Abstract
Malignant syphilis is a rare and severe variant of secondary syphilis. It is clinically characterized by large papular, nodular and ulcerative lesions affecting the trunk and the extremities and covered with thick crust. We present a case of 52-year-old homosexual male who developed malignant syphilis and this was the first clinical manifestation of HIV infection. The patient was treated successfully with intravenous aqueous crystalline penicillin G. Physicians should recognize malignant syphilis and consider it in all HIV-infected individuals with ulceronodular skin lesions.
Key words: HIV, malignant syphilis.
Introduction
Malignant syphilis (also known as lues maligna or pustuloulcerative syphilis) is a rare, severe variant of secondary syphilis, clinically characterized by large nodular and ulcerative lesions covered with thick crust.1 Its incidence decreased at the beginning of the 20th century but an increase has been reported after 1987, affecting patients with HIV infection.
The diagnosis can be challenging for the clinician. We present a patient with lues maligna as the first clinical manifestation of HIV infection.
Case Report
A 52-year-old homosexual male was admitted in our clinic with a three week history of an extensive, febrile, papulonodular rash affecting his face (leonine facies, Figure 1), trunk (Figure 2), extremities, including palms and soles (Figures 3 and 4). The lesions were multiple, erythematous papules and nodules occasionally ulcerative with round or oval configuration. They had no pain or pruritus, no tendency to central healing and a number of these lesions were covered with a brown-black, thick crust. No mucosal lesions were seen.
Figure 1.

Erythematous ulceronodular lesions on the face producing a leonine facies.
Figure 2.

Multiple, erythematous ulceronodular lesions affecting the trunk.
Figure 3.

Erythematous papules and nodules on the left palm.
Figure 4.

Multiple papules and nodules on the right sole.
On clinical examination the patient had a temperature of 38.4°C, his blood pressure was 120/80 mmHg, heart rate 100/minute and respiration rate 15/min. He also complained of general malaise, headache, myalgias and loss of approximately 8 kilograms within the last 3 weeks. A 4mm punch biopsy was taken from the margin of an ulcerative lesion and histological examination showed dilatation of blood vessels with perivascular dermal infiltrate composed of many plasma cells (Figure 5).
Figure 5.
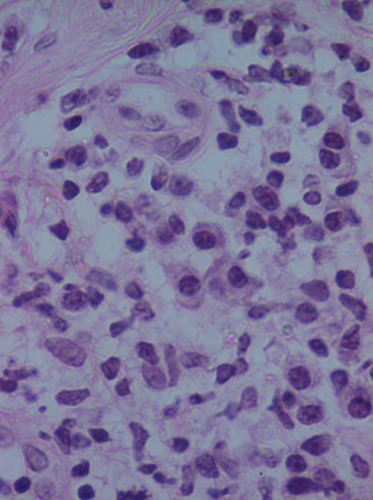
Histological examination revealed perivascular dermal infiltrate composed of many plasma cells (hematoxylin and eosin stain, magnification x400).
No spirochetes were seen. Staining and cultures for bacteria, mycobacteria and fungi were negative. Nucleic acid amplification tests for cytomegalovirus, varicella-zoster virus and herpes simplex virus, were also negative.
Laboratory investigations revealed a positive serology for HIV (Elisa and Western-Blot), and Venereal disease research laboratory test (VDRL) was reactive in 128 dilutions with a positive Treponema pallidum hemagglutination (TPHA). At that time, his CD4+ T lymphocyte count was 329/mm3 and his HIV viral load 65,855 copies/mL. Serology for hepatitis B and C was negative and a chest x-ray film was normal. The possibility of neurosyphilis was considered but the patient did not consent in a cerebrospinal fluid examination.
The patient started highly active antiretroviral therapy (HAART) and also treated with four million units of intravenous aqueous crystalline penicillin G at four-hour intervals per day, preceded by a single dose of intramuscular prednisone 50 mg. Topical fusidic acid ointment was also applied on ulcerative lesions, to avoid a superinfection. He responded very well to penicillin and no Jarisch-Herxheimer reaction was seen during treatment. He was discharged from hospital after 14 days of treatment.
On follow-up visit, three months after treatment, the patient presented with postinflammatory hyperpigmentation and a few residual scars. VDRL test showed a titer of 1:4, his CD4+ T lymphocyte count was 504/mm3 and HIV viral load was 11,000 copies/mL.
Discussion
Cutaneous disorders are a frequent presenting feature of HIV infection and/or AIDS.2
Malignant syphilis was firstly described by Bazin in 1859 as a nodular variant of syphilis. It represents an uncommon clinical manifestation that is possibly attributed to poor health, malnutrition, widespread use of antibiotics and corticosteroids and, most importantly, the presence of HIV infection.3
The diagnostic criteria of malignant syphilis include strongly positive serological test, a severe Jarisch-Herxheimer reaction and a good response to antibiotic therapy.4 In our case, the diagnosis of lues maligna was confirmed by the positive VDRL and TPHA titers, the characteristic ulceronodular lesions, the plasma-cells infiltration and the rapid response to penicillin treatment. There was no Jarisch-Herxheimer reaction probably because of his immunosuppression or the pre-medication with the systemic corticosteroids.
The histological findings of lues maligna are similar to those of secondary syphilis. Spirochetes are rarely found in the lesions or detected using Warthin-Starry stains.3 Rapid plasma reagin (RPR) titers in patients with lues maligna may be extremely high and remain in such levels despite antibiotic therapy. Nonetheless, negative RPR titers from prozone phenomenon have been reported.5
The exact mechanism of the development of malignant syphilis in HIV (+) patients is not yet known. It seems that the pathogenic interaction between HIV and Treponema pallidum may reduce the immunologic response to treponemal infection through a decrease in cell-mediated immunity, macrophage functional defect and possibly, immunomodulation of the humoral immunity response.6
The natural course of syphilis may be altered in HIV-infected patients but in most cases the manifestations remain typical.
Our case highlights the association between HIV infection and malignant syphilis. Physicians should recognize this condition and consider it in all HIV-infected individuals with ulceronodular skin lesions.
References
- 1.Sanchez MR. Syphilis. In: Wolff K, Goldsmith L, Katz S, et al., editors. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York: Mc Graw Hill; 2008. pp. 1955–1977. [Google Scholar]
- 2.De Socio GV, Simonetti S, Tomasini C, et al. Malignant syphilis with ocular involvement in an HIV-infected patient. Int J STD AIDS. 2011;22:298–300. doi: 10.1258/ijsa.2010.010389. [DOI] [PubMed] [Google Scholar]
- 3.Tucker JD, Shah S, Jarell AD, et al. Lues maligna in early HIV infection case report and review of the literature. Sex Transm Dis. 2009;36:512–4. doi: 10.1097/OLQ.0b013e3181a2a946. [DOI] [PubMed] [Google Scholar]
- 4.Fisher DA, Chang LW, Tuffanelli DL. Lues maligna. Presentation of a case and a review of the literature. Arch Dermatol. 1969;99:70–3. doi: 10.1001/archderm.99.1.70. [DOI] [PubMed] [Google Scholar]
- 5.Watson KM, White JM, Salisbury JR, Creamer D. Lues maligna. Clin Exp Dermatol. 2004;29:625–7. doi: 10.1111/j.1365-2230.2004.01630.x. [DOI] [PubMed] [Google Scholar]
- 6.Tosca A, Stavropoulos PG, Hatziolou E, et al. Malignant syphilis in HIV-infected patients. Int J Dermatol. 1990;29:575–8. doi: 10.1111/j.1365-4362.1990.tb03472.x. [DOI] [PubMed] [Google Scholar]


