Abstract
Introduction
There has been an increasing interest in studying the stigma of alcohol use disorders (AUDs) yet scant research has evaluated the conceptualization and measurement of alcohol stigma. This study examined the measurement properties (i.e. factor structure) and validity of the alcohol-adapted Perceived Devaluation-Discrimination scale (PDD), which assesses the construct of perceived alcohol stigma (PAS).
Materials and Methods
Our sample included 34,386 respondents from the Wave 2 assessment in the National Epidemiologic Survey on Alcohol and Related Conditions, a population-representative survey of noninstitutionalized United States adults. Analytic procedures included confirmatory factor analysis and structural equation modeling.
Results
One factor (perceived devaluation-discrimination) and two factor (perceived devaluation, perceived discrimination) confirmatory factor analytic models fit the data well (CFI=0.958, TLI=0.942, RMSEA=0.056; CFI=0.962, TLI=0.946, RMSEA=0.054; respectively) when adjusting for item wording effects with a latent method factor. Despite having a better fit to the data (χ2(1) = 542, p < 0.0001), the two factors were highly correlated (r=0.90), which led us to favor a one-factor model. Structural equation models found that the inverse relationship between PAS and perceived interpersonal social support was strongest for persons with a stigmatized-labeling status. The same was not true in analyses predicting social network involvement.
Conclusions
A one-factor solution of perceived alcohol stigma had superior parsimony. The alcohol-adapted PDD appears to be a psychometrically sound measure and exhibits relationships that are consistent with modified labeling theory.
Keywords: Perceived stigma, alcohol use disorders, social consequences, confirmatory factor analysis, structural equation modeling
INTRODUCTION
As stigma pertains to alcohol use disorders (AUDs) and more broadly to substance use disorders (SUDs), socially constructed labels such as alcoholic or addict evoke stereotypes of being unpredictable, dangerous, irresponsible, of bad character, and at fault for one’s illness (Crisp et al. 2000). Public stigma, defined as the general public’s evaluations and reactions towards persons with stigmatized conditions (Corrigan and Watson 2002), is particularly negative for AUDs. In fact, attitudes towards persons with AUDs appear to be worse than the attitudes towards depression or schizophrenia (Schomerus et al. 2010). Increasing attention has been given to the consequences of stigma for persons with AUDs, including the development of standardized measures to assess the degree to which affected persons suffer from stigma (Fortney et al. 2004; Keyes et al. 2010; Luoma et al. 2010; Schomerus et al. 2011; Smith et al. 2010).
The categories of perceived stigma, experienced stigma, and self-stigma have been used to group stigma measures pertinent to the perspective of stigmatized persons (Brohan et al. 2010). Briefly, perceived stigma is the awareness of public stigma. Experienced stigma involves actual occurrences of discrimination attributed to a stigmatized condition. Self-stigma is a process where the negative evaluations associated with public stigma are incorporated into one’s sense of self. Instruments are also available that measure stigma from the perspective of the general public (e.g. attribution and social distance scales; see Link et al. 2004; Brown 2011). Measures of structural (contextual) stigma often utilize policy data or qualitative analysis (Link et al. 2004; Hatzenbuehler et al. 2011).
Although understanding and quantifying alcohol stigma itself is an important step in determining the impact of stigma on the recovery from alcohol problems, we are aware of few alcohol-specific stigma measures. For example, researchers have adapted vignette measures to assess the perceived stigma of both alcohol use and the receipt of alcohol treatment (Fortney et al. 2004), and the Self-Stigma in Alcohol Dependence (SSAD) scale (Schomerus et al. 2011), an adaptation of the Self-Stigma of Mental Illness Scale (SSMI; Corrigan et al. 2006) assesses the extent to which alcohol-affected persons have internalized alcohol stigma. The Perceived Devaluation-Discrimination scale (PDD) (Link, 1987), developed to assess perceived stigma regarding mental illness, has been adapted to measure the perceived stigma of AUDs, referred to as perceived alcohol stigma (PAS) (Ruan et al. 2008). Like the original measure, it assesses expectations of devaluation and discrimination by querying how “most other people” think or act towards persons with current or prior alcohol problems.
Several adaptations of the PDD for AUD/SUD, including the one examined in this paper, have been found to have strong psychometric properties, including good internal consistency (α=0.82), excellent test-retest reliability (ICC=0.93), and satisfactory content and face validity (Ruan et al. 2008; Luoma et al. 2010). As well, PAS scores have been correlated with lower mental health functioning scores and a decreased likelihood of alcohol treatment (Keyes et al. 2010; Smith et al. 2010).
Still, additional methodological work in this area is needed. In particular, the two constituents of the PDD - “perceived devaluation” (i.e., expectation of loss of status) and “perceived discrimination” (i.e., expectation of being kept at a social distance – or denied certain social opportunities, e.g., job, partner) – have not been systematically evaluated as distinct dimensions. Some have argued, that discrimination should be operationalized as a completely separate construct from stigma (Deacon 2006; Sayce 1998). However, the distinction between the two dimensions in the PDD has been obscured in some research, where a single score has been created from all items (Keyes et al 2010), or two dimensions are assumed via creation of two subscales (Smith 2010) but not psychometrically evaluated. Further, evidence from exploratory factor analysis has been presented that suggest that the positively- and negatively-worded items may induce separate latent factors that reflect “perceived acceptance and non-negative evaluation” and “perceived discrimination and negative evaluation”, respectively (Interian et al. 2010). To our knowledge, there are no confirmatory factor analytic (CFA) studies that have described the factor structure of the PDD.
In addition to the unexplored factor structure, the mechanisms through which perceived alcohol stigma may result in negative consequences have not been investigated. Modified labeling theory states that while all individuals develop perceptions of public stigma, only those who carry a stigmatized label (e.g. alcoholic) will suffer negative consequences from this awareness (Link et al. 1987). In the mental illness literature, labeled status is often inferred from the presence of prior treatment, since treated individuals may be labeled through receiving a diagnosis, or in revealing their condition to others (Corrigan 2004). Due to anticipations of devaluation and discrimination, labeled persons may react by employing coping orientations such as social withdrawal, concealment, or educating others about their condition, which are specific mechanisms hypothesized to cause further harm (Link et al. 1989; Link and Phelan 2001). Empirical work has validated that perceived stigma (Wahl 1999; Luoma et al. 2010) and experiences of rejection (Wright et al. 2000) are associated with such stigma coping orientations, and in turn, these orientations are associated with a variety of negative social consequences and psychological distress (Link et al. 1997; Link et al. 1991; Link et al. 1989). Critics maintain that the theory could be improved by incorporating evidence regarding the heterogeneity in perceived stigma (Freidl et al. 2003) as well as the varying responses that individuals have to societal labels and perceived stigma, including coping with stigma by recognizing its illegitimacy (Camp et al. 2002).
While investigations of alcohol stigma have been informed by the serious mental illness literature, the latent construct of perceived stigma, as well as mechanisms of PAS that lead to adverse consequences, may be unique. AUDs are distinct across certain dimensions (e.g. origin, harm/peril, concealability, disruptiveness) that contribute to the process and outcomes of stigma (Jones et al. 1984; Link and Phelan 2001). For example, the degree of blame and dangerousness associated with AUDs appears to be worse as compared to other mental illnesses (Schomerus et al. 2010), yet their concealability and disruptiveness may be more easily managed due to the social acceptability of drinking and the temporary nature of intoxication and hangover.
The purposes of the current study were to identify the factor structure of the alcohol-adapted PDD and to establish its construct validity, using data from nationally representative general population sample. We evaluated construct validity by examining the relationship between PAS and two proximal outcomes associated with stigma coping strategies: social network involvement and perceived interpersonal social support. Based upon early work describing modified labeling theory (Link, 1987; Link et al., 1989) we hypothesized that: 1) perceived devaluation and perceived discrimination were unique dimensions of PAS; and 2) the relationship between PAS and perceived interpersonal social support or social network involvement would be negative for persons with lifetime AUDs and magnified for those who had been labeled, operationalized by either lifetime receipt of, or having a perceived need for, alcohol treatment. While studies of modified labeling theory often only use treatment participation to infer labeling status, we also included perceived need for treatment to recognize that treatment participation is much less common for AUDs than for substance-unrelated psychiatric disorders (Kessler et al. 1996), and labeling status exists on a continuum that includes self-labeling (Thoits 1985).
METHOD
Data source
Data from Wave 1 and Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) were analyzed in this study (Grant et al. 2007). NESARC used a complex survey design to yield population-representative estimates of United States adults living in noninstitutionalized settings in 2000. Interviews for Wave 2 were conducted from 2004-2005 and included 34,653 respondents, reflecting an 86.7% follow-up rate among Wave 1 participants who were eligible for re-interview. Response at Wave 2 was not associated with age, race/ethnicity, gender, socioeconomic status, or lifetime AUD (Grant et al. 2009). The methodology and participants of NESARC have been described in prior studies (Grant et al. 2004; Grant et al. 2009).
Measures
Perceived alcohol stigma
The Wave 2 NESARC data included the 12-item Perceived Devaluation-Discrimination scale (PDD) (Link 1987), adapted for use in measuring PAS (α=0.82) (Ruan et al. 2008). The PDD was administered to all Wave 2 respondents (regardless of alcohol consumption status) after the alcohol section of the interview. Seven PDD items assessed perceived discrimination (e.g. “Most employers will pass over the application of a former alcoholic in favor of another applicant”). Five items assessed perceived devaluation, (e.g. “Most people feel that entering alcohol treatment is a sign of personal failure”). Responses were measured with a six-point Likert-type scale, ranging from strongly agree to strongly disagree. Six items used reverse wording to prevent response biases. Items with reverse wording were recoded so higher scores indicated higher levels of PAS. The PDD items, their endorsement proportions, and information about reverse wording and a priori dimensions (i.e. perceived devaluation and perceived discrimination) are provided in Supplement A.
Alcohol-affected status
To compare PAS throughout the entire sample, we divided participants into five mutually exclusive categories based on lifetime alcohol consumption, lifetime AUD, and lifetime treatment status. Categories 1-2 divided respondents who never met criteria for AUD into 1) those who never drank alcohol (“Lifetime abstainer”) and 2) those who drank alcohol, but never met criteria for AUD (“Lifetime unaffected”). Categories 3-4 reflected differences in current AUD status among those who ever met criteria for AUD, including: 3) had AUD prior to the past year, but not in the past year (“Recovered”); and 4) met criteria in the past year (“Current AUD”). Category 5 includes persons who had ever been treated for AUD or ever perceived a need for treatment (“Labeled”). Hence, categories 3 and 4 did not include persons with AUDs who received or perceived a need for alcohol treatment.
The AUDADIS-IV assessed for alcohol consumption and DSM-IV AUDs including alcohol abuse and dependence (Grant et al. 2003). Test-retest reliabilities for past-year and lifetime measures ranged from ICC=0.47-0.84 for alcohol consumption, ICC=0.76-0.89 for individual AUD symptoms, and κ=0.70-0.74 for AUD diagnoses (Grant et al. 2003). Treatment for alcohol problems was assessed at Wave 1 and Wave 2 by asking, “Have you ever gone anywhere or seen anyone for a reason that was related in any way to your drinking” while listing various sources of professional and informal (i.e. 12-step) help. Perceived need for treatment was assessed at Wave 1 and Wave 2 by asking, “Was there ever a time when you thought you see [someone] for your drinking, but didn’t go?” Reliabilities for treatment-related measures have not been published.
Perceived interpersonal social support
Twelve items assessed perceived interpersonal social support (henceforth referred to as “social support”) reflecting the interpersonal resources available to respondents at Wave 2. We reversed the scores of six items so that higher scores for all questions (on a Likert-type scale ranging from 1-4) indicated more social support. This scale exhibits good internal consistency (α=0.82) (Ruan et al. 2008).
Social network involvement
The Social Network Index (Cohen et al. 1997) assessed the extent of involvement in 10 types of social relationships separately (e.g. relatives, co-workers, neighbors) by querying the total number of persons seen or talked to every two weeks in person or via the internet or phone at Wave 2. A summed score across all relationships exhibits relatively low internal consistency (α=0.62) yet good test-retest reliability (ICC=0.70) (Hatzenbuehler et al. 2011; Ruan et al. 2008). In the NESARC data, the scale of each individual item was truncated to 50 persons yielding a final summed index with a range of 0 to 235. We truncated the individual scores to 7 persons, which provided a more normal distribution in the summed index (range 0 to 51).
Closeness to persons with AUDs
Following Keyes and colleagues (2010), we coded as positive anyone reporting alcohol problems in any first-degree relative or in any live-in relationship with a partner.
Sociodemographic characteristics
Demographic variables were assessed based on wave 2 assessment, with categories chosen to be comparable with prior NESARC stigma studies (Keyes et al., 2010; Smith et al., 2010). Race/ethnicity was based on five groupings: White; Black; Native American or Alaskan Native; Asian, Hawaiian, or Pacific Islander; and Hispanic or Latino. Hispanic or Latino ethnicity was assessed separately from race, but respondents were classified as Hispanic or Latino regardless of race category. Categorical variables were used for age (<35 years, 35-49, 50-64, and >=65), education (less than high school, high school or GED equivalent, and greater than high school), and personal income (<$20,000, $20,000-$34,999, $35,000-$59,999, and >=$60,000). Gender was analyzed with females as the reference group.
Analytic plan
We used SUDAAN version 10.0.1 (Research Triangle Institute, 2008) to calculate descriptive statistics and Mplus version 6.12 (Muthén and Muthén 1998-2010) to conduct CFA and structural equation modeling (SEM). SUDAAN uses a Taylor series linearization to adjust the standard errors of estimates to take into account the complex sampling methodology of NESARC; Mplus uses a sandwich estimator for this purpose. The weighted least squares estimator with mean and variance correction (WLSMV) is implemented in Mplus, which properly analyzes items with ordinal measurement properties (Lubke and Muthén 2004). Mplus uses all available data during estimation, thus analyses excluded respondents with missing data on all items of a scale but retained participants who had complete data or missing data on one or more items. We used simple random sampling to split the data into halves which we designated “test” and “validation” samples. All analyses were first conducted in the test sample and then verified with the validation sample for replication (i.e. a “split-half approach”). We ran CFA models using the WLSMV estimator then replicated them using the robust maximum likelihood (MLR) estimator.
Factor structure of PAS and rationale for model selection
To determine the factor structure underlying the PDD items, we computed five CFA models (see Figure 1). We examined parameter estimates and indices of global model fit, including the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and the Root Mean Square Error of Approximation (RMSEA) (Hu and Bentler 1999) to identify the best-fitting models. The Mplus DIFFTEST procedure was used to test for significant differences in fit among nested models.
Figure 1.
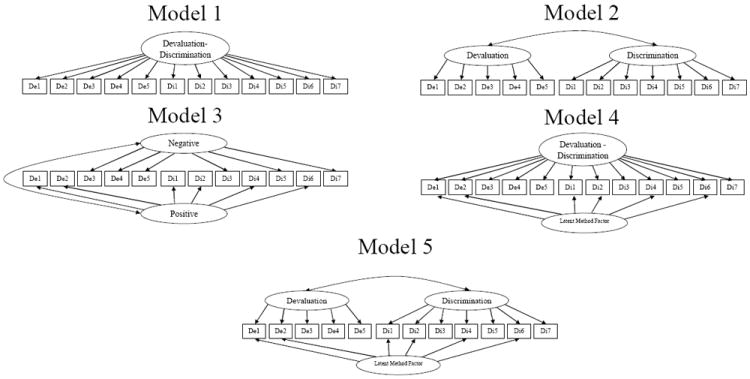
Five confirmatory factor analytic models of perceived alcohol stigma measured by the alcohol-adapted Perceived Devaluation-Discrimination scale. Model 1- One substantive factor (perceived devaluation-discrimination). Model 2- Two substantive factors (perceived devaluation and perceived discrimination). Model 3- Two substantive factors representing positive and negatively worded items (perceived devaluation/discrimination and perceived non-negative evaluation/acceptance). Model 4- One substantive factor (perceived devaluation-discrimination) and a latent method factor (LMF) to adjust for positively worded items. Model 5- Two substantive factors (perceived devaluation and perceived discrimination) and an LMF to adjust for positively worded items.
Models 1 and 2 sought to answer the question, do the data support perceived devaluation-discrimination as a single factor (model 1), or as two factors (model 2)? Model 3 attempted to determine the plausibility of positive and negative dimensions of perceived stigma as proposed by others (Interian et al. 2010). Finally, motivated by evidence from prior factor analytic studies that extracted separate “method factors” to adjust for positively- and negatively-worded items (Marsh et al. 2010), we specified Models 4 (a single PDD factor) and 5 (two PDD factors) as analogs of Models 1 and 2, while statistically adjusting for method effects. We accomplished this by specifying the positively worded items to load on a latent method factor (LMF), which ‘parses’ the item wording effects from the ‘true’ factor structure underlying the items (Marsh et al. 2010). As depicted in Figure 1, the LMF was specified to be uncorrelated with the latent factors.
Construct validity
After establishing the best-fitting CFA model, we used SEM to examine the construct validity of the latent stigma factors, by testing associations between PAS and social support and social network involvement. First we specified unadjusted and adjusted main-effects models to examine these relationships among lifetime drinkers and separately by alcohol-affected status. Next, we ran models among lifetime drinkers while including an interaction between latent PAS and alcohol-affected status, using the Mplus latent moderated structural equations approach with the maximum likelihood estimator. Lifetime abstainers were excluded from these analyses, as described later, due to the poorer model fit of the PDD in that subgroup.
RESULTS
Sample characteristics
Characteristics of NESARC respondents for the overall sample and separately by alcohol-affected status are displayed in Table 1. The weighted data are representative of the U.S. population. About 12.6% were lifetime abstainers, 52.7% drank alcohol but never met criteria for AUD (unaffected), 20.5% met criteria for AUD in their lifetime but not in the past year (recovered), 7.4% had a current AUD, and 6.8% were considered labeled. Just 13.7% of those with current AUD met criteria for the first time in the past year (not shown in the table). Among persons who were labeled, 29.8% thought that they needed treatment or received it in the past year, and the remaining met these criteria prior to the past year (also not shown). Abstainers had the highest levels of PAS, and were the least likely to have close contact with persons with alcohol problems. PAS scores were similar across the drinking groups, regardless of affected status. Those meeting criteria for AUD were more likely to be male, and to have higher levels of close contact with other persons with alcohol use problems.
Table 1.
Characteristics of Wave 2 NESARC participants overall (n=34,373) and for subgroups defined by lifetime alcohol status
| Overall | By lifetime alcohol status, % (SE) | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Characteristic | % (SE) | Abstainer (n=4,634) | Unaffected (n=18,459) | Recovered (6,640) | Current (n=2,365) | Labeled (n=2,288) | X2 (df) |
| Overall | 12.6 (0.48) | 52.7 (0.63) | 20.5 (0.54) | 7.4 (0.23) | 6.8 (0.20) | ||
| Gender | 48 (4)* | ||||||
| Male | 47.9 (0.34) | 28.7 (1.01) | 40.5 (0.53) | 62.9 (0.80) | 70.6 (0.99) | 70.7 (1.07) | |
| Female | 52.1 (0.34) | 71.3 (1.01) | 59.5 (0.53) | 37.1 (0.80) | 29.4 (0.99) | 29.3 (1.07) | |
| Age | 21 (12)* | ||||||
| <35 | 25.4 (0.39) | 21.3 (0.80) | 23.9 (0.50) | 23.6 (0.66) | 46.9 (1.32) | 26.6 (1.14) | |
| 35-49 | 31.1 (0.36) | 23.2 (0.93) | 29.3 (0.46) | 37.3 (0.73) | 32.9 (1.30) | 39.5 (1.14) | |
| 50-64 | 24.1 (0.29) | 22.0 (0.88) | 25.0 (0.37) | 25.5 (0.63) | 15.7 (0.79) | 26.6 (1.12) | |
| >=65 | 19.3 (0.34) | 33.5 (1.19) | 21.8 (0.48) | 13.6 (0.47) | 4.44 (0.46) | 7.3 (0.61) | |
| Marital status | 16 (8)* | ||||||
| Presently married | 63.8 (0.48) | 61.5 (0.94) | 65.2 (0.66) | 69.5 (0.69) | 51.3 (1.29) | 53.6 (1.20) | |
| Previously married | 18.9 (0.26) | 23.1 (0.76) | 18.9 (0.32) | 15.5 (0.48) | 15.1 (0.80) | 25.2 (1.00) | |
| Never married | 17.4 (0.45) | 15.4 (0.71) | 15.9 (0.59) | 15.0 (0.56) | 33.7 (1.29) | 21.3 (1.03) | |
| Race/ethnicity | 16 (7)* | ||||||
| White | 70.9 (1.54) | 54.7 (2.39) | 70.1 (1.65) | 80.1 (1.11) | 75.4 (1.61) | 74.8 (1.63) | |
| Black | 11.1 (0.66) | 16.0 (1.07) | 11.6 (0.76) | 7.39 (0.52) | 10.0 (0.90) | 9.7 (0.80) | |
| Native American | 2.2 (0.18) | 2.6 (0.54) | 1.6 (0.16) | 2.7 (0.32) | 2.1 (0.43) | 4.4 (0.61) | |
| Asian | 4.3 (0.52) | 10.3 (1.41) | 4.5 (0.49) | 1.7 (0.37) | 2.23 (0.59) | 1.3 (0.32) | |
| Hispanic | 11.6 (1.19) | 16.5 (1.84) | 12.2 (1.28) | 8.1 (0.85) | 10.3 (1.23) | 9.9 (1.37) | |
| Income | 15 (12)* | ||||||
| <=19,999 | 42.2 (0.55) | 64.2 (1.03) | 42.6 (0.62) | 31.6 (0.83) | 30.7 (1.00) | 42.7 (1.45) | |
| 20,000-34,999 | 23.1 (0.35) | 18.3 (0.77) | 23.8 (0.45) | 23.0 (0.67) | 25.4 (1.15) | 25.0 (1.04) | |
| 35,000-59,999 | 20.2 (0.31) | 10.5 (0.57) | 20.0 (0.41) | 24.3 (0.58) | 26.0 (0.99) | 21.0 (1.09) | |
| > 60,000 | 14.5 (0.53) | 7.1 (0.71) | 13.7 (0.54) | 21.2 (0.97) | 18.0 (1.01) | 11.3 (0.89) | |
| Education | 14 (8)* | ||||||
| <HS | 14.0 (0.45) | 25.6 (1.14) | 13.1 (0.44) | 10.3 (0.52) | 9.3 (0.73) | 16.8 (1.04) | |
| HS or GED | 27.5 (0.53) | 32.0 (1.08) | 27.5 (0.56) | 24.7 (0.80) | 26.2 (1.24) | 29.2 (1.09) | |
| >HS | 58.5 (0.63) | 42.5 (1.24) | 59.5 (0.63) | 65.0 (0.95) | 64.6 (1.29) | 54.0 (1.38) | |
| First degree relative with alcohol problems | 38.6 (0.66) | 29.5 (1.15) | 33.7 (0.69) | 46.9 (0.79) | 39.5 (1.20) | 68.3 (1.14) | 39 (4)* |
| Lives or lived with a life partner with alcohol problems | 15.5 (0.33) | 11.0 (0.53) | 13.3 (0.36) | 17.5 (0.58) | 13.9 (0.74) | 36.5 (1.23) | 38 (4)* |
| Continuous variables | Mean (SD) | F (df) | |||||
|
| |||||||
| Lifetime AUD symptom count | 1.8 (2.60) | -- | 0.4 (0.60) | 3.6 (2.09) | 4.2 (2.20) | 7.5 (2.69) | 7,238 (4)* |
| Perceived alcohol stigma (PAS) | 37.8 (8.47) | 40.1 (8.34) | 37.9 (8.41) | 36.9 (8.32) | 37.5 (8.11) | 36.5 (9.17) | 58 (4)* |
| Perceived interpersonal social support (ISS) | 42.5 (5.45) | 41.6 (6.04) | 42.8 (5.33) | 42.7 (5.24) | 42.7 (5.00) | 41.6 (6.02) | 34 (4)* |
| Social Network Involvement (SNI) | 13.7 (7.57) | 13.3 (7.85) | 13.9 (7.56) | 13.5 (7.47) | 14.1 (7.28) | 12.6 (7.44) | 15 (4)* |
Chi-square and F tests were design-based and test for overall differences in the characteristic across subgroups.
The test statistic achieved statistical significance at p <0.0001.
SE=standard error, SD=standard deviation. For continuous variables, means are reported from the observed (summed scale) scores. The summed PAS score has 1,080 missing values due to nonresponse on >2 items; mode imputation was used in the case of nonresponse to <=2 PAS items.
Dimensionality of PAS
We report the results for CFA models 1-5 in the full sample of NESARC participants. Importantly, the same patterns of model fit and factor structure emerged in the test, validation, and overall samples (see supplement B and supplement C to compare the global model fit and parameter estimates, respectively).
Of the five CFA models tested, the models that did not adjust for method effects (models 1, 2 and 3) were worse fitting. Models with a TLI and CFI greater than approximately 0.95 and an RMSEA close to 0.06 are generally considered acceptable (Hu and Bentler, 1999). Models 1 and 2, which were consistent with the summed-scale approaches to using the PDD, did not fit the data well (CFI, TLI, RMSEA all under the criteria for good fit, < .95 for CFI, TLI and > .06 for RMSEA). Model 3, which tested for a latent positive and negative dimension of stigma, fit somewhat better than Models 1 and 2 but still fell short of optimal model fit criteria. Models 4 and 5, which adjusted for method effects, had good fit. The AIC and BIC statistics generated using MLR estimation were also lower in Models 4 and 5 compared to the other models, providing additional evidence of better fit when adjusting for parsimony. Nested model comparisons indicated that model 5, which included two substantive factors of perceived discrimination and perceived devaluation, and a latent method factor, had a significantly better fit to the data than model 4, χ2 (1) = 542, p < 0.0001.
Factor loadings for models 4 and 5 are displayed in Table 2. All of the factor loadings were statistically significant at p < 0.001. The inter-factor correlation between the perceived devaluation and perceived discrimination factors in model 5 was very high, at r=0.901, indicative of low discriminant validity between the two. Thus, the remaining analyses were conducted with Model 4, which had a single PDD factor.
Table 2.
Standardized factor loadings for confirmatory factor analytic models 4 and 5 (n=34,386a NESARC wave 2 participants)
| Item | Model 4: One PDD factor with adjustment for method effects
|
Model 5: Two PDD factors with adjustment for method effects
|
|||
|---|---|---|---|---|---|
| Perceived Devaluation-Discrimination | Latent Method Factor | Perceived Devaluation* | Perceived Discrimination* | Latent Method Factor | |
| Devaluation1 | 0.385 | 0.659 | 0.395 | 0.658 | |
| Devaluation2 | 0.430 | 0.721 | 0.439 | 0.728 | |
| Devaluation3 | 0.493 | 0.506 | |||
| Devaluation4 | 0.657 | 0.676 | |||
| Devaluation5 | 0.697 | 0.720 | |||
| Discrimination1 | 0.310 | 0.580 | 0.316 | 0.581 | |
| Discrimination2 | 0.472 | 0.545 | 0.482 | 0.550 | |
| Discrimination3 | 0.548 | 0.564 | |||
| Discrimination4 | 0.480 | 0.317 | 0.496 | 0.313 | |
| Discrimination5 | 0.578 | 0.595 | |||
| Discrimination6 | 0.469 | 0.312 | 0.483 | 0.309 | |
| Discrimination7 | 0.387 | 0.395 | |||
Parameters from WLSMV-estimated models are displayed.
267 participants were excluded due to missing data on all items of the stigma scale. All freely-estimated parameters were significant at p<.001.
PDD=perceived devaluation-discrimination.
The correlation between the perceived devaluation and perceived discrimination factor was r=0.901. Global model fit for Model 4 was CFI=0.958, TLI=0.942, RMSEA=0.056. For Model 5, CFI=0.962, TLI=0.946, RMSEA=0.054.
Performance of the measure across persons affected and unaffected by alcohol
The NESARC data are unique in that perceived stigma was assessed regardless of respondents’ AUD or drinking status. Thus, we tested whether the factor configuration of the alcohol-adapted PDD held across the five status groups by conducting CFA Model 4 in each group separately. The alcohol-adapted PDD exhibited poorer fit statistics among lifetime abstainers compared to the other groups (see Supplement D).
Construct validity
We excluded the abstinent group from construct validity analyses due the poorer model fit statistics that we observed in that subgroup. The cells of Table 3 display the unadjusted and adjusted estimates of PAS for main-effects models that regressed social variables on PAS. The rows contain estimates within each analytic sample (i.e. all lifetime drinkers collapsed, and separated by AUD status), and two major column groupings contain estimates for each dependent variable. Persons with higher PAS reported lower social support and social network involvement, even after adjusting for sociodemographic characteristics and closeness to persons with alcohol problems. This finding held across all groups, regardless of AUD status.
Table 3.
The unadjusted and adjusted relationships between perceived alcohol stigma and social support and social involvement. Estimates are provided for NESARC respondents with lifetime drinking, and for subgroups defined by AUD-affected status.
| Dependent variables
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Perceived interpersonal social support
|
Social network involvement
|
|||||||
| STD β | β | SE (β) | p | STD β | β | SE (β) | p | |
| Sample | Unadjusted estimates for perceived alcohol stigma | |||||||
|
| ||||||||
| All lifetime drinkers | -0.15 | -2.01 | 0.11 | <0.001 | -0.08 | -1.58 | 0.17 | <0.001 |
| Subgroups of drinkers | ||||||||
| Lifetime unaffected | -0.14 | -2.01 | 0.15 | <0.001 | -0.09 | -1.81 | 0.23 | <0.001 |
| Recovered | -0.14 | -1.77 | 0.20 | <0.001 | -0.08 | -1.39 | 0.28 | <0.001 |
| Current AUD | -0.16 | -2.15 | 0.33 | <0.001 | -0.07 | -1.42 | 0.56 | 0.011 |
| Labeled | -0.21 | -2.86 | 0.36 | <0.001 | -0.08 | -1.33 | 0.44 | 0.003 |
|
| ||||||||
| Adjusteda estimates for perceived alcohol stigma
|
||||||||
| All lifetime drinkers | -0.13 | -1.88 | 0.11 | <0.001 | -0.06 | -1.29 | 0.17 | <0.001 |
| Subgroups of drinkers | ||||||||
| Lifetime unaffected | -0.13 | -1.83 | 0.16 | <0.001 | -0.07 | -1.41 | 0.24 | <0.001 |
| Recovered | -0.13 | -1.64 | 0.20 | <0.001 | -0.06 | -1.18 | 0.27 | <0.001 |
| Current AUD | -0.15 | -2.12 | 0.34 | <0.001 | -0.06 | -1.18 | 0.52 | 0.023 |
| Labeled | -0.19 | -2.64 | 0.34 | <0.001 | -0.07 | -1.11 | 0.43 | 0.009 |
The cells display the unadjusted and adjusted estimates for PAS. The rows contain estimates by analytic sample (i.e. all lifetime drinkers collapsed, and separated by AUD status). The two major column groupings contain estimates for each dependent variable, which were tested in separate models. All other models fit the data well (CFI & TLI > 0.95; RMSEA <0.06).
Models adjusted for race/ethnicity, age, income, education, marital status, and closeness to persons with alcohol problems. Italicized p-values are statistically significant at p <0.05.
A significant interaction effect was found when examining the relationship between PAS and social support (but not for social network involvement), in which persons classified as labeled had a significantly stronger relationship than those who were unaffected by alcohol problems (Table 4). Given similar levels of PAS, persons who were labeled reported significantly lower levels of social support than those who were unaffected; further, as PAS levels increased, labeled persons’ levels of social support were increasingly lower.
Table 4.
The adjusted relationship between perceived alcohol stigma and social support and social involvement among lifetime drinkers, dependent on alcohol-affected status
| Independent variable | Dependent variables
|
|||||
|---|---|---|---|---|---|---|
| Perceived interpersonal social support
|
Social network involvement
|
|||||
| β | SE (β) | p | β | SE (β) | p | |
| Intercept | 42.30 | 0.18 | <0.001 | 16.06 | 0.26 | <0.001 |
| Perceived alcohol stigma | -0.48 | 0.48 | <0.001 | -0.37 | 0.07 | <0.001 |
| Alcohol-affected status group | ||||||
| Lifetime unaffected (ref) | -- | -- | -- | |||
| Recovered | -0.36 | 0.10 | <0.001 | -0.66 | 0.13 | <0.001 |
| Current AUD | -0.50 | 0.12 | <0.001 | 0.13 | 0.19 | 0.508 |
| Labeled | -1.05 | 0.15 | <0.001 | -0.79 | 0.19 | <0.001 |
| Interaction term | ||||||
| PAS *Lifetime unaffected (ref) | -- | -- | -- | -- | -- | -- |
| PAS * Recovered | -0.04 | 0.08 | 0.611 | 0.01 | 0.11 | 0.902 |
| PAS * Current AUD | -0.10 | 0.12 | 0.405 | 0.13 | 0.18 | 0.465 |
| PAS * Labeled | -0.43 | 0.13 | 0.001 | 0.03 | 0.15 | 0.863 |
The two major column groupings contain estimates by each dependent variable, which were tested in separate models. Models adjusted for race/ethnicity, age, income, education, marital status, and closeness to persons with alcohol problems. Italicized p-values are statistically significant at p <0.05. Presently, standardized estimates are not available for latent variable interaction models in Mplus.
DISCUSSION
The PDD has been used widely to study the stigma of serious mental illness and has been adapted to measure the stigma of AUDs and other SUDs. To our knowledge, this is the first study to systematically evaluate the factor structure of the PDD and the construct validity of the alcohol-adapted version. A one-factor model with adjustment for method effects offered the most parsimonious solution to modeling PAS. The labeled group had the strongest inverse relationship between PAS and social support as expected, yet the same was not true for analyses involving social network involvement. Measurement and theoretical insights can be derived from these findings.
While the hypothesized two-factor model had the best fit to the data, the extremely high inter-factor correlation (r=0.9) suggested that the perceived devaluation and perceived discrimination factors had low discriminant validity (Brown 2006). Our selection of a one-factor model is consistent with the most common use of the original and adapted scales (“perceived devaluation-discrimination”) (Keyes et al. 2010; Link et al. 1989; Luoma et al. 2010). While “positive” and “negative dimensions” of perceived stigma have been proposed (Interian et al. 2010), our models did not support that structure.
Perhaps, our findings may offer insight into debates regarding whether discrimination should be distinct from a stigma construct that includes only negative social evaluations. Some have argued that such a separation would promote research studying their interplay (Deacon 2006). Our findings suggest that at least for perceived stigma, the overlap in constructs is so high that few unique properties may be identified. Our results are consistent with a prior study of racial/ethnic differences in PAS using the NESARC data in which separate scales were used for discrimination and devaluation, which found the same associations for both scales in all but one instance (Smith et al 2010). However, cross-sectional studies can inflate correlations between causally related variables, and thus to disentangle potential differences between the constructs, it may be that prospective studies that separately assess perceptions and actual experiences of devaluation and discrimination are needed.
While the factor structure was replicable across drinkers and AUD-affected groups, fit statistics were less acceptable among lifelong abstainers. To assume that an underlying construct is similar across subgroups, a scale must at a minimum exhibit the same factor configuration across groups (Horn and Mcardle 1992). Thus, comparisons of PAS in abstainers versus other groups should be interpreted with caution. Conceptions of PAS may be different for lifelong abstainers due to their lower rates of being close to persons with alcohol problems, which could magnify or alter expectations of the stigma-related experiences of AUD-affected individuals. It is also possible that reasons for lifelong abstention, such as certain religious affiliations, influence conceptions of PAS, which could be a topic for future study.
Our tests of construct validity revealed interesting findings. Our main effects models found an inverse relationship between PAS and both measures among unaffected persons, although the effect was small. Perhaps, self-reports of PAS may be confounded with variables associated with lower social support and social network involvement, which is not possible to disentangle in cross-sectional data. As well, potentially confounding variables, such as neuroticism, should be considered as control variables when assessing self-reports of stigma (Link et al. 2004; Major et al. 2002).
However, among labeled persons, there was a significantly stronger inverse relationship between PAS and social support. As such, our findings are in line with mental illness research on stigma and social support (Livingston and Boyd 2010), but differ from a prior study of perceived substance use stigma in a SUD treatment sample, where no association was found (Luoma et al. 2010). As in our study, others have reported an interaction between stigma and labeling status when examining hypothesized stigma coping orientations and consequences (Kroska and Harkness 2006; Link et al. 1997; Link et al. 1989; Link et al. 1991). Our findings suggest that the alcohol-adapted PDD may be adequate to test propositions of modified labeling theory as applied to the study of alcohol stigma. Longitudinal studies are needed to determine the directionality of the relationship between alcohol stigma and social support.
Though, we did not observe an interaction between PAS and labeling status for social network involvement. Our measure of social network involvement, however, was not specific as other studies’ measures where meaningful distinctions between in-home and out of home social network involvement could be made (Link et al. 1989; Perlick 2001). Our results might have been different if a more refined measure of social network involvement was used. On the other hand, social networks of persons with AUDs may be less affected by alcohol stigma, although the extent to which alcohol stigma contributes or not to social network composition is unknown. Others have found that heavy drinkers have very high rates of alcohol-focused friendships (Leonard et al. 2000), but whether this holds for those with AUD, or is partially driven by stigma, is an open question.
Importantly, through a systematic comparison of CFA models, we found that adjustments for method effects were necessary to achieve adequate model fit. This suggests that scores based on summed PDD items are confounded with method effects/measurement error. Future work should use a CFA approach with method effects adjustments to model PDD. Basic SEM texts describe approaches to adjust for measurement error such as correlating the uniqueness of items with similar wording (i.e. the “correlated uniqueness” approach) or using latent method factors (Brown 2006).
Limitations
The use of cross-sectional data precludes causal inferences. It is possible that increased social support leads to decreases in stigma (Mueller et al. 2006). While in stigma research, labeling status is commonly inferred from treatment receipt (as in the present study), comparisons with untreated persons may be confounded by other characteristics of treatment seekers beyond those considered here. While we also considered persons who perceived a need for treatment as labeled, sensitivity analyses indicated that the inclusion or exclusion of perceived need from our labeling criteria did not alter the findings. Also, self-reports of perceived stigma may be influenced by characteristics such as personality traits or social desirability, which were not addressed in the current analyses. While we used a split-sample approach to identify and confirm the factor structure of the PDD, these models should be replicated in other samples. Future work should evaluate the measurement invariance of the PDD to ensure that item bias does not influence differences in PAS across subgroups.
Conclusion
The alcohol-adapted PDD appears to be a psychometrically and theoretically sound instrument for measuring PAS in samples of drinkers. A one-factor solution of the alcohol-adapted PDD offered a parsimonious approach to modeling PAS. To achieve optimal model fit, statistical adjustment for method effects introduced by reverse item wording was necessary. Future work should evaluate the measure’s sensitivity to change over time, and the extent to which results are impacted by self-report bias (e.g. neuroticism). Additional existing measures should be adapted to evaluate the stigma of AUDs, such as measures of stigma coping orientations.
Supplementary Material
Acknowledgments
We thank David F. Gillespie, PhD at the George Warren Brown School of Social Work for his feedback on this project, and Dr. Bruce G. Link at the Mailman School of Public Health, Columbia University, for his generous consultations. We are also grateful for the thoughtful feedback provided by the anonymous reviewers of Alcoholism: Clinical and Experimental Research.
This investigation was supported by the National Institutes of Health (NIH) under the Ruth L. Kirschtein National Research Service Awards 5T32DA015035 and F31AA021034 (JEG), as well as grants AA12640, DA14363 (KKB) and AA11998. The funding sources had no involvement in the development or submission of this manuscript.
Footnotes
Contributors
JEG conceptualized the study’s design, conducted statistical analyses, and prepared drafts of the manuscript. SDK provided methodological consultation and edited drafts of the manuscript. KKB provided mentoring, edited drafts of the manuscript, and helped conceptualize the study’s design.
Declaration of Interest: All authors declare that they have no conflicts of interest.
References
- Brohan E, Slade M, Clement S, Thornicroft G. Experiences of mental illness stigma, prejudice and discrimination: a review of measures. BMC Health Serv Res. 2010;10:80. doi: 10.1186/1472-6963-10-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA. Standardized measures for substance use stigma. Drug Alcohol Depend. 2011;116:137–141. doi: 10.1016/j.drugalcdep.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory Factor Analyses for Applied Research. Guilford; New York, NY: 2006. [Google Scholar]
- Camp DL, Finlay WM, Lyons E. Is low self-esteem an inevitable consequence of stigma? An example from women with chronic mental health problems. Soc Sci Med. 2002;55:823–834. doi: 10.1016/s0277-9536(01)00205-2. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. JAMA. 1997;277:1940–1944. [PubMed] [Google Scholar]
- Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1:16–20. [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: Implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25:875–884. [Google Scholar]
- Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- Deacon H. Towards a sustainable theory of health-related stigma: lessons from the HIV/AIDS literature. J Community Appl Soc Psychol. 2006;16:418–425. [Google Scholar]
- Fortney J, Mukherjee S, Curran G, Fortney S, Han X, Booth BM. Factors associated with perceived stigma for alcohol use and treatment among at-risk drinkers. J Behav Health Serv Res. 2004;31:418–429. doi: 10.1007/BF02287693. [DOI] [PubMed] [Google Scholar]
- Freidl M, Lang T, Scherer M. How psychiatric patients perceive the public’s stereotype of mental illness. Social Psychiatry and Psychiatric Epidemiology. 2003;38:269–275. doi: 10.1007/s00127-003-0626-3. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Kaplan KK, Stinson FS. Source and Accuracy Statement: Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions 2007 [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, McLaughlin KA. The protective effects of social/contextual factors on psychiatric morbidity in LGB populations. Int J Epidemiol. 2011;40:1071–1080. doi: 10.1093/ije/dyr019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn JL, Mcardle JJ. A practical and theoretical guide to measurement invariance in aging research. Exp Aging Res. 1992;18:117–144. doi: 10.1080/03610739208253916. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- Interian A, Ang A, Gara MA, Link BG, Rodriguez MA, Vega WA. Stigma and depression treatment utilization among Latinos: utility of four stigma measures. Psychiatr Serv. 2010;61:373–379. doi: 10.1176/appi.ps.61.4.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones EE, Farina A, Hastorf AH, Markus H, Miller D, Scott RA. Social stigma: the psychology of marked relationships. WH Freeman; New York: 1984. [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, McLaughlin KA, Link B, Olfson M, Grant BF, Hasin D. Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol. 2010;172:1364–1372. doi: 10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroska A, Harkness SK. Stigma Sentiments and Self-Meanings: Exploring the Modified Labeling Theory of Mental Illness. Soc Psychol Q. 2006;69:325–348. [Google Scholar]
- Leonard KE, Kearns J, Mudar P. Peer networks among heavy, regular and infrequent drinkers prior to marriage. J Stud Alcohol. 2000;61:669–673. doi: 10.15288/jsa.2000.61.669. [DOI] [PubMed] [Google Scholar]
- Link BG. Understanding Labeling Effects in the Area of Mental Disorders: An Assessment of the Effects of Expectations of Rejection. Am Sociol Rev. 1987;52:96–112. [Google Scholar]
- Link BG, Cullen FT, Frank J, Wozniak J. The Social Rejection of Former Mental Patients: Understanding Why Labels Matter. Am J Sociol. 1987;92:1461–1500. [Google Scholar]
- Link BG, Cullen FT, Struening EL, Shrout P, Dohrenwend BP. A Modified Labeling Theory Approach to Mental Disorders: An Empirical Assessment. Am Sociol Rev. 1989;54:400–423. [Google Scholar]
- Link BG, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: can negative consequences of mental illness labeling be avoided? J Health Soc Behav. 1991;32:302–320. [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing Stigma. Annu Rev Sociol. 2001;27:363–385. [Google Scholar]
- Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38:177–190. [PubMed] [Google Scholar]
- Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophr Bull. 2004;30:511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc Sci Med. 2010;71:2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Lubke GH, Muthén BH. Applying Multigroup Confirmatory Factor Models for Continuous Outcomes to Likert Scale Data Complicates Meaningful Group Comparisons. Struct Equ Modeling. 2004;11:514–534. [Google Scholar]
- Luoma JB, O’Hair AK, Kohlenberg BS, Hayes SC, Fletcher L. The development and psychometric properties of a new measure of perceived stigma toward substance users. Subst Use Misuse. 2010;45:47–57. doi: 10.3109/10826080902864712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major B, Quinton WJ, McCoy SK. Antecedents and consequences of attributions to discrimination: Theoretical and empirical advances. In: Zanna MP, editor. Advances in Experimental Social Psychology. Vol. 34. Academic Press; 2002. pp. 251–330. [Google Scholar]
- Marsh HW, Scalas LF, Nagengast B. Longitudinal tests of competing factor structures for the Rosenberg Self-Esteem Scale: Traits, ephemeral artifacts, and stable response styles. Psychol Assess. 2010;22:366–81. doi: 10.1037/a0019225. [DOI] [PubMed] [Google Scholar]
- Mueller B, Nordt C, Lauber C, Rueesch P, Meyer PC, Roessler W. Social support modifies perceived stigmatization in the first years of mental illness: a longitudinal approach. Soc Sci Med. 2006;62:39–49. doi: 10.1016/j.socscimed.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 5. Muthén and Muthén; Los Angeles: 1998-2010. [Google Scholar]
- Perlick DA. Stigma as a Barrier to Recovery: Adverse Effects of Perceived Stigma on Social Adaptation of Persons Diagnosed With Bipolar Affective Disorder. Psychiatr Serv. 2001;52:1627–1632. doi: 10.1176/appi.ps.52.12.1627. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayce L. Stigma, discrimination and social exclusion: What’s in a word? Journal of Mental Health. 1998;7:331. doi: 10.1080/09638239817932. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Corrigan PW, Klauer T, Kuwert P, Freyberger HJ, Lucht M. Self-stigma in alcohol dependence: Consequences for drinking-refusal self-efficacy. Drug Alcohol Depend. 2011;114:12–17. doi: 10.1016/j.drugalcdep.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The Stigma of Alcohol Dependence Compared with Other Mental Disorders: A Review of Population Studies. Alcohol Alcohol. 2010;46:105–112. doi: 10.1093/alcalc/agq089. [DOI] [PubMed] [Google Scholar]
- Smith SM, Dawson DA, Goldstein RB, Grant BF. Examining perceived alcoholism stigma effect on racial-ethnic disparities in treatment and quality of life among alcoholics. J Stud Alcohol Drugs. 2010;71:231–236. doi: 10.15288/jsad.2010.71.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits PA. Self-Labeling Processes in Mental Illness: The Role of Emotional Deviance. Am J Sociol. 1985;91:221–249. [Google Scholar]
- Wahl OF. Mental health consumers’ experience of stigma. Schizophrenia Bull. 1999;25:467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- Wright ER, Gronfein WP, Owens TJ. Deinstitutionalization, social rejection, and the self-esteem of former mental patients. J Health Soc Behav. 2000;41:68–90. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


