Abstract
Background
The purpose of this study is to evaluate the effects of docosahexaenoic acid (DHA), a major omega-3-polyunsaturated fatty acid (ω-3-PUFAs), in the development of experimental choroidal neovascularization (CNV) in rodents.
Methods
Experimental second generation Long Evans rats fed with diets of varying ω-3-PUFA content designed to produce significantly different retinal DHA levels were used in our studies. A transgenic mouse model (fat-1) engineered to over-produce DHA was also studied. CNV was induced by rupture of Bruch's membrane using laser photocoagulation. At 7 days after induction, animals were euthanatized, and eyes were collected. RPE/choroid flatmounts were labeled with isolectin IB4 to determine CNV lesion volumes using confocal microscopy and high-performance 3D imaging software.
Results
The median of CNV complex volumes of animals with DHA-adequate diets was lower by 63% relative to that of animals with DHA-deficient diets. The median of CNV complex volumes in fat-1 transgenic mice was decreased by 59% relative to that of wild type controls.
Conclusions
Dietary intake or genetic manipulation to increase the sources of DHA significantly diminished the volume of induced CNV lesions in rodents. They suggest that consumption of ω-3-PUFAs may serve to prevent CNV.
Keywords: DHA, Omega-3 fatty acids, Choroidal neovascularization, Diet, Fat-1, Laser-induced CNV
Introduction
Neovascular Age-related Macular Degeneration (AMD) is a disease in which choroidal blood vessels grow pathologically to invade the retina through breaks in Bruch's membrane, thus causing irreparable blindness [1]. Laser rupture of Bruch's membrane offers a successful means of inducing choroidal neovascularization (CNV) in rodent models [2], and provides an excellent basis for evaluating factors that affect the induction and progression of CNV.
The role of lipids in angiogenesis is beginning to be defined. Omega-3-polyunsaturated fatty acids (ω-3-PUFAs) have the capacity to play roles in many processes of AMD, such as neovascularization, inflammation, and alterations in the capillary structure and integrity [3]. Docosahexaenoic acid (22:6n-3, DHA) is the major ω-3-PUFA of the retina, found primarily in neural and vascular cell membranes incorporated into phospholipids [4]. The outer retina has the highest DHA phospholipid concentrations per unit weight among tissues in our bodies and DHA is the major fatty acid of retinal photoreceptor outer segment membranes. Dietary intake of ω-3-PUFAs can significantly affect retinal levels of ω-3-PUFAs, and levels of retinal DHA increase in mice fed with diets enriched in ω-3-PUFAs [5]. Epidemiological studies have revealed an important inverse relationship between dietary intake of the ω-3-PUFA and risk of developing advanced AMD [6-10]. Several in vivo and in vitro studies have demonstrated the benefit of DHA for retinal function, photoreceptor survival and rhodopsin regeneration [11-13]. In contrast, tissue DHA insufficiency can negatively affect retinal signaling and is associated with alterations in retinal function [14]. In vivo studies point to the effects of ω-3-PUFAs on the vascular retina. Connor et al. [15] have demonstrated that ω-3-PUFAs, such as DHA and its precursors, eicosapentaenoic acid (20:5n-3, EPA) and α-linolenic acid (18:3n-3, LNA)), as well as bioactive ω-3-PUFA-derived mediators neuroprotectin D1, resolvin D1 and resolvin E1 can attenuate pathological retinal angiogenesis in experimental animal models. Koto et al. [16] have reported that an EPA-rich diet results in significant suppression of CNV and CNV-related inflammatory molecules in mice and in cultured macrophages and endothelial cells. More recently, Sheets et al. [17] demonstrated that i.p. injections of the downstream DHA-derived mediator neuroprotectin D1 can attenuate laser-induced CNV in mice. Although these conclusions imply the role of ω-3-PUFAs as inhibitors of angiogenesis and give them therapeutic potential as dietary protectors against angiogenic diseases such as AMD, the effects of DHA on CNV are as of yet unknown.
The purpose of this study is to evaluate the effect of DHA on choroidal neovessel volume using an experimental model for CNV and a quantification protocol developed in our laboratory [18]. We compared rats fed with a DHA-adequate diet to those with a DHA-deficient diet designed specifically to produce significant differences in retinal DHA levels. We also used transgenic mice engineered to carry a fat-1 gene from C. elegans, which results in a physiological overproduction of DHA [19]. We report evidence for attenuation of CNV by increasing DHA sources via dietary intake or genetic means.
Materials and Methods
Animals
Time pregnant, Long Evans rats were obtained commercially (Charles River, Portage, IL) at gestational day 3 and maintained at the NIAAA animal facility. They were divided into two dietary groups and fed either an ω-3 adequate or ω-3 deficient diet throughout pregnancy and lactation as previously described [20]. Pups were maintained on the same diets as their dams. Transgenic mice engineered to carry a fat-1 gene from C. elegans, which results in a physiological over-expression of long chain ω-3 PUFAs [19] and were housed and fed at the NEI animal facility. All animal procedures were approved by the NIAAA or NEI Animal Care and Use Committees.
Diets
Long Evans rats were subjected to very low levels of ω-3 fatty acids through two generations, and a separate group of animals was maintained on an ω-3 adequate diet of the same composition as described previously [5]. Rats were made ω-3 deficient using a safflower oilbased diet and their offspring (F2 generation) were weaned to the same diet at 3 weeks of age. To provide for the low ω-3 fatty acid content, the basal fat ingredients used for the ω-3 deficient diet were hydrogenated coconut and safflower oils (see Table 1 in [5]). In the ω-3 adequate diet, a small amount of flaxseed oil and DHASCO (42% ± 1% of fatty acids as DHA) (Martek Biosciences, Columbia, MD) were added to supply LNA and DHA, respectively. The content of the key fatty acid variables of the two diets, LNA and DHA, were 0.04% and non-detectable in the ω-3 deficient diet, but were 2.6% and 1.3% of total fatty acids, respectively, in the ω-3 adequate diet [5]. Diet and water were provided ad libitum.
Laser-induced CNV technique
Laser treatment was performed on each retina to induce CNV, as described before [18]. Control and experimental animals were anesthetized, and a 532-nm laser was used to rupture Bruch's membrane. Using a contact fundus laser lens, four laser spots of 50 μM in diameter were applied to each fundus surrounding the optic nerve with a ND: YAG 532 nm laser (Alcon, Fort Worth, TX). Laser exposure time was 0.1 seconds, with a power between 80 and 90mW. Bubble was used to confirm breakage of Bruch's membrane. Animals were maintained on the same diets as before laser treatment for 7 days after laser injury and then were euthanized and the eyes were removed and fixed. In rats, eyes were removed with the nictitans membrane attached for orientation. In mice, a corneal cut was made on the nasal side of the eye for the same purpose.
Choroidal-RPE flatmounts, grid-confocal microscopy, neovessel volume quantification
Specimens were flat mounted, imaged, and quantified using a method previously described [18]. Specific markers were used to stain the nuclei (DAPI), endothelial cells (Isolectin-IB4) and RPE cells actin cytoskeleton (Phalloidin). A grid-confocal (Improvision Inc.) mounted on an inverted microscope (Nikon TE2000-U) was used to collect z-series using a 40X oil-immersion objective. Images with bubble formation were collected sequentially for DAPI, Phalloidin, and Isolectin-IB4 Alexa Fluor conjugated fluorescent dyes. DAPI (blue signal) was detected at a 358-461 nm wavelength, Alexa Fluor 488 (500-550 nm) detected phalloidin in green, and the Alexa Fluor 568 (580-675 nm) signal for Isolectin-IB4 was detected in red. Multiplane Z-series images were collected with a confocal microscope and were exported to an image-analysis program (Volocity, Improvision, Perking Elmer). An image sequence was generated from the original Z-series and three-dimensional reconstructions of the lesions were generated. By turning off the channels representing nuclei and RPE cells, the red channel representing neovessels and microglia was isolated. Images were cropped to exclude microglia, and the volume of the blood vessels was quantified three times per laser spot and expressed in cubic microns.
For the comparison of the adequate and deficient DHA diets we used repeated measures linear regression. This takes into account the correlation among the repeated measures per mouse. The log of the volume was used to normalize the distribution of the volume. We used the MIXED procedure of the SAS Software, version 9.2 (SAS Institute Inc, Cary, NC). For the comparison of the wild type versus fat-1 mice the Wilcoxon rank-sum test was used in SAS.
Results
DHA-deficient diets and CNV
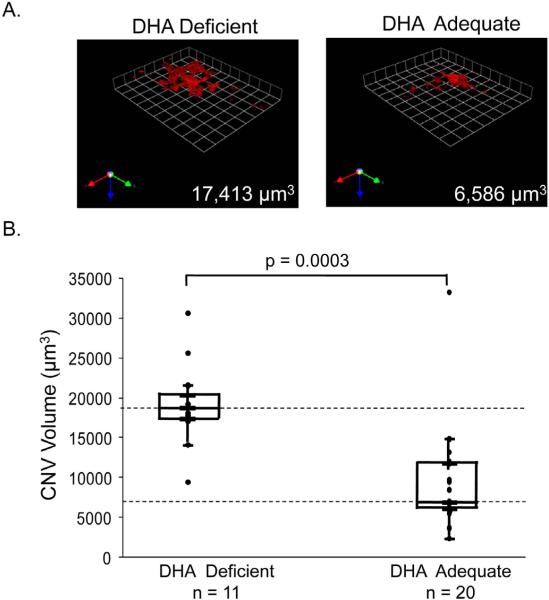
It has been previously shown that the retinal DHA level can be regulated by ω-3 fatty acid modulation of the diet [5] and that increasing the sources of dietary ω-3 fatty acids reduces experimental pathological retinal angiogenesis [15]. Thus, we undertook to further evaluate the effects of DHA in experimental choroidal angiogenesis in the second generation of rats fed with diets designed to yield significant differences in retinal DHA content [5]. Second generation rats were fed with ω-3 deficient and ω-3 adequate diets. Moriguchi et al. [5] have shown that while the mean body and brain weights of the animals raised on the two diets are not significantly different by 7 weeks of age, the ω-3 deficient diet is very effective in inducing ω-3 fatty acid deficiency in retina (retinal DHA level decreases from 32% of total fatty acids in the ω-3 adequate group to 5.4% in the ω-3-deficient group, i.e., an 83% decrease). Then CNV was induced by rupture of Bruch's membrane using laser photocoagulation in eyes of rats at 8 weeks of age for the two groups. At seven days after CNV induction, choroidal neo vessels were labeled and CNV complex volumes were quantified using a cellular imaging software from three dimensional reconstructed immune fluorescent images. The volume of CNV was measured to evaluate and compare the effects of dietary intake of ω-3 PUFA on the development of CNV. Figure 1A shows CNV complexes labeled with Alexa568-conjugated-isolectin IB4, which was used to label newly formed vessels (red). Quantification of CNV complexes from ω-3 deficient and ω-3 adequate rats is summarized in Figure 1B. ω-3 deficient fed rats had a median CNV complex volume of 18,399 μm3 (log(volume) = 9.8). The CNV complex volumes were significantly lower in ω-3-adequate fed rats with a median volume of 6761 μm3 (log (vol) = 8.8). The difference in log volumes indicates that the deficient diet resulted in a higher log (volume) of 0.86 over that of the adequate diet. The difference was statistically significant with a p=0.0003. A 95% confidence limit for the 0.86 estimate is (0.42, 1.30). This indicates that lesions in animals on ω–3 adequate diets were 63% smaller in median volume than those on ω–3 deficient diets. The results show that DHA deficient diets increased vulnerability to pathological choroidal angiogenesis in rats.
Figure 1.
Neovessel volumes from rats fed ω-3-PUFA deficient and adequate diets. (A) Representative red channel projections (neovessels) from animals with DHA deficient and DHA adequate diets. Bottom right depicts lesion volumes. (B) Box and whisker representation: Neovessel volumes from DHA-deficient and DHA-adequate diets; n = number of lesions; lesions came from 4 animals (deficient), and from 5 animals (adequate). Adequate diets yielded lesions with a median volume 63% smaller than those of deficient diets. Each point represents the mean value of a triplicate measurement. Dotted horizontal lines represent median values of neovessel volume for rats with DHA deficient and DHA adequate diets.
CNV in a genetic animal model that elevates DHA levels
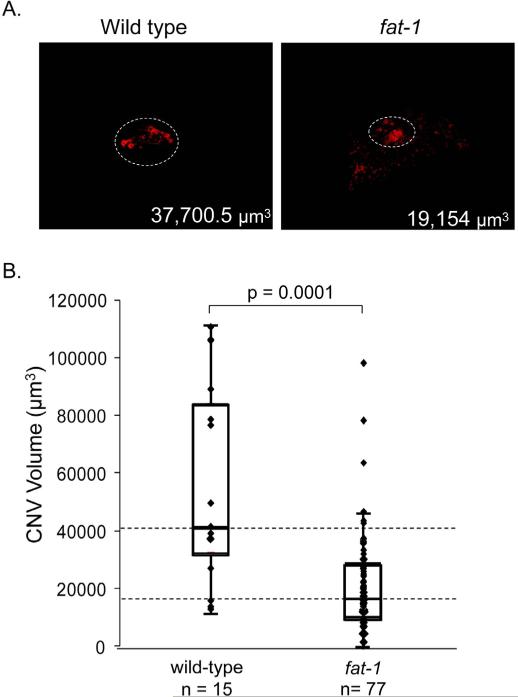
We further tested the effects of increasing the retinal DHA levels by genetic means on development of experimental CNV in mice. We used a genetic model in which overexpression of the C. elegans fat-1 gene in transgenic mice converts ω-6 PUFA to ω-3 PUFA, resulting in elevated tissue levels of ω-3 PUFA [19] and, in particular, it was reported that retina DHA content was 28% in fat-1 mice and 18% in wild type mice [15]. Figure 2A shows CNV complexes labeled with Alexa568-conjugated-isolectin IB4 of wild type and fat-1 mice. Quantification of CNV complexes from wild type and fat-1 mice in Figure 2B revealed that wild type mice had a median CNV complex volume of 41,560 μm3 and fat-1 mice decreased significantly with a median volume of 17,098 μm3 (P < 0.0001). This indicates that an increase of DHA in the retina by genetic means yielded lesions of median volume values 59% smaller in volume than those of control (wild type). The results demonstrate that elevating the DHA levels in mice can increase protection to pathological choroidal angiogenesis.
Figure 2.
Neovessel volumes from transgenic (fat-1) mice (A) Representative red channel projections (neovessels) from wild-type and fat-1 transgenics. Bottom right depicts lesion volumes. (B) Box and whisker representation: Neovessel volumes from transgenic mice that overproduce DHA (fat-1 mice), and wild type controls; n = number of lesions (17 animals for fat-1 mice and 4 animals for wild type mice). Fat-1 lesions were 59% smaller in volume than control lesions. All samples were quantified in μm3 using an image analysis module. Each point represents the mean value of a triplicate measurement. Dotted horizontal lines represent median values of neovessel volume for both conditions.
Discussion
Previous epidemiological studies have shown inverse relations between ω-3 PUFAs intake and incidence in developing neovascular AMD [6]. The present study shows the association between the vascular area of the choroid induced by rupturing the Bruch's membrane with laser energy in rats or mice and DHA levels modulated by dietary or genetic means, respectively. Both sets of experiments, i.e., using DHA adequate/DHA deficient diets and fat-1 transgenic/wild type mice, were designed to produce animals that differ significantly in their retinal levels of DHA relative to their controls as described before [5,15,19]. A clear relation between attenuation of CNV and DHA levels was observed. The conclusions indicate that while a decrease in rat retinal DHA levels is permissive to pathological choroidal angiogenesis, elevating the DHA levels in mice increases protection to pathological CNV. In addition, they support the idea that DHA may play an important role in modulating processes implicated in protecting against CNV development and in turn, the pathogenesis of AMD, and that while deficiency of DHA intake is detrimental, supplementing DHA intake may be of benefit in preventing AMD.
The few outlying points in Figure 1 and Figure 2 raise some concerns about variables that would compromise the ability of elevated DHA from preventing experimental CNV in a small number of cases, even though the entire sample size shows a significant reduction in CNV with elevated DHA. It is clear that variability occurs among experimental CNV lesion volumes [15,36,37]. In a previous article, we described variability in the extent of the neovascular response to laser treatments among lesions in the same animal and among animals [15], and noted that similar variability has been reported in patients with CNV [38]. It has been suggested that the differences in background fluorescence present in lesions may affect the measurement, and that significant variability among CNV lesion size may also be explained by diversity in sensitivity to laser energy, differences in the focus of the laser spot, differences in the quality of the laser beam [36]. Interestingly, Hörster et al. [37] induced CNV in mice with laser energy and found spontaneous regression of CNV activity within 14 days after induction. Although, the individual variability among points is a fact, the statistical analyses show that the groups with higher DHA have lower CNV lesion volumes than their counterparts with lower DHA.
Although we did not perform retinal fatty acid analyses, the dietary model has been extensively characterized in this regard in past studies [5,15,39]. A developmental study of retinal DHA loss [39] showed that there was a reduction in DHA of 88% (at birth), 87% (day 5), 86% (day 10), 84% (day20) and 83% (day 50) in n-3 deficient animals relative to those with adequate diets. However, at adulthood, at 91 days of age, the retinal DHA loss had fallen to only 75% in the n-3 deficient group. Thus there was a very constant and significant percentage loss of DHA over the time course of the experiment in Figure 1, and this indicates that it is likely that the level of DHA loss in the current experiment is somewhat more than that observed in related experiments using a similarly deficient diet and where the measurement has been performed at adulthood. Similarly, the reported retinal DHA increases in the genetic model fat-1 are significantly higher than those in wild type animals [15,40].
Comparisons between the present study and previous studies on the effects of DHA precursors and down-stream metabolites on CNV development were performed. Koto et al. [16] reported the evaluation of laser-induced CNV in mice fed with a diet supplemented with 5% EPA relative to control mice fed with a diet in which linoleic acid (18:2n-6, LA), an arachidonic acid precursor, replaced EPA. The EPA rich diet results in suppression of CNV volume (33% decrease at 7 days post-laser) with parallel increases in the serum and RPE-choroid EPA levels in EPA fed mice compared to their LA-fed counterparts [16]. Since there is little or no EPA in the retina, it is likely that the EPA effect was due either to conversion to DHA or perhaps to one of the resolvins. In another report, Sheets et al. [17] compared laser-induced CNV in mice receiving i.p. injections of 114 μg/kg of neuroprotectin D1 and those with sham injections every two days after laser photocoagulation. Neuroprotectin D1 significantly attenuated CNV volume (46% and 68% decrease at 7 and 14 days post-laser, respectively) relative to sham injected controls. Similarly, our results with increasing DHA sources by dietary intake or genetic means show significant CNV suppression (63% and 59% decrease in CNV volume by 7 days post-laser relative to controls, respectively). In summary, these studies indicate that long chain ω-3 fatty acids or their bioactive metabolites may potentially modulate processes impacting CNV.
DHA release from phospholipids and production of its downstream metabolites can be upregulated by several neurotrophins and growth factors, such as pigment epithelium-derived factor (PEDF), a very efficient modulator [21]. PEDF is a natural protein of the retina with antiangiogenic, anti-inflamatory and neurotrophic properties. Its levels decrease in eyes of patients with neovascular AMD and in the retina of animals immediately after breakage of Bruch's membrane with laser exposure [22-26]. Its molecular mechanism of action involves fatty acid metabolism since PEDF binds to and stimulates PEDFR, a phospholipase that liberates fatty acids from phospholipids [27,28]. While in the healthy retina, the abundant DHA phospholipids are available substrates for the PEDFR phospholipase activity, in a DHA deficient retina there is a depletion of these substrates. Upon PEDF upregulation, the PEDFR activity can be stimulated to produce the necessary DHA-derived metabolites for anti-angiogenesis. In this way, the levels of retinal PEDF and DHA can determine sensitivity to angiogenesis inhibition and increase protection to the retina.
Several studies point to mechanisms of action of DHA as an anti-CNV mediator (reviewed by San Giovanni et al. [29]). Some have lead to proposals of DHA having anti-inflammatory properties, in part based on its ability to downregulate key cytokines involved in systemic inflammation, e.g. tumor necrosis factor-α. [15]. Studies in vivo and in live cells have described that ω-3 PUFAs suppress retinal neovascularization via a peroxisome proliferator-activated receptor gamma-dependent reduction of inflammatory activity and endothelial cell activation [30]. More recently, it has been proposed that the high affinity binding of DHA to fatty acid binding protein 7 (FABP7/BLBP) [31] results in translocation of the protein from the cytoplasm to the nucleus where DHA is transferred to peroxisome proliferator-activated receptor gamma and leads to downregulation of migratory genes and cell migration [32]. Experiments with live cells have also shown that incorporation of DHA into membrane phospholipids can directly affect the fluidity of plasma membranes to deplete and displace the key signaling molecules embedded in the endothelial cell surfaces, thus changing the responses of growth factors and cytokines needed for angiogenesis [33-35]. Taken together, these mechanisms of action of DHA would result in protection against choroidal neovascularization.
Given that Western diets are often low in ω-3 PUFAs, and an increase in DHA levels is found associated with reduced risk of CNV [6,7], the present results indicate that supplementing DHA intake may be of benefit in preventing CNV. A recent nutritional AMD treatment phase I study reported significant blood enrichment in EPA and DHA in a AMD population after six months of oral supplementation with fish oil and no adverse effects were observed [41]. This study supports the feasibility of a long-term double-masked prospective case-control study in an AMD population in order to evaluate a potential benefit from oral supplementation with DHA.
Acknowledgements
The work was supported by the intramural research program of the US National Institutes of Health (NIH) with Project number 1ZIA-EY000306 to S.P.B. We thank Dr. John Paul San Giovanni for interesting discussions, carefully proofreading of the manuscript and providing the fat-1 mice (a generous gift of Dr. Jing Ka).
Footnotes
Publisher's Disclaimer: This article was originally published in a journal by OMICS Publishing Group, and the attached copy is provided by OMICS Publishing Group for the author's benefit and for the benefit of the author's institution, for commercial/research/educational use including without limitation use in instruction at your institution, sending it to specific colleagues that you know, and providing a copy to your institution's administrator. All other uses, reproduction and distribution, including without limitation commercial reprints, selling or licensing copies or access, or posting on open internet sites, your personal or institution's website or repository, are requested to cite properly.
Citation: Taaheri SM, Agarwal M, Amaral J, Fedorova I, Agrón E, et al. (2011) Effects of Docosahexaenoic Acid in Preventing Experimental Choroidal Neovascularization in Rodents. J Clinic Experiment Ophthalmol 2:187. doi:10.4172/2155-9570.1000187
Refernces
- 1.Hyman L, Neborsky R. Risk factors for age-related macular degeneration: an update. Curr Opin Ophthalmol. 2002;13:171–175. doi: 10.1097/00055735-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Dobi ET, Puliafito CA, Destro M. A new model of experimental choroidal neovascularization in the rat. Arch Ophthalmol. 1989;107:264–269. doi: 10.1001/archopht.1989.01070010270035. [DOI] [PubMed] [Google Scholar]
- 3.SanGiovanni JP, Chew EY. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog Retin Eye Res. 2005;24:87–138. doi: 10.1016/j.preteyeres.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Fliesler SJ, Anderson RE. Chemistry and metabolism of lipids in the vertebrate retina. Prog Lipid Res. 1983;22:79–131. doi: 10.1016/0163-7827(83)90004-8. [DOI] [PubMed] [Google Scholar]
- 5.Moriguchi T, Loewke J, Garrison M, Catalan JN, Salem N., Jr Reversal of docosahexaenoic acid deficiency in the rat brain, retina, liver, and serum. J Lipid Res. 2001;42:419–427. [PubMed] [Google Scholar]
- 6.SanGiovanni JP, Agron E, Clemons TE, Chew EY. Omega-3 long-chain polyunsaturated fatty acid intake inversely associated with 12-year progression to advanced age-related macular degeneration. Arch Ophthalmol. 2009;127:110–112. doi: 10.1001/archophthalmol.2008.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sangiovanni JP, Agron E, Meleth AD, Reed GF, Sperduto RD, et al. {omega}-3 Long-chain polyunsaturated fatty acid intake and 12-y incidence of neovascular age-related macular degeneration and central geographic atrophy: AREDS report 30, a prospective cohort study from the Age-Related Eye Disease Study. Am J Clin Nutr. 2009;90:1601–1607. doi: 10.3945/ajcn.2009.27594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seddon JM, Cote J, Rosner B. Progression of age-related macular degeneration: association with dietary fat, transunsaturated fat, nuts, and fish intake. Arch Ophthalmol. 2003;121:1728–1737. doi: 10.1001/archopht.121.12.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.SanGiovanni JP, Chew EY, Agron E, Clemons TE, Ferris FL, 3rd, et al. The relationship of dietary omega-3 long-chain polyunsaturated fatty acid intake with incident age-related macular degeneration: AREDS report no. 23. Arch Ophthalmol. 2008;126:1274–1279. doi: 10.1001/archopht.126.9.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chong EW, Robman LD, Simpson JA, Hodge AM, Aung KZ, et al. Fat consumption and its association with age-related macular degeneration. Arch Ophthalmol. 2009;127:674–680. doi: 10.1001/archophthalmol.2009.60. [DOI] [PubMed] [Google Scholar]
- 11.Bazan NG. Cell survival matters: docosahexaenoic acid signaling, neuroprotection and photoreceptors. Trends Neurosci. 2006;29:263–271. doi: 10.1016/j.tins.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 12.German OL, Insua MF, Gentili C, Rotstein NP, Politi LE. Docosahexaenoic acid prevents apoptosis of retina photoreceptors by activating the ERK/MAPK pathway. J Neurochem. 2006;98:1507–1520. doi: 10.1111/j.1471-4159.2006.04061.x. [DOI] [PubMed] [Google Scholar]
- 13.Rotstein NP, Politi LE, German OL, Girotti R. Protective effect of docosahexaenoic acid on oxidative stress-induced apoptosis of retina photoreceptors. Invest Ophthalmol Vis Sci. 2003;44:2252–2259. doi: 10.1167/iovs.02-0901. [DOI] [PubMed] [Google Scholar]
- 14.Niu SL, Mitchell DC, Lim SY, Wen ZM, Kim HY, et al. Reduced G protein-coupled signaling efficiency in retinal rod outer segments in response to n-3 fatty acid deficiency. J Biol Chem. 2004;279:31098–31104. doi: 10.1074/jbc.M404376200. [DOI] [PubMed] [Google Scholar]
- 15.Connor KM, SanGiovanni JP, Lofqvist C, Aderman CM, Chen J, et al. Increased dietary intake of omega-3-polyunsaturated fatty acids reduces pathological retinal angiogenesis. Nat Med. 2007;13:868–873. doi: 10.1038/nm1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koto T, Nagai N, Mochimaru H, Kurihara T, Izumi-Nagai K, et al. Eicosapentaenoic acid is anti-inflammatory in preventing choroidal neovascularization in mice. Invest Ophthalmol Vis Sci. 2007;48:4328–4334. doi: 10.1167/iovs.06-1148. [DOI] [PubMed] [Google Scholar]
- 17.Sheets KG, Zhou Y, Ertel MK, Knott EJ, Regan CE, Jr, et al. Neuroprotectin D1 attenuates laser-induced choroidal neovascularization in mouse. Mol Vis. 2010;16:320–329. [PMC free article] [PubMed] [Google Scholar]
- 18.Campos M, Amaral J, Becerra SP, Fariss RN. A novel imaging technique for experimental choroidal neovascularization. Invest Ophthalmol Vis Sci. 2006;47:5163–5170. doi: 10.1167/iovs.06-0156. [DOI] [PubMed] [Google Scholar]
- 19.Kang JX, Wang J, Wu L, Kang ZB. Transgenic mice: fat-1 mice convert n-6 to n-3 fatty acids. Nature. 2004;427:504. doi: 10.1038/427504a. [DOI] [PubMed] [Google Scholar]
- 20.Fedorova I, Hussein N, Baumann MH, Di Martino C, Salem N., Jr An n-3 fatty acid deficiency impairs rat spatial learning in the Barnes maze. Behav Neurosci. 2009;123:196–205. doi: 10.1037/a0013801. [DOI] [PubMed] [Google Scholar]
- 21.Mukherjee PK, Marcheselli VL, Barreiro S, Hu J, Bok D, et al. Neurotrophins enhance retinal pigment epithelial cell survival through neuroprotectin D1 signaling. Proc Natl Acad Sci U S A. 2007;104:13152–13157. doi: 10.1073/pnas.0705949104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amaral J, Becerra SP. Effects of human recombinant PEDF protein and PEDF-derived peptide 34-mer on choroidal neovascularization. Invest Ophthalmol Vis Sci. 2010;51:1318–1326. doi: 10.1167/iovs.09-4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhutto IA, McLeod DS, Hasegawa T, Kim SY, Merges C, et al. Pigment epithelium-derived factor (PEDF) and vascular endothelial growth factor (VEGF) in aged human choroid and eyes with age-related macular degeneration. Exp Eye Res. 2006;82:99–110. doi: 10.1016/j.exer.2005.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holekamp NM, Bouck N, Volpert O. Pigment epithelium-derived factor is deficient in the vitreous of patients with choroidal neovascularization due to age-related macular degeneration. Am J Ophthalmol. 2002;134:220–227. doi: 10.1016/s0002-9394(02)01549-0. [DOI] [PubMed] [Google Scholar]
- 25.Ogata N, Wada M, Otsuji T, Jo N, Tombran-Tink J, et al. Expression of pigment epithelium-derived factor in normal adult rat eye and experimental choroidal neovascularization. Invest Ophthalmol Vis Sci. 2002;43:1168–1175. [PubMed] [Google Scholar]
- 26.Renno RZ, Youssri AI, Michaud N, Gragoudas ES, Miller JW. Expression of pigment epithelium-derived factor in experimental choroidal neovascularization. Invest Ophthalmol Vis Sci. 2002;43:1574–1580. [PubMed] [Google Scholar]
- 27.Notari L, Baladron V, Aroca-Aguilar JD, Balko N, Heredia R, et al. Identification of a lipase-linked cell membrane receptor for pigment epithelium-derived factor. J Biol Chem. 2006;281:38022–38037. doi: 10.1074/jbc.M600353200. [DOI] [PubMed] [Google Scholar]
- 28.Subramanian P, Notario PM, Becerra SP. Pigment epithelium-derived factor receptor (PEDF-R): a plasma membrane-linked phospholipase with PEDF binding affinity. Adv Exp Med Biol. 2010;664:29–37. doi: 10.1007/978-1-4419-1399-9_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.SanGiovanni JP, Mehta S, Mehta S. Variation in lipid-associated genes as they relate to risk of advanced age-related macular degeneration. World Rev Nutr Diet. 2009;99:105–158. doi: 10.1159/000193002. [DOI] [PubMed] [Google Scholar]
- 30.Stahl A, Sapieha P, Connor KM, Sangiovanni JP, Chen J, et al. Short communication: PPAR gamma mediates a direct antiangiogenic effect of omega 3-PUFAs in proliferative retinopathy. Circ Res. 2010;107:495–500. doi: 10.1161/CIRCRESAHA.110.221317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu LZ, Sanchez R, Sali A, Heintz N. Ligand specificity of brain lipid-binding protein. J Biol Chem. 1996;271:24711–24719. doi: 10.1074/jbc.271.40.24711. [DOI] [PubMed] [Google Scholar]
- 32.Mita R, Beaulieu MJ, Field C, Godbout R. Brain fatty acid-binding protein and omega-3/omega-6 fatty acids: mechanistic insight into malignant glioma cell migration. J Biol Chem. 2010;285:37005–37015. doi: 10.1074/jbc.M110.170076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen W, Esselman WJ, Jump DB, Busik JV. Anti-inflammatory effect of docosahexaenoic acid on cytokine-induced adhesion molecule expression in human retinal vascular endothelial cells. Invest Ophthalmol Vis Sci. 2005;46:4342–4347. doi: 10.1167/iovs.05-0601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen W, Jump DB, Esselman WJ, Busik JV. Inhibition of cytokine signaling in human retinal endothelial cells through modification of caveolae/lipid rafts by docosahexaenoic acid. Invest Ophthalmol Vis Sci. 2007;48:18–26. doi: 10.1167/iovs.06-0619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Opreanu M, Lydic TA, Reid GE, McSorley KM, Esselman WJ, et al. Inhibition of cytokine signaling in human retinal endothelial cells through downregulation of sphingomyelinases by docosahexaenoic acid. Invest Ophthalmol Vis Sci. 2010;51:3253–3263. doi: 10.1167/iovs.09-4731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Campa C, Kasman I, Ye W, Lee WP, Fuh G, et al. Effects of an anti–VEGF-A monoclonal antibody on laser-induced choroidal neovascularization in mice: optimizing methods to quantify vascular changes. Invest Ophthalmol Vis Sci. 2008;49:1178–1183. doi: 10.1167/iovs.07-1194. [DOI] [PubMed] [Google Scholar]
- 37.Ryan SJ. Subretinal neovascularization: Natural history of an experimental model. Arch Ophthalmol. 1982;100:1804–1809. doi: 10.1001/archopht.1982.01030040784015. [DOI] [PubMed] [Google Scholar]
- 38.Hörster R, Müther PS, Vierkotten S, Schröder S, Kirchhof B, et al. 24th Annual Conference of the German Retina Society. Aachen, 17.-18.06.2011. German Medical Science GMS Publishing House; Düsseldorf: 2011. In-vivo and ex-vivo characterization of laser-induced choroidal neovascularization variability in mice. German Retina Society. [Google Scholar]
- 39.Salem N, Jr, Loewke J, Catalan JN, Majchrzak S, Moriguchi T. Incomplete replacement of docosahexaenoic acid by n-6 docosapentaenoic acid in the rat retina after an n-3 fatty deficient diet. Exp Eye Res. 2005;81:655–663. doi: 10.1016/j.exer.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 40.Suh M, Sauvé Y, Merrells KJ, Kang JX, Ma DW. Supranormal electroretinogram in fat-1 mice with retinas enriched in docosahexaenoic acid and n-3 very long chain fatty acids (C24-C36). Invest Ophthalmol Vis Sci. 2009;50:4394–4401. doi: 10.1167/iovs.08-2565. [DOI] [PubMed] [Google Scholar]
- 41.Querques G, Benlian P, Chanu B, Portal C, Coscas G, et al. Nutritional AMD treatment phase I (NAT-1): feasibility of oral DHA supplementation in agerelated macular degeneration. Eur J Ophthalmol. 2009;19:100–106. doi: 10.1177/112067210901900115. [DOI] [PubMed] [Google Scholar]