Abstract
Objectives. We examined the impact of access to paid sick days (PSDs) and stay-at-home behavior on the influenza attack rate in workplaces.
Methods. We used an agent-based model of Allegheny County, Pennsylvania, with PSD data from the US Bureau of Labor Statistics, standard influenza epidemic parameters, and the probability of staying home when ill. We compared the influenza attack rate among employees resulting from workplace transmission, focusing on the effects of presenteeism (going to work when ill).
Results. In a simulated influenza epidemic (R0 = 1.4), the attack rate among employees owing to workplace transmission was 11.54%. A large proportion (72.00%) of this attack rate resulted from exposure to employees engaging in presenteeism. Universal PSDs reduced workplace infections by 5.86%. Providing 1 or 2 “flu days”—allowing employees with influenza to stay home—reduced workplace infections by 25.33% and 39.22%, respectively.
Conclusions. PSDs reduce influenza transmission owing to presenteeism and, hence, the burden of influenza illness in workplaces.
Voluntary social distancing measures, such as encouraging sick people to stay home from work, are powerful tools for controlling spread during a contagious disease outbreak.1 For example, the Centers for Disease Control and Prevention recommends that people with influenza stay home for 24 hours after their fever has resolved.2 However, not everyone is able to adhere to these recommendations: 42% of workers would not get paid if they stayed home when ill.3 Willingness to stay home when ill may thus be correlated with access to paid sick days (PSDs).4–6 In the United States, the Bureau of Labor Statistics reports that 33% of the civilian workforce lacked PSDs in 2010 and that access to PSDs varies depending on workplace size and wage level. Access to PSDs ranged from 53% in workplaces with fewer than 50 employees to 85% in workplaces with 500 or more employees and from 35% in the lowest wage quartile to 87% in the highest quartile.7
Unequal access to PSDs has been hypothesized to be a source of health disparities in the workplace. Blumenshine et al.8 proposed a model in 2008 that predicted that social determinants, including inability to take time off from work, could result in unequal levels of illness and death during an influenza pandemic. They hypothesized that staying away from work, if employed as a social distancing policy during a pandemic, was likely to be more difficult for lower-wage workers, as they would be less able to afford losing income. Those who lack PSDs at work may be at higher risk for exposure owing to colleagues not staying home when ill.9 Presenteeism (going to work or school when ill) leads to further spread of illness by infectious people. Employees who lack PSDs may go to work ill, leading to the spread of infection at work. However, the number of cases expected owing to presenteeism among employees has not previously been examined to our knowledge.
In the 2009 H1N1 pandemic, risk of exposure owing to work-related inability to engage in social distancing was significantly related to race and ethnicity.5 Furthermore, those who reported work-related barriers to social distancing, including lack of access to sick leave, had 1.08 times higher odds (P < .01) of self-reported influenza-like illness incidence compared with those who were able to engage in social distancing.4 Recent research has shown that independent of infectious disease spread in the workplace, nonfatal occupational injuries occurred at a higher rate among those without access to PSDs than among those with access to PSDs.10
Bills under consideration at multiple levels—city and state legislatures—propose providing access to PSDs for employees.11 Health impact assessments of such PSD policies have hypothesized that they would reduce workplace contagion because ill workers would stay home from work, thus reducing workplace transmission.9,12,13 These assessments did not account for the nonlinearity in infectious disease spread (each infected person can infect multiple contacts, resulting in an exponential increase in attack rate over time) or the multiple locations in which contacts can occur (households, schools, workplaces, neighborhoods).
We examined the impact of access to PSDs on influenza incidence using an agent-based model. In an agent-based model, each individual in a population is represented along with the individual’s social contact networks in households, schools, workplaces, and neighborhoods. Such a model thus permits an examination of transmission patterns in these locations. Infectious disease researchers have used agent-based models extensively to quantify policy impacts, including studies that examine the effects of vaccination and school closure policies during an influenza pandemic on disease outcomes at the overall population level.14–18 However, previous models have not examined the determinants of behavior but, instead, have usually assumed certain levels of compliance in the population.14–18 Agent-based modeling remains fairly novel among health behavior researchers studying the impact of access to resources on behavior, disease, and disparities in outcomes.19–22
We examined the impact of a universal PSD policy and alternative interventions aimed at increasing voluntary social distancing behavior by asking the following questions: How much does presenteeism contribute to disease transmission in the workplace? What proportion of transmission owing to presenteeism is from those without access to PSD? How many cases of influenza would a universal PSD policy prevent? Would alternative interventions to increase the number of days spent at home when ill have an impact on reducing workplace contagion? In keeping with calls for equity-focused health impact assessments,23,24 we have reported the effect of policies and interventions on health equity in the workplace.
METHODS
We used an open-source, agent-based modeling platform called FRED (Framework for Reconstructing Epidemic Dynamics),25 an updated version of the epidemic model used in previous pandemic intervention studies.17,18 FRED uses synthetic populations (county, state, national) on the basis of data from the American Community Survey, LandScan USA data, and census aggregated data.26 Using FRED, we mapped each household, school, and workplace to a specific geographic location and assigned agents to schools or workplaces on the basis of location, size of school or workplace, and commuting patterns.26 Each agent has a set of sociodemographic characteristics, including age, gender, race, employment status, household income, and household location. Health information (including current health status, date of infection, presence of symptoms, infectiousness, and susceptibility) is associated with each agent in FRED. During each simulated day, agents interacted with other agents who shared the same social activity locations and had a probability of disease transmission on the basis of parameters from published studies.27 We used the synthetic population of Allegheny County, Pennsylvania, (which included 1 242 755 simulated individuals living in and around the city of Pittsburgh) in this study. We assumed complete susceptibility to influenza infection in the population, as may be expected with a pandemic influenza strain.
Behavioral Parameters
For our model, we assumed that employees’ access to PSDs depended on the size of their workplace, in accordance with data from the National Compensation Survey, 2010.7 Thus, the percentage of employees with access to PSDs was 53% in workplaces with 2 to 49 employees, 58% in workplaces with 50 to 99 employees, 70% in workplaces with 100 to 499 employees, and 85% in workplaces with 500 or more employees.7 Table 1 outlines the behavioral parameters used in the model.
TABLE 1—
Behavioral Parameters Used in the Baseline, Universal PSDs, 1 Flu Day, and 2 Flu Days Model Scenarios: Allegheny County, PA
| Agent Characteristic/Parameter | Baseline | Universal PSDs Scenario | 1 Flu Day Scenario | 2 Flu Days Scenario |
| With PSDs | ||||
| % stay home | 72 | 72 | 72 | 72 |
| Average days at home | 1.7 | 1.7 | 2.7 | 3.7 |
| No PSDs | ||||
| % stay home | 52 | N/A | 72 | 72 |
| Average days at home, % (no.) | 1.7 | N/A | 52 (2.7), 20 (1.0)a | 52 (3.7), 20 (2.0)b |
Note. PSD = paid sick day. For any scenario, we assumed that a maximum of 72% (rather than 100%) of employees stayed home to reflect the fact that factors other than access to PSDs affect the decision to stay home when ill. We can expect some percentage of employees (28% in our model) to go to work ill even when given PSDs or flu days.
52% of those without PSD stayed home for 2.7 days on average and an additional 20% stayed home for 1 day on average.
52% of those without PSD stayed home for 3.7 days on average and an additional 20% stayed home for 2 days on average.
The baseline scenario of the model corresponded to current workplace patterns of employees’ stay-at-home behavior. In this baseline scenario, 72% of employees who had access to PSDs28 and 52% of those without PSDs29 stayed home when ill with influenza. In both cases, we assumed that sick employees stayed home for 1.7 days on average28 and did not interact with others in the community while confined to the home. We counted cases that resulted from exposure at work as cases owing to workplace transmission. We counted cases that resulted from exposure to a symptomatic, infectious co-worker as cases owing to presenteeism.
We compared the baseline scenario against 2 other scenarios using the model. In the “universal PSDs” scenario, we assumed that all employees had access to PSDs and, hence, behaved as those with access to PSDs did in the baseline condition: 72% stayed home for 1.7 days on average when ill with influenza. In the “flu days” scenario, we examined the impact of a hypothetical intervention in which all employees (regardless of access to PSDs) had access to 1 or 2 “flu days”—days they could stay home from work and be paid if ill with influenza. This policy was aimed at increasing the number of days employees spend at home when ill with influenza (rather than the proportion of employees who stay home from work when ill). As in the baseline scenario, we assumed that 72% of employees who had access to PSDs and 52% of employees who did not have access to PSDs stayed home when sick, but those who did stay home now spent 2.7 days (under the 1 flu day scenario) or 3.7 days (under the 2 flu days scenario) at home rather than the baseline 1.7 days. We retained the assumption that 28% of employees, whether having access to PSDs or not, continued to go to work when ill even when given flu days to reflect the fact that factors other than access to PSDs30 affect the decision to stay home when ill. Finally, we assumed that the remaining 20% of employees who did not have access to PSDs now stayed home for 1 day (under the 1 flu day scenario) or 2 days (under the 2 flu days scenario) when ill with influenza (Table 1).
We applied all scenarios to the same synthetic population in Allegheny County. Employment status for a given individual was constant over all runs. For each run, we determined an employee’s probability of having PSDs from the employee’s workplace size. We seeded the epidemic using random individuals, and, hence, the exact individuals who became sick differed from run to run. Thus, an employee’s decision to stay home was probabilistic from run to run. We performed multiple runs of the simulation for each scenario to gather population-level statistics.
Epidemiological and Statistical Calculations
We ran the model 50 times for each scenario to get reliable, population-level estimates; the time horizon for the model was 100 days, long enough to cover the epidemic outbreak. We averaged the cumulative number of employees infected in each workplace size category—2 to 49, 50 to 99, 100 to 499, and 500 or more employees—over the 50 runs to get an estimate of the proportion of employees infected owing to transmission in the workplace over the course of the epidemic (attack rate). We have reported SDs over the 50 runs. We used the final number of infections owing to transmission in workplaces, infections owing to presenteeism, and infections caused by symptomatic and asymptomatic workers to calculate odds ratios (ORs). We considered a P value < .05 to be statistically significant. We performed sensitivity analyses by examining the attack rate owing to workplace transmission and presenteeism in response to changes in the value of 1 parameter while holding all other parameters at the baseline value.
RESULTS
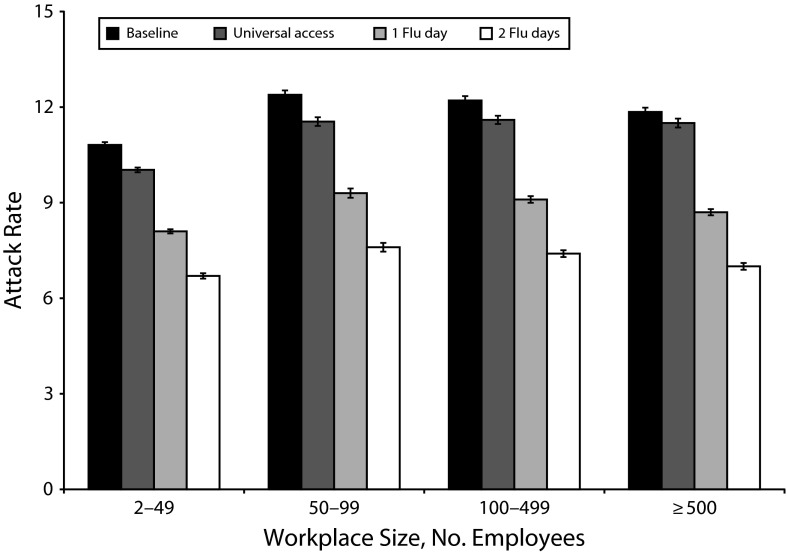
In a simulated epidemic with an influenza virus with R0 = 1.4, the attack rate among employed adults owing to workplace transmission was 11.54% (95% CI = 11.50, 11.57). On average, there were 66 444 infections overall owing to workplace transmission, including 47 768 infections owing to presenteeism among 575 866 employees in Allegheny County. The attack rate (owing to workplace transmission) in each workplace size category is shown in Figure 1. Under this baseline condition, an employee had 1.17 times higher odds of being infected by someone without PSDs engaging in presenteeism than of being infected by someone with PSDs engaging in presenteeism (95% CI = 1.13, 1.21), suggesting that providing universal access to PSDs could affect the workplace influenza attack rate by decreasing presenteeism.
FIGURE 1—
Percentage of employees infected owing to workplace transmission in workplaces in each size category: Allegheny County, PA.
Note. Averages over 50 model runs for baseline, universal access to paid sick days, 1 flu day, and 2 flu day scenarios are shown. Error bars reflect SD from the average.
Universal Paid Sick Days Scenario
Under the assumption that all employees had access to PSDs, the overall attack rate among employees owing to workplace transmission was 10.86% (95% CI = 10.83, 10.89). There were 62 548 infections owing to workplace transmission among employed adults. Thus, a universal PSD policy resulted in 3896 fewer infections owing to workplace transmission (i.e., a 5.86% decrease in attack rate in the workplace) including 3530 fewer infections owing to presenteeism (i.e., a 7.39% decrease) compared with the baseline scenario. The attack rate (owing to workplace transmission) in each workplace size category is shown in Figure 1. Workplaces with 2 to 49 employees had a 7.24% decrease in infections, workplaces with 50 to 99 employees had a 6.80% decrease, workplaces with 100 to 499 employees had a 5.18% decrease, and workplaces with 500 or more employees had a 3.34% decrease in infections owing to workplace transmission under a universal PSD policy compared with the baseline scenario.
Flu Days Scenarios
The flu days policy allowed employees to stay home from work for 1 or 2 additional PSDs when ill with influenza. When employees had access to 1 flu day, the overall attack rate among employees owing to workplace transmission was reduced from 11.54% in the baseline scenario to 8.62% (95% CI = 8.59, 8.64). There were 49 611 infections owing to workplace transmission among employees. Thus, a 1 flu day policy resulted in 16 833 fewer infections owing to workplace transmission (i.e., a 25.33% decrease), including 15 182 fewer infections owing to presenteeism (i.e., a 31.78% decrease) compared with the baseline. The attack rate owing to workplace transmission in each workplace size category is shown in Figure 1. Workplaces with 2 to 49 employees had a 24.66% decrease, 50 to 99 employee workplaces had a 24.93% decrease, 100 to 499 employee workplaces had a 25.76% decrease, and workplaces with 500 or more employees had a 26.42% decrease in infections owing to workplace transmission from a 1 flu day policy.
When employees had access to 2 flu days, the overall attack rate owing to workplace transmission among employees was 7.01% (95% CI = 6.98, 7.04). There were 40 385 cases owing to workplace transmission, that is 26 059 fewer cases (a 39.22% decrease) including 23 427 fewer cases owing to presenteeism (a 49.04% decrease) compared with the baseline scenario. The attack rate owing to workplace transmission in each workplace size category is shown in Figure 1. Workplaces with 2 to 49 employees had a 38.38% decrease, 50 to 99 employee workplaces had a 39.01% decrease, 100 to 499 employee workplaces had a 39.39% decrease, and workplaces with 500 or more employees had a 40.77% decrease in attack rate owing to workplace transmission from a 2 flu days policy.
Equity Assessment of Interventions
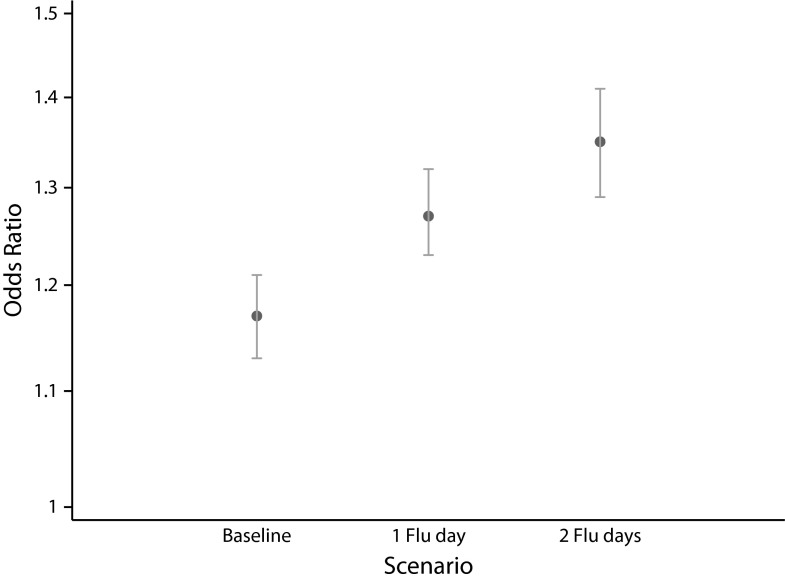
Whereas a universal PSD policy would remove the inequity in access to PSDs among employees, the same is not true for an intervention granting flu days, assuming that employees receive flu days over and above any PSDs they may already have access to. We therefore examined the impact of providing flu days on the odds of being infected owing to presenteeism by someone without access to PSDs compared with someone with access to PSDs. We found that an employee’s odds of being infected by someone without PSDs engaging in presenteeism compared with the odds of being infected by someone with PSDs engaging in presenteeism increased from 1.17 (95% CI = 1.13, 1.21) in the baseline scenario to 1.27 (95% CI = 1.23, 1.32) when employees had access to 1 flu day (P < .001) and to 1.35 (95% CI = 1.29, 1.41) when employees had access to 2 flu days (P < .001; Figure 2).
FIGURE 2—
Odds ratio of being infected by workplace transmission owing to presenteeism by those without access to paid sick days compared with those with paid sick days in the baseline, 1 flu day, and 2 flu day scenarios: Allegheny County, PA.
Note. Whiskers indicate standard deviation from the average.
Compared with the baseline scenario in which 39.01% of infections resulting from presenteeism were caused by those without access to PSDs, 41.14% of infections resulting from presenteeism were caused by those without access to PSDs under the 1 flu day policy, and 42.57% of infections resulting from presenteeism were caused by those without access to PSDs under a 2 flu days policy. Thus, compared with the baseline condition, flu day policies resulted in those without PSDs contributing a greater proportion of influenza transmission in the workplace than did those with PSDs.
Sensitivity Analyses
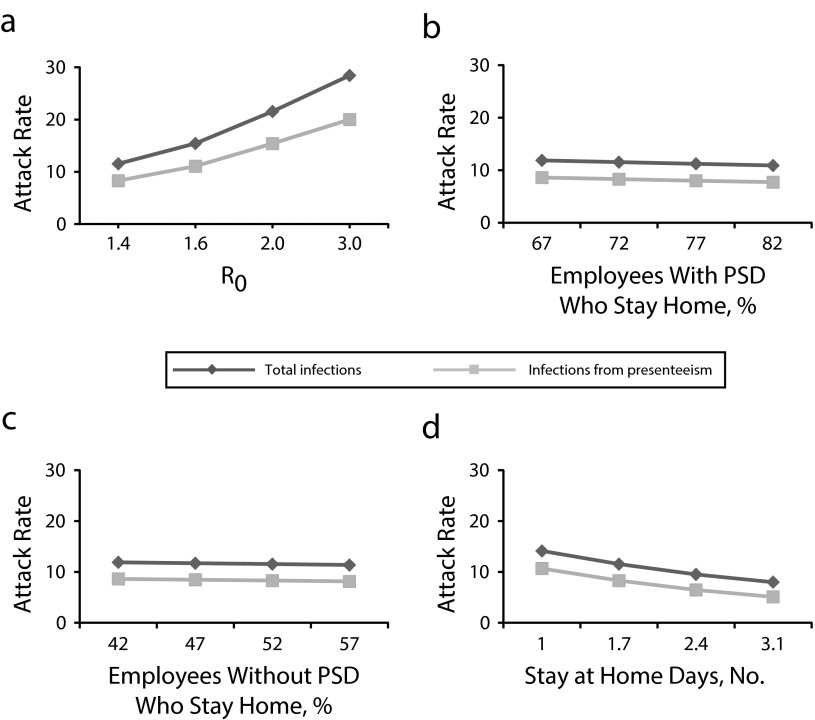
Figure 3 presents the sensitivity of workplace influenza attack rate to the reproductive rate, R0, and behavioral parameters (proportion of employees with and without PSDs who stay home from work when ill and the number of days spent away from work). Workplace attack rate is highly sensitive to virus R0, as expected (Figure 3a). Increases (and decreases) in the proportion of employees who stay home from work if ill (with or without access to PSDs) had a somewhat small impact on attack rate; for example, a 10 percentage-point increase in the proportion of those with PSDs who stayed home from work decreased the attack rate by 0.64% (Figure 3b). Increasing the number of days that employees with influenza spend at home by 0.7 days (17% of the average 4.1-day influenza infectious period) compared with baseline decreased the attack rate by 2.02% (Figure 3d).
FIGURE 3—
Sensitivity of percentage of employees infected during the epidemic owing to workplace transmission and percentage infected owing to presenteeism to (a) reproductive rate (R0), (b) percentage of employees with paid sick days who stay home from work when ill, (c) percentage of employees without PSDs who stay home from work when ill, (d) and number of days spent at home on average when sick with influenza: Allegheny County, PA.
Note. PSD = paid sick day.
DISCUSSION
This is the first study to our knowledge to employ modeling to assess the impact of a universal PSD policy on infectious disease transmission in the workplace. Our results show that universal access to PSDs would reduce influenza infections in the workplace by 5.86%, and an alternative intervention (flu days) aimed at increasing time spent away from work when ill would reduce infections in the workplace by 25.33% (1 flu day) or 39.22% (2 flu days) compared with baseline. Employees staying home from work when symptomatic with influenza, that is, a reduction in presenteeism, drove the reduction in attack rate in all 3 scenarios. In contrast to universal PSDs, which would result in a higher percentage reduction in the attack rate in small workplaces, flu days would cause greater reductions in the attack rate in large workplaces. Simulated influenza attack rates in the workplace were sensitive to increases in the proportion of people (with and without PSD) staying home when ill as well as to an increase in the time spent away from work.
Limitations
The current model made several simplifying assumptions that should be explored in further research. One limitation in our model is the assumption of complete mixing in a given workplace. Research has shown that networks in workplaces are characterized by high levels of clustering,31–33 suggesting that although infectious disease may not spread rapidly throughout a workplace, infection may occur in clusters of employees. Research on homophily in organizations suggests that assortative mixing may occur by race/ethnicity and gender.34–36 It is not known whether employees engage in assortative mixing in the workplace by access to PSDs. Under the flu day policies modeled here, employees were more likely to be infected by those without PSDs than by those with PSDs; if the recipients of this infection also lack PSDs (or share attributes such as income level or race with the infector), disparities in infection could result. For future studies, it may therefore be important to gather empirical estimates of workplace encounter networks—especially by socioeconomic factors such as income and social class—to allow an examination of potential infection clusters in workplaces, that is, not only who contributes to transmission in the workplace but also who the recipients of influenza transmission are.
Under our assumptions of stay-at-home behavior among employees (72% stay home when ill if they have access to PSDs; 52% without access stay home when ill; duration of staying home is 1.7 days on average), a universal PSD policy would reduce the attack rate owing to workplace transmission by 5.86% compared with baseline. Yet, in removing disparities in access to PSDs, a universal PSD policy could pave the way for more effective interventions (e. g., access to flu days) to have a more equitable impact on reducing influenza burden among employees. Furthermore, the impact of a universal PSD policy was inversely related to workplace size. Small workplaces, which have lower baseline levels of access to PSDs, would have a larger reduction in workplace infections than would larger workplaces.
In our sensitivity analyses, there was a larger reduction in the number of workplace infections in response to increases in the number of days that employees stay home when ill than to increases in the proportion of people staying home. Recent research on the impact of the paid family leave act in California shows that rates of family leave usage increased in response to the new law even in workplaces that previously made family leave available to employees.37 This suggests that a public endorsement for paid leave could change the social norm, resulting in an increase in rates of leave usage even among those who had access before policy enactment. In the case of a universal PSD law, people who did not previously have access to PSDs would be more likely to stay home when ill when they receive access to PSDs, but such a policy may lead to an increase in the proportion of people who stay home when ill even among those who previously had access to PSDs. Thus, flu days and health education campaigns to increase time spent away from work when ill with influenza, in conjunction with universal access to PSDs, may have the largest impact on reducing overall workplace infection rates. Future research should examine the economic impacts of a universal PSD policy as well as additional impacts such as the attack rate in schools, which may change as a result of employed parents’ ability to stay home from work and keep ill children home from school.
Conclusions
Multiple factors—including cognitive factors such as guilt associated with missing work and concern about work not getting done as well as social determinants such as job security and access to PSDs3,6,30,38—affect employees’ decision to stay home from work when experiencing influenza-like illness symptoms. We focused on access to PSDs to understand its contribution to this important behavior and to the subsequent spread of influenza-like illness in the workplace. Future research should examine the interaction between individual-level cognitive factors (e.g., worker attitudes toward staying home from work when ill) and contextual factors (e.g., availability of PSDs in the workplace and managerial and peer attitudes toward utilization of PSD) in relation to voluntary stay-at-home behavior among employed adults.
Acknowledgments
This work was supported by the National Institute of General Medical Sciences (grant U54GM088491).
Note. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the article.
Human Participant Protection
Institutional review board approval was not needed because this study used secondary data.
References
- 1.Public Health and Law Enforcement Emergency Prepardness Workgroup. Coordinated implementation of community response measures (including social distancing) to control the spread of pandemic respiratory disease. 2008. Available at: http://www.supreme.courts.state.tx.us/emtf/pdf/CRM-MOU-ReviewCopy.pdf. Accessed March 14, 2013.
- 2. CDC says “take 3” actions to fight the flu. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/flu/protect/preventing.htm. Accessed September 18, 2012.
- 3.Blendon RJ, Koonin LM, Benson JM et al. Public response to community mitigation measures for pandemic influenza. Emerg Infect Dis. 2008;14(5):778–786. doi: 10.3201/eid1405.071437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar S, Quinn SC, Kim KH, Daniel LH, Freimuth VS. The impact of workplace policies and other social factors on self-reported influenza-like illness incidence during the 2009 H1N1 pandemic. Am J Public Health. 2012;102(1):134–140. doi: 10.2105/AJPH.2011.300307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quinn SC, Kumar S, Freimuth VS, Musa D, Casteneda-Angarita N, Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health. 2011;101(2):285–293. doi: 10.2105/AJPH.2009.188029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sumner S, Brown LG, Frick R et al. Factors associated with food workers working while experiencing vomiting or diarrhea. J Food Prot. 2011;74(2):215–220. doi: 10.4315/0362-028X.JFP-10-108. [DOI] [PubMed] [Google Scholar]
- 7.Employee Benefits in the United States. Washington, DC: US Bureau of Labor Statistics; March 2010. [Google Scholar]
- 8.Blumenshine P, Reingold A, Egerter S, Mockenhaupt R, Braveman P, Marks J. Pandemic influenza planning in the United States from a health disparities perspective. Emerg Infect Dis. 2008;14(5):709–715. doi: 10.3201/eid1405.071301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.A Health Impact Assessment of the Healthy Families Act of 2009. Oakland, CA: Human Impact Partners and San Francisco Department of Public Health: June 2009. [Google Scholar]
- 10.Asfaw A, Pana-Cryan R, Rosa R. Paid sick leave and nonfatal occupational injuries. Am J Public Health. 2012;102(9):e59–e64. doi: 10.2105/AJPH.2011.300482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. National Partnership for Women and Families. State and local action on paid sick days. 2012. Available at: http://www.nationalpartnership.org/site/DocServer/NP_PSD_Tracking_Doc.pdf?docID=1922. Accessed May 31, 2012.
- 12.Lovell V. Valuing Good Health in San Francisco: The Costs and Benefits of a Proposed Paid Sick Days Policy. Washington, DC: Institute for Women’s Policy Research; 2006. [Google Scholar]
- 13.Heymann J, Rho HJ, Schmitt J, Earle A. Ensuring a healthy and productive workforce: comparing the generosity of paid sick day and sick leave policies in 22 countries. Int J Health Serv. 2010;40(1):1–22. doi: 10.2190/HS.40.1.a. [DOI] [PubMed] [Google Scholar]
- 14.Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006;442(7101):448–452. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee BY, Bailey RR, Wiringa AE et al. Economics of employer-sponsored workplace vaccination to prevent pandemic and seasonal influenza. Vaccine. 2010;28(37):5952–5959. doi: 10.1016/j.vaccine.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee BY, Brown ST, Cooley P et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract. 2010;16(3):252–261. doi: 10.1097/PHH.0b013e3181ce594e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee BY, Brown ST, Cooley PC et al. A computer simulation of employee vaccination to mitigate an influenza epidemic. Am J Prev Med. 2010;38(3):247–257. doi: 10.1016/j.amepre.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee BY, Brown ST, Korch GW et al. A computer simulation of vaccine prioritization, allocation, and rationing during the 2009 H1N1 influenza pandemic. Vaccine. 2010;28(31):4875–4879. doi: 10.1016/j.vaccine.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Auchincloss AH, Diez Roux AV. A new tool for epidemiology: the usefulness of dynamic-agent models in understanding place effects on health. Am J Epidemiol. 2008;168(1):1–8. doi: 10.1093/aje/kwn118. [DOI] [PubMed] [Google Scholar]
- 20.Auchincloss AH, Riolo RL, Brown DG, Cook J, Diez Roux AV. An agent-based model of income inequalities in diet in the context of residential segregation. Am J Prev Med. 2011;40(3):303–311. doi: 10.1016/j.amepre.2010.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang Y, Diez Roux AV, Auchincloss AH, Rodriguez DA, Brown DG. A spatial agent-based model for the simulation of adults’ daily walking within a city. Am J Prev Med. 2011;40(3):353–361. doi: 10.1016/j.amepre.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galea S, Riddle M, Kaplan GA. Causal thinking and complex system approaches in epidemiology. Int J Epidemiol. 2010;39(1):97–106. doi: 10.1093/ije/dyp296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simpson S, Mahoney M, Harris E, Aldrich R, Stewart-Williams J. Equity-focused health impact assessment: a tool to assist policy makers in addressing health inequalities. Environ Impact Asses. 2005;25(7–8):772–782. [Google Scholar]
- 24.Bonnefoy J, Morgan A, Kelly MP, Butt J, Bergman V. 2007. Constructing the evidence base on the social determinants of health: a guide. Available at: http://www.who.int/social_determinants/knowledge_networks/add_documents/mekn_final_guide_112007.pdf. Accessed March 14, 2013. [Google Scholar]
- 25.Grefenstette J, Brown ST, Rosenfeld R . Framework for reconstructing epidemic dynamics (FRED) user guide. 2013. Available at: http://www.midas.pitt.edu/FRED/FRED_UserGuide.pdf. Accessed January 24, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.RTI International. US synthesized population 2005–2009 Version 2.0. 2012. Available at: https://www.epimodels.org/midasdocs/SynthPop/2005-2009_synth_pop_ver2_quickstart.pdf. Accessed September 25, 2012. [Google Scholar]
- 27.Longini IM, Jr, Nizam A, Xu S et al. Containing pandemic influenza at the source. Science. 2005;309(5737):1083–1087. doi: 10.1126/science.1115717. [DOI] [PubMed] [Google Scholar]
- 28.Palmer LA, Rousculp MD, Johnston SS, Mahadevia PJ, Nichol KL. Effect of influenza-like illness and other wintertime respiratory illnesses on worker productivity: the Child and Household Influenza-Illness and Employee Function (CHIEF) study. Vaccine. 2010;28(31):5049–5056. doi: 10.1016/j.vaccine.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 29.Clemans-Cope L, Perry CD, Kenney GM, Pelletier JE, Pantell MS. Access to and use of paid sick leave among low-income families with children. Pediatrics. 2008;122(2):e480–e486. doi: 10.1542/peds.2007-3294. [DOI] [PubMed] [Google Scholar]
- 30.National Foundation for Infectious Diseases. Flu in the Workplace: Key Facts and Figures. Bethesda, MD: National Foundation for Infectious Diseases; 2006. [Google Scholar]
- 31.Read JM, Eames KT, Edmunds WJ. Dynamic social networks and the implications for the spread of infectious disease. J R Soc Interface. 2008;5(26):1001–1007. doi: 10.1098/rsif.2008.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Danon L, House TA, Read JM, Keeling MJ. Social encounter networks: collective properties and disease transmission. J R Soc Interface. 2012;9(76):2826–2833. doi: 10.1098/rsif.2012.0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smieszek T, Burri E, Scherzinger R, Scholz R. Collecting close-contact social mixing data with contact diaries: reporting errors and biases. Epidemiol Infect. 2012;140(4):744–752. doi: 10.1017/S0950268811001130. [DOI] [PubMed] [Google Scholar]
- 34.Brass DJ. Men’s and women’s networks: a study of interaction patterns and influence in an organization. Acad Manage J. 1985;28(2):327–343. [Google Scholar]
- 35.Ibarra H. Homophily and differential returns: sex differences in network structure and access in an advertising firm. Adm SCI Q. 1992;37(3):422–447. [Google Scholar]
- 36.McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: homophily in social networks. Annu Rev Sociol. 2001;27:415–444. [Google Scholar]
- 37.Houser L, Vartanian T. Policy Matters: Public Policy, Paid Leave for New Parents, and Economic Security for US Workers. New Brunswick, NJ: Center for Women and Work, Rutgers University; 2012. [Google Scholar]
- 38.Steers RM, Rhodes SR. Major influences on employee attendance: a process model. J Appl Psychol. 1978;63(4):391–407. [Google Scholar]