The induction of follicular regulatory T cells and control of germinal center reactions require the adaptor protein Traf3, in part because of Traf3-induced expression of ICOS.
Abstract
Regulatory T cells (Treg cells) control different aspects of immune responses, but how the effector functions of Treg cells are regulated is incompletely understood. Here we identified TNF receptor–associated factor 3 (TRAF3) as a regulator of Treg cell function. Treg cell–specific ablation of TRAF3 impaired CD4 T cell homeostasis, characterized by an increase in the Th1 type of effector/memory T cells. Moreover, the ablation of TRAF3 in Treg cells resulted in increased antigen-stimulated activation of follicular T helper cells (TFH cells), coupled with heightened formation of germinal centers and production of high-affinity IgG antibodies. Although the loss of TRAF3 did not reduce the overall frequency of Treg cells, it attenuated the antigen-stimulated production of follicular Treg cells (TFR cells). TRAF3 signaling in Treg cells was required to maintain high level expression of inducible co-stimulator (ICOS), which in turn was required for TFR cell generation and inhibition of antibody responses. These findings establish TRAF3 as a mediator of Treg cell function in the regulation of antibody responses and suggest a role for TRAF3 in mediating ICOS expression in Treg cells.
Foxp3+ regulatory T cells (Treg cells) form a major population of CD4+ immunosuppressive T cells that plays a pivotal role in maintaining peripheral immune tolerance and preventing autoimmune diseases (Sakaguchi et al., 2008). In addition, Treg cells also restrain the immunity against foreign antigens and cancer. The development, maintenance, and function of Treg cells are dependent on the master transcription factor Foxp3 and factors that regulate Foxp3 expression and function (Josefowicz et al., 2012). Genetic deficiencies in these core regulatory factors typically lead to impaired self-tolerance and homeostasis of T cells, coupled with severe autoimmune disorders. Strong evidence suggests that Treg cells represent a diverse cell population, comprising functionally distinct subsets that control different types of immune responses (Campbell and Koch, 2011; Josefowicz et al., 2012). The molecular mechanism that regulates the differentiation and function of the diverse Treg cells subsets remains poorly understood.
Recent studies have identified a specific subset of Treg cells, the follicular Treg cells (TFR cells), which are localized in the B cell follicles and specialized for the control of germinal center (GC) reactions (Chung et al., 2011; Linterman et al., 2011; Wollenberg et al., 2011). Formation of GCs is essential for various events of a T-dependent humoral immune response, such as antibody class switching, somatic hypermutation, and affinity maturation (Ramiscal and Vinuesa, 2013). The GC reactions depend on follicular T helper cells (TFH cells), a subset of CD4+ T effector cells which provide essential help to cognate B cells for their activation and differentiation in GCs (Linterman et al., 2012). The TFR cells resemble the TFH cells in that they express high levels of the chemokine receptor CXCR5, the inducible co-stimulator (ICOS), and the inhibitory receptor PD-1 (Linterman et al., 2012). However, in contrast to TFH cells, the TFR cells express Foxp3 and possess immunosuppressive function. It appears that the TFR cells are generated from CXCR5− Treg cells, instead of naive T cells, in response to T cell–dependent antigens. The TFR cell production requires the transcription factor Bcl-6 and is negatively regulated by the inhibitory receptor PD-1 (Chung et al., 2011; Linterman et al., 2011; Sage et al., 2013). However, the intracellular signaling events involved in the induction of TFR cells are largely unknown.
The TNF receptor (TNFR)–associated factors (TRAFs) form a family of signaling adaptors that mediate signal transduction from both the TNFRs and various other immune receptors (Ha et al., 2009). Among the TRAF family members, TRAF3 is particularly complex in signaling functions, which differ in the context of different receptors in different cell types (Hildebrand et al., 2011). In B cells, TRAF3 functions as a negative regulator of the noncanonical NF-κB signaling pathway and B cell survival. TRAF3 physically interacts with the NF-κB–inducing kinase (NIK) and mediates continuous degradation of this central component of the noncanonical NF-κB pathway (Liao et al., 2004). Thus, loss of TRAF3 causes constitutive activation of noncanonical NF-κB, coupled with B cell hyperplasia and aberrant production of antibodies (He et al., 2006; Xie et al., 2007; Gardam et al., 2008). Similar abnormalities have been observed in B cell conditional transgenic mice expressing a stable form of NIK that lacks the TRAF3-binding motif (NIKΔT3; Sasaki et al., 2008). In contrast to its negative role in B cell homeostasis, TRAF3 has a positive role in mediating TCR signaling and T cell–dependent immune responses (Xie et al., 2011). Interestingly, the TRAF3 deficiency is associated with an increase in the frequency of Treg cells, although the role of TRAF3 in regulating the homeostasis and function of Treg cells remains unknown (Hildebrand et al., 2011; Xie et al., 2011).
In the present study, we directly examined the function of TRAF3 in Treg cells by generating Treg cell–specific TRAF3 KO (Traf3Treg-KO) mice. We show that TRAF3 is dispensable for the homeostasis of the general population of Treg cells. However, TRAF3 has a particularly important role in the regulation of TFR cell generation and GC reactions. The Treg cell–specific TRAF3 deficiency severely inhibited the antigen-stimulated production of TFR cells, coupled with deregulated activation of TFH cells and heightened GC reactions. Consequently, the Traf3Treg-KO mice have elevated production of high-affinity antibodies of the IgG subtypes. Mechanistically, TRAF3 is required for maintaining the high-level expression of ICOS in Treg cells. We provide evidence that ICOS deficiency compromises the induction of TFR cells and the control of GC reactions. These findings shed light on the signaling mechanism that mediates TFR cell induction and identify TRAF3 as a crucial factor involved in this specific process.
RESULTS
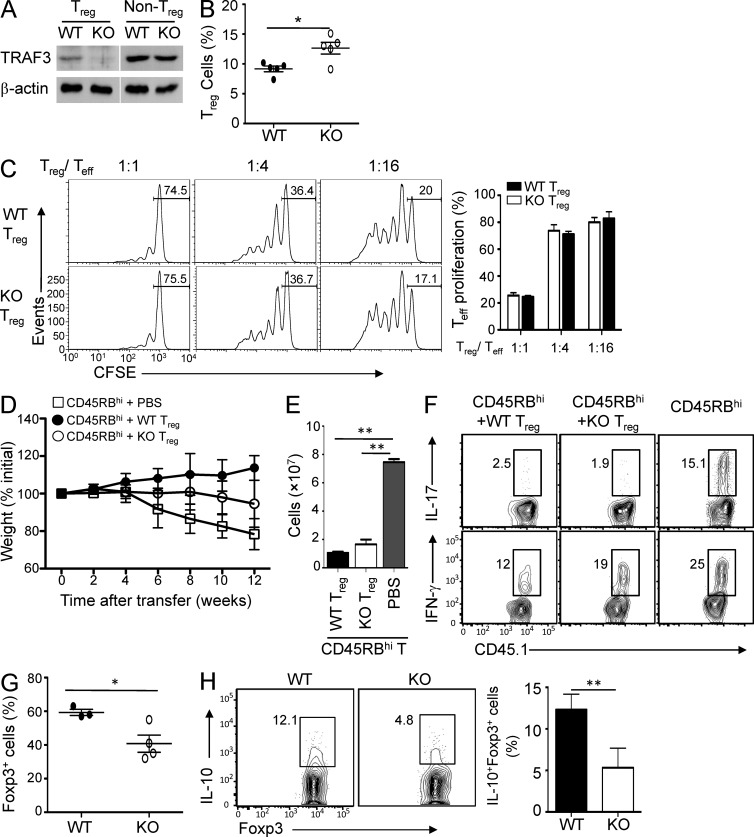
TRAF3 deficiency partially impaired the in vivo function of Treg cells
To study the function of TRAF3 in Treg cells, we generated Treg-conditional TRAF3 KO mice by crossing the Traf3-floxed mice with Foxp3-Cre mice (Fig. 1 A). Ablation of TRAF3 did not reduce, but even moderately increased, the frequency of Treg cells in the spleen (Fig. 1 B). To examine the effect of TRAF3 deficiency on the immunosuppressive function of Treg cells, we performed in vitro suppression assays using Treg cells purified from the spleen of WT and Traf3Treg-KO mice. The WT and TRAF3-deficient Treg cells had comparable efficiencies in suppressing the proliferation of naive T cells (Fig. 1 C), suggesting a dispensable role for TRAF3 in regulating the in vitro function of Treg cells.
Figure 1.
Treg cell–specific TRAF3 ablation does not reduce Treg cell frequency but partially impairs the in vivo function of Treg cells. (A) Treg (CD4+CD25+YFP+) and non-Treg (CD4+CD25−YFP−) T cells were sorted from the WT-R26YFP (WT) and Traf3Treg-KOR26YFP (KO) mice, and TRAF3 expression was assessed by immunoblot. β-Actin served as a loading control. (B) The frequency of Foxp3+ Treg cells (among CD3+CD4+ cells) in the spleen of WT and Traf3Treg-KO (KO) mice (6 wk old) was assessed by flow cytometry; data are presented as mean ± SD of five mice per group. Data are representative of five independent experiments. (C) Naive CD4+ T cells (Teff) were labeled with CFSE and activated by anti-CD3 plus antigen-presenting cells (irradiated splenocytes from WT mice, depleted of CD3+ T cells) in the presence of the indicated ratios of WT or KO Treg cells. Naive CD4+ T cell proliferation was measured as dilution of the cytosolic dye CFSE. Data are presented as a representative plot (left) and a summary graph (right) of six mice per genotype in three independent experiments. (D) Rag1-KO mice were adoptively transferred with WT B6.SJL CD45RBhi naive CD4+ T cells (CD45.1+) along with either PBS buffer or sorted Treg cells (CD45.1−), and body weight was monitored. (E and F) CD45RBhi CD4+ T cells (CD45.1+) were transferred into recipient mice as in D (on week 5), and the total number (E) and frequency (F) of Th1 and Th17 cells in the spleen of the recipient mice were assessed by ICS. Eight mice in two different experiments were used for each group. (G and H) The frequency of adoptively transferred Foxp3+ Treg cells (G) and IL-10–producing Treg cells (gated on Foxp3+ cells) in the spleen of the recipient mice described in D was determined by flow cytometry (5 wk after adoptive transfer; H). (C–E, G, and H) Mean ± SD is shown. Data are representative of two independent experiments. *, P < 0.05; and **, P < 0.01.
We next examined the in vivo function of Treg cells using a well-defined adoptive transfer model, which involved cotransfer of CD45RBhi naive CD4+ T cells with Treg cells purified from the WT and Traf3Treg-KO mice. As expected, adoptive transfer of CD45RBhi naive T cells into Rag1-KO mice induced severe body weight loss of the recipient mice, coupled with massive expansion of the transferred T cells, and these pathological phenotypes were efficiently blocked when the naive T cells were cotransferred with WT Treg cells (Fig. 1 D). Compared with the WT Treg cells, the TRAF3-deficient Treg cells exhibited a reduced ability to suppress the expansion and pathological activity of the naive T cells (Fig. 1, E and F). Although the mutant Treg cells remained fully functional in inhibiting the production of Th17 cells from the cotransferred naive CD4+ T cells, their ability to suppress the generation of Th1 cells was partially impaired (Fig. 1 F). After the adoptive transfer, a lower number of TRAF3-deficient Treg cells was recovered compared with that of the WT Treg cells (Fig. 1 G), suggesting reduced expansion or survival of the mutant Treg cells. Furthermore, they showed a reduced level of IL-10 production (Fig. 1 H). Collectively, these data suggest that Treg cell–specific TRAF3 deficiency does not compromise the homeostasis or in vitro function of Treg cells but partially impairs the in vivo functions of Treg cells.
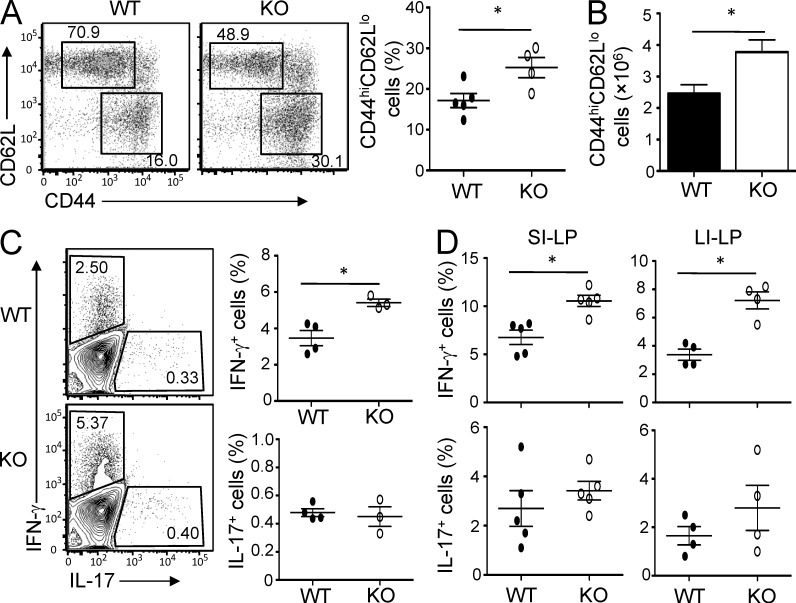
Altered CD4 T cell homeostasis in Traf3Treg-KO mice
To assess the function of the TRAF3-deficient Treg cells under nontransferred conditions, we examined the homeostasis of CD4+ T cells in peripheral lymphoid organs. The spleens and lymph nodes of the Traf3Treg-KO mice contained an enhanced frequency of CD4+ T cells with memory-like markers (CD44hiCD62Llo; Fig. 2, A and B). Among the memory-like CD4+ T cells in the peripheral lymphoid organs, there was a significant increase in the frequency of IFN-γ–producing Th1 cells in the Traf3Treg-KO mice, although the frequency of Th17 cells was generally low and not significantly different between the WT and mutant mice (Fig. 2 C).
Figure 2.
Altered CD4+ T cell homeostasis in Traf3Treg-KO mice. (A–D) Spleens (A–C; n = 4–5) or small and large intestine lamina propria (D; n = 6) were harvested from 8-wk-old WT or Traf3Treg-KO (KO) mice and analyzed by flow cytometry for the frequency (A) and absolute number (B) of memory-like (CD44hiCD62Llo) CD4+ T cells, and the frequency of IL-17– and IFN-γ–producing CD4+ T cells (C and D) was assessed using ICS. Mean ± SD is shown. Data are representative of five independent experiments. *, P < 0.05.
Treg cells play an important role in maintaining T cell homeostasis in the intestine, an organ with dynamic interactions between the immune system and microbiota (MacDonald et al., 2011). The Treg cell–specific TRAF3 deficiency resulted in a moderate increase in the frequency of CD4+ T cells, but not the CD8+ T cells, in the lamina propria of the small and large intestines (not depicted). Among the CD4+ T cells, there was a significantly increased frequency of Th1 cells in the lamina propria of Traf3Treg-KO mice (Fig. 2 D). Thus, the loss of TRAF3 in Treg cells altered the homeostasis of T cells, a finding which was consistent with the partially compromised function of the TRAF3-deficient Treg cells (Fig. 1, D–F). It is important to note, however, that the overall phenotype of the Traf3Treg-KO mice in T cell homeostasis was considerably milder compared with that observed in mutant mice lacking Foxp3 or its major regulators that mediate the development and core functions of Treg cells (Josefowicz et al., 2012). Moreover, the Traf3Treg-KO mice only displayed relatively mild tissue inflammation at older ages, mostly seen in the lung and the liver (not depicted). These results suggest that TRAF3 may regulate a specific function, instead of mediating the core suppressive activity, of Treg cells.
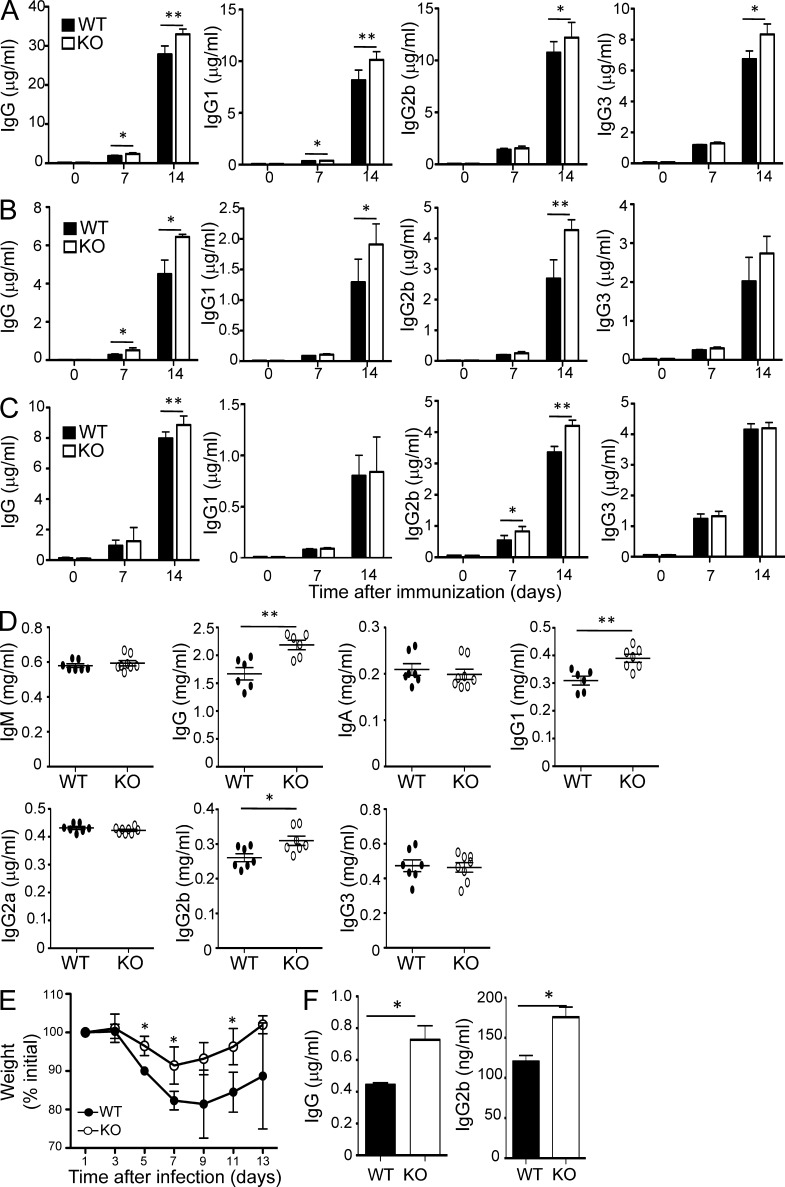
Treg cell–specific TRAF3 controls antigen-stimulated humoral immune responses
In addition to maintaining T cell homeostasis and preventing autoimmune diseases, Treg cells play an important role in modulating immune responses to foreign antigens. To examine the role of TRAF3 in mediating this latter function of Treg cells, we analyzed the effect of Treg cell–specific TRAF3 deficiency on the induction of antibodies by well-characterized protein and nonprotein antigens. Upon immunization of a protein antigen, sheep RBCs (SRBCs), the young Traf3Treg-KO and WT control mice produced comparable levels of IgM (not depicted). However, the Traf3Treg-KO mice produced significantly more IgG and its subtypes (Fig. 3 A). Similar results were obtained when the mice were immunized with another protein antigen composed of the hapten 4-hydroxy-3-nitrophenylacetyl (NP) conjugated to the carrier protein KLH (NP-KLH; Fig. 3 B). ELISA assays using NP9-BSA (for high affinity) and NP26-BSA (for global affinity) suggested that the Treg cell–specific TRAF3 ablation particularly enhanced the production of high-affinity antibodies (Fig. 3 B and not depicted). In response to immunization by a nonprotein antigen, NP-Ficoll, the production of high-affinity IgG, mainly IgG2b, was only moderately enhanced in the Traf3Treg-KO mice (Fig. 3 C).
Figure 3.
Treg cell–specific TRAF3 controls antigen-stimulated humoral immune responses. (A) WT and Traf3Treg-KO mice (8 wk old) were immunized i.p. with SRBCs, and serum SRBC–specific Ig was measured 14 d later by ELISA (n = 5). (B and C) WT and Traf3Treg-KO mice (6–8 wk old) were immunized i.p. with KLH-NP26 (B) or Ficoll-NP26 for 12 d (C), and NP9 (high affinity) Ig was measured 12 d later by ELISA (B: n = 4; C: n = 9). (D) Basal concentrations of Ig isotypes and IgG subclasses in the sera of 18–20-wk-old WT and Traf3Treg-KO mice were measured by ELISA (n = 7). (E and F) WT and Traf3Treg-KO mice (8 wk old; n = 10) were intranasally infected with influenza virus H1N1 and monitored for bodyweight loss (E) and serum anti-H1N1 IgG antibody titer on day 13 (F). (A–F) Mean ± SD is shown. Data are representative of four (A–D) or two (E and F) independent experiments. *, P < 0.05; and **, P < 0.01.
We also examined the effect of TRAF3 deficiency on the basal level of antibodies in different ages of mice. At a young age, the WT and Traf3Treg-KO mice had comparable serum concentrations of antibodies (not depicted). However, older Traf3Treg-KO mice (18–20 wk old) had an elevated basal level of serum IgG, particularly IgG1 and IgG2b (Fig. 3 D). These results suggest that expression of TRAF3 in Treg cells is important for controlling the magnitude of humoral immune responses, especially the production of high-affinity IgG antibodies.
To further assess the role of Treg cell–specific TRAF3 in mediating humoral immune responses, we used a model of influenza infection, which is known to trigger strong T cell–dependent antibody responses (Elsner et al., 2012). As expected, the WT mice experienced bodyweight loss after the intranasal infection with the A/PR8 (H1N1) strain of influenza virus (Fig. 3 E). Importantly, under the same infection conditions, the Traf3Treg-KO mice had much less bodyweight reduction compared with the WT mice (Fig. 3 E). Moreover, the Traf3Treg-KO mice also produced significantly higher levels of antiviral IgG antibodies (Fig. 3 F). These results emphasize the biological significance of the TRAF3-mediated Treg cell regulation.
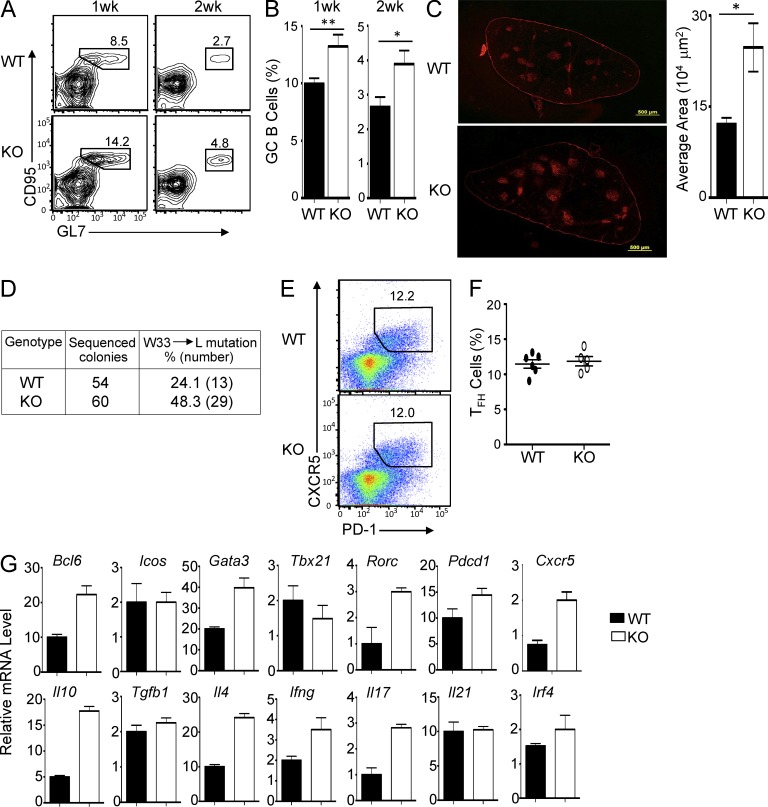
Treg cell–specific TRAF3 regulates TFH cell function and GC formation
A hallmark of T cell–dependent antibody responses is the formation of GCs, which are required for various events of the humoral immune response, including antibody class switching, somatic hypermutation, and affinity maturation (Ramiscal and Vinuesa, 2013). Because the Treg cell–specific TRAF3 deficiency preferentially promoted the production of high-affinity antibodies of a major secondary isotype, IgG, we examined the role of TRAF3 in regulating GC formation by flow cytometry, based on the typical surface markers of GC B cells. As expected, immunization of the WT animals with SRBCs induced production of GC B cells, which peaked around 1 wk and declined around 2 wk after the immunization (Fig. 4 A). Importantly, the Traf3Treg-KO mice produced a markedly higher frequency of GC B cells than the WT mice (Fig. 4, A and B). Parallel immunofluorescence assays also revealed the formation of enlarged GCs in the spleen of the Traf3Treg-KO mice after SRBC immunization (Fig. 4 C).
Figure 4.
Treg cell–specific TRAF3 regulates TFH cell function and GC formation. (A and B) WT and Traf3Treg-KO (KO) mice (8 wk old) were immunized i.p. with SRBCs, and the frequency of GC B cells (CD95+GL7+) among B220+ cells was assessed by flow cytometry. Data are presented as a representative plot (A) and mean ± SD based on five mice for each group (B). (C) Mice were immunized as in A and B, and GCs were analyzed by immunofluorescence detection of PNA+ cells. Graph shows average GC areas as mean ± SD based on multiple slides. Data are representative of four WT and three Traf3Treg-KO (KO) mice. Bars, 500 µm. (D) Frequency of W33 to L mutation in the GC B cells of SRBC-immunized WT and Traf3Treg-KO mice (10 d after immunization), determined by sequencing the cDNA clones constructed using pooled RNA from six WT and six KO mice. (E and F) WT-R26YFP (WT) or Traf3Treg-KOR26YFP (KO) mice were immunized as in A, and 10 d later, the frequency of TFH cells (CXCR5+PD-1+) among CD4+YFP− T cells was assessed by flow cytometry. Data are presented as a representative plot (E) and mean ± SD (F) based on six mice for each group. (G) TFH cells were sorted from the spleens of the WT and KO mice in E and F, and expression of the indicated genes was assessed by RT-PCR. Mean ± SEM is shown. Data in A–G are representative of three to four independent experiments. *, P < 0.05; and **, P < 0.01.
Formation of GCs is associated with antibody somatic hypermutations, a mechanism which generates high-affinity antibodies (Allen et al., 1987; Weiss et al., 1992). Given the enhanced GC formation in Traf3Treg-KO mice, we analyzed the antibody somatic hypermutation frequency in the immunized WT and Traf3Treg-KO mice based on the tryptophan (W) 33 to leucine (L) hotspot mutation in the Ig heavy chain variable gene VH186.2 (Allen et al., 1988). Consistent with the elevated GC formation in the Traf3Treg-KO mice, these mutant animals had a profoundly higher frequency of W33 to L mutations (Fig. 4 D).
GC formation and antibody class switching are dependent on TFH subtype of CD4+ helper T cells. We found that in response to SRBC immunization, the WT and Traf3Treg-KO mice produced a comparable frequency of TFH cells (Fig. 4, E and F). Interestingly, however, the TFH cells derived from the Traf3Treg-KO mice displayed hyperexpression of genes encoding several cytokine genes, including IL-4, IL-10, IL-17, and IFN-γ (Fig. 4 G). Furthermore, the expression of several transcription factors, such as Bcl-6, Gata-3, and RORγt, were also elevated in the TFH cells derived from the immunized Traf3Treg-KO mice (Fig. 4 G). Of note, TFH cells are known to produce different effector cytokines depending on the nature of antigens, which appears to influence the antibody class switching in a humoral immune response (Bauquet et al., 2009; Linterman et al., 2012). Several of these cytokines, IL-4, IL-17, and IFN-γ, have been shown to mediate B cell help and induction of antibody class switching toward the generation of different IgG subtypes (Bauquet et al., 2009; Mitsdoerffer et al., 2010; Linterman et al., 2012). Thus, the perturbed TFH cell activation provided explanations for the aberrant formation of GCs and hyper production of IgG isotypes in Traf3Treg-KO mice.
TRAF3 is important for TFR cell induction
Recent studies identified a subset of Treg cells, the TFR cells, which controls the function of TFH cells and GC reactions (Chung et al., 2011; Linterman et al., 2011; Wollenberg et al., 2011). TFR cells are characterized by expression of the chemokine receptor CXCR5, which mediates their migration into the lymphoid follicles (Linterman et al., 2012). In addition, the TFR cells also express high levels of the co-inhibitory molecule PD-1 and the transcription factor Bcl-6, respectively exerting negative and positive roles in TFR regulation (Chung et al., 2011; Linterman et al., 2011; Wollenberg et al., 2011; Sage et al., 2013).
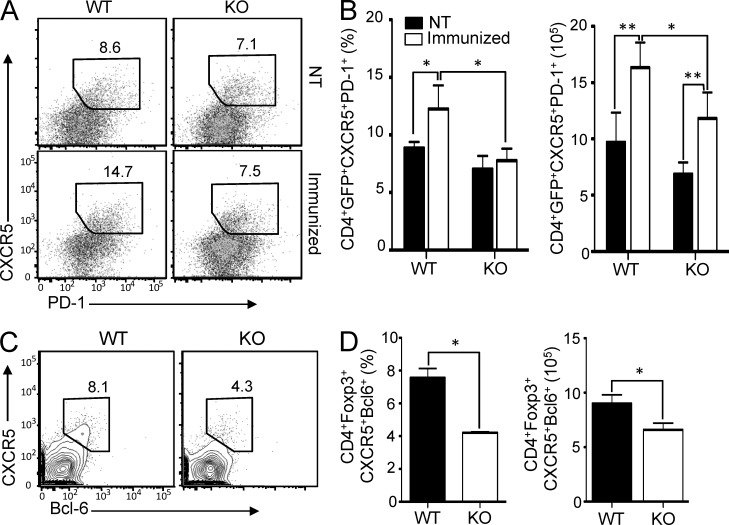
The particularly prominent phenotype of the Traf3Treg-KO mice in TFH cell activation and humoral immune responses prompted us to examine the induction and function of TFR cells. We analyzed the TFR cells based on their surface expression of CXCR5 and PD-1 within the population of GFP+ (expressed from the Foxp3-GFP-hCre transgene) Treg cells. As expected, the spleens of the WT mice contained a small population of CXCR5+PD-1+GFP+ TFR cells, and this population was significantly increased in response to SRBC immunization (Fig. 5, A and B). Under unimmunized conditions, the TFR frequency of the Traf3Treg-KO mice was only moderately lower than that of the WT mice (Fig. 5, A and B). However, these mutant animals were attenuated in antigen-stimulated production of TFR cells after SRBC immunization (Fig. 5, A and B). To further confirm this remarkable result, we stained the TFR cells based on their surface expression of CXCR5 and intracellular expression of Bcl-6 and Foxp3. This method once again revealed a defect of the Traf3Treg-KO mice in TFR cell production in response to immunization with SRBCs (Fig. 5, C and D). Thus, although TRAF3 is dispensable for the homeostasis of Treg cells, it is important for the induction of a specific subset of Treg cells, the TFR cells, involved in the control of GC formation and humoral immune responses. This finding explains the aberrant induction of GCs and high-affinity antibodies in the Traf3Treg-KO mice.
Figure 5.
TRAF3 is required for TFR cell induction. (A and B) WT-R26YFP and Traf3Treg-KO-R26YFP (KO) mice (8 wk old) were immunized with SRBCs, and 10 d later, the frequency of TFR cells (CXCR5+PD-1+YFP+CD4+) in the spleen was assessed by flow cytometry. Data are presented as a representative plot (A) and mean ± SD (B) based on eight WT and nine KO mice. (C and D) Mice were immunized as in A and B, and the frequency and absolute number of TFR cells was assessed by flow cytometry based on surface staining of CXCR5 and intracellular staining of Bcl-6 within Foxp3+CD4+ Treg cells. Data are presented as a representative plot (C) and mean ± SD (D) based on eight WT and nine KO mice. (A–D) Data are representative of three to four independent experiments.*, P < 0.05; and **, P < 0.01.
TRAF3 mediates ICOS gene expression in Treg cells
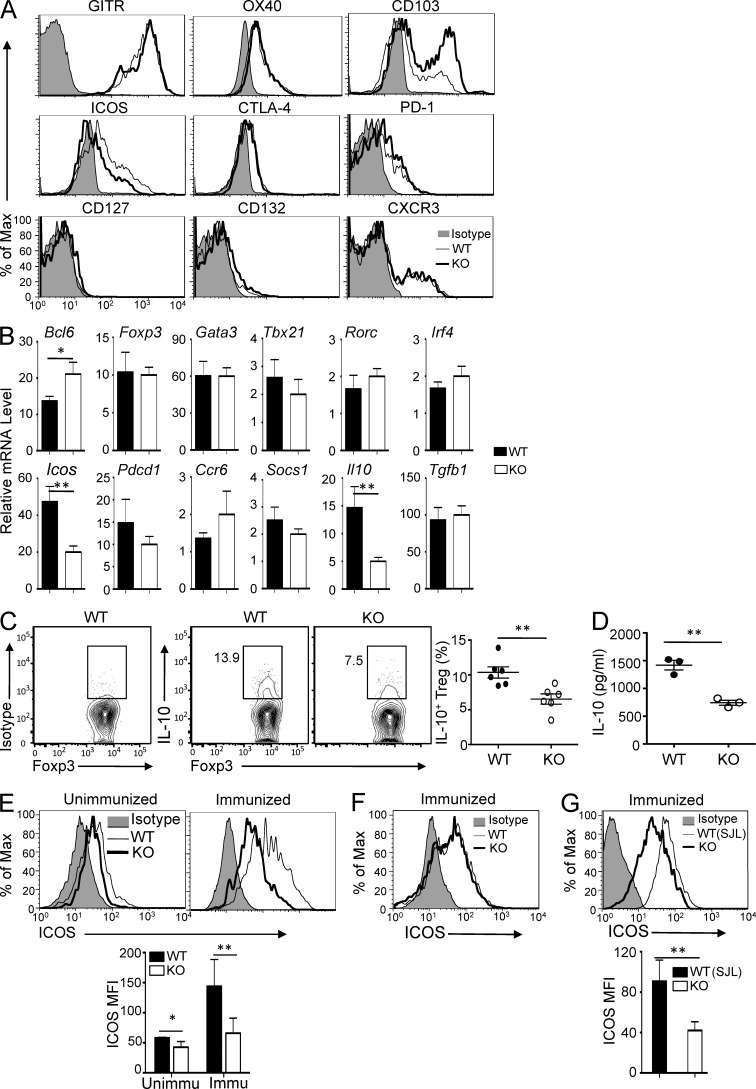
To assess the molecular mechanism by which TRAF3 regulates Treg cell function, we examined the expression of signature molecules on WT and TRAF3-deficient Treg cells. Although the TRAF3 deficiency did not affect the expression of most of the Treg cell surface markers analyzed, it caused an increase in the frequency of CD103hi Treg cell populations (Fig. 6 A). The increase in CD103hi Treg cells might be caused by their elevated activation, as expression of this molecule is known to be associated with effector/memory type Treg cells (Huehn et al., 2004). Interestingly, the TRAF3-deficient Treg cells had a profound reduction in the expression level of ICOS (Fig. 6 A), a co-stimulatory molecule thought to mediate specific Treg cell functions, such as IL-10 gene induction and TFR cell development (Ito et al., 2008; Busse et al., 2012; Redpath et al., 2013; Sage et al., 2013). QPCR analysis further confirmed the defect in Icos gene expression (Fig. 6 B). Moreover, the TRAF3-deficient Treg cells were also impaired in the induction of IL-10 expression (Fig. 6, B–D). These findings further suggest the involvement of TRAF3 in the regulation of specific aspects of Treg cell functions.
Figure 6.
TRAF3 mediates ICOS gene expression via a MAP kinase pathway in Treg cells. (A) Expression of the indicated surface markers on Foxp3+CD4+ Treg cells from the spleens of WT and Traf3Treg-KO mice (6 wk old) was assessed by flow cytometry. (B) Expression of the indicated genes in Treg cells from 6-wk-old WT or Traf3Treg-KO (KO) mice was assessed by RT-PCR. Mean ± SEM is shown. (C) The frequency of IL-10–producing cells among YFP+CD4+ Treg cells from the spleen of WT-R26YFP (WT) and Traf3Treg-KO-R26YFP (KO) mice was assessed by flow cytometry. Data are presented as a representative plot (left) and the mean ± SD of six mice for each group. The left panel of C shows the isotype control for IL-10 ICS. (D) GFP+CD25+CD4+ Treg cells were sorted from the spleens of three WT and three KO mice and stimulated for 24 h with PMA and ionomycin. IL-10 secretion was measured by ELISA. (E and F) WT or Traf3Treg-KO (KO) mice (6 wk old; n = 5) were immunized with SRBCs, and 10 d later, ICOS expression in TFR (E) or TFH (F) cells was assessed by flow cytometry. Graph in E shows the mean fluorescence intensity (MFI) of ICOS based on five mice for each group. (D–F) Mean ± SD is shown. (G) Rag1-KO recipient mice were adoptively transferred with 1:1 ratio of mixed bone marrows of WT (B6.SJL, CD45.1+) and Traf3Treg-KO (KO, CD45.2+) mice. 6 wk later, mice were immunized with SRBCs, and ICOS expression on gated WT (CD4+CD45.1+Foxp3+) and KO (CD4+CD45.2+Foxp3+) Treg cells was assessed by flow cytometry at day 10 after immunization. Graph shows MFI as mean ± SD from four mice for each group. Data are representative of three to four (A–F) or two (G) independent experiments. *, P < 0.05; and **, P < 0.01.
Because Traf3Treg-KO mice had a defect in TFR cell induction, we tested whether TRAF3 was required for antigen-stimulated ICOS expression on TFR cells. As seen with the total Treg cells, ICOS expression was reduced on TFR cells under unimmunized conditions (Fig. 6 E). Importantly, the defect of the TRAF3-deficient TFR cells in ICOS expression became much more drastic after immunization of the mice with the protein antigen SRBCs (Fig. 6 E). Furthermore, this defect appeared to be cell intrinsic because it was not detected in the Foxp3− non-Treg cells (Fig. 6 F). A mixed bone marrow adoptive transfer experiment revealed that the TRAF3-deficient Treg cells had reduced ICOS expression even when they were developed in the presence of WT Treg cells in the same recipient mice (Fig. 6 G), thus further suggesting a cell-intrinsic role for TRAF3 in the regulation of ICOS expression in Treg cells.
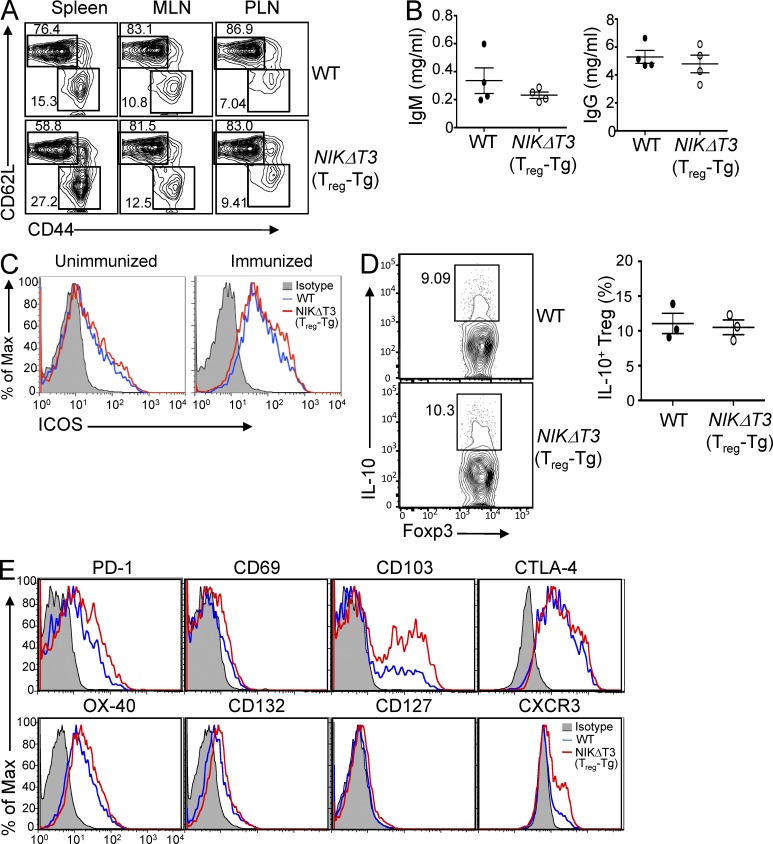
NIK overexpression does not inhibit ICOS expression
The signaling function of TRAF3 is complex and may vary among cell types (Hildebrand et al., 2011). TRAF3 is known to bind to NIK and mediate NIK degradation, thereby negatively regulating the noncanonical NF-κB signaling (Sun, 2012). Loss of TRAF3 causes accumulation of NIK and constitutive activation of noncanonical NF-κB in B cells and T cells (Liao et al., 2004; He et al., 2006; Xie et al., 2007; Gardam et al., 2008). To examine how TRAF3 regulates ICOS expression, we examined the potential involvement of noncanonical NF-κB activation. We used a transgenic mouse expressing a stabilized form of NIK lacking its TRAF3-binding motif (NIKΔT3) under the control of a loxP-flanked stop cassette (Sasaki et al., 2008). By crossing these mice with the Foxp3-GFP-hCre mice, we generated Treg-conditional NIKΔT3 transgenic (NIKΔT3Treg-Tg) mice. As seen with the Traf3Treg-KO mice, the NIKΔT3Treg-Tg mice displayed a moderate increase in memory-like effector T cells (Fig. 7 A). This result suggested that deregulated noncanonical NF-κB activation might partially impair the function of Treg cells. However, the NIKΔT3Treg-Tg mice did not show obvious abnormalities in antibody responses (Fig. 7 B) or reduced expression of ICOS and IL-10 in Treg cells (Fig. 7, C and D). In fact, the level of ICOS was even slightly enhanced in these mutant Treg cells (Fig. 7 C), probably reflecting their abnormal activation. Consistent with this idea, another activation marker, CD103, was also enhanced on the NIKΔT3 Treg cells (Fig. 7 E).
Figure 7.
NIK overexpression in Treg cells does not inhibit the expression of ICOS and IL-10 or perturb antibody production. (A) The frequency of memory (CD44hiCD62Llo) and naive (CD44loCD62Lhi) CD4+ T cells in WT and NIKΔT3Treg-Tg mice (12 wk old; n = 4) was analyzed by flow cytometry. (B) Serum IgM and IgG in unmanipulated WT and NIKΔT3Treg-Tg mice (12–16 wk old; n = 4) was measured by ELISA. (C) Expression of ICOS in CD4+Foxp3+ T cells from WT and NIKΔT3Treg-Tg mice (6 wk old; n = 3) was assessed by flow cytometry. (D) Frequency of IL-10–producing cells among GFP+CD4+ Treg cells from the spleen of WT and NIKΔT3Treg-Tg mice (6 wk old; n = 3) was measured by ICS. (B and D) Mean ± SD is shown. (E) Expression of the indicated surface markers on Foxp3+CD4+ Treg cells from the spleens of WT and NIKΔT3Treg-Tg mice (8 wk old) was assessed by flow cytometry. Data are representative of four independent experiments.
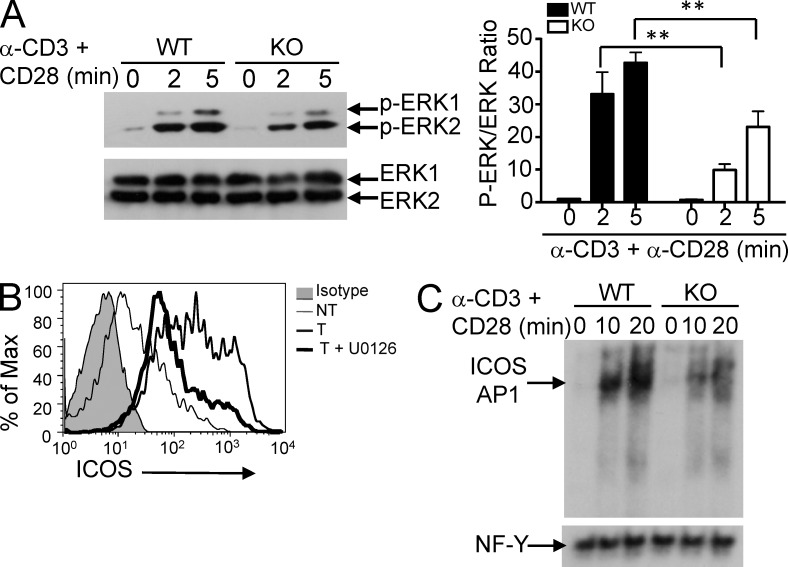
TRAF3-mediated ICOS induction involves activation of ERK and AP1
In conventional T cells, TRAF3 has a role in mediating TCR-stimulated activation of the MAP kinase ERK (Xie et al., 2011). We found that loss of TRAF3 in Treg cells also inhibited the activation of ERK by the TCR and CD28 signals (Fig. 8 A). To test whether attenuated ERK activation contributed to the reduced expression of ICOS in Treg cells, we used a selective ERK inhibitor, U0126. Indeed, the ERK inhibitor severely inhibited the induction of ICOS expression (Fig. 8 B). ICOS promoter contains an AP1-binding site that is important for promoter activation by the TCR/CD28 signals (Watanabe et al., 2012). Consistently, we found that cross-linking the TCR and CD28 in WT T cells led to rapid activation of AP1 that bound to the ICOS AP1 probe (Fig. 8 C). Moreover, the TRAF3 deficiency attenuated the activation of AP1 (Fig. 8 C). These findings suggest that TRAF3 regulates ICOS gene induction via an ERK–AP1 signaling pathway.
Figure 8.
TRAF3 mediates TCR/CD28-stimulated activation of ERK and AP1. (A) Treg cells (CD4+YFP+CD25+) were sorted from WT-R26YFP and Traf3Treg-KO-R26YFP mice and stimulated for the indicated time periods with anti-CD3 plus anti-CD28 using a cross-linking method. Levels of total and phosphorylated ERK1,2 were assessed by immunoblot. Data are presented as a representative blot (left) and a summary graph based on quantification of three independent blots (right). Mean ± SD is shown. (B) ICOS expression on sorted WT Treg cells that were either not treated (NT) or treated with anti-CD3 plus anti-CD28 in the absence (T) or presence (T + U0126) of an ERK inhibitor, 50 µM U0126, for 24 h was assessed by flow cytometry. (C) Nuclear extracts were prepared from WT or TRAF3-deficient CD4+ T cells stimulated with anti-CD3 plus anti-CD28 for the indicated time periods, and EMSA was performed using ICOS AP1 or the control NF-Y oligonucleotide probes. Data are representative of three independent experiments. **, P < 0.01.
ICOS expression in Treg cells is required for the formation and function of TFR cells
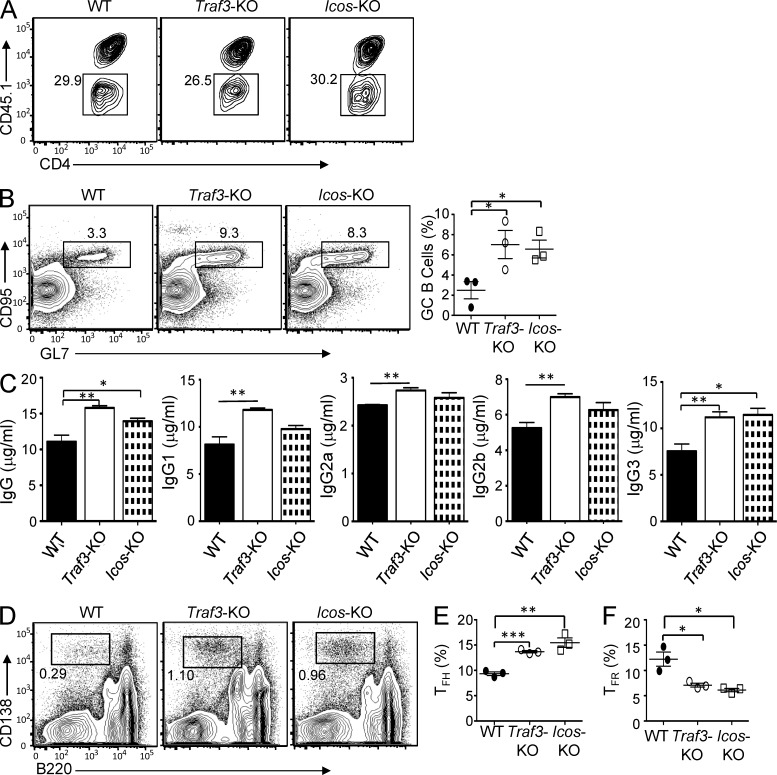
A recent study suggests that Icos-KO mice have a defect in TFR cell induction, although it is unclear whether this function is cell intrinsic (Sage et al., 2013). We used a Treg cell adoptive transfer model to examine whether the expression of ICOS in Treg cells is required for the development and function of TFR cells. We adoptively transferred the T cell–deficient Tcrb/Tcrd double KO (Tcrb/Tcrd-dKO) mice with WT naive CD4+ T cells together with Treg cells purified from WT, Traf3Treg-KO, or Icos-KO mice and then challenged the mice with SRBC antigen. The different Treg cells were highly similar in homeostasis after the adoptive transfer (Fig. 9 A). In contrast, although the WT Treg cells efficiently suppressed the induction of GCs in the immunized recipient mice, the TRAF3-deficient Treg cells were largely defective in this function (Fig. 9 B). The similar deficiency was observed with the ICOS-deficient Treg cells (Fig. 9 B).
Figure 9.
ICOS is essential for controlling TFH cell function and GC formation. Sorted naive CD4+ T cells (CD4+CD62LhiCD44loCD25−) from WT B6.SJL mice (5 wk old; CD45.1+) and sorted Treg T cells (CD4+YFP+CD25+) from WT, Traf3Treg-KO (Traf3-KO), or Icos-KO mice (6 wk old; CD45.2+) were mixed in a 5:1 ratio and intravenously transferred into Tcrb/Tcrd-dKO mice. 2 d later, recipient mice were immunized with SRBCs and sacrificed for experiments 14 d after immunization. (A) Frequency of Treg cells (CD45.1−) and naive CD4+ T cells (CD45.1+) in the spleen of Tcrb/Tcrd-dKO recipients was assessed by flow cytometry. (B) Frequency of GC B cells (GL7+CD95+) among B220+ cells was assessed by flow cytometry. Data are presented as a representative plot (left) and mean ± SD (right) based on three mice for each group. (C) SRBC-specific antibody levels in the sera of Tcrb/Tcrd-dKO recipient mice transferred with WT, Traf3-KO, and Icos-KO Treg cells was assessed by ELISA. Mean ± SD is shown. (D) Frequency of plasma cells (B220−CD138+) in the spleens of the Tcrb/Tcrd-dKO recipients was assessed by flow cytometry. (E and F) Frequency of the TFH (CXCR5+PD-1+Foxp3−CD4+) cells among CD4+Foxp3− T cells (E) and the frequency of TFR (CXCR5+PD-1+GFP+CD4+) cells among CD4+Foxp3+ Treg cells (F) were assessed by flow cytometry. Data are presented as mean ± SD based on three mice for each group and are representative of two independent experiments. *, P < 0.05; **, P < 0.01; and ***, P < 0.001.
We next examined the production of high-affinity IgG antibodies in the immunized recipient mice. Consistent with the deficiency of the Traf3-KO and Icos-KO Treg cells in suppressing the GC formation, they also displayed attenuated function in the control of IgG production compared with the WT Treg cells (Fig. 9 C). Moreover, the recipient mice of Traf3-KO and Icos-KO Treg cells contained substantially higher levels of plasma cells (Fig. 9 D) and TFH cells (Fig. 9 E), coupled with reduced frequency of TFR cells (Fig. 9 F). Collectively, these data suggest that TRAF3 and ICOS have a Treg cell–intrinsic role in mediating the generation and function of TFR cells.
DISCUSSION
The Foxp3+ Treg cells represent a functionally diverse population composed of subsets that regulate different immune functions (Campbell and Koch, 2011; Josefowicz et al., 2012). The signaling mechanism that regulates the functional diversity of Treg cells is still poorly understood. In the present study, we have identified TRAF3 as a signaling factor that mediates the effector function of Treg cells, particularly their control of GC formation and antibody responses. Our data suggest that TRAF3 is involved in the induction of the recently defined TFR cells, a subset of Treg cells specialized in the control of GC reactions (Chung et al., 2011; Linterman et al., 2011; Wollenberg et al., 2011). Consequently, the mice with Treg cell–specific TRAF3 deficiency display heightened responses to antigens in the formation of GCs and production of high-affinity antibodies.
A recent study suggests that TRAF3 ablation in total T cells, by crossing the Traf3-floxed mice with CD4-Cre mice, causes an increase in the percentage of Foxp3+ Treg cells (Xie et al., 2011). Because TRAF3 is knocked out during the double-positive stage of thymocyte development in this approach, it is thought that TRAF3 may regulate the development of Treg cells (Hildebrand et al., 2011). Our present study revealed that ablation of TRAF3 in committed Treg cells, using the Foxp3-Cre system, also caused a moderate, but significant, increase in the Treg cell frequency. Our finding is consistent with the previous observation and further suggests that TRAF3 may negatively regulate both the early development and the late-stage maturation or survival of Treg cells. Interestingly, despite their increased Treg cell frequency, the Traf3Treg-KO mice had impaired conventional T cell homeostasis, characterized by an increase in the percentage of CD4+ T cells with memory/effector surface markers. This result suggests a positive role for TRAF3 in the regulation of Treg cell function. In contrast, the phenotype of the Traf3Treg-KO mice in T cell homeostasis is considerably weaker than that observed in mice lacking Foxp3 or other factors required for the development and core functions of Treg cells. The Traf3Treg-KO mice also had only moderate immune cell infiltrations in the nonlymphoid tissues, particularly the lung. Consistently, adoptive transfer experiments revealed that the TRAF3-deficient Treg cells had weakly reduced ability to suppress the expansion and pathogenesis of CD4+ T cells. We observed reduced expression of IL-10 in the TRAF3-deficient Treg cells, which may contribute to their partially impaired function in maintaining immune homeostasis.
Despite the relatively weak phenotype in immune homeostasis, the Traf3Treg-KO mice had a prominent abnormality in antigen-stimulated GC reactions. In response to T-dependent antigens, these mutant animals formed enlarged GCs in the spleen and produced markedly more GC B cells, coupled with hyper production of high-affinity IgG subtypes. Gene expression analyses suggest the aberrant activation of TFH cells. Of particular interest is the elevated production of various effector cytokines, including IL-4, IL-10, IL-17, and IFN-γ, by the TFH cells derived from the immunized Traf3Treg-KO mice. Production of these cytokines by normal TFH cells has been observed previously and thought to regulate B cell proliferation and antibody class switching (Rousset et al., 1992; King et al., 2008; Bauquet et al., 2009; Mitsdoerffer et al., 2010). Thus, deregulated production of these effector cytokines by TFH cells may contribute to the heightened GC formation and antibody responses in the Traf3Treg-KO mice. The aberrant TFH cell activation was apparently caused by the defect of these mutant animals in producing TFR cells. Upon immunization with a T-dependent antigen, the WT mice had a substantial increase in the TFR cells, whereas the Traf3Treg-KO mice were severely attenuated in this response. In an adoptive transfer model, the TRAF3-deficient Treg cells also displayed a severe defect in generating TFR cells and suppressing GC responses. Under the transfer conditions, the TRAF3-deficient Treg cells also had significantly reduced ability to suppress the production of TFH cells. These results suggest that TRAF3 may regulate a signaling pathway in Treg cells that is particularly important for their conversion into TFR cells during an immune response.
The generation of TFR cells from Foxp3+ Treg cells is critically dependent on the transcription factor Bcl-6 (Chung et al., 2011; Linterman et al., 2011; Wollenberg et al., 2011). Our data suggested that TRAF3 is not required for expression of Bcl-6 or the various Treg cell signature molecules. Instead, TRAF3 appeared to be required for maintaining the high-level expression of ICOS in Treg cells because the TRAF3 deficiency greatly reduced, although did not completely block, the expression of ICOS at both RNA and protein levels. By using an adoptive transfer approach, we obtained in vivo evidence that ICOS expression in Treg cells is crucial for Treg cell–mediated suppression of GC formation and antibody responses. Like the TRAF3-deficient Treg cells, the ICOS-deficient Treg cells were severely attenuated in the generation of TFR cells and suppression of GC induction in response to immunization. These findings provide a mechanistic insight into the function of TRAF3 in regulating TFR cell production and antibody responses. We believe that ICOS induction is an important, but probably not the only, mechanism by which TRAF3 regulates TFR cell induction and antibody responses.
The signaling function of TRAF3 is complex and differs in different cell types and in the context of different receptors (Hildebrand et al., 2011). One important function of TRAF3 is to mediate degradation of NIK and, thereby, negatively regulate the noncanonical NF-κB signaling (Liao et al., 2004). This negative signaling function of TRAF3 is particularly important for maintaining normal homeostasis and function of B cells, although its role in other cell types remains unclear (He et al., 2006; Xie et al., 2007; Gardam et al., 2008). Our data suggest that the activation of noncanonical NF-κB might contribute to the moderate defect of the TRAF3-deficient Treg cells in maintaining CD4+ T cell homeostasis because perturbed CD4+ T cell homeostasis was also detected in mice with conditional expression of stable form of NIK (NIKΔT3Treg-Tg mice). However, the noncanonical NF-κB activation is unlikely responsible for the functional defect of the TRAF3-deficient Treg cells in the regulation of GC reactions. Unlike the TRAF3 deficiency, conditional expression of NIKΔT3 in Treg cells did not cause hyperproduction of IgG or other antibody isotypes. The NIKΔT3-expressing Treg cells did not show any defect in ICOS expression either. Instead, our data suggest a positive role for TRAF3 in mediating the TCR signaling in Treg cells. As seen in conventional T cells (Xie et al., 2011), the loss of TRAF3 in Treg cells resulted in attenuated activation of the MAP kinase ERK. We obtained evidence that ERK is important for TCR-stimulated ICOS expression in Treg cells.
In summary, we have identified TRAF3 as a signaling factor that mediates the effector function of Treg cells, particularly in the control of humoral immune responses. Although TRAF3 is dispensable for the homeostasis of Treg cells, it is crucial for antigen-stimulated production of TFR cells. Our data suggest that the Treg cell regulatory function of TRAF3 involves induction of the co-stimulatory molecule ICOS, which is the result of impaired ERK activation. Our study has also revealed the requirement of Treg cell–specific ICOS in the induction of TFR cells and the control GC responses. These findings not only establish a novel role of TRAF3 in the regulation of Treg cell function and humoral immune responses, but also shed new light onto the signaling mechanism regulating the specific functions of Treg cells.
MATERIALS AND METHODS
Mice.
Foxp3-GFP-hCre BAC transgenic mice (Zhou et al., 2008; The Jackson Laboratory) were backcrossed for nine generations to the C57BL/6 background and then crossed with Traf3-floxed mice (C57BL/6 background; Gardam et al., 2008) to produce age-matched Traf3+/+Foxp3GFP-hCre (termed WT) and Traf3fl/flFoxp3GFP-hCre (termed Traf3Treg-KO) mice. In some experiments, these mice were further crossed with the Rosa26-YFP Cre reporter (termed R26YFP; C57BL/6J background; The Jackson Laboratory) to generate WT and Traf3Treg-KO mice that express YFP in their Treg cells (termed WT-R26YFP and Traf3Treg-KOR26YFP mice, respectively). The Traf3-floxed mice were also crossed with CD4-Cre (C57BL/6 background; The Jackson Laboratory) mice to produce mice harboring TRAF3 deletion in total T cells (called Traf3TKO mice). NIKΔT3 mice (C57BL/6 background; The Jackson Laboratory) express a stabilized form of NIK lacking the TRAF3-binding motif (NIKΔT3) from the Rosa26 locus under the control of a loxP-flanked stop cassette (Sasaki et al., 2008). These mice were crossed with the Foxp3-GFP-hCre mice (backcrossed to C57BL/6 background) to generate Treg-conditional NIKΔT3 transgenic (NIKΔT3Treg-Tg) and internal WT control mice. B6.SJL (expressing the CD45.1 congenic marker), Tcrb/Tcrd-dKO, Icos-KO, and Rag1-KO mice (all in C57BL/6 background) were obtained from the Jackson Laboratory. For all experiments, WT littermates were used as controls. Mice were maintained in a specific pathogen–free facility of the University of Texas MD Anderson Cancer Center, and all animal experiments were performed in accordance with protocols approved by the Institutional Animal Care and Use Committee of the University of Texas MD Anderson Cancer Center.
Cell preparation and flow cytometry analysis.
Mononuclear cells were isolated from the spleen and intestinal lamina propria as previously described (Reiley et al., 2006; Chang et al., 2012). Treg cells were purified by flow cytometric cell sorting based on their expression of CD25 and the YFP marker from WT-R26YFP or Traf3Treg-KO-R26YFP mice. Flow cytometric analyses and cell sorting were performed (Reiley et al., 2006) using a FACSCalibur (BD) and FACSAria (BD), respectively. For intracellular cytokine staining (ICS), cells were stimulated with 50 ng/ml PMA plus 750 ng/ml ionomycin for 4–6 h in the presence of 10 µg/ml monensin, and the fixed cells were incubated with the indicated antibodies and subjected to flow cytometry. FITC-conjugated anti-CD95 (BD); PE-conjugated anti–PD-1, anti-CD138, anti–Bcl-6, anti-CTLA4, and anti-CXCR3 (BD); allophycocyanin (APC)-conjugated anti-GL7 and anti-CXCR5 (BD Bioscience); and PE-Cy7–conjugated anti-CD8 and anti-CD4 (eBioscience) were used. Other antibodies were described previously (Chang et al., 2012).
Mouse immunization.
Age-matched WT and Traf3Treg-KO mice (6–8 wk old) were immunized i.p. with 2 × 109 SRBCs (Cocalico Biologicals), 100 µl NP-KLH (1 mg/ml), or 100 µl NP-Ficoll (1 mg/ml) and sacrificed at the indicated times for analyzing serum antibody concentration and GC formation.
Influenza viral infection.
WT and Traf3Treg-KO mice were subjected to intranasal infection with a nonlethal dose (25 tissue culture ID50 units in 25 µl PBS per mouse) of influenza virus A/PR8 (H1N1) under isoflurane anesthesia. Body weight change was monitored every another day for 13 d. On day 13, influenza-specific antibodies in the serum were detected by ELSIA as described previously (Elsner et al., 2012). In brief, ELISA plates were coated with influenza virus overnight at 4°C, blocked with 1% BSA in PBS, and then loaded with serum samples prediluted in 1% BSA. After 3 h of incubation, the plates were washed three times with PBST buffer, and the bound antibody was detected by with biotinylated goat anti–mouse antibody and streptavidin-HRP using TMB as substrate.
Histology and GC analysis.
Organs were removed from sacrificed mice, fixed in 10% neutral buffered formalin, embedded in paraffin, and sectioned for hematoxylin-eosin staining. For GC formation analysis, SRBC-immunized mice were sacrificed after 10 d of immunization. Frozen spleen sections were fixed in methanol/acetone (2:1) for 10 min, followed by blocking for 30 min in a biotin- and serum-free SuperBlock buffer (Thermo Fisher Scientific). The GCs were detected using biotinylated peanut agglutinin (Vector Laboratories) followed by Alexa Fluor 594–conjugated streptavidin (Molecular Probes). The sections were mounted using an antiquenching agent (Vectashield; Vector Laboratories) and analyzed under a fluorescent microscope (DP70; Olympus). Panoramic pictures were taken and the GCs counted. The area and perimeter of each GC from each mouse (n = 3) were obtained using ImageJ software (National Institutes of Health). The area and perimeter are expressed in micrometers. GC B cells were analyzed by flow cytometry after staining with FITC-conjugated anti-CD95, PE-conjugated anti-B220, and APC-conjugated anti-GL7, and plasma B cells were analyzed similarly by staining with FITC-conjugated anti-B220 and PE-conjugated anti-CD138. For detecting TFH cells, the cells were stained with FITC-conjugated anti-CD4, PE-conjugated PD-1, and APC-conjugated CXCR5, followed by permeabilization with a Foxp3 staining kit (eBioscience) and intracellular staining with PE-conjugated anti–Bcl-6. TFH cells were detected similarly except the inclusion of intracellular staining with FITC-conjugated anti-Foxp3 or the GFP marker.
ELISA.
For SRBC or NP-specific antibody detection, Nunc Immuno Plate MaxiSorp plates (Thermo Fisher Scientific) were coated with SRBC lysate, NP9-BSA, or NP26-BSA and incubated overnight at 4°C. After blocking with 1% BSA in PBS, the plates were incubated with serially diluted standard or samples and then with HRP-conjugated detection antibodies. After colorimetric reaction (tetramethylbenzidine; Moss), the absorbance at 450 nm was measured using an ELISA plate reader. For IL-10 detection, Nunc plates were coated with 1 µg/ml anti–IL-10 capture antibody in 50 mM sodium bicarbonate and incubated overnight at 4°C. The coated plates were incubated with supernatant of the Treg cell culture and subjected to colorimetric detection as described above.
Immunoblot and real-time quantitative RT-PCR.
Purified Treg and CD4+ T cells were lysed in RIPA buffer supplemented with inhibitors of phosphatases and the proteases. For analyzing ERK phosphorylation, the cells were stimulated with agonistic anti-CD3 and anti-CD28 antibodies using a cross-linking method (Reiley et al., 2007) before lysis. The cell lysates were fractionated by SDS-PAGE and subjected to immunoblot assays with the indicated antibodies. For analyzing RNA expression, total cellular RNA was isolated and subjected to real-time quantitative RT-PCR assays as previously described (Chang et al., 2011). The gene-specific primer sets are listed in Table S1.
Electrophoretic mobility shift assay (EMSA).
Nuclear extract preparation and EMSA were performed as described previously (Ganchi et al., 1992) using 32P-radiolabeled oligonucleotide probes. The probes used were mouse ICOS AP1, 5′-TTCATCCATCTAGTCATTCATTTACGCATC-3′; and NF-Y, 5′-AAGAGATTAACCAATCACGTACGGTCT-3′.
In vitro and in vivo Treg cell suppression assays.
The in vitro Treg cell suppression assay was performed as previously described (Chang et al., 2012). In vivo Treg cell assays were performed essentially as described previously (Chang et al., 2012). For examining the in vivo roles of Treg cells in the regulation of GC reactions, sorted CD4+CD62LhiCD44loCD25− naive T cells from B6.SJL mice (5–6 wk old) and sorted CD4+GFP+CD25+ Treg cells from WT, Traf3Treg-KO, and Icos-KO mice (5–6 wk old) were intravenously transferred into Tcrb/Tcrd-dKO mice. Recipient mice were immunized with SRBC 2 d after adoptive transfer and sacrificed 14 d later for analyzing serum antibodies and lymphocyte populations.
Antibody somatic hypermutation analyses.
WT and Traf3Treg-KO mice were immunized with SRBCs and sacrificed after 10 d for isolating GC B cells by flow cytometric cell sorting based on the B220+CD95+GL7+ surface markers. Somatic hypermutation was analyzed based on the W33 to L hotspot mutation, essentially as previously described (Muramatsu et al., 2000). In brief, VH186.2 transcripts were amplified by PCR using the VH186.2 (5′-GCTGTATCATGCTCTCTTG-3′) and CHγ-1 (5′-GGTGCTATCCGGTCCCTGAGT-3′) primer pairs, and the PCR products were inserted into the pGEM-T vector by TA cloning. Randomly picked cDNA clones were sequenced for identification of the W33 to L mutations.
Statistical analysis.
Prism software (GraphPad Software) was used for two-tailed unpaired Student’s t tests. P-values of <0.05 or <0.01 were considered significant and very significant, respectively.
Online supplemental material.
Table S1 lists the gene-specific primers used for real-time RT-PCR analyses. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20131019/DC1.
Supplementary Material
Acknowledgments
We thank the Centenary Institute of Cancer Medicine and Cell Biology for TRAF3-floxed mice. We also thank the personnel from the Flow Cytometry, DNA Analysis, Histology, and Genetically Engineered Mouse core facilities at the University of Texas MD Anderson Cancer Center for their technical assistance.
This study was supported by grants from National Institutes of Health (AI057555, AI064639, GM84459, and AI104519 to S.-C. Sun and CA131207 to S.E. Ullrich) and partially supported by a Sister Institution Network Fund and a seed fund from the Center for Inflammation and Cancer at the University of Texas MD Anderson Cancer Center.
The authors have no conflicting financial interests.
Author contributions: J.-H. Chang and H. Hu designed and performed most of the experiments, prepared the figures, and wrote part of the manuscript; J. Jin performed the histology experiment; N. Puebla-Osorio performed the GC immunofluorescence staining experiment; Y. Xiao provided technical help; R. Brink contributed the Traf3-floxed mice; B.E. Gilbert contributed the influenza virus; S.E. Ullrich was involved in supervision of N. Puebla-Osorio; and S.-C. Sun supervised the work and wrote the manuscript.
Footnotes
Abbreviations used:
- APC
- allophycocyanin
- EMSA
- electrophoretic mobility shift assay
- GC
- germinal center
- ICOS
- inducible co-stimulator
- ICS
- intracellular cytokine staining
- NIK
- NF-κB–inducing kinase
- NP
- 4-hydroxy-3-nitrophenylacetyl
- SRBC
- sheep RBC
- TFH cell
- follicular T helper cell
- TFR cell
- follicular Treg cell
- TRAF
- TNF receptor–associated factor
References
- Allen D., Cumano A., Dildrop R., Kocks C., Rajewsky K., Rajewsky N., Roes J., Sablitzky F., Siekevitz M. 1987. Timing, genetic requirements and functional consequences of somatic hypermutation during B-cell development. Immunol. Rev. 96:5–22 10.1111/j.1600-065X.1987.tb00506.x [DOI] [PubMed] [Google Scholar]
- Allen D., Cumano A., Simon T., Sablitzky F., Rajewsky K. 1988. Modulation of antibody binding affinity by somatic mutation. Int. J. Cancer Suppl. 41:1–8 10.1002/ijc.2910410802 [DOI] [PubMed] [Google Scholar]
- Bauquet A.T., Jin H., Paterson A.M., Mitsdoerffer M., Ho I.C., Sharpe A.H., Kuchroo V.K. 2009. The costimulatory molecule ICOS regulates the expression of c-Maf and IL-21 in the development of follicular T helper cells and TH-17 cells. Nat. Immunol. 10:167–175 10.1038/ni.1690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busse M., Krech M., Meyer-Bahlburg A., Hennig C., Hansen G. 2012. ICOS mediates the generation and function of CD4+CD25+Foxp3+ regulatory T cells conveying respiratory tolerance. J. Immunol. 189:1975–1982 10.4049/jimmunol.1103581 [DOI] [PubMed] [Google Scholar]
- Campbell D.J., Koch M.A. 2011. Phenotypical and functional specialization of FOXP3+ regulatory T cells. Nat. Rev. Immunol. 11:119–130 10.1038/nri2916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J.H., Xiao Y., Hu H., Jin J., Yu J., Zhou X., Wu X., Johnson H.M., Akira S., Pasparakis M., et al. 2012. Ubc13 maintains the suppressive function of regulatory T cells and prevents their conversion into effector-like T cells. Nat. Immunol. 13:481–490 10.1038/ni.2267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang M., Jin W., Chang J.H., Xiao Y., Brittain G.C., Yu J., Zhou X., Wang Y.H., Cheng X., Li P., et al. 2011. The ubiquitin ligase Peli1 negatively regulates T cell activation and prevents autoimmunity. Nat. Immunol. 12:1002–1009 10.1038/ni.2090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung Y., Tanaka S., Chu F., Nurieva R.I., Martinez G.J., Rawal S., Wang Y.H., Lim H., Reynolds J.M., Zhou X.H., et al. 2011. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nat. Med. 17:983–988 10.1038/nm.2426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsner R.A., Ernst D.N., Baumgarth N. 2012. Single and coexpression of CXCR4 and CXCR5 identifies CD4 T helper cells in distinct lymph node niches during influenza virus infection. J. Virol. 86:7146–7157 10.1128/JVI.06904-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganchi P.A., Sun S.-C., Greene W.C., Ballard D.W. 1992. IκB/MAD-3 masks the nuclear localization signal of NF-κB p65 and requires the transactivation domain to inhibit NF-κB p65 DNA binding. Mol. Biol. Cell. 3:1339–1352 10.1091/mbc.3.12.1339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardam S., Sierro F., Basten A., Mackay F., Brink R. 2008. TRAF2 and TRAF3 signal adapters act cooperatively to control the maturation and survival signals delivered to B cells by the BAFF receptor. Immunity. 28:391–401 10.1016/j.immuni.2008.01.009 [DOI] [PubMed] [Google Scholar]
- Ha H., Han D., Choi Y. 2009. TRAF-mediated TNFR-family signaling. Curr. Protoc. Immunol. Chapter 11:Unit 11.9D. [DOI] [PubMed] [Google Scholar]
- He J.Q., Zarnegar B., Oganesyan G., Saha S.K., Yamazaki S., Doyle S.E., Dempsey P.W., Cheng G. 2006. Rescue of TRAF3-null mice by p100 NF-κB deficiency. J. Exp. Med. 203:2413–2418 10.1084/jem.20061166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrand J.M., Yi Z., Buchta C.M., Poovassery J., Stunz L.L., Bishop G.A. 2011. Roles of tumor necrosis factor receptor associated factor 3 (TRAF3) and TRAF5 in immune cell functions. Immunol. Rev. 244:55–74 10.1111/j.1600-065X.2011.01055.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huehn J., Siegmund K., Lehmann J.C., Siewert C., Haubold U., Feuerer M., Debes G.F., Lauber J., Frey O., Przybylski G.K., et al. 2004. Developmental stage, phenotype, and migration distinguish naive- and effector/memory-like CD4+ regulatory T cells. J. Exp. Med. 199:303–313 10.1084/jem.20031562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito T., Hanabuchi S., Wang Y.H., Park W.R., Arima K., Bover L., Qin F.X., Gilliet M., Liu Y.J. 2008. Two functional subsets of FOXP3+ regulatory T cells in human thymus and periphery. Immunity. 28:870–880 10.1016/j.immuni.2008.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josefowicz S.Z., Lu L.F., Rudensky A.Y. 2012. Regulatory T cells: mechanisms of differentiation and function. Annu. Rev. Immunol. 30:531–564 10.1146/annurev.immunol.25.022106.141623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King C., Tangye S.G., Mackay C.R. 2008. T follicular helper (TFH) cells in normal and dysregulated immune responses. Annu. Rev. Immunol. 26:741–766 10.1146/annurev.immunol.26.021607.090344 [DOI] [PubMed] [Google Scholar]
- Liao G., Zhang M., Harhaj E.W., Sun S.C. 2004. Regulation of the NF-kappaB-inducing kinase by tumor necrosis factor receptor-associated factor 3-induced degradation. J. Biol. Chem. 279:26243–26250 10.1074/jbc.M403286200 [DOI] [PubMed] [Google Scholar]
- Linterman M.A., Pierson W., Lee S.K., Kallies A., Kawamoto S., Rayner T.F., Srivastava M., Divekar D.P., Beaton L., Hogan J.J., et al. 2011. Foxp3+ follicular regulatory T cells control the germinal center response. Nat. Med. 17:975–982 10.1038/nm.2425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linterman M.A., Liston A., Vinuesa C.G. 2012. T-follicular helper cell differentiation and the co-option of this pathway by non-helper cells. Immunol. Rev. 247:143–159 10.1111/j.1600-065X.2012.01121.x [DOI] [PubMed] [Google Scholar]
- MacDonald T.T., Monteleone I., Fantini M.C., Monteleone G. 2011. Regulation of homeostasis and inflammation in the intestine. Gastroenterology. 140:1768–1775 10.1053/j.gastro.2011.02.047 [DOI] [PubMed] [Google Scholar]
- Mitsdoerffer M., Lee Y., Jäger A., Kim H.J., Korn T., Kolls J.K., Cantor H., Bettelli E., Kuchroo V.K. 2010. Proinflammatory T helper type 17 cells are effective B-cell helpers. Proc. Natl. Acad. Sci. USA. 107:14292–14297 10.1073/pnas.1009234107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muramatsu M., Kinoshita K., Fagarasan S., Yamada S., Shinkai Y., Honjo T. 2000. Class switch recombination and hypermutation require activation-induced cytidine deaminase (AID), a potential RNA editing enzyme. Cell. 102:553–563 10.1016/S0092-8674(00)00078-7 [DOI] [PubMed] [Google Scholar]
- Ramiscal R.R., Vinuesa C.G. 2013. T-cell subsets in the germinal center. Immunol. Rev. 252:146–155 10.1111/imr.12031 [DOI] [PubMed] [Google Scholar]
- Redpath S.A., van der Werf N., Cervera A.M., MacDonald A.S., Gray D., Maizels R.M., Taylor M.D. 2013. ICOS controls Foxp3(+) regulatory T-cell expansion, maintenance and IL-10 production during helminth infection. Eur. J. Immunol. 43:705–715 10.1002/eji.201242794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiley W.W., Zhang M., Jin W., Losiewicz M., Donohue K.B., Norbury C.C., Sun S.C. 2006. Regulation of T cell development by the deubiquitinating enzyme CYLD. Nat. Immunol. 7:411–417 10.1038/ni1315 [DOI] [PubMed] [Google Scholar]
- Reiley W.W., Jin W., Lee A.J., Wright A., Wu X., Tewalt E.F., Leonard T.O., Norbury C.C., Fitzpatrick L., Zhang M., Sun S.C. 2007. Deubiquitinating enzyme CYLD negatively regulates the ubiquitin-dependent kinase Tak1 and prevents abnormal T cell responses. J. Exp. Med. 204:1475–1485 10.1084/jem.20062694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rousset F., Garcia E., Defrance T., Péronne C., Vezzio N., Hsu D.H., Kastelein R., Moore K.W., Banchereau J. 1992. Interleukin 10 is a potent growth and differentiation factor for activated human B lymphocytes. Proc. Natl. Acad. Sci. USA. 89:1890–1893 10.1073/pnas.89.5.1890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sage P.T., Francisco L.M., Carman C.V., Sharpe A.H. 2013. The receptor PD-1 controls follicular regulatory T cells in the lymph nodes and blood. Nat. Immunol. 14:152–161 10.1038/ni.2496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakaguchi S., Yamaguchi T., Nomura T., Ono M. 2008. Regulatory T cells and immune tolerance. Cell. 133:775–787 10.1016/j.cell.2008.05.009 [DOI] [PubMed] [Google Scholar]
- Sasaki Y., Calado D.P., Derudder E., Zhang B., Shimizu Y., Mackay F., Nishikawa S., Rajewsky K., Schmidt-Supprian M. 2008. NIK overexpression amplifies, whereas ablation of its TRAF3-binding domain replaces BAFF:BAFF-R-mediated survival signals in B cells. Proc. Natl. Acad. Sci. USA. 105:10883–10888 10.1073/pnas.0805186105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S.C. 2012. The noncanonical NF-κB pathway. Immunol. Rev. 246:125–140 10.1111/j.1600-065X.2011.01088.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe M., Nakajima S., Ohnuki K., Ogawa S., Yamashita M., Nakayama T., Murakami Y., Tanabe K., Abe R. 2012. AP-1 is involved in ICOS gene expression downstream of TCR/CD28 and cytokine receptor signaling. Eur. J. Immunol. 42:1850–1862 10.1002/eji.201141897 [DOI] [PubMed] [Google Scholar]
- Weiss U., Zoebelein R., Rajewsky K. 1992. Accumulation of somatic mutants in the B cell compartment after primary immunization with a T cell-dependent antigen. Eur. J. Immunol. 22:511–517 10.1002/eji.1830220233 [DOI] [PubMed] [Google Scholar]
- Wollenberg I., Agua-Doce A., Hernández A., Almeida C., Oliveira V.G., Faro J., Graca L. 2011. Regulation of the germinal center reaction by Foxp3+ follicular regulatory T cells. J. Immunol. 187:4553–4560 10.4049/jimmunol.1101328 [DOI] [PubMed] [Google Scholar]
- Xie P., Stunz L.L., Larison K.D., Yang B., Bishop G.A. 2007. Tumor necrosis factor receptor-associated factor 3 is a critical regulator of B cell homeostasis in secondary lymphoid organs. Immunity. 27:253–267 10.1016/j.immuni.2007.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie P., Kraus Z.J., Stunz L.L., Liu Y., Bishop G.A. 2011. TNF receptor-associated factor 3 is required for T cell-mediated immunity and TCR/CD28 signaling. J. Immunol. 186:143–155 10.4049/jimmunol.1000290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X., Jeker L.T., Fife B.T., Zhu S., Anderson M.S., McManus M.T., Bluestone J.A. 2008. Selective miRNA disruption in T reg cells leads to uncontrolled autoimmunity. J. Exp. Med. 205:1983–1991 10.1084/jem.20080707 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.