanced cervical cancer after suboptimal chemoradiotherapy.
In world literature there are few studies addressing this issue. Comparing our data with study carried out by Walji et al.[5] who analyzed 19 cases, the causes for unsuccessful brachytherapy were similar. Stenosis of cervical os was the most common cause for unsuccessful insertion of brachytherapy. Attempting insertion in such a situation leads to trauma to surrounding structures and creation of false passage. Only five patients in their study had undergone hysterectomy and none of their patients developed recurrence after adjuvant hysterectomy at a median follow-up of 60 months. Out of 38 patients in our study, recurrence was noted in 15 patients. This difference may be due to a small number of patients evaluated in the prior study. The only post-operative complication noted in the earlier study was wound infection. We noted a range of post-operative complications. Most importantly, post-chemoradiotherapy, dissecting the tissues and defining the tissue planes was more difficult, which explains some of the complications observed. However all complications could be managed conservatively. Multicenter data has also shown that hysterectomy can be safely done after chemoradiation.[6] Another study by Cetina et al.[7] who analyzed 40 cases, has shown that hysterectomy after EBRT has a similar outcome compared to EBRT with brachytherapy. Hysterectomy in their study was carried out within 7 weeks of EBRT. Operative complications were minimal in their study. The five years overall survival in their study was 78%. In our study at the end of 36 months, the overall survival was 71%.
The role of hysterectomy after radiation has been highlighted by a study form Monk et al.[8] where they noted its effectiveness in large cervical tumor, cervical tumor that respond poorly to radiation, and in patients unable to undergo brachytherapy in cervical cancer.
Another important observation of our study was the adequacy of local control. Most common site of recurrence was the para-aortic lymph nodes. This underscores the effective local control rendered by adjuvant type 1 extra-fascial hysterectomy, which can substitute for brachytherapy in selected patients. Only long-term data can prove if this management option can be adopted. Even at 36 months follow-up, the long-term toxicities like bladder and sexual dysfunction and proctitis were not seen as these had received suboptimal radiotherapy with salvage/desperate hysterectomy.
The limitations of our study are that all the patients who underwent adjuvant hysterectomy had good response to initial chemoradiotherapy. The number of patients is small and the retrospective nature of this study also is a major drawback. Majority of cervical cancers present with locally advanced disease in India. Many patients receive suboptimal therapy due to poor brachytherapy resources.[9] EBRT with chemotherapy followed by type 1 extra-fascial hysterectomy can be a good alternative for these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Green JA, Kirwan JM, Tierney JF, Symonds P, Fresco L, Collingwood M, et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: A systematic review and meta-analysis. Lancet. 2001;358:781–6. doi: 10.1016/S0140-6736(01)05965-7. [DOI] [PubMed] [Google Scholar]
- 3.Coia L, Won M, Lanciano R, Marcial VA, Martz K, Hanks G. The Patterns of Care Outcome Study for cancer of the uterine cervix. Results of the Second National Practice Survey. Cancer. 1990;66:2451–6. doi: 10.1002/1097-0142(19901215)66:12<2451::aid-cncr2820661202>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 4.Logsdon MD, Eifel PJ. Figo IIIB squamous cell carcinoma of the cervix: An analysis of prognostic factors emphasizing the balance between external beam and intracavitary radiation therapy. Int J Radiat Oncol Biol Phys. 1999;43:763–75. doi: 10.1016/s0360-3016(98)00482-9. [DOI] [PubMed] [Google Scholar]
- 5.Walji N, Chue AL, Yap C, Rogers LJ, El-Modir A, Chan KK, et al. Is there a role for adjuvant hysterectomy after suboptimal concurrent chemoradiation in cervical carcinoma? Clin Oncol (R Coll Radiol) 2010;22:140–6. doi: 10.1016/j.clon.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Classe JM, Rauch P, Rodier JF, Morice P, Stoeckle E, Lasry S, et al. Surgery after concurrent chemoradiotherapy and brachytherapy for the treatment of advanced cervical cancer: Morbidity and outcome: Results of a multicenter study of the GCCLCC (Groupe des Chirurgiens de Centre de Lutte Contre le Cancer) Gynecol Oncol. 2006;102:523–9. doi: 10.1016/j.ygyno.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 7.Cetina L, Garcia-Arias A, Candelaria M, Cantú D, Rivera L, Coronel J, et al. Brachytherapy versus radical hysterectomy after external beam chemoradiation: A non-randomized matched comparison in IB2-IIB cervical cancer patients. World J Surg Oncol. 2009;7:19. doi: 10.1186/1477-7819-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monk BJ, Solh S, Johnson MT, Montz FJ. Radical hysterectomy after pelvic irradiation in patients with high risk cervical cancer or uterine sarcoma: Morbidity and outcome. Eur J Gynaecol Oncol. 1993;14:506–11. [PubMed] [Google Scholar]
- 9.Tatsuzaki H, Levin CV. Quantitative status of resources for radiation therapy in Asia and Pacific region. Radiother Oncol. 2001;60:81–9. doi: 10.1016/s0167-8140(01)00330-9. [DOI] [PubMed] [Google Scholar]


