Abstract
In November 2003, OPTN policy was amended to allow kidney transplant (KT) candidates to accrue waiting time while registered as status 7, or inactive. We evaluated trends in inactive listings and the association of inactive status with transplantation and survival, studying 262,824 adult first-time KT candidates listed between 2000–2011. The proportion of waitlist candidates initially listed as inactive increased from 2.3% pre-policy change to 31.4% in 2011. Candidates initially listed as inactive were older, more often female, African-American, and with higher body mass index. Post-policy change, conversion from initially inactive to active status generally occurred early if at all: at one year after listing, 52.7% of initially inactive candidates had been activated; at 3 years, only 66.3% had been activated. Inactive status was associated with a substantially higher waitlist mortality (aHR 2.21, 95%CI:2.15–2.28, p<0.001) and lower rates of eventual transplantation (aRR 0.68, 95%CI:0.67–0.70, p<0.001). In summary, waitlist practice has changed significantly since November 2003, with a sharp increase in the number of inactive candidates. Using the full waitlist to estimate organ shortage or as a comparison group in transplant outcome studies is less appropriate in the current era.
Keywords: Kidney Transplantation, Deceased Donor, Waitlist, Inactive Status
INTRODUCTION
The kidney transplant waitlist serves as a pool for potential kidney transplant recipients, an indicator of organ shortage, and a comparison group in studies of the benefit of transplantation (1–3). Because transplantation cannot be implemented as a randomized intervention, studies estimating transplant benefit often use waitlisted candidates as the counterfactual: what would have happened to a given transplant recipient had he/she not been transplanted. This type of analysis assumes that, except for the transplant itself, a waitlisted candidate is essentially identical to a matched transplant recipient of similar demographics and comorbidities. We hypothesized that this assumption, particularly in recent years, may not be accurate.
While the growth of the kidney transplant waitlist has been the subject of much concern (4), less attention has been given to its changing phenotype. Waitlist additions stem disproportionately from older age groups (5). Furthermore, in November 2003, OPTN policy 3.5.11 was amended to allow kidney transplant candidates to accrue waiting time while registered as status 7, or inactive (6). Since that time, the number of new inactive candidates has more than doubled, while active candidates have remained fairly stable (5,7). Whether candidates initially registered as inactive have the same demographic characteristics, waitlist survival, transplant potential, and post-transplant survival as initially active candidates has not been rigorously examined.
Using first-time kidney transplant candidates listed between 2000 and 2011, we evaluated patient characteristics associated with initial waitlist status, conversion from inactive to active status and, in turn, associations of inactive status with waitlist survival and eventual transplantation. Because inactive status is sometimes used as a placeholder for reasons other than a candidate’s medical fitness – until completion of the transplant work-up, for example, or achievement of a threshold body mass index (BMI) for surgery – we examined whether associations were different by age, gender, race, and BMI. Finally, hypothesizing that waitlist activity might capture unmeasured factors associated with mortality, we evaluated initial waitlist status and time spent inactive as a predictor of post-transplant survival.
MATERIALS AND METHODS
Study population
First-time kidney-only adult transplant candidates waitlisted between January 1, 2000 and December 31, 2011 were identified using data from the Scientific Registry of Transplant Recipients (SRTR), with follow-up through February 29, 2012 (N=262,824). Waitlist activity was assessed at a candidate (and not registrant) level. If a candidate were registered at multiple centers, listings were combined such that a candidate active with at least one center was considered active for that period of time. Mortality data were augmented by the SRTR through linkage with the Social Security Death Master File; graft survival data were augmented by the SRTR through linkage with Centers for Medicare & Medicaid Services.
Characterization of kidney transplant candidates
Candidates on the kidney transplant waitlist were classified as initially active or initially inactive, and in four categories using time-varying active status: always active, initially active but made inactive at some point (either temporarily or permanently), initially inactive but made active at some point (either temporarily or permanently), and always inactive. Baseline comorbid conditions and demographic characteristics were derived from the Transplant Candidate Registration (TCR) forms. In the case of multiple listings, a comorbidity was considered present if reported on any TCR form; BMI was estimated as the mean of all TCR-reported values. Differences across active status category were evaluated by t-tests and χ2 tests for continuous and categorical variables, respectively. Type of dialysis at listing was missing in 9.3% of candidates, and a missing indicator was used in multivariate analysis. All other variables except peripheral vascular disease (6.4% missing) were missing in less than 5% of candidates, and complete case analysis was used. As sensitivity analysis, multivariate analyses were re-run excluding peripheral vascular disease with no material change in results.
Model covariates
Transplant candidate covariates included listing year, gender, age, race, mode of renal replacement therapy at listing, previous non-kidney transplant, diabetes, peripheral vascular disease, primary cause of kidney disease, BMI, poor functional status, multi-listing (yes or no), and whether a candidate indicated that they would accept an organ from a donor infected with Hepatitis C Virus (HCV). The latter variable was considered a proxy for HCV infection in the candidate – a necessary assumption, since OPTN does not capture the HCV status of waitlist candidates, and one that likely underestimates the burden of HCV among the waitlist (8).
Regional variation in listing practice
Regional variation in initial listing practices was explored using random effects logistic regression, specifying a random intercept for transplant region and fully adjusting for candidate characteristics as well as listing year. This technique allows the rate of initial inactive listings to vary by region. The calculated intraclass correlation of latent responses can be used to estimate the proportion of variation in initial listing practice explained by variation across regions.
Natural history of initially inactive candidates
For initially inactive candidates listed post-policy change (2004–2011; N=48, 149), the cumulative incidences of activation, live donor transplantation prior to activation, and death prior to activation were estimated using the Fine and Gray method, which incorporates rates of competing events (9). Cox proportional hazards regression was used to estimate associations with activation or death prior to activation, adjusted for candidate variables described in the “Model covariates” section and censoring for live donor transplantation and death prior to activation or activation, respectively. Pre-policy change candidates were not included in these analyses, as the vast majority of waitlist candidates prior to November 2003 were initially listed as active.
Outcomes associations with active status
The associations of active status with transplantation (either living or deceased donor) and death prior to transplantation were estimated in all candidates listed post-policy change (2004–2011; N=192,229). The independent risk of waitlist mortality associated with active status (treated as a time-varying covariate) was estimated using Cox-proportional hazards regression, censoring for transplantation. The association between initial active status and eventual transplantation (either living or deceased donor) was estimated using modified Poisson regression, as previously described (10). The association of time-varying active status with eventual transplantation was not performed because, by definition, a participant cannot receive a deceased donor organ while inactive. All analyses were adjusted for candidate covariates described in the “Model covariates” section, and the interactions between active status and age, sex, race, and BMI were tested. Crude three-year rates of transplantation and death (irrespective of transplantation) were estimated in all incident candidates (2000–2008; N=185,429), categorizing into pre-policy change and initially active and initially inactive post-policy change.
Post-transplant outcomes by waitlist activity
Associations of waitlist activity with outcomes post-kidney transplantation were examined in all post-policy listed candidates who eventually received a deceased donor transplant (2004–2011; N=46,743). Associations between initial inactive status, proportion of waitlist time spent inactive, and post-transplant patient and death-censored graft survival were estimated using Cox proportional hazards regression, adjusting for multi-listing, recipient factors (gender, race, age, private insurance, pre-transplant renal replacement therapy type, dialysis vintage, BMI, cause of kidney disease, plasma reactive antibody (PRA) ≥ 40%, poor functional status, diabetes, peripheral vascular disease, previous non-kidney transplant, and HCV) and donor/transplant factors (year of transplant, zero antigen mismatch, expanded criteria donor organ, donor after cardiac death, cold ischemia time, and donor age). All analyses were performed using Stata 12.1/MP for Linux (StataCorp, College Station, TX).
RESULTS
Trends in waitlist status
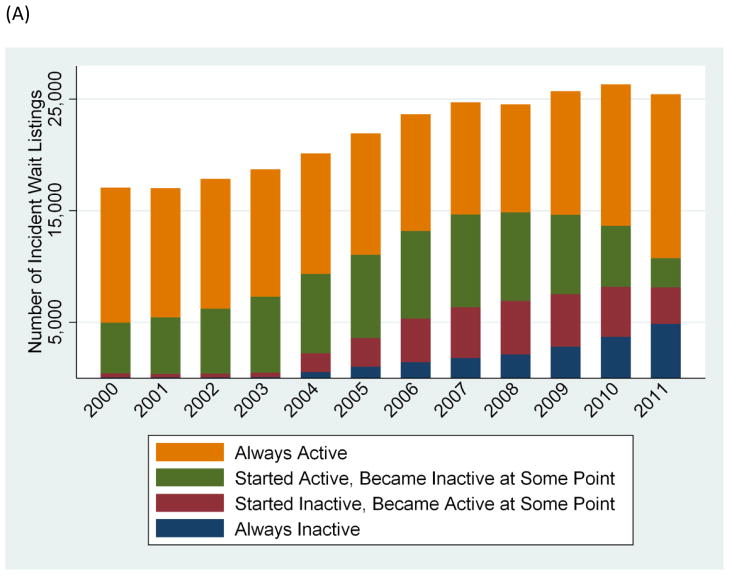
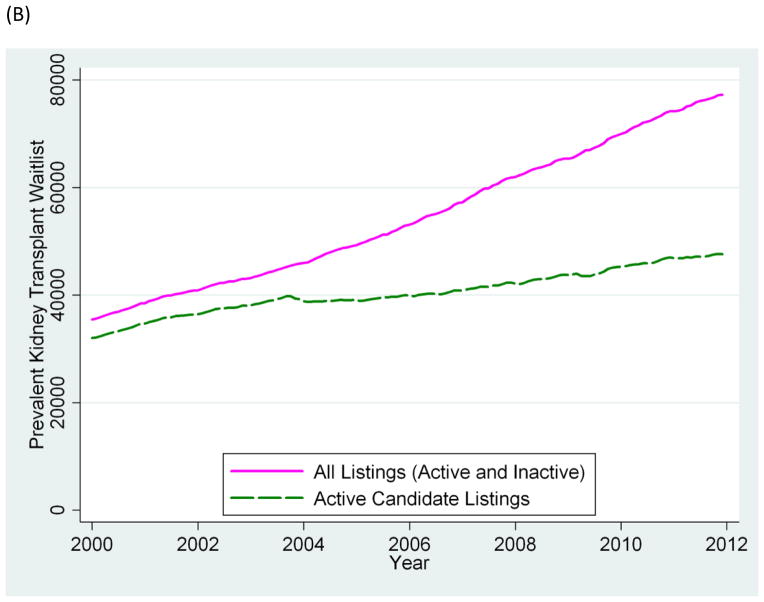
From 2000 to 2011, there was substantial change in the composition of the kidney transplant waitlist. The proportion of new candidates initially listed as inactive increased from 2.1% in 2003 pre-policy change (2.3% over January 2000–November 2003) to 11.0% in 2004 right after the amendment to OPTN policy 3.5.11; this proportion continued to increase to 31.9% in 2011 (Figure 1A). Thus, while overall first-time waitlist additions increased by 3.7% annually (from 17,072 in 2000 to 25,414 in 2011), the number of active candidate additions remained relatively stable, with an annual growth rate of only 0.3% (16,648 in 2000 to 17,307 in 2011). Trends in prevalent first-time waitlisted candidates were similar: the proportion active dropped from 90.2% in 2000 to 61.6% in 2011 (Figure 1B). In the population listed post-policy change, conversion from inactive to active status occurred early after listing if at all: at one year, 52.7% of those listed as initially inactive had been activated; at 3 years, only 66.3% had been activated (Figure 2).
Figure 1.
First-time adult kidney-only transplant waitlist candidates: (A) incident listings by initial and subsequent active status; (B) prevalent listings, by active status
Figure 2.
Cumulative incidence of activation and death prior to activation of initially inactive first-time kidney-only waitlist candidates listed between 2004 and 2011 estimated using the Fine and Gray method (N=48, 149)*
*Estimated cumulative incidence at 7 years: 71.6% activated (vital status post-activation not estimated), 14.6% died prior to activation, and 4.6% received a live donor transplant prior to activation.
Candidate characteristics by waitlist activity
When stratified by initial listing status and subsequent waitlist activity (which is affected by the time under follow up and the risk of death), there were distinct differences in candidate characteristics by subgroup (Table 1). Candidates who remained inactive throughout their waiting period were older (18.1% aged 65 or older, compared with 15.1%, 15.9%, and 14.9% in the initially inactive but converted to active, initially active but converted to inactive, and continuously active groups, respectively, p<0.001 for all comparisons). More continuously inactive candidates were female, African-American, with diabetes, poor functional status, peripheral vascular disease, and higher BMI. In contrast, the continuously active group was younger and generally had fewer comorbidities.
Table 1.
Candidate characteristics by initial waitlist status and subsequent activity, 2000–2011*
| Always Inactive | Started Inactive, But Active At Least Once | Started Active, But Inactive At Least Once | Always Active | |
|---|---|---|---|---|
| N (%) | 18,385 (7.0%) | 31,431 (12.0%) | 76,031 (28.9%) | 136,977 (52.1%) |
| Age (mean, years) | 53.4 | 51.7 | 52.0 | 51.0 |
| Sex (%): | ||||
| Male | 6.9 | 12.0 | 28.7 | 52.5 |
| Female | 7.2 | 11.9 | 29.3 | 51.6 |
| Race (%): | ||||
| Caucasian | 6.5 | 12.2 | 27.8 | 53.5 |
| African-American | 7.7 | 12.0 | 31.6 | 48.7 |
| Other | 7.2 | 11.4 | 28.0 | 53.4 |
| Cause of Kidney Disease (%): | ||||
| Glomerulonephritis | 5.1 | 12.0 | 26.9 | 56.0 |
| Diabetes | 8.9 | 12.0 | 31.1 | 48.1 |
| Congenital | 5.0 | 13.2 | 25.5 | 56.4 |
| Hypertension | 7.1 | 11.8 | 29.6 | 51.5 |
| Other | 6.4 | 11.5 | 27.5 | 54.7 |
| Dialysis Status at Listing (%): | ||||
| Preemptive | 7.5 | 13.5 | 24.4 | 54.7 |
| Hemodialysis | 6.4 | 10.9 | 31.0 | 51.7 |
| Peritoneal Dialysis | 4.7 | 11.4 | 30.9 | 53.0 |
| BMI (mean, kg/m2) | 29.7 | 28.6 | 28.4 | 27.7 |
| Previous (non-kidney) transplant (%) | 6.5 | 10.2 | 28.9 | 54.4 |
| Diabetes (%) | 8.8 | 12.0 | 30.9 | 48.3 |
| Peripheral vascular disease (%) | 9.9 | 12.5 | 33.6 | 44.0 |
| Hepatitis C (%)** | 4.2 | 7.6 | 21.8 | 66.3 |
| Poor functional status (%) | 8.2 | 9.2 | 29.3 | 53.3 |
| Multi-listed (%) | 1.2 | 15.3 | 39.7 | 43.9 |
| Time spent active (mean, percentage) | 0.0 | 59.5 | 65.3 | 100.0 |
| Region (%): | ||||
| 1 (CT, ME, MA, NH, RI, East VT) | 4.3 | 7.5 | 39.5 | 48.8 |
| 2 (DE, DC, MD, NJ, PA, WV, North VA) | 7.3 | 11.6 | 24.6 | 56.5 |
| 3 (AL, AR, FL, GA, LA, MS, PR) | 5.0 | 9.3 | 33.3 | 52.3 |
| 4 (OK, TX) | 7.6 | 10.9 | 26.4 | 55.1 |
| 5 (AZ, CA, NV, NM, UT) | 7.0 | 9.4 | 28.5 | 55.2 |
| 6 (AL, HI, ID, MT, OR, WA) | 9.0 | 22.3 | 36.4 | 32.3 |
| 7 (IL, MN, ND, SD, WI) | 7.4 | 14.1 | 23.2 | 55.4 |
| 8 (CO, IO, KS, MO, NE, WY) | 4.2 | 19.9 | 27.7 | 48.2 |
| 9 (NY, West VT) | 14.2 | 17.8 | 19.9 | 48.0 |
| 10 (IN, MI, OH) | 2.3 | 8.2 | 40.0 | 49.6 |
| 11 (KY, NC, SC, TN, Southern VA) | 8.7 | 13.3 | 29.8 | 48.2 |
For continuous variables, mean values reflect the cell-wise mean. For categorical variables, % reflects the row-wise percentage.
Candidate indicated a willingness to accept an HCV positive organ – used as a proxy for the candidate’s HCV status.
Regional differences in waitlist activity
All regions demonstrated increased use of inactive status post-policy change. Regions with the highest rates of initial inactive listing included Region 9 and Region 6; Regions 1 and 10 had the lowest rates (Table 1). These trends were particularly pronounced in recent years: since 2008, 53.3% and 43.5% of incident listings were initially inactive in Region 9 and Region 6, respectively, compared with 20.3% and 13.3% in Regions 1 and 10. After adjustment for listing year and candidate variables shown in Table 1, region explained only 5.5% (7.4% since 2008) of the variation in initial inactive listing.
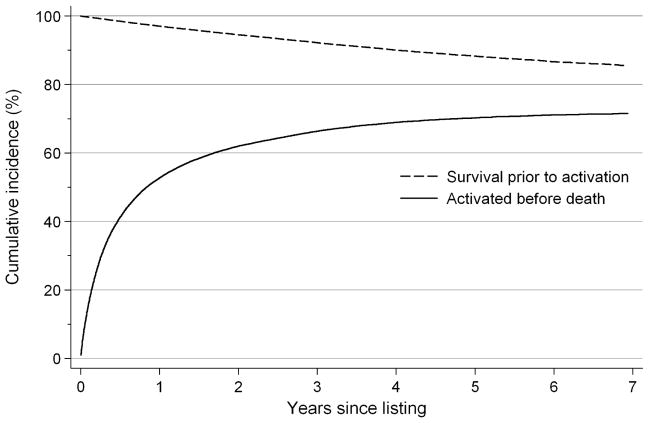
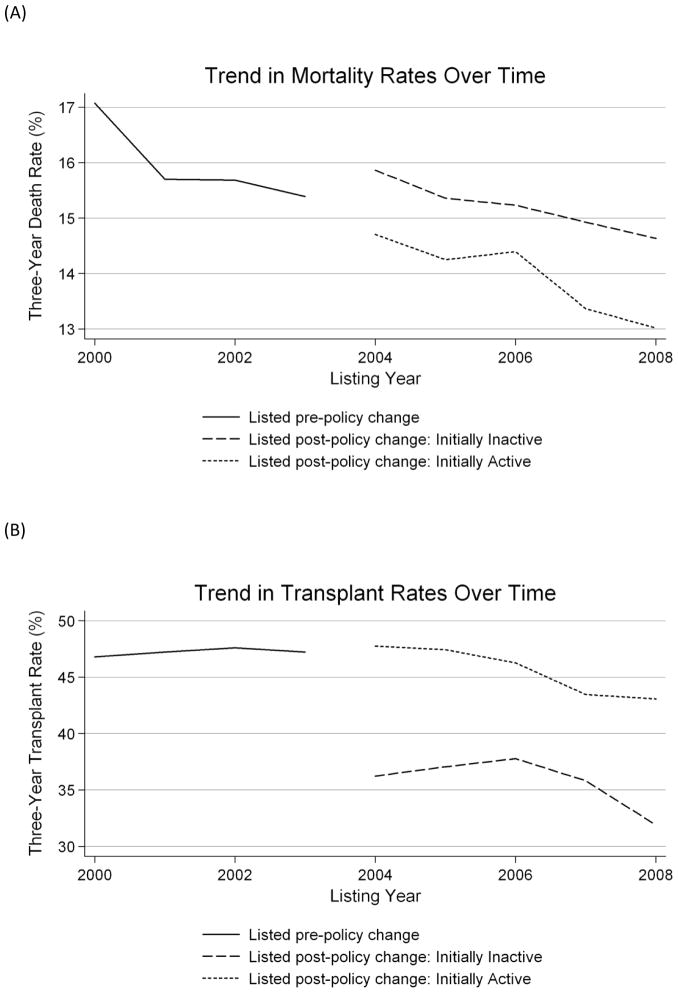
Candidate outcomes pre-and post-policy change
Overall, crude three-year mortality rates among incident kidney transplant candidates (irrespective of initial active status or eventual transplantation) declined over time, from 17.1% in 2000 to 13.5% in 2008 (p<0.001 for trend) (Figure 3A). Three-year transplantation rates also declined over time, from 46.8% in 2000 to 40.0% in 2008 (p<0.001 for trend) (Figure 3B). Initially inactive candidates had higher rates of overall mortality and lower rates of transplantation in all years post-policy change when compared with initially active candidates (mean three-year mortality rate, 15.1% vs. 14.0%, p<0.001; mean three-year transplantation rate, 35.4% vs. 45.7%, p<0.001). This difference was driven primarily by continuously inactive candidates: from the time of initial listing, candidates who were converted to active at some point actually had lower rates of mortality than initially active candidates (9.6% vs. 14.0%, p<0.001). Their crude three-year rate of transplantation lagged that of continuously active candidates but not those who became inactive at some point (43.3%, 21.8%, and 63.4% among initially inactive but activated at some point, initially active but made inactive at some point, and continuously active candidates, respectively, p<0.001 for all comparisons).
Figure 3.
By transplant candidate listing year: trends in (A) 3-year mortality irrespective of transplantation and(B) 3-year transplantation rates, post-2004 stratified by initial active status
Activation among initially inactive candidates
Among candidates initially listed as inactive post-policy change, factors independently associated with subsequent waitlist activation were Caucasian race, male sex, use of peritoneal dialysis, hypertension, earlier listing year, and multiple listings (Table 2). Conversely, factors associated with lower likelihood of subsequent waitlist activation were older age, diabetes, higher BMI, peripheral vascular disease, HCV, poor functional status, and use of hemodialysis.
Table 2.
Among initially inactive candidates, characteristics associated with transition to active status, 2004–2011
| Characteristic | Adjusted Hazard Ratio (95% CI) | P-Value |
|---|---|---|
| Age (per decade) | 0.98 (0.97–0.99) | <0.001 |
| Female sex | 0.94 (0.92–0.97) | <0.001 |
| Race: | ||
| Caucasian | Reference | |
| African-American | 0.82 (0.80–0.85) | <0.001 |
| Other | 0.84 (0.82–0.87) | <0.001 |
| BMI (per kg/m2) | 0.98 (0.98–0.98) | <0.001 |
| Previous (non-kidney) transplant | 1.08 (0.98–1.19) | 0.1 |
| Diabetes | 0.91 (0.87–0.95) | <0.001 |
| Peripheral vascular disease | 0.84 (0.80–0.88) | <0.001 |
| Poor functional status | 0.92 (0.87–0.97) | 0.002 |
| HCV positive * | 0.89 (0.83–0.95) | <0.001 |
| Etiology of Renal Disease: | ||
| Glomerular | Reference | |
| Diabetes | 0.84 (0.79–0.88) | <0.001 |
| Congenital | 1.02 (0.98–1.07) | 0.3 |
| Hypertensive | 0.85 (0.82–0.88) | <0.001 |
| Interstitial | 0.81 (0.75–0.87) | <0.001 |
| Miscellaneous | 0.79 (0.76–0.83) | <0.001 |
| Type of RRT at listing: | ||
| Preemptive | Reference | |
| Hemodialysis | 0.95 (0.93–0.98) | 0.001 |
| Peritoneal Dialysis | 1.15 (1.09–1.20) | <0.001 |
| Multi-listed | 1.62 (1.57–1.68) | <0.001 |
| Listing year | 0.97 (0.96–0.97) | <0.001 |
Candidate indicated a willingness to accept an HCV positive organ – used as a proxy for the candidate’s HCV status.
Active status and waitlist survival
Among candidates listed post-policy change, an inactive status (modeled as a time-varying covariate, not just at initial listing) conferred twice the risk of death on the waitlist (adjusted hazard ratio (aHR) 2.21, 95% CI: 2.15–2.28, p<0.001). This association did not differ by age (p=0.9 for interaction) or gender (p=0.4 for interaction); however, there was a stronger association between inactive status and death in Caucasians (aHR 2.40, 95% CI: 2.30–2.51, p<0.001) than African-Americans (aHR 2.00, 95% CI: 1.90–2.12, p<0.001; p<0.001 for interaction) or those of non-Caucasian, non-African-American race (aHR 2.14, 95% CI: 2.01–2.27, p<0.001; p=0.002 for interaction). The association of inactive status with mortality was attenuated among patients with higher BMI and initial inactive status (p<0.001 for each interaction). Initial inactive status was also associated with waitlist mortality, although the measure of association was considerably smaller (aHR 1.04, 95% CI: 1.01–1.07, p=0.009).
Initial status and subsequent transplantation
From the time of listing, patients initially listed as inactive post-policy change had a 37% lower rate of eventual transplantation (adjusted relative rate (aRR) 0.63, 95% CI: 0.62–0.65, p<0.001) than those initially listed as active, even after adjustment for multiple candidate covariates, listing year, and multi-listing status. Notably, this association was driven solely by continuously inactive candidates: when excluding these candidates, there was no adjusted association between initial status and eventual transplantation (aRR 1.01, 95% CI: 0.98–1.04, p=0.4).
Similar to the association with waitlist mortality, there was no interaction between initial inactive status and transplantation by age (p=0.6 for interaction) or gender (p=0.3 for interaction). However, there was a significant interaction by race: initial inactive status was more strongly associated with failure to receive transplantation among African-Americans (aRR 0.59, 95% CI: 0.56–0.61, p<0.001) than it was among Caucasians (aRR 0.65, 95% CI: 0.69–0.74, p<0.001) (p for interaction<0.001). There was no statistically significant interaction in the association between initial listing status and transplantation among Caucasians and those of non-Caucasian, non-African-American race.
Waitlist activity and post-deceased donor kidney transplant survival
Among the 46,473 kidney transplant candidates listed post-policy change who eventually received a deceased donor organ, there were no significant associations between initial waitlist status or proportion of time spent inactive and post-transplant mortality (initial inactive status: aHR 0.91, 95% CI: 0.82–1.01, p=0.07; proportion of time spent inactive, aHR 1.12, 95% CI: 0.95–1.31, p=0.2). Similarly there were no associations between waitlist activity and graft loss (initial inactive status: aHR 1.09, 95% CI: 0.86–1.40, p=0.5; proportion of time spent inactive, aHR 0.90, 95% CI: 0.60–1.35, p=0.6).
DISCUSSION
This national study of kidney transplant waitlist activity demonstrates the changing phenotype of the waitlist candidate after the OPTN policy 3.5.11 amendment, and its implications for waitlist survival and transplantation. Subsequent to the policy amendment in November 2003, there was a dramatic increase in the number of inactive candidates, including candidates initially listed as inactive and those whose status changed from active to inactive. These changes were observed in all regions, but particularly in Regions 9 and 6, where in recent years approximately half of the incident candidates were initially listed as inactive.
The recent increase in continuously inactive candidates – that is, patients initially listed as inactive who were never activated – may be partially explained by the shorter follow-up: they have had less time since listing to undergo a status change. However, given that the majority of initially inactive candidates are activated within a year and that the numbers of initially inactive but activated at some point have remained relatively stable, it appears that centers may be increasingly reluctant to activate candidates. Factors driving this reluctance – possibly, the increased focus on center outcomes, or the increased listing of older and/or more marginal candidates – merit further study.
Candidates initially listed as inactive experienced higher mortality and lower transplantation rates than those initially listed as active, but these differences were driven primarily by candidates who remained inactive throughout their entire waitlist experience – approximately one-third of the initially inactive candidates. Candidates with an inactive status at a given point in time (nearly 40% on December 1, 2011) had more than twice the risk of death and, by definition, were ineligible for deceased donor transplantation. These findings call into question the validity of using the full current waitlist as a comparison group for studies of transplant outcomes. In addition, they imply the organ shortage may be overestimated when considering transplant candidates irrespective of waitlist status. Importantly, these results should not be viewed as evidence for causality. The decision to make a candidate inactive is likely not the cause of the increased mortality: it is not clear that inactive candidates would be better served had they been transplanted. The real comparison for a group of inactive patients is other end-stage renal disease patients, not the general waiting list.
Many ground-breaking studies of transplant benefit have used the waitlist as an exchangeable cohort for transplant recipients (1–3,11). The assumption is that the waitlist survival experience is comparable to that of a transplant recipient, conditioned on adjustment variables, had they not received a transplant. While this premise may have been reasonable pre-policy change, we demonstrate that it is unlikely to hold in today’s environment: nearly one-third of all candidates are initially listed as inactive, with one-third of these candidates never undergoing activation, and a growing number of once active candidates currently listed as inactive. It appears that the amendment to OPTN policy 3.5.11 may have resulted in a flux of medically (or at least logistically) marginal candidates with lower transplant and survival potential. Thus, when constructing a comparison group in time-to-event analysis of the post-policy change era, active status must be considered. A transplant recipient should be compared with an active waitlist candidate of similar demographics and dialysis duration, conditioned on time since listing.
Another consequence of the OPTN policy amendment is the added complexity in estimating organ shortage. When a substantial proportion of the waitlist is not immediately eligible for deceased donor transplantation, their contribution to the disparity between organ supply and organ demand is unclear. Continuously inactive candidates will never receive an organ from the waitlist, and once an initially active candidate is deactivated, their probability of eventual transplantation plummets. With the uninterrupted accrual of waiting time, transplant centers have little incentive to remove unsuitable candidates from the waitlist. To assess current organ demand, perhaps only active candidates merit enumeration; to predict future demand, the rates and timing of conversion from inactive to active status should be considered.
A worrisome observation is the interaction of race with inactive status. Disparities in access to transplantation have been demonstrated at nearly every step in the transplantation process: the rates of referral, completion of pre-transplant evaluation, waitlisting, deceased donor transplantation once waitlisted, and live donor transplantation are all lower among African-Americans than Caucasians (12–17). Here, we demonstrate another disparity: African-Americans are more likely to be initially listed as inactive and less likely to be activated, yet their inactive status is less predictive of mortality and more predictive of not being transplanted than that among Caucasians. These associations persist despite adjustment for private insurance and other demographic and comorbid conditions, such as age and BMI. In other words, African-Americans appear to be listed as inactive less often for reasons related to medical fitness. Addressing reasons behind an inactive status and facilitating activation may help improve racial disparities in transplantation.
Strengths of this study include a nationally comprehensive review of the kidney transplant waitlist and waitlist practice patterns. We examine the effect of inactive listing in multiple settings: initial listing, listing over time, and the cumulative proportion of time spent inactive. For the first time, we describe associations with waitlist mortality, eventual transplantation, and post-transplant survival. However, certain limitations must be noted. This study is observational in nature, and we can only capture candidate factors that were collected by the OPTN. Unfortunately, the reason for status change was not captured in the vast majority of cases. We cannot reliably discern whether candidates were made inactive for medical or logistical reasons, and different centers may use inactive status for different reasons. However, the associations (and the modification of associations) with mortality suggest that, on average, an inactive status denotes a more medically marginal candidate, and that the poor medical fitness associated with inactive status may be less applicable to African-American candidates than Caucasian candidates.
In summary, since the amendment to OPTN policy 3.5.11, a far greater proportion of waitlist candidates are listed as inactive, and these candidates have higher mortality and lower transplant rates than those with an active status. Without taking this into account, the current kidney organ shortage is overestimated, and the validity of the waitlist as a comparison population for estimating survival benefit is questionable.
Acknowledgments
As a study of SRTR data, this work was supported in part by Health Resources and Services Administration contract 234-2005-37011C. The data reported here have been supplied by the Minneapolis Medical Research Foundation as the contractor for the SRTR. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy of or interpretation by the SRTR or the US Government.
Funding sources: Morgan Grams, National Kidney Foundation of Maryland, K08DK092287; Dorry Segev, NIH grants K23AG032885 (co-funded by the American Federation of Aging Research) and R21DK085409.
Abbreviations
- aHR
adjusted Hazard Ratio
- aRR
adjusted Relative Rate
- BMI
Body-Mass Index
- CI
Confidence Interval
- HCV
Hepatitis C Virus
- KT
Kidney Transplant
- OPTN
Organ Procurement and Transplantation Network
- PRA
Plasma Reactive Antibody
- SRTR
Scientific Registry of Transplant Recipients (SRTR)
- TCR
Transplant Candidate Registration
Footnotes
DISCLOSURES
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
References
- 1.Ojo AO, Hanson JA, Meier-Kriesche H, Okechukwu CN, Wolfe RA, Leichtman AB, et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-listed transplant candidates. J Am Soc Nephrol. 2001;12(3):589–597. doi: 10.1681/ASN.V123589. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341(23):1725–1730. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 3.Segev DL, Kucirka LM, Oberai PC, Parekh RS, Boulware LE, Powe NR, et al. Age and comorbidities are effect modifiers of gender disparities in renal transplantation. J Am Soc Nephrol. 2009;20(3):621–628. doi: 10.1681/ASN.2008060591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schold J, Srinivas TR, Sehgal AR, Meier-Kriesche HU. Half of kidney transplant candidates who are older than 60 years now placed on the waiting list will die before receiving a deceased-donor transplant. Clin J Am Soc Nephrol. 2009;4(7):1239–1245. doi: 10.2215/CJN.01280209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Renal Data System. USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2010. [Google Scholar]
- 6.United Network for Organ Sharing. [Accessed 3/7, 2012.];Bylaws and Policies. 2011 Available at: http://optn.transplant.hrsa.gov/PoliciesandBylaws2/policies/pdfs/policy_7.pdf.
- 7.McCullough KP, Keith DS, Meyer KH, Stock PG, Brayman KL, Leichtman AB. Kidney and pancreas transplantation in the United States, 1998–2007: access for patients with diabetes and end-stage renal disease. Am J Transplant. 2009;9(4 Pt 2):894–906. doi: 10.1111/j.1600-6143.2009.02566.x. [DOI] [PubMed] [Google Scholar]
- 8.Kucirka LM, Singer AL, Ros RL, Montgomery RA, Dagher NN, Segev DL. Underutilization of hepatitis C-positive kidneys for hepatitis C-positive recipients. Am J Transplant. 2010;10(5):1238–1246. doi: 10.1111/j.1600-6143.2010.03091.x. [DOI] [PubMed] [Google Scholar]
- 9.Fine JP, Gray RJ. A Proportional Hazards Model for the Subdistribution of a Competing Risk. Journal of the American Statistical Association. 1999;94(446):496–509. [Google Scholar]
- 10.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 11.Montgomery RA, Lonze BE, King KE, Kraus ES, Kucirka LM, Locke JE, et al. Desensitization in HLA-incompatible kidney recipients and survival. N Engl J Med. 2011;365(4):318–326. doi: 10.1056/NEJMoa1012376. [DOI] [PubMed] [Google Scholar]
- 12.Kasiske BL, London W, Ellison MD. Race and socioeconomic factors influencing early placement on the kidney transplant waiting list. J Am Soc Nephrol. 1998;9(11):2142–2147. doi: 10.1681/ASN.V9112142. [DOI] [PubMed] [Google Scholar]
- 13.Hall YN, Choi AI, Xu P, O’Hare AM, Chertow GM. Racial ethnic differences in rates and determinants of deceased donor kidney transplantation. J Am Soc Nephrol. 2011;22(4):743–751. doi: 10.1681/ASN.2010080819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epstein AM, Ayanian JZ, Keogh JH, Noonan SJ, Armistead N, Cleary PD, et al. Racial disparities in access to renal transplantation--clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343(21):1537–44. 2. doi: 10.1056/NEJM200011233432106. preceding 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolfe RA, Ashby VB, Milford EL, Bloembergen WE, Agodoa LY, Held PJ, et al. Differences in access to cadaveric renal transplantation in the United States. Am J Kidney Dis. 2000;36(5):1025–1033. doi: 10.1053/ajkd.2000.19106. [DOI] [PubMed] [Google Scholar]
- 16.Kucirka LM, Grams ME, Lessler J, Hall EC, James N, Massie AB, et al. Association of race and age with survival among patients undergoing dialysis. JAMA. 2011;306(6):620–626. doi: 10.1001/jama.2011.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall EC, James NT, Garonzik Wang JM, Berger JC, Montgomery RA, Dagher NN, et al. Center-level factors and racial disparities in living donor kidney transplantation. Am J Kidney Dis. 2012;59(6):849–857. doi: 10.1053/j.ajkd.2011.12.021. [DOI] [PubMed] [Google Scholar]